Summary
Background
Hypertension has long been recognised as a major risk factor for coronary artery disease, stroke and kidney disease. Despite a multitude of new pharmacological agents, in the Sudan, a significant proportion of hypertensive patients’ blood pressure remains uncontrolled. An important, often underutilised treatment approach is therapeutic lifestyle changes (TLC). This study aimed to assess the knowledge, attitude and practice of patients with regard to TLC in the management of hypertension in a Khartoum locality in 2016.
Methods
The study was cross sectional and descriptive. Data were collected via structured interviews using a questionnaire. Full coverage of patients attending Ahmed Gasim and Al-Shaab hospitals for follow up during August and September 2016 was carried out. Descriptive and inferential statistics were utilised for data analysis.
Results
We identified 112 patients for participation in this study. There was a slight preponderance of females (54.5%) and older age, with 58% in the 55- to 70-year age group. When assessed for knowledge on lifestyle and habits that affect blood pressure, respondents were most familiar with the fact that salt consumption affects blood pressure, 93.8% answering correctly. After knowledge scores were calculated, only 31.3% of participants had above-average knowledge on blood pressure and TLC. The lifestyle change the respondents were least adherent to was regular exercise, with 59.8% of participants struggling with this. Participants’ most-cited obstacle was lack of motivation, the same answer being most frequent for each lifestyle change.
Conclusion
This study demonstrated that although the hypertensive patients were generally aware of the importance of TLC in its management, they struggled to implement this. The researcher believes that novel approaches are needed to help motivate patients who are diagnosed with hypertension in a third-world country such as Sudan, and apply their knowledge regarding TLC.
Keywords: hypertension, lifestyle changes, Sudan, exercise, blood pressure
Hypertension is generally defined as sustained blood pressure at rest above 140/90 mmHg or the need for antihypertensive medication.1 It has long been recognised as a major risk factor for coronary artery disease, stroke and kidney disease. Responsible for up to 50% of deaths worldwide, the prevalence of hypertension has a large impact on the health economies of both developed and developing countries.2 Available data suggest that Sudan has one of the highest incidences of hypertension in Africa, with prevalence rates of 20% reported in the general population.3
Despite a multitude of new pharmacological agents, a significant proportion of hypertensive patients’ blood pressure remains uncontrolled in the Sudan.4 An important, often underutilised treatment approach is therapeutic lifestyle changes (TLC). This involves the modification of certain aspects of a patient’s lifestyle, mainly restricting sodium-rich foods, weight loss, increased physical activity, smoking cessation and moderation of alcohol intake.5
Hypertension is a common, treatable disease, with uncontrolled hypertension having serious multisystem sequelae.6 Considering this and the global and local trends of increasing prevalence of hypertension, ensuring compliance with antihypertensive measures should be a high priority. In addition, given the economic constraints due to the high cost and side-effect profile of antihypertensive drugs, adoption of a healthy lifestyle remains the cornerstone of hypertension management.
Understanding, implementation of and compliance with TLC are challenging aspects in the management of hypertension due to varying socio-economic backgrounds, education levels and time afforded for consultations. This study examined these factors to elucidate their relative association with compliance as well as patients’ overall understanding of TLC. Understanding these will allow physicians to emphasise aspects of TLC that are poorly understood by patients, as well as highlighting potential barriers to TLC implementation, in order to advise public health policy.
Methods
This was a cross-sectional, descriptive, analytical study. Hypertension clinics in Ahmed Gasim Hospital and El-Shaab Teaching Hospital were utilised as the study area. The Ahmed Gasim Hospital is a state hospital located in Khartoum North. It has three specialities, paediatrics, renal and cardiology, but no accident and emergency unit. It accepts referrals from other hospitals. It currently has three cardiology wards with a total of 30 beds, and two coronary care units (CCU) with a total of 20 beds. Cardiology referral clinics and echocardiography are carried out every day of the week.
