Abstract
Background
Concerns about the safety of silicone breast implants (SBIs) have existed for years, but a causal relation between systemic complaints and SBIs has not been proven. Nevertheless, some women are worried and even request explantation.
Objectives
This study aimed to review the explantation procedures performed, focusing on patient-reported symptoms preoperatively, the effect of explantation, and the effect of breast reconstruction on these symptoms.
Methods
A retrospective chart review was performed for patients who had undergone explantation between 2010 and 2020 at Maastricht University Medical Center. Patients who had undergone tissue expander removal, tissue expander–implant exchange, or direct implant exchange were excluded.
Results
More than half of the patients undergoing explantation reported complaints, mostly pain. Some 15% reported systemic complaints they believed were implant related. Breast implant illness (BII) was found to be the fifth most common indication for explantation (11.2%). A history of either allergies or implant rupture resulted in higher odds ratios of having BII (odd ratios, 2.1 and 2.1, respectively). Subjective improvement of BII after explantation was reported by about 60% of patients.
Conclusions
A relatively low prevalence of suggested BII exists among women undergoing explantation; 1 in 9 procedures were performed for this reason. Allergy and implant rupture may increase the likelihood of having BII. About 60% of BII patients experienced an improvement in their complaints after implant removal. Autologous breast reconstruction appears a good alternative. Prospective studies into health complaints and quality of life should be performed to confirm the effectiveness of explantation as a therapy for BII.
Level of Evidence: 4
Following their introduction in the 1960s, millions of women received silicone breast implants (SBIs) for cosmetic breast augmentation or breast reconstruction. The procedure is associated with risks of both aesthetic and clinical sequelae, such as malposition, capsular contracture, and pain.1 Concerns have continued to grow about the impact of silicone particles potentially migrating through the body, and the development of systemic symptoms, which the literature refers to as breast implant illness (BII).2 Although the majority of women appear content with their implants, some report a pattern of systemic health complaints of varying severity, such as myalgia, arthralgia, fever, fatigue, dry eyes and mouth, and cognitive impairments.3,4 However, the current literature has found insufficient evidence to associate these symptoms with SBIs.5,6
Despite the lack of evidence of an association between complaints and SBIs, some women are worried and request that their implants be removed. The few studies that have examined this population have shown subjective improvement in patient-reported complaints after SBI explantation.7-9 Indeed, a recent literature review has calculated that 75% of patients with silicone-related complaints experienced at least temporary relief of their symptoms once their implants were removed.10
Many studies have been conducted into the longevity and local complications of breast implants, predominantly infection, capsular contracture, and implant rupture.1,11,12 However, little attention has been paid to those systemic complaints that precede explantation and the postoperative course of these complaints. Another underinvestigated topic is the effect of reconstruction after explantation in patients with self-reported complaints. Therefore, the aim of this study was to review all explantation procedures where no implant was replaced that had been performed in our center during the last 10 years; the specific focus was on examining patient-reported symptoms preoperatively, the effect of explantation, and the effect of breast reconstruction on these symptoms.
METHODS
Patient Selection
A retrospective chart review was performed for patients who had undergone explantation of their breast implants between January 2010 and April 2020. Patients included were women of all ages, with silicone- or saline-filled breast implants for both cosmetic and reconstructive reasons, who had had their implants removed for any reason at Maastricht University Medical Center. The implants could have been inserted at other clinics. Patients excluded were those who had undergone tissue expander removal, tissue expander–implant exchange, and direct implant exchange.
Data Abstraction
A standardized abstraction form was used to extract the following information from the electronic medical records: demographic data (age, body mass index [BMI], smoking status, allergies, medical history, and cancer therapy), implant details (material, manufacturer, and volume), clinical data (clinical symptoms and reason for explantation), surgery dates, implant rupture, and breast reconstruction after explantation. Systemic symptoms, other than local pain, that women felt were connected to their breast implants were referred to as “suggested breast implant illness.”
Data Analysis
Data were analyzed with descriptive statistics. Characteristics of implants and prevalence of symptoms were reported as counts and percentages. Continuous variables were represented as mean [standard deviation] and range. An independent-samples t test was performed to compare means between subgroups. Differences in percentages between groups were tested with Pearson’s chi-square test or Fisher’s exact test. Multivariable logistic regression was performed to identify factors associated with the occurrence of BII, adjusted for potential confounding factors. Results were quantified as odds ratios with 95% confidence intervals. All analyses were performed in IBM SPSS Statistics version 25 with an α level of 0.05 determining significance.
