Abstract
Background
Postoperative adverse events may be associated with substantial morbidity and mortality. Numerous severity grading systems for these events have been introduced and validated but have not yet been systematically applied in paediatric surgery. This study aimed to analyse the advantages and disadvantages of these classifications in a paediatric cohort.
Methods
Unexpected events associated with interventional or organizational problems in the department of paediatric surgery during 2017–2020 were prospectively documented daily for all children. Events were classified according to the Clavien–Dindo grading system during monthly morbidity and mortality conferences. All events were also classified according to five additional grading systems: T92, contracted Accordion, expanded Accordion, Memorial Sloan Kettering Cancer Center, and Comprehensive Complication Index (CCI)®.
Results
Of 6296 patients, 673 (10.7 per cent) developed adverse events and 240 (35.7 per cent) had multiple events. Overall, 1253 adverse events were identified; of these, 574 (45.2 per cent) were associated with surgical or medical interventions and 679 (54.8 per cent) included organizational problems. The grading systems demonstrated high overall correlation (rpears = 0.9), with minor differences in sentinel events. The Clavien–Dindo classification offered the most detailed assessment. However, these details had only limited additional value. The CCI® scores were correlated with other grading systems (rpears = 0.9) and were useful in analysing multiple events within individual patients.
Conclusion
Grading systems demonstrated similar scoring patterns for minor and sentinel events, with none being superior for unexpected events in children. However, the CCI® can be a major improvement in assessing morbidity in patients with multiple events. Its use is therefore recommended in prospective studies on paediatric surgery.
The authors described the use of different severity grading systems and their advantages and disadvantages in a paediatric cohort. None of the five assessed classification systems were shown to be superior. However, the CCI® can be a major improvement in assessing morbidity in children with multiple events.
Introduction
Postoperative adverse events may be associated with substantial morbidity and mortality1,2. However, inconsistent definitions of complications and unexpected events have limited accurate analysis of surgical outcomes.
In 1992, Clavien et al. introduced a novel approach, named the T92 grading system, to rank complications based on their severity and consequences. Their system differentiated adverse events into three types of negative outcomes: complications; failure to cure; and sequelae3. The strength of this classification was in grading the events based on therapy. The system was acknowledged by numerous surgeons. However, its scientific use has remained limited. Therefore, the T92 grading system was revised in 2004, which resulted in a five-scale classification system according to Clavien–Dindo4. The main improvements in the new system were more detailed grading of life-threatening events and inclusion of long-term disability due to complications.
The Clavien–Dindo classification system has been used in various prospective studies and evolved into the most important grading tool for postoperative adverse events5–7. It has improved postoperative documentation and discussion of adverse events in general surgery, and has been used and modified by trauma, vascular, and urological surgeons8–10.
Other grading systems for the severity of postoperative adverse events have been introduced over time. These mainly include four additional systems. An early modification of the T92 classification system by Martin et al. is commonly referred to as the Memorial Sloan Kettering Cancer Center (MSKCC) classification11. Although these two classifications were similar, the main differences were observed in the numbering of complications. However, numerous studies have used shorter versions of these classifications for simpler documentation of unexpected events. Therefore, in 2009, the then novel Accordion classification of postoperative complications offered an abbreviated and extended version, with focus on its use in clinical studies based on their sample size12. The expansion of grading in the extended version related specifically to severe complications, thus offering a more detailed documentation of sentinel events12.
Whereas the previous grading systems were based solely on the definition and treatment of a single adverse event, the recently formulated Comprehensive Complication Index (CCI®), introduced by a Zurich study group, was demonstrated to be an effective quantification system for postoperative morbidity and highly correlated with the costs of treatment13,14. The CCI® is a metric that includes all recorded complications in an individual. These complications are weighted according to severity based on a prior ranking with the Clavien–Dindo classification in a single formula. Subsequently, the CCI® has been validated in multiple prospective randomized trials, and its use has been suggested to significantly decrease the sample size of studies15–17. Additionally, the CCI® can be applied for cost assessments, independent of the healthcare system14.
Paediatric surgeons have commonly used the Clavien–Dindo classification in retrospective and prospective studies. The authors of this study recently reported the implementation of a daily documentation algorithm for adverse events by use of the Clavien–Dindo classification at a tertiary academic institution for paediatric surgery and emphasized its importance in clinical practice18. Prospective assessment of unexpected events helped to identify organizational shortcomings and develop preventative strategies19. However, other grading systems have not yet been transferred into the specialty of paediatric surgery. The authors believe that knowledge of the advantages and disadvantages of different systems will be of great interest to the surgical community.