The El-Shaab Teaching Hospital is a government hospital specialising in cardiology. It is located in the centre of Khartoum. It has three main specialities, cardiology, renal and neurology. There are two cardiology wards for male and female patients with a total of 48 beds, a CCU with six beds and two intermediatecare units attached to the CCU, accommodating 12 beds. Cardiology referral clinics are available every day of the week.
Patients between the ages of 25 and 70 years attending follow up at the cardiology referral clinics in the Ahmed Gasim and El-Shaab hospitals who were previously diagnosed as hypertensive made up the study population. Patients with co-morbidities and those who had had a previous cardiovascular event were included. Patients excluded were those who did not give consent to participate or were admitted to hospital.
There was no sample frame since the sampling was non-probability due to the lack of a registry for hypertension patients. The sample selection method was full coverage of hypertensive patients attending the cardiology referral clinic of El-Shaab Teaching Hospital on Sundays, Tuesdays and Thursdays during the period from 14 August to 1 September 2016 and of all hypertensive patients attending the cardiology referral clinic of Ahmed Gasim Hospital on Sundays, Tuesdays and Thursdays during the period from 4 to 22 September 2016.
Ethical approval for this study was obtained from the ethics review board at the University of Khartoum. Informed verbal consent for participation was obtained from each subject in the study. The author declares no conflict of interest. Information obtained from subjects was held confidentially and used strictly for academic purposes only.
Statistical analysis
A structured interview using an anonymous questionnaire was used for collection of data. Descriptive and inferential statistics were used for data analysis. Software used was SPSS version 21.0.
Independent variables were socio-demographic data of patients, occurrence of previous cardiovascular events, duration of consultations and knowledge level. Dependent variables were different levels of TLC implementation and knowledge level.
Results
We identified 112 hypertensive patients for inclusion in the study, with 100% consenting and completing the study. Of the participants, there was a slight preponderance of females (54.5%) and older age, with 58% in the 55- to 70-year age group, the majority being married (88.4%). Participants were of varying education levels, with primary school education the most frequently attained level of education (27.7%). A high proportion of participants were unemployed (43.8%) and most had not experienced a previous cardiovascular event (67.9%). Table 1 shows the demographics of the study population.
Table 1. Socio-demographic characteristics of the participants.
| Characteristics | Number | Percentage |
| Gender | ||
| Male | 51 | 45.5 |
| Female | 51 | 45.5 |
| Age, years | ||
| 25-39 | 9 | 8 |
| 40-54 | 38 | 33.9 |
| 55-70 | 65 | 58 |
| Marital status | ||
| Single | 6 | 5.4 |
| Married | 99 | 88.4 |
| Widowed | 4 | 3.6 |
| Divorced | 3 | 2.7 |
| Education level | ||
| Primary school | 31 | 27.7 |
| Secondary school | 24 | 21.4 |
| Higher education | 15 | 13.4 |
| Illiterate | 23 | 20.5 |
| Khalwa | 19 | 17 |
| Occupation | ||
| Unemployed | 49 | 43.8 |
| Labourer | 3 | 2.7 |
| Service job | 18 | 16.1 |
| Self employed | 24 | 21.4 |
| Retired | 18 | 16.1 |
| Previous cardiovascular event | ||
| Yes | 36 | 32.1 |
| No | 76 | 67.9 |
Knowledge
To determine the participants’ level of knowledge on blood pressure and therapeutic lifestyle changes, respondents were asked seven questions, five pertaining to lifestyle changes, one question on the ideal blood pressure and one on the general management of hypertension. Respondents were then given a score out of seven depending on their answers, and categorised as ‘below average’, ‘average’ or ‘above average’ in knowledge level.
Regarding ideal blood pressure knowledge, 53.6% of respondents did not know what their ideal blood pressure should be (Fig. 1). When asked what the optimal mode of hypertension management was, most patients (73.2%) answered correctly, stating both antihypertensives and lifestyle changes.
Fig. 1.