This study was approved by the Ethics Committee at the Maastricht University Medical Center. Patient consent was not required.
RESULTS
Patient and Implant Characteristics
One hundred and ninety-seven patients underwent an explantation procedure during this 10-year period. Their mean age was 52.0 years (range, 24-81 years) and their mean BMI was 25.1 kg/m2 (range, 17.3-44.6 kg/m2). Patient and implant characteristics are presented in Table 1. In total, 303 breast implants from 10 manufacturers were removed. Ninety procedures (45.7%) were unilateral, whereas in the other 107 cases (54.3%) implants were removed bilaterally. The average time from implant placement to explantation was 102.8 months (range, 0-586 months), and the total exposure to implants averaged 130.4 months (range, 0-586 months).
Table 1.
Patient and Implant Characteristics
| Total patients (n) | 197 |
| Total implants removed (n) | 303 |
| Age (years) | 52.0 [12.1] (24-81) |
| BMI (kg/m2) | 25.1 [4.7] (17.3-44.6) |
| Smoker | 51 (25.9) |
| Allergies | 81 (41.1) |
| Implant reason | |
| Cosmetic | 67 (34.0) |
| Reconstruction | 130 (66.0) |
| Implant type | |
| Silicone filled | 172 (87.3) |
| Saline filled | 13 (6.6) |
| Unknown | 12 (6.3) |
| Implant manufacturer | |
| Eurosilicone (GC Aesthetics, Dublin, Ireland) | 91 (30.0) |
| Allergan (Irvine, CA) | 42 (13.9) |
| McGhan (Allergan) | 29 (9.6) |
| Mentor (Irvine, CA) | 18 (5.9) |
| Polytech (Dieburg, Germany) | 9 (3.0) |
| Arion (Mougins, France) | 7 (2.3) |
| CUI (Santa Barbara, CA) | 3 (1.0) |
| Silimed (Rio de Janeiro, Brazil) | 2 (0.7) |
| Rofil (Breda, the Netherlands) | 2 (0.7) |
| Inamed (Santa Barbara, CA) | 2 (0.7) |
| Unknown | 98 (32.3) |
| Implant volume (cc) | 372 [144.3] (100-850) |
BMI, body mass index. Values are n (%) or mean [standard deviation] (range) unless otherwise stated.
Indications for Explantation
The primary indications for explantation included: severe capsular contracture (14.7%); implant rupture (14.2%); pain in the absence of implant rupture or evident capsular contracture (13.2%); infection without exposure of the implant (13.2%); suggested implant-related systemic symptoms/BII (11.2%); unsatisfactory aesthetic result/asymmetry (9.1%); exposure of the breast implant as a result of infection or wound dehiscence (8.1%); breast cancer or prophylactic breast surgery (8.1%); seeking autologous breast reconstruction with no specific cause reported (4.6%); extensive concern about the safety of silicone exposure (1.0%); other reasons (2.5%).
Self-Reported Complaints
Fifty-two percent of the women who underwent explantation reported complaints that they attributed to their implants. The most common complaint was local pain, which was present in 40.6% of all cases.
Twenty-nine patients (14.7%) reported suggested BII. They experienced 1 or more systemic complaints, other than pain, that they attributed to the breast implants. The most commonly reported self-reported complaints were fatigue, arthralgia, and myalgia (Table 2). All women with suggested BII had SBIs. In the medical history of these women, a high rate of psychological and functional comorbidities was found (see Supplemental Table 1, available online at www.aestheticsurgeryjournal.com, for an overview of these 29 BII patients, their medical history, and their implant-related complaints). Women with BII were not significantly younger (mean age, 50.6 years; range, 29-68 years) than women without BII (mean age, 52.3 years; range, 24-81 years), nor did they have a significantly higher BMI (mean, 25.4 kg/m2; range, 17.7-39.7 kg/m2) than women without BII (mean, 25.1 kg/m2; range, 17.3-44.6 kg/m2). Neither the in situ duration of the removed implant nor the total duration of implant exposure was significantly different between the 2 groups. BII patients did report allergies more often and their removed implants were more often found to be ruptured. A comparison of the characteristics of women with and without BII is presented in Table 3.
Table 2.