The aim of this study was to evaluate the different severity grading systems in routine paediatric surgical practice and to analyse the CCI® as a novel metric for summarizing multiple events in individual patients.
Methods
Ethical approval was obtained from the local ethics committee (approval no 2739–2015), which also approved two protocol amendments (protocol no 8680_BO_K_2019 and 9557_BO_K_2021). Informed consent was obtained from the legal guardians on admission. The study was registered at ClinicalTrials.gov (NCT04827641). The authors followed the STROBE reporting guidelines (see Table S1)20.
Unexpected events in all patients in the study department between 1 January 2017 and 30 November 2020 were documented prospectively. The department of paediatric surgery at the Hannover Medical School is the only tertiary academic institution in the German federal state of Lower-Saxony serving approximately eight million inhabitants. The clinical spectrum of the department includes neonatal, gastrointestinal, hepatobiliary, thoracic, oncological, and paediatric urological surgery. The paediatric surgical team includes seven consultants and seven trainees.
Documentation of unexpected events
Documentation of unexpected events was performed by the designated team members (C.Z. and J.B.) during daily routine team conferences, as described previously18,19. Briefly, the on-call team members and other staff reported any unexpected event that had occurred within the previous 24 hours. After weekends, all events were reported that had occurred during the past 72 hours. One member of the designated team actively asked the participants in the team conferences for any additional minor or major events to be documented during every morning report. Furthermore, all inpatients were discussed three times a week, to complete any missing information. It was therefore expected that all events were documented during the study period. Events included those that had occurred in inpatients and outpatients, and in the paediatric emergency department. Data of each event included patient demographics, diagnoses, treatments/operations, and types of events. The data were stored in a password-encrypted database by the designated team members (C.Z., J.B., and O.M.S.).
After detailed workup, all events were discussed during monthly morbidity and mortality (M&M) conferences, which were attended by all surgical and non-surgical team members and nurses. The events were presented, discussed, and classified by the team according to the Clavien–Dindo classification. Any disagreements regarding the classification of adverse events were discussed during M&M conferences and the result was documented by the moderator from the designated team. A final agreement on the classification of events was obtained for all presented events during the study period. Changes in standard operating procedures (SOPs) were documented during M&M conferences.
Definition of unexpected events
A modified definition of events according to Mazeh et al. was used, as reported previously18,19,21. Based on this definition, the events were stratified as follows: subsequent deviation from the planned pre-, intra-, and postoperative courses; subsequent changes in management with any delay in treatment or recovery; and ongoing disease/disability. Unexpected events associated with surgical and non-surgical treatments were included. Organizational problems, such as miscommunication and postponement of operations because of limited admission, anaesthesia, paediatric surgery, or intensive care facilities, were included, as well as errors concerning the preparation or scheduling of an operation or perioperative diagnostics.
Expected events comprised deviations from the planned interventional approach included on the consent forms (for example, conversion for laparoscopic procedures).
Wound healing disorders were defined based on the criteria by Horan et al.22. Infection of a central line was defined as a catheter-related bloodstream infection (CRBSI) whenever a positive culture of the catheter tip or blood culture specimens or clinical sepsis was present22. Urinary tract infections were defined according to the definition by Horan et al.22. Anastomotic leaks or stenosis following bowel surgery were confirmed using radiographic imaging, endoscopy, or surgical exploration with subsequent dilatation or revision. Error was broadly defined as an act of omission or commission in the planning or execution that contributed to, or had the potential to contribute to, an unintended result23.
For additional events, the authors used a modification of the definitions proposed by Mazeh et al.21, which differentiated the following entities. Bowel dysmotility/adhesion was defined as either hyperperistalsis (for example, diarrhoea) or signs of intestinal obstruction (mechanical or paralytic ileus). Postoperative haematoma or seroma was defined as a collection of blood or fluid in or around a surgical site, confirmed by ultrasound or other imaging. Postoperative bleeding was defined as ongoing haemorrhage from an operation site with or without the need for surgical intervention or transfusion. Catheter leakage was defined as spillage of fluids from a catheter, resulting in repair or removal of the catheter.