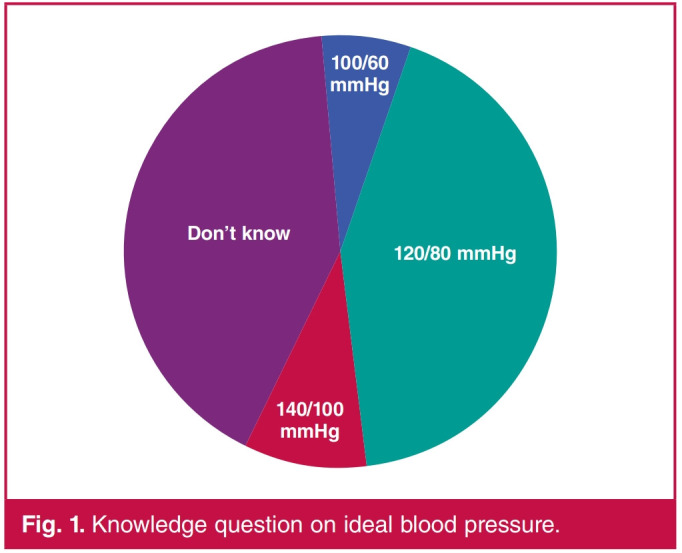
Knowledge question on ideal blood pressure.
When assessed for knowledge on lifestyle and habits that affect blood pressure, respondents were most familiar with the fact that salt consumption affects blood pressure, 93.8% answering correctly. Alcohol’s effect on blood pressure was the least familiar to participants, 53.6% answering that alcohol doesn’t affect blood pressure. Table 2 shows participants’ response to knowledge questions.
Table 2. Participants’ response to knowledge questions.
| Question | Answer | Number | Percentage |
| Salt consumption | Yes | 105 | 93.8 |
| No | 7 | 6.3 | |
| Being overweight | Yes | 74 | 66.1 |
| No | 38 | 33.9 | |
| Exercise | Yes | 80 | 71.4 |
| No | 32 | 28.6 | |
| Smoking | Yes | 64 | 57.1 |
| No | 48 | 42.9 | |
| Alcohol consumption | Yes | 52 | 46.4 |
| No | 60 | 53.6 |
Knowledge scores were calculated from the seven questions on knowledge and categorised into below-average (zero to three correct answers), average (four to five correct answers) and above-average (six to seven correct answers) knowledge levels. Only 31.3% of participants had above-average knowledge on blood pressure and TLC, most respondents answering more than two questions incorrectly. Fig. 2 gives overall knowledge scores.
Fig. 2.
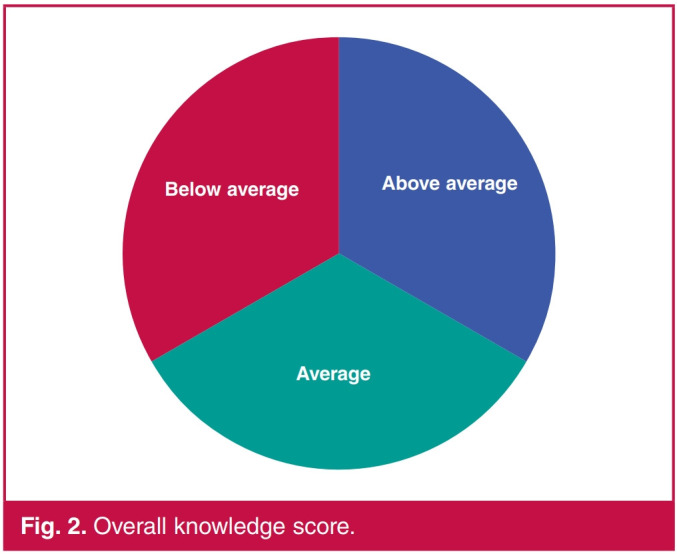
Overall knowledge score.
Regarding participants’ perception of consultation with doctors, they were asked specifically about each lifestyle change they were counselled upon and the perceived duration they thought they were counselled for on lifestyle changes by a medical professional (Table 3). Seventeen respondents said they were never counselled on lifestyle changes, while of those who were counselled, the most frequent perceived duration of consultation was reported to be ‘less than five minutes’ (33.9%) (Fig. 3).