Self-Reported Complaints in Women With Suggested Breast Implant Illness
| Complaint | N (%) |
|---|---|
| Fatigue | 18 (62.1) |
| Arthralgia | 15 (51.7) |
| Myalgia | 10 (34.5) |
| Sicca | 6 (20.7) |
| Skin problems/itch/rash | 4 (13.8) |
| Cognitive impairment | 5 (17.2) |
| Pyrexia/hyperhidrosis | 5 (17.2) |
| Headaches | 4 (13.8) |
| Neurologic deficit | 3 (10.3) |
| Immune diseases | 3 (10.3) |
| Hair loss | 2 (6.9) |
| Vertigo | 2 (6.0) |
| Others | 7 (24.1) |
Table 3.
Comparison of Characteristics of Women With and Without BII
| Characteristic | BII | No BII | P value |
|---|---|---|---|
| Total patients | 29 (14.7) | 168 (85.3) | — |
| Total implants removed | 51 (16.8) | 252 (83.2) | — |
| Age (years) | 50.6 [12.3] | 52.3 [11.1] | 0.475 |
| BMI (kg/m2) | 25.4 [4.7] | 25.1 [4.7] | 0.768 |
| Smoker | 7 (24.1) | 44 (27.3) | 0.721 |
| Allergies | 17 (58.6) | 64 (38.3) | 0.040 |
| Breast cancer therapy | |||
| Radiation therapy | 5 (17.2) | 41 (25.6) | 0.333 |
| Chemotherapy | 6 (27.3) | 60 (39.5) | 0.069 |
| Hormone therapy | 1 (3.6) | 41 (27.0) | 0.007 |
| Immunotherapy | 2 (7.1) | 9 (5.9) | 0.682 |
| Implant reason | |||
| Cosmetic | 13 (44.8) | 54 (32.1) | 0.183 |
| Reconstruction | 16 (55.2) | 114 (67.9) | |
| Implant type | |||
| Silicone filled | 29 (100.0) | 141 (91.6) | 0.226 |
| Saline filled | 0 (0.0) | 13 (8.3) | |
| Previous implant exchange | 10 (34.5) | 42 (25.0) | 0.537 |
| Implant rupture | 11 (40.7) | 34 (20.7) | 0.023 |
| Time implant in situ (months) | 101.0 [58.6] | 102.8 [103.8] | 0.875 |
| Total exposure to implants (months) | 146.5 [109.0] | 127.5 [127.0] | 0.450 |
| Total exposure to implants (months) | 146.5 [109.0] | 127.5 [127.0] | 0.450 |
Values are n (%) or mean [standard deviation]. BII, breast implant illness.
Multivariable logistic regression that included age, allergies, radiotherapy, chemotherapy, hormone therapy, and implant rupture as independent variables showed that none of these variables were significant independent susceptibility factors for BII, although some odds ratios may indicate potential clinical relevance (Table 4).
Table 4.
Univariable and Multivariable Logistic Regression Analysis of Factors Associated With the Occurrence of Breast Implant Illness in Women Undergoing Explantation
| Variables | OR (95% CI) | P value | Adjusted OR (95% CI) | P value |
|---|---|---|---|---|
| Age | 1.0 (1.0-1.0) | 0.473 | 1.0 (0.9-1.0) | 0.381 |
| Allergy | 2.3 (1.0-5.1) | 0.044 | 2.1 (0.9-4.9) | 0.109 |
| Radiotherapy | 0.6 (0.2-1.7) | 0.337 | 0.6 (0.1-2.9) | 0.545 |
| Chemotherapy | 0.4 (0.2-1.1) | 0.075 | 0.9 (0.2-3.6) | 0.933 |
| Hormone therapy | 0.1 (0.0-0.8) | 0.026 | 0.2 (0.0-5.3) | 0.098 |
| Implant rupture | 2.6 (1.1-6.2) | 0.027 | 2.1 (0.8-5.3) | 0.130 |
CI, confidence interval; OR, odds ratio.
Breast Reconstruction After Implant Removal
After explantation, the majority of the women opted for breast shaping surgery without the use of implants. Autologous flap reconstruction (41.1%), mastopexy (10.7%), or lipofilling (2%) was performed. Some women opted for implants again within the study period (4.1%). Women opting for breast shaping or reconstructive surgery were slightly younger (51.4 years, range, 24-73 years vs 52.9 years, range, 27-81 years; P = 0.435) and had a higher BMI (25.7 vs 24.3 kg/m2; P = 0.065) compared with women who did not.