Categorization of adverse events
Events associated with surgical and non-surgical interventions and events not associated with interventions, such as organizational problems, management problems, or underlying disease, were differentiated. Organizational and management problems were prospectively assessed and graded as minor events (grade I) if the patients did not experience any impact on their health status.
Classification of adverse events
The severity of adverse events was finally classified prospectively according to the Clavien–Dindo classification (grades I–V) by the team during M&M conferences4. These were divided into minor non-life-threatening events (grades I–IIIb) and sentinel events resulting in serious physical or psychological injury or death (grades IV–V) by use of the modification by Rodziewicz et al.24.
All events that had been classified according to the Clavien–Dindo system were reclassified by designated team members (J.B. and O.M.S.) according to the additional four grading systems (Table S2). Briefly, the T92 system includes four grades (grades I–IV) and five levels of complications3. The MSKCC classification was the first attempt to modify the T92 system and includes five grades (grades I–V) for severity of adverse events11,25,26. The contracted Accordion classification for assessment of the severity of complications includes four grades (grades I–IV)12. The extended version of the Accordion classification includes six grades (grades I–VI)12. Strasberg et al.12 recommend the application of the extended classification in large studies with a focus on complex procedures, for example oesophageal and pancreatic resection, because of the risk of severe complications. The expansion of grading occurs exclusively in areas with severe complications.
Additionally, the study assessed the CCI® score for all patients. The CCI® score is a validated metric for grading postoperative morbidity on a scale of zero (no complication) to 100 (death)14,17. The CCI® score is based on prior ranking by the Clavien–Dindo system and includes multiple adverse events in a single patient. The CCI® score was calculated using the template available at http://www.cci.assessurgery.com, as previously reported by Staiger et al.14 CCI® score assessment can be performed in all patients (including from preterm to 17 years of age) with a single unexpected event, including single minor events during the perioperative period (for example, one grade I event correlates with a CCI® score of 8.7) (see Table S3 and Figure S1). For calculation of the CCI® score, the authors included all events in an individual within the follow-up period of 90 days (3 months) following an intervention. For events appearing later than 90 days after the intervention, a new case identification number was created and a new/additional CCI® score was calculated. Therefore, the analysis could include multiple CCI® scores in single individuals within the study period.
Differentiating items
The severity grading systems were analysed in terms of differentiation of items. Eight criteria for severity assessment of adverse events were identified, including unforeseen drug administration, differentiation between oral and intravenous drug administration, bedside procedures, use of antibiotics, blood transfusion and/or parenteral nutrition, procedures performed under general anaesthesia, endoscopic or radiological interventions, differentiation between single- and multiorgan failure, and standalone grading for death. The scoring systems were reviewed for differentiation of these items.
Follow-up data
Data of patients who were readmitted or seen in the outpatient clinic because of adverse events were included. All available data from follow-up were reviewed by the designated team members (C.Z., J.B., and O.M.S.) and used to assess the five systems.
Statistical analysis
Statistical analysis was performed using GraphPad Prism (v8.0; GraphPad Software, San Diego, California, USA). Pearson’s correlation coefficient was used (rpears) to compare the Clavien–Dindo classification with T92, the contracted and extended Accordion, and MSKCC’s Surgical Secondary Events Grading systems; rpears > 0.8 was defined as strong, and rpears > 0.9 as very strong. Data are presented as mean(s.d.). Statistical significance was set at P < 0.050.
Results
Of the 6296 patients who were treated during the study period, 673 patients (10.7 per cent) experienced adverse events. A total of 1253 adverse events were identified; 433 (64.3 per cent), 127 (18.9 per cent), and 113 (16.8 per cent) had one, two, and more than two events respectively. The mean age of the cohort at the time of the adverse event was 76.5(4.3) months.
Patient age at time of adverse events
A total of 421 events (33.6 per cent) occurred in children aged under 1 year, and 220 events (17.6 per cent) in toddlers aged 1–3 years. A total of 133 (10.6 per cent) of the events occurred in children aged 3–5 years, 194 events (15.5 per cent) in those aged 5–12 years, and 285 events (22.7 per cent) in those aged 12–18 years.