Table 3. Which lifestyle changes participants received counselling on.
| Lifestyle change | Answer | Number | Percentage |
| Salt consumption | Yes | 81 | 72.3 |
| No | 31 | 27.7 | |
| Being overweight | Yes | 48 | 42.9 |
| No | 64 | 57.1 | |
| Exercise | Yes | 53 | 47.3 |
| No | 59 | 52.7 | |
| Smoking | Yes | 45 | 40.2 |
| No | 67 | 59.8 | |
| Alcohol consumption | Yes | 24 | 21.4 |
| No | 88 | 78.6 |
Fig. 3.
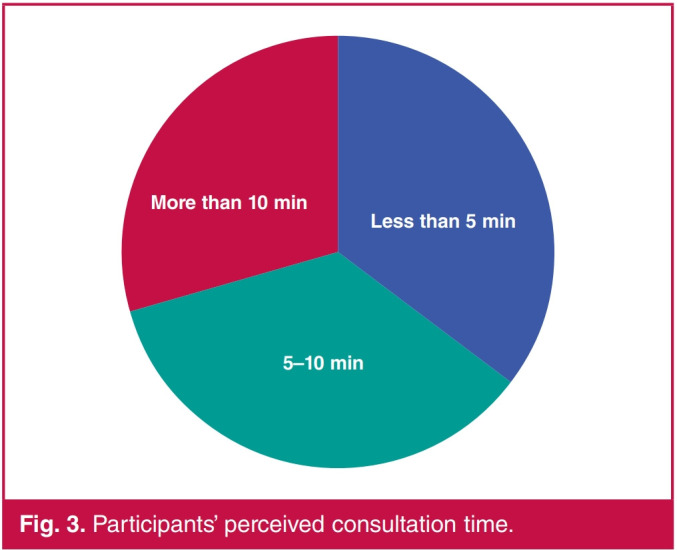
Participants’ perceived consultation time.
Fig. 4.
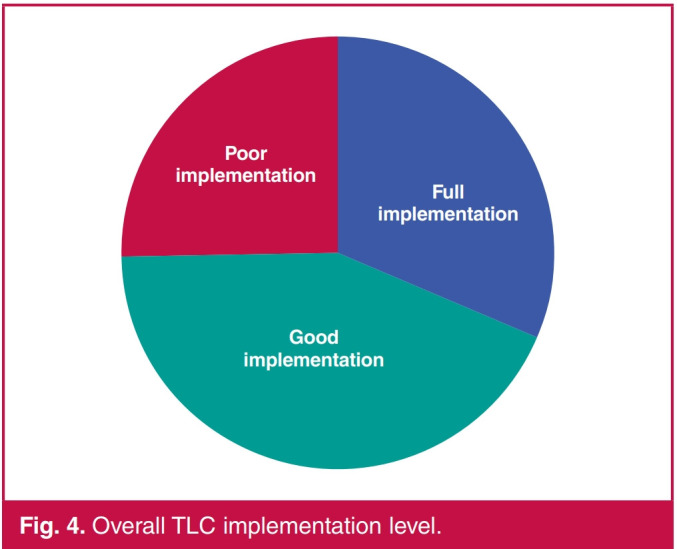
Overall TLC implementation level.
Fig. 5.