Effect of Explantation and Breast Reconstruction on Complaints
In women with implant-related complaints, including pain, explanting the implants improved complaints in no less than 72.0% of the cases. Women with suggested BII experienced improvement of the systemic complaints in 58.6%; in 31.0% complaints were persistent. For 3 BII patients (10.3%), no follow-up of the systemic complaints was reported.
In those women with suggested BII who underwent autologous breast reconstruction, improvement of systemic complaints occurred in 63.3%; 27.3% did not notice any improvement. For 1 BII patient with autologous breast reconstruction, no follow-up was reported.
Women who did not experience improvement in their symptoms after explantation were slightly younger (48.8 years, range, 29-65 years vs 50.2 years, range, 30-68 years), had a higher BMI (26.4 vs 25.3 kg/m2), and were exposed to implants longer (182.7 vs 133.2 months) than women who did experience improvement in symptoms. The differences were not statistically significant. Univariate analysis showed no associations between improvement of systemic complaints and the following variables: radiotherapy, chemotherapy, hormone therapy, immunotherapy, allergy, implant reason, previous implant exchange, implant rupture, and autologous free flap reconstruction. A significant association was found with smoking status: nonsmokers more often experienced an improvement in complaints after explantation (P = 0.034).
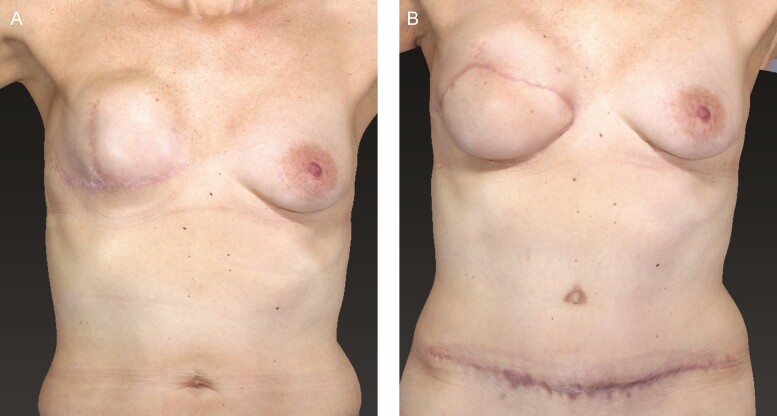
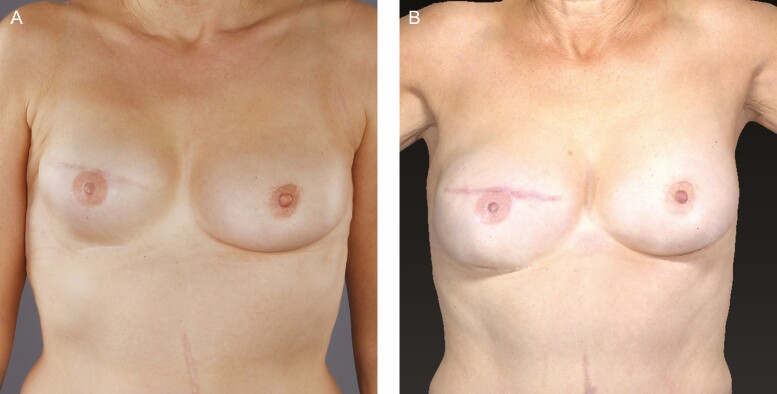
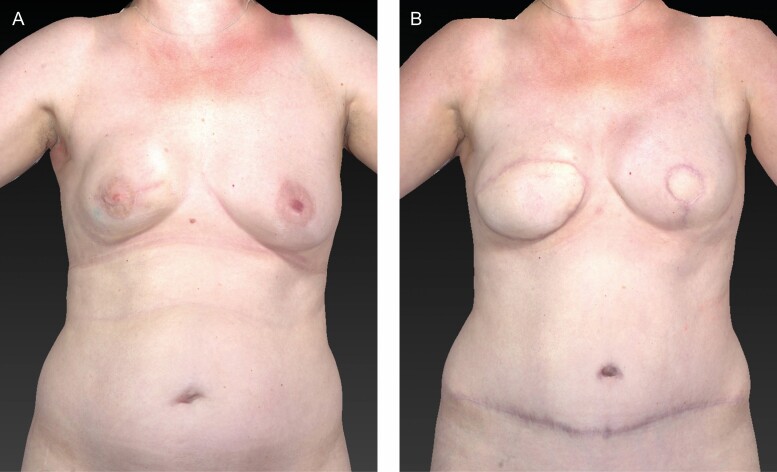
Pre- and postoperative examples of tertiary deep inferior epigastric artery perforator flap breast reconstructions are shown in Figures 1A to 3B.