Events related to surgical subspecialties
In stratifying the number of events to paediatric surgical subspecialties, 100 events (8.0 per cent) were registered in neonatal surgery, 201 events (16.0 per cent) in gastrointestinal surgery, 46 events (3.7 per cent) in hepatobiliary surgery, 65 events in thoracic surgery (5.2 per cent), 78 events (6.2 per cent) in oncological surgery, and 262 events (20.9 per cent) in paediatric urology. A total of 501 events (40 per cent) were related additional procedures, not associated with the subspecialties.
Categorization of adverse events
A total of 574 (45.2 per cent) adverse events were associated with surgical and non-surgical interventions, whereas 679 (54.8 per cent) events were associated with organizational and management problems. Of the 574 intervention-associated events, 485 (84.4 per cent) were managed by surgical and non-surgical interventions, whereas the remaining 89 (25.6 per cent) were managed conservatively using bedside procedures and medicines (antibiotics, parenteral nutrition, blood transfusion). A total of 386 (79.6 per cent) patients required an intervention under general anaesthesia, whereas 99 (20.4 per cent) patients were managed by an intervention without general anaesthesia or under local anaesthesia. Of those 99 patients, 80 (80.8 per cent) had more than one event and 51 (51.5 per cent) underwent at least one additional procedure under general anaesthesia. Of the 386 patients who underwent procedures under general anaesthesia, 343 (88.9 per cent) underwent surgical reinterventions, whereas 43 (11.1 per cent) underwent radiological or endoscopic interventions under general anaesthesia.
Comparison of classifications of adverse events
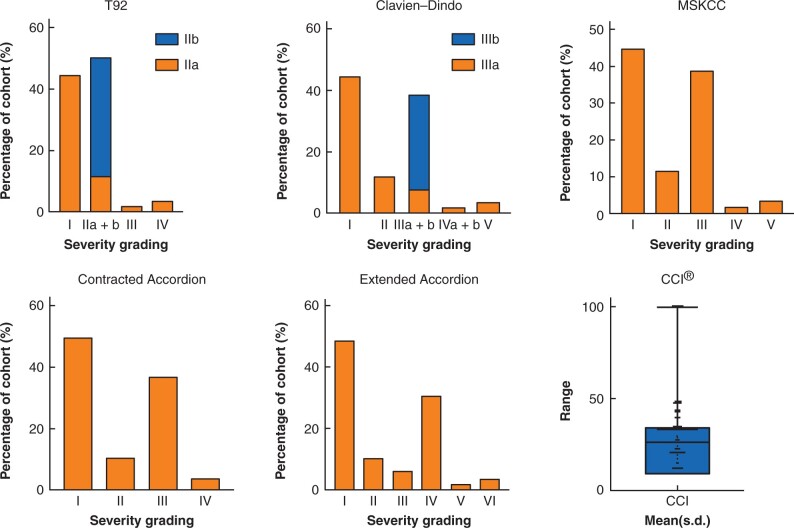
Results of classification of 1253 adverse events using the five systems are presented in Fig. 1. Differences were mainly observed with minor events (grades I–III or I–IV) (see Table S4), including different gradings of drug groups (antibiotics) and procedures (chest tube, urinary catheter insertion). The median score was 2 in all grading systems, with similar patterns, despite differences in scale and numbering of events in the classification systems (see Table S5). According to all severity grading systems, minor events were identified in 94.9 to 96.5 per cent and major/sentinel events in 3.5 to 5.1 per cent of events. Fig. 1 illustrates similar patterns in all classifications, except the contracted Accordion system. Stratification of grades revealed grade I events in 44.4 to 49.4 per cent of patients. Grade II events were documented in 10.1 to 11.8 per cent of patients with use of four of the grading systems. However, according to the T92 classification, grade II events were subclassified; grade IIa events were observed in 11.8 per cent and grade IIb events in 38.7 per cent of patients. Grade IIb in the T92 classification system corresponds to grade III in the MSKCC classification system (38.7 per cent), the sum of grades IIIa (7.9 per cent) and IIIb (30.8 per cent) in the Clavien–Dindo classification system, and grades III (5.9 per cent) and IV (30.4 per cent) in the extended Accordion classification system. The contracted Accordion classification system demonstrated different distribution patterns, beginning from grade III, because of summarization of events in one grade—ranging from endoscopic/radiological/surgical interventions to multiorgan failure—and consequently including both minor and major events.
Fig. 1.
Assessment of five severity grading systems stratified in terms of grading, and a box plot for the CCI®, with visualization of the mean(s.d.) for 1253 adverse events and 771 CCI® scores in 673 patients; CCI®, Comprehensive Complication Index.