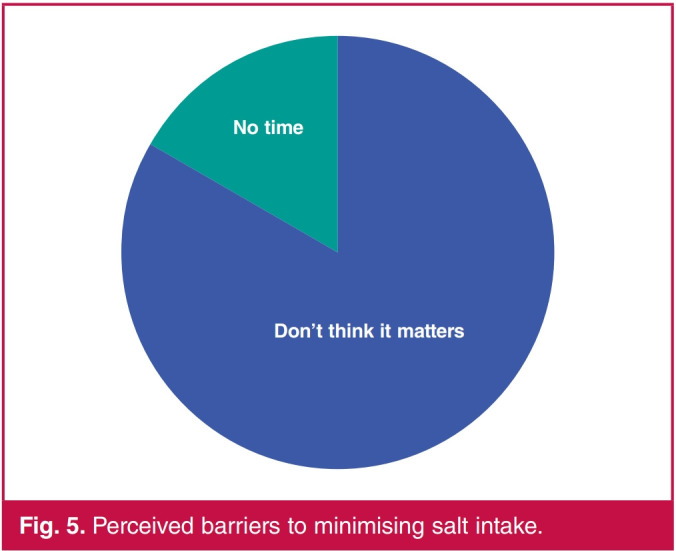
Perceived barriers to minimising salt intake.
Fig. 6.
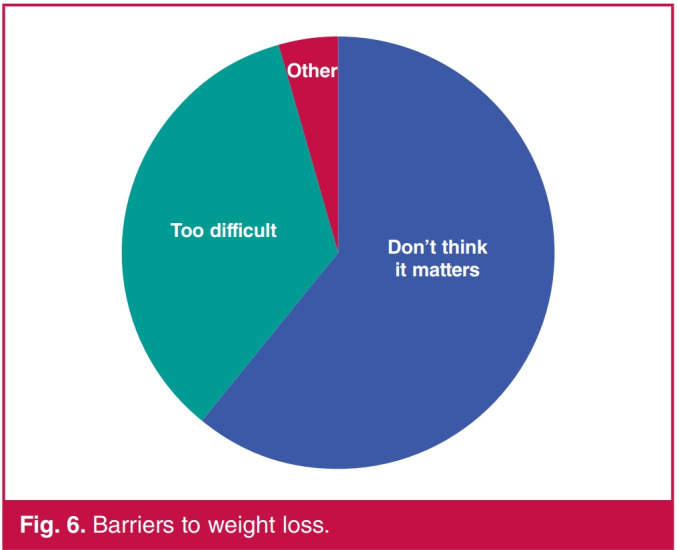
Barriers to weight loss.
Fig. 7.
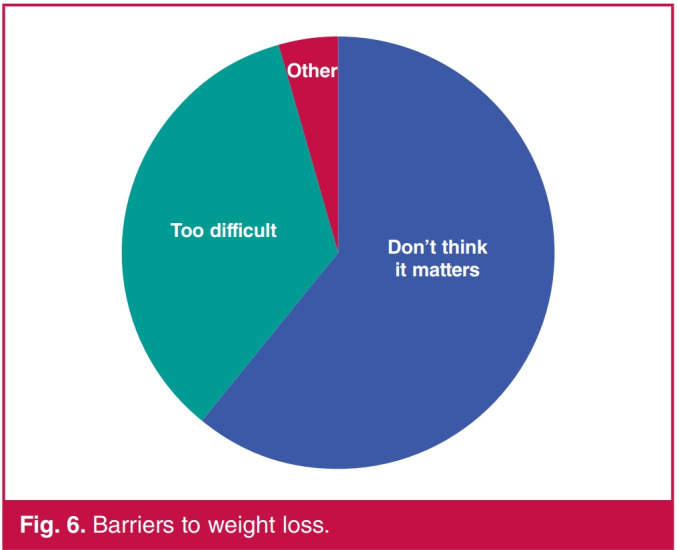
Barriers to exercise.
Fig. 8.
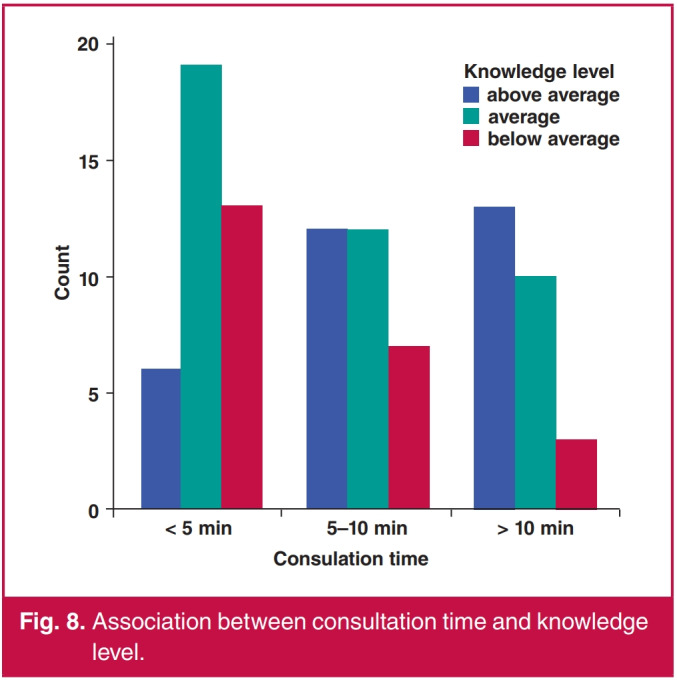
Association between consultation time and knowledge level.
Attitude and practice
Participants were asked questions on their adherence to TLC, and the barriers they perceived were preventing them from implementing such changes if they were not adherent. The respondents were then categorised into different groups of level of implementation based on their responses.
Regarding the five questions asked on implementation of therapeutic lifestyle changes, refraining from alcohol consumption was the lifestyle change most frequently adhered to, with 100% of respondents reporting no alcohol consumption, followed by smoking cessation with 96.4% saying they did not smoke. The lifestyle change respondents were least adherent to was regular exercise, with 59.8% of participants admitting to not exercising on most days (Table 4).
Table 4. Participants’ implementation of TLC.
| TLC | Answer | Number | Percentage |
| Minimising salt intake | Yes | 95 | 84.8 |
| No | 17 | 15.2 | |
| Weight-loss plan | Yes | 87 | 77.7 |
| No | 25 | 22.3 | |
| Regular exercise | Yes | 45 | 40.2 |
| No | 67 | 59.8 | |
| Smoking | Yes | 4 | 3.6 |
| No | 108 | 96.4 | |
| Alcohol consumption | Yes | 0 | 0 |
| No | 100 | 100 |
After categorising participants’ implementation level into ‘poor’, ‘good’ or ‘full implementation’ according to the number of changes adhered to, only 29.5% of respondents were found to be fully implementing TLC, with 25% classified as poor implementation (zero to two changes) and 45.5% classified as good implementation (three or four changes) (Fig. 4).
Concerning patients’ perceived barriers to implementing TLC, their most frequent response to why they were not implementing a certain change was that they did not feel it mattered enough, the same answer being most frequent for each lifestyle change (Table 5, Figs 5–7).
Table 5. Patients’ perceived barriers to TLC implementation.
| TLC | Perceived barrier | Number | Percentage |
| Minimising | Don't think it matters | 14 | 82.4 |
| salt intake | No time | 3 | 17.6 |
| Weight loss | Don't think it matters | 16 | 64 |
| Too difficult | 8 | 32 | |
| Other | 1 | 4 | |
| Regular | Don't think it matters | 27 | 41.5 |
| exercise | No time | 19 | 29.2 |
| No facilities | 6 | 9.2 | |
| Too difficult | 13 | 20 |
Factors affecting knowledge level and TLC implementation
Regarding participants’ level of knowledge on hypertension, males were found to be more knowledgeable than females (p = 0.021), and those with a higher education level also had significantly better knowledge scores than other participants of lower educational status (p = 0.001). Also, patients who reported their consultation time to be more than 10 minutes had greater knowledge levels than those who reported their consultation to have taken less time (Fig. 8). No associations were found between age, marital status, occupation, previous cardiovascular events and knowledge level.
Concerning overall TLC implementation level, sociodemographic factors, previous cardiovascular events, consultation times or even knowledge level did not prove to be associated factors, with no statistically significant differences being recorded between the different groups.