Correlation between the Clavien–Dindo classification and the grades of four other systems
A strong correlation was identified between the Clavien–Dindo classification system and the T92 (rpears = 0.95, P < 0.0001), contracted and extended Accordion (rpears = 0.94, P < 0.0001 and rpears = 0.96, P < 0.0001 respectively), and MSKCC classification systems (rpears = 0.99, P < 0.0001) (Table 1 and Figure S2). These results were also observed after stratification of all classifications into minor events (rpears ≥ 0.9, P < 0.0001) and major/sentinel events (rpears ≥ 0.9, P < 0.0001).
Table 1.
Correlation between the Clavien–Dindo grade and scores of T92, contracted Accordion, extended Accordion, and MSKCC for 1253 adverse events in 673 patients
| Clavien–Dindo classification versus |
||||
|---|---|---|---|---|
| T92 | Contracted Accordion | Extended Accordion | MSKCC | |
| r pears | 0.95 | 0.94 | 0.96 | 0.99 |
| 95 per cent c.i. | (0.94,0.95) | (0.93,0.95) | (0.95,0.96) | (0.98,0.99) |
| R-squared | 0.9 | 0.9 | 0.92 | 0.97 |
| P | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 |
MSKCC, Memorial Sloan Kettering Cancer Center; rpears, Pearson’s correlation coefficient.
The comprehensive complication index (CCI®)
A total of 771 CCI® scores were calculated, with 1253 adverse events detected (Fig. 1). A CCI® score of 8.7–33.6 was identified in 408 (52.9 per cent) patients, 33.7–46.1 in 297 (38.5 per cent) patients, and more than 46.2 in 66 (8.6 per cent) patients. Scores higher than 46.2 (n = 66) included 43 infants with grade V Clavien–Dindo event (death) that corresponded to CCI® of 100. Two children had CCI® > 80. Both had been hospitalised for several months. One had a history of inflammatory bowel disease and was admitted because of a toxic megacolon for various surgical and endoscopic procedures, long-term antibiotics, immunosuppressive treatment, and parenteral nutrition resulting in 20 events during the in-hospital stay and the follow-up period. The other was an infant with cardiac necrotizing enterocolitis who underwent multiple surgical procedures and encountered life-threatening electrolyte fluctuations and central line infections.
Correlation between the comprehensive complication index (CCI®) scores and Clavien–Dindo scores
Of 673 patients, 240 (35.7 per cent) had more than one event. The study aimed to investigate whether CCI® scores provided information on the severity of the events in the cohort or whether accumulation of multiple minor (non-life-threatening) events in a single patient distorted the analysis. The authors found that CCI® scores correlated with the Clavien–Dindo grades in patients with one event and with the highest Clavien–Dindo score in patients with multiple events. A very strong correlation (rpears = 0.9, P < 0.0001) was detected, indicating high sensitivity of the CCI® score to distinguish between minor and major events in patients (Fig. 2).
Fig. 2.
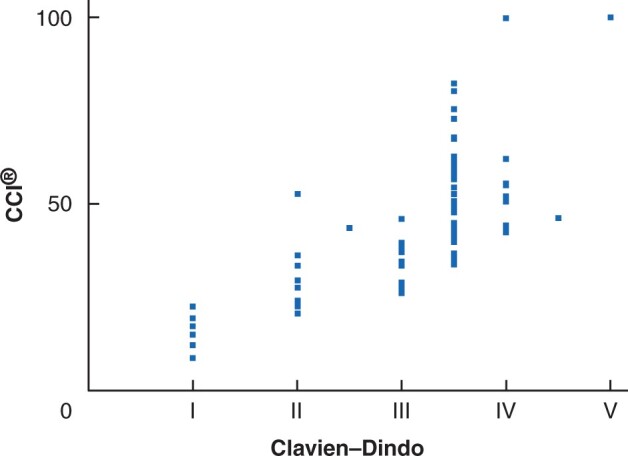
Correlation between the highest Clavien–Dindo grade in 673 patients with multiple adverse events and 771 CCI® scores for a total of 1253 adverse events. CCI®, Comprehensive Complication Index.
Items for severity grading of adverse events
The Clavien–Dindo classification system included seven out of the eight criteria for severity assessment of adverse events (87.5 per cent), whereas the extended Accordion and MSKCC systems included five criteria each (62.5 per cent) and the T92 and contracted Accordion systems included two criteria each (25 per cent) (Table 2).
Table 2.
Differentiating items according to severity grading scores
| Items | Clavien– Dindo | T92 | Contracted Accordion | Extended Accordion | MSKCC |
|---|---|---|---|---|---|
| Identification of unforeseen drug administration | × | × | × | × | × |
| Differentiation between oral and intravenous administration of drugs | − | − | − | − | × |
| Differentiation of bedside procedures from invasive procedures ± general anaesthesia | × | − | × | × | × |
| Identification of antibiotics, blood transfusions, and parenteral nutrition | × | − | − | × | × |
| Differentiation between procedures performed without and with general anaesthesia | × | − | − | × | − |
| Differentiation of endoscopic or radiological interventions without and with general anaesthesia | × | − | − | − | − |
| Differentiation between single- and multiorgan failure | × | − | − | − | − |
| Standalone grade for death | × | × | × | × | × |
MSKCC, Memorial Sloan Kettering Cancer Center. x = item included in the severity grading systems; – = item not included in the severity grading system.
Changes in standard operating procedures during the study period
During the study period, 39 M&M meetings were held. A total of 64 changes to the SOPs were documented, 44 (68.8 per cent) of which were associated with events following surgical and non-surgical interventions. Those SOP changes included standardized instructions for diagnostic algorithms and therapeutic interventions. The remaining 20 SOP changes (31.2 per cent) were associated with organizational and management problems. To implement these SOP changes, system quality improvement infrastructures with an in-house risk management team were available.
Discussion
The present study confirmed that all grading systems demonstrated identical median values despite differences in scale and numbering of adverse events. This can be explained by the high number of non-life-threatening events in the study cohort. All the investigated grading systems, except the contracted Accordion classification system, offer a standalone grade for invasive procedures. However, only the Clavien–Dindo classification system differentiates procedures performed without (grade IIIa) and those performed with general anaesthesia (grade IIIb).
In the study cohort, 80 per cent of interventions were performed under general anaesthesia (grade IIIb). A detailed review of the remaining 20 per cent of interventions (grade IIIa) revealed that a majority of procedures were performed under sedation with anaesthetic support and post-interventional monitoring in the recovery room. Furthermore, a third of patients with grade IIIa complications, according to the Clavien–Dindo classification, had already been managed in a paediatric ICU. Of 99 patients with grade IIIa complications, 81 per cent had more than one unexpected event and 52 per cent had at least one additional event of grade IIIb or higher. Therefore, Clavien–Dindo grade IIIa had only limited additional value to the study cohort. It is worth mentioning that, in contrast to adults, minor procedures in children, including wound revisions and change of vacuum dressings, are usually performed under general anaesthesia. A notable feature of the Clavien–Dindo differentiation concerning anaesthesia may also be concluded from the multicentre APRICOT study27, in which the incidence of critical events under general anaesthesia in children was significantly higher than that under sedation; however, the all-cause in-hospital mortality was independent of the type of anaesthesia. Other studies have confirmed the intensive peri-interventional management of children, resulting in improved safety with procedural sedation, which may indicate that differentiation between general and local anaesthesia in children may be unnecessary28–30.
All grading systems, except the contracted Accordion classification, include a standalone grade for sentinel events, organ failure, and organ loss. The Clavien–Dindo classification system remains the only system to differentiate between single-organ and multiorgan dysfunction. However, in this series, grade IVb (multiorgan failure) complication was observed in only one patient. Again, Clavien–Dindo grade IVb had only limited additional value to the study cohort. Additional analysis of the sentinel events demonstrated that they mainly occurred in the group of neonatal surgery with children aged less than 1 year, including 14 grade IV events (14 of 21; 66.7 per cent) and 37 grade V (death) events (37 of 43; 86.0 per cent).
Severity grading systems focus on single complications that occur during the perioperative period. They do not include information on complications during follow-up and multiple complications in a single patient. This gap may be filled by the CCI®, which was introduced as a metric of postoperative morbidity, including all complications in individual patients in a single formula14.