Discussion
Hypertension is a public health issue of utmost importance, as it is a major reversible risk factor for heart attack, renal failure and stroke. Being a reversible risk factor, the priority in medical research endeavours should be finding new and more effective measures to control hypertension and prevent related complications.
Lifestyle modifications are a suitable primary healthcare measure in the control of hypertension and prevention of its sequelae,2 as well as a suitable adjunct to medical therapy. The issue with the implementation of TLC is ensuring patients have both adequate knowledge and motivation to adopt these lifestyles. This cross-sectional, descriptive study conducted in Ahmed Gasim Hospital and Al-Shaab Teaching Hospital in Khartoum state aimed to assess patients’ level of knowledge, attitudes and practice towards hypertension and TLC, and the barriers patients perceived to implementing these changes.
The lifestyle changes participants were questioned on were salt reduction, weight loss, regular exercise, smoking cessation and moderation of alcohol intake. Overall, the results of the study showed that hypertensive subjects possessed a good general knowledge regarding TLC and were implementing these modifications to a certain extent.
The lifestyle change found to be most implemented was abstaining from alcohol; none of the respondents reported any alcohol intake, which is most probably due to the cultural and religious beliefs of the area. This was followed by smoking cessation (96.4%), where cultural background probably played a big role. Most respondents were never smokers in their early years. A high percentage of respondents (84.8%) were actively reducing their salt intake since diagnosis with hypertension, which can only be explained by the fact that patients were actively adopting healthier lifestyles. Exercise was the lifestyle modification least adhered to by hypertensive patients, where 60% admitted to not regularly exercising.
The reason reported most often by participants for not implementing each of the lifestyle modifications was ‘not thinking it matters’ or ‘laziness’, which could be interpreted as patients not being adequately motivated by health givers to adopt healthier lifestyles and not being educated properly on their importance as adjuncts to pharmacological therapy.
Participants were most knowledgeable on the importance of reducing salt intake in managing hypertension (93.8%), which was reflected in their implementation, as it was the lifestyle change most applied that could not be explained by the cultural background of the study area. More than half of the respondents answered incorrectly to whether alcohol consumption affected blood pressure, suggesting the idea that abstaining from alcohol consumption was more of a cultural issue.
A high percentage of participants (71.4%) answered correctly that regular exercise can help lower blood pressure but it was not reflected in their implementation, exercise being the modification least applied. This implies that other than just being given the knowledge of such lifestyle changes, patients need to be motivated adequately by doctors. Further affirming this view is the fact that no association was found between patients’ level of knowledge and their degree of implementation of TLC.
Although duration of consultation was found to be associated with participants’ level of knowledge (p = 0.039), it did not affect their degree of implementation, which may imply that different methods and skills of motivating patients to adhere to lifestyle changes may be needed and not simply spending more time on each consultation.
Perhaps worryingly, no association was found between previous cardiovascular events and patients’ knowledge level, as a previous event would usually stipulate more intense counselling of lifestyle changes. This requires further study, assessing clinicians’ practice in this regard.
Upon reviewing the literature in comparison with the results of this study, the general level of knowledge of participants was found to be comparable to most studies on this topic, one such study conducted on attitudes and practice in Cape Coast in Ghana,7 another one being conducted in South Africa.8 Salt restriction was the most well-known lifestyle change in both, with both populations having good knowledge on hypertension management.
Results from a Canadian national survey in terms of implementation also partially agreed with the results of this study, with the population having a generally high implementation level.9 Salt restriction was the lifestyle change most frequently adhered to. It was also comparable with this study with regard to perceived barriers to implementation, as ‘not wanting to do so’ and ‘not feeling it matters’ were both frequently reported barriers, similar to that reported in this study. This further confirms the idea that patients were not being adequately motivated by health givers.
Of the studies conducted on awareness of patients of hypertension and its associated risk factors, one such study carried out in Khartoum found uncontrolled hypertension to be associated with a lack of awareness towards lifestyle changes and adherence to medication. As far as the researcher’s knowledge is concerned, no other study has been undertaken assessing the knowledge, attitude and practice of hypertensive patients towards TLC specifically.