The authors calculated 771 CCI® scores and identified individual patients with up to 20 events during the in-hospital stay and follow-up period of 3 months. The CCI® scores adequately weighted the sentinel events, compared with minor non-life-threatening events. After excluding the CCI® score of 100 (death), only two patients had scores above 80. Both patients were hospitalized for several months and experienced repeated life-threatening events. To understand the weighting of major and minor events in the metric, the authors correlated the CCI® scores with the highest Clavien–Dindo grades in individual patients, which demonstrated high correlation (r pears= 0.9). Children with multiple non-life-threatening events still had lower scores, compared with those with a sentinel event. Sentinel events may be associated with additional complications, longer duration of hospital stay, and longer follow-up periods. Therefore, the CCI® may be a better routine grading system in individual patients with multiple complications.
The CCI® is not intended to replace the Clavien–Dindo classification, as they both work in close concert13,14. The focus of the Clavien–Dindo classification and its ordinal scale is to offer a simple and practicable tool in the clinical routine, especially for the presentation of single events in M&M conferences13,14. In contrast, the CCI®, with its longitudinal assessment of multiple complications, is valuable in interpreting overall morbidity and therefore might be better to evaluate perioperative care. Therefore, those who developed the CCI® strongly recommend the use of both classification systems for clinical and scientific purposes13,14.
In this study, analysis of the CCI® focused on postoperative morbidity only. However, it has also been demonstrated that the CCI® is also a reliable predictor of costs of surgical care14. This investigation has not yet been applied to a paediatric cohort but could highlight an additional benefit of incorporating the CCI® into future studies.
This present study has some limitations. While the Clavien–Dindo classification was used prospectively, additional grading systems were documented retrospectively. The authors aimed to reduce the bias by having a designated team responsible for collecting all data and grades. Furthermore, the profile of procedures in the study cohort was heterogeneous and included abdominal, hepatobiliary, thoracic, urogenital, and numerous other types of operations. However, the study focused on events, rather than on a comparative analysis of groups of procedures.
The systems used in this study demonstrated high correlation in the grading of postoperative events. None of the grading systems were superior to others in documenting unexpected events. Based on the authors’ previous experience, the Clavien–Dindo classification is a simple tool for assessment of single events and is used routinely in M&M meetings at their institution19. Furthermore, the Clavien–Dindo classification can be used for CCI® score calculations, which may be an adequate and valuable metric for documentation of multiple events in individual patients and is now included in the authors’ institutional protocol.
Funding
The study was funded by the general budget of the departments involved.
Disclosure. The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Supplementary Material
References
- 1. Tevis ES, Cobian AG, Truong HP, Craven MW, Kennedy GD.. Implications of multiple complications on the postoperative recovery of general surgery patients. Ann Surg 2016;263:1213–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ; participants in the VA National Surgical Quality Improvement Program. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:326–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clavien PA, Sanabria JR, Strasberg SM.. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992;111:518–526. [PubMed] [Google Scholar]
- 4. Dindo D, Demartines N, Clavien PA.. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D. et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg 2013;258:37–45. [DOI] [PubMed] [Google Scholar]
- 6. Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A. et al. Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 2017;265:284–290. [DOI] [PubMed] [Google Scholar]
- 7. Maggiori L, Rullier E, Lefevre JH, Régimbeau JM, Berdah S, Karoui M. et al. Does a combination of laparoscopic approach and full fast track multimodal management decrease postoperative morbidity? A multicenter randomized controlled trial. Ann Surg 2017;266:729–737. [DOI] [PubMed] [Google Scholar]
- 8. Mitropoulos D, Artibani W, Biyani CS, Jensen JB, Roupret M, Truss M.. Validation of the Clavien–Dindo grading system in urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus 2018;4:608–613. [DOI] [PubMed] [Google Scholar]