One of the aspects of this study was to examine whether patients were receiving counselling on lifestyle changes from their doctors and how long they perceived the consultation took. About 85% of participants reported receiving advice on lifestyle change. This proportion is surprisingly high when compared to results reported by a study from Australia,10 where less than 30% of patients recalled ever receiving advice on lifestyle change. This discrepancy might be explained by the difference in study population as our study recruited from speciality cardiology clinics as opposed to primary practice. The same can be assumed for the generally high level of knowledge and degree of implementation demonstrated by participants in this study.
Limitations
The fact that subjects were selected from referral clinics could be considered a limitation of this study. Other limitations are the small sample size of 112 participants, and that the hospitals selected were from Khartoum and Bahri localities only. Hence generalisations cannot be drawn to all of Khartoum state, only to populations with characteristics similar to those of the sample.
Since no standardised tool for assessing knowledge and practice of patients towards lifestyle changes exists, the researcher designed the questionnaire based on the literature and what would be applicable to the study population. Hence the comparison of results between different studies is difficult. Another limitation was that implementation of lifestyle changes was assessed by yes/no questions and no varying degrees of implementation were reported, which may have made the results less accurate.
Conclusion
This study demonstrated that hypertensive patients were generally knowledgeable about hypertension and the importance of TLC in its management, particularly the importance of minimising salt intake. Patients implemented regular exercise least often and gave ‘don’t think it matters’ or ‘laziness’ as their main perceived barrier. Participants gave this reason despite ample knowledge of lifestyle changes and being advised by doctors on these changes. This was deduced since no association was found between patients’ level of knowledge or duration of consultation and their degree of implementation of lifestyle change. The researcher believes that novel approaches are needed to help motivate patients diagnosed with hypertension apply their knowledge regarding TLC.
The author recommends more comprehensive research on this topic to accurately ascertain patients’ perception of TLC as adjuncts to pharmacological therapy. Once patients’ perceived barriers are better understood, novel and more effective approaches to consultation may then be developed and applied.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM. et al. Heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation. 2012;125(1): :e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Status Report on Noncommunicable Diseases: 2010. Geneva: World Health Organization, 2011 [Google Scholar]
- 3.Suliman A. The state of heart disease in Sudan. Cardiovasc J Afr. 2011;22(4):191–196. doi: 10.5830/CVJA-2010-054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babiker FA, Lamia AE, Moukhyer ME. Awareness of hypertension and factors associated with uncontrolled hypertension in Sudanese adults. Cardiovasc J Afr. 2013;24(6):208–212. doi: 10.5830/CVJA-2013-035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darling MS. Non-pharmaceutical management of hypertension among middle-aged and older adults: a literature review. Unpublished thesis submitted to the faculty of the College of Nursing, University of Arizona, 2009 [Google Scholar]
- 6.Moser M. The Clinical Management of Hypertension (8th edn) Professional USA: Communications Inc, 2008. [Google Scholar]
- 7.Anowie F, Darkwa S. Knowledge, attitude and lifestyle practices of hypertensive patients in the Cape-Coast metropolis Ghana. J Sci Res Rep. 2015;8(7):1–15. [Google Scholar]
- 8.Rakumakoe MD. To determine the knowledge, attitudes and perceptions of hypertensive patients towards lifestyle modification in controlling hypertension. 2011:1–61. In partial fulfillment of MSc (Med) in the field of sports medicine. [Google Scholar]
- 9.Gee ME, Bienek A, Campbell NRC, Bancej CM, Robitaille C, Kaczorowski J. et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension. Am J Cardiol. 2012;109(4):570–575. doi: 10.1016/j.amjcard.2011.09.051. [DOI] [PubMed] [Google Scholar]
- 10.Booth AO, Nowson CA. Patient recall of receiving lifestyle advice for overweight and hypertension from their general practitioner. BMC Family Pract. 2010;11:8. doi: 10.1186/1471-2296-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