- 9. Inaraja-Pérez GC, Júlvez-Blancas M.. Usefulness of the Clavien–Dindo classification to rate complications after carotid endarterectomy and its implications in patient prognosis. Ann Vasc Surg 2019;55:232–238. [DOI] [PubMed] [Google Scholar]
- 10. Naumann DN, Vincent LE, Pearson N, Beaven A, Smith IM, Smith K. et al. An adapted Clavien–Dindo scoring system in trauma as a clinically meaningful non-mortality endpoint. J Trauma Acute Care Surg 2017;83:241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martin RCG, Brennan MF, Jaques DP.. Quality of complication reporting in the surgical literature. Ann Surg 2002;235:803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Strasberg SM, Linehan DC, Hawkins WG.. The accordion severity grading system of surgical complications. Ann Surg 2009;250:177–186. [DOI] [PubMed] [Google Scholar]
- 13. Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA.. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 2013;258:1–7. [DOI] [PubMed] [Google Scholar]
- 14. Staiger RD, Cimino M, Javed A, Biondo S, Fondevila C, Périnel J. et al. The Comprehensive Complication Index (CCI®) is a novel cost assessment tool for surgical procedures. Ann Surg 2018;268:784–791. [DOI] [PubMed] [Google Scholar]
- 15. Linecker M, Botea F, Raptis DA, Nicolaescu D, Limani P, Alikhanov R. et al. Perioperative omega-3 fatty acids fail to confer protection in liver surgery: results of a multicentric, double-blind, randomized controlled trial. J Hepatol 2020;72:498–505. [DOI] [PubMed] [Google Scholar]
- 16. Poves I, Burdio F, Morató O, Iglesias M, Radosevic A, Ilzarbe L. et al. Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg 2018;268:731–739. [DOI] [PubMed] [Google Scholar]
- 17. Slankamenac K, Nederlof N, Pessaux P, de Jonge J, Wijnhoven BPL, Breitenstein S. et al. The comprehensive complication index: a novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann Surg 2014;260:757–762. [DOI] [PubMed] [Google Scholar]
- 18. Sethi MVA, Zimmer J, Ure BM, Lacher M.. Prospective assessment of complications on a daily basis is essential to determine morbidity and mortality in routine pediatric surgery. J Pediatr Surg 2016;51:630–633. [DOI] [PubMed] [Google Scholar]
- 19. Zoeller C, Kuebler JF, Ure BM, Brendel J.. Incidence of complications, organizational problems, and errors: unexpected events in 1605 patients. J Pediatr Surg 2021;56:1723–1727. [DOI] [PubMed] [Google Scholar]
- 20. Von Elm E, , AltmanDG, , EggerM, , PocockSJ, , GøtzschePC, , Vandenbroucke JP.. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mazeh H, Cohen O, Mizrahi I, Hamburger T, Stojadinovic A, Abu-Wasel B. et al. Prospective validation of a surgical complications grading system in a cohort of 2114 patients. J Surg Res 2014;188:30–36. [DOI] [PubMed] [Google Scholar]
- 22. Horan TC, Andrus M, Dudeck MA.. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–332. [DOI] [PubMed] [Google Scholar]
- 23. Grober ED, Bohnen JMA.. Defining medical error. Can J Surg 2005;48:39–44. [PMC free article] [PubMed] [Google Scholar]
- 24. Rodziewicz TL, Houseman B, Hipskind JE.. Medical Error Reduction and Prevention . In: StatPearls. Treasure Island: StatPearls Publishing, 2021. https://www.ncbi.nlm.nih.gov/books/NBK499956/. [PubMed] [Google Scholar]
- 25. Kooby DA, Fong Y, Suriawinata A, Gonen M, Allen PJ, Klimstra DS. et al. Impact of steatosis on perioperative outcome following hepatic resection. J Gastrointest Surg 2003;7:1034–1044. [DOI] [PubMed] [Google Scholar]
- 26. Strong VE, Selby LV, Sovel M, Disa JJ, Hoskins W, Dematteo R. et al. Development and assessment of Memorial Sloan Kettering Cancer Center’s Surgical Secondary Events grading system. Ann Surg Oncol 2015;22:1061–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Habre W, Disma N, Virag K, Becke K, Hansen TG, Jöhr M. et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Resp Med 2017;5:412–425. [DOI] [PubMed] [Google Scholar]
- 28. Grunwell JR, McCracken C, Fortenberyy J, Stockwell J, Kamat P.. Risk factors leading to failed procedural sedation in children outside the operating room. Pediatr Emerg Care 2014;30:381–387. [DOI] [PubMed] [Google Scholar]
- 29. Grunwell JR, Travers C, McCracken CE, Scherrer PD, Stormorken AG, Chumpitazi CE. et al. Procedural sedation outside of the operating room using ketamine in 22,645 children: a report from the pediatric sedation research consortium. Pediatr Crit Care Med 2016;17:1109–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee JR, Lee JH, Lee HM, Kim N, Kim MH.. Independent risk factors for adverse events associated with propofol-based pediatric sedation performed by anesthesiologists in the radiology suite: a prospective observational study. Eur J Pediatr 2021;180:1413–1422. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.