Figure 1.
(A) Preoperative image of a 51-year-old female patient with a unilateral breast implant 1 year in situ. The patient reported a tight and unnatural feeling. (B) Postoperative image of the patient 4 months after unilateral tertiary deep inferior epigastric artery perforator reconstruction.
Figure 3.
(A) Preoperative image of a 60-year-old female patient with a unilateral implant 6 years in situ. Suggested breast implant illness (fatigue, arthralgia, myalgia). (B) Postoperative image of the patient 16 months after unilateral tertiary deep inferior epigastric artery perforator reconstruction.
Figure 2.
(A) Preoperative image of a 46-year-old female patient with a unilateral breast implant 1 year in situ. The patient reported severe capsular contracture and pain. Postoperative image of the patient 7 months after unilateral tertiary DIEP reconstruction and contralateral primary DIEP reconstruction after prophylactic mastectomy (BRCA1 gene mutation). DIEP, deep inferior epigastric artery perforator.
DISCUSSION
It is known that breast implants for both cosmetic and reconstructive purposes eventually need to be replaced or removed, mostly due to aesthetic dissatisfaction or capsular contracture.6,12,13 In daily practice, however, systemic complaints or concerns about the safety of SBIs are increasingly being discussed by women as a reason for considering an explantation. In this study, we have reviewed all explantation procedures performed in our center during the preceding 10 years in order to examine patient-reported symptoms preoperatively, the effect of explantation, and the effect of breast reconstruction on these symptoms.
In our study, more than half of the patients undergoing explantation reported complaints, with pain the most common symptom; 1 in 7 patients reported suggested implant-related systemic complaints other than pain. Although an association has never been proven between these complaints and implants, suggested BII was found to be the fifth most common indication for explantation. Some 60% of all BII patients reported a subjective improvement of their implant-related complaints following removal of the implants, and this proportion was even slightly higher in women who subsequently underwent flap reconstruction. This is in line with the results of our previously published systematic review.10 Correspondingly, in the case reports published thereafter, 2 of the 3 cases experienced improvement after explantation.14-16
Focusing on patients with the most severe complaints, we found several notable results. All of these patients had SBIs and their implants were ruptured significantly more often than in other cases. Although in recent years our center has mainly placed silicone implants, it has been hypothesized that silicone elicits an allergy-like immune response. This may result in an autoimmune/inflammatory syndrome induced by adjuvants (ASIA syndrome).3,17 Preexisting allergies are thought to be a risk factor and were found more frequently in women with this syndrome.18 In line with this hypothesis, we found that allergies were significantly common in women with systemic complaints. By removing the adjuvant (SBI), the immune response should decrease.19 Following explantation, over half of the patients in our study indeed experienced clinical improvement. One patient with ulcerative colitis was even able to discontinue the anti-inflammatory drug mesalazine after the implants had been removed, indicating a strong decrease in inflammation after explantation. However, those patients with the most severe systemic complaints are less likely to see their symptoms improve, suggesting that they might have developed a chronic immune response. Implant rupture and gel bleed may cause extracapsular migration of silicone-containing particles which are not completely removed when the implant is explanted. Consequently, according to this ASIA hypothesis, the immune response continues.20
Another important finding in this BII subgroup was the high prevalence of functional and psychological conditions in their medical history. This finding corresponds to studies that have shown higher levels of significant psychological symptoms in women with breast implants and women requesting explantation, irrespective of whether these symptoms were a result of the implants.21-24 A subset of these women may suffer from somatization disorder.22,25 Furthermore, authors have hypothesized that BII is a functional somatic syndrome, comparable with fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome.26,27 These syndromes have a lot of overlap in symptoms, making it difficult to distinguish between complaints caused by the implants and complaints that would also have occurred without implants, as a result of a functional syndrome. They are commonly associated with female gender and psychological factors, such as psychiatric comorbidity and health worry preoccupation.28,29 The latter may be related to fear of harmful side effects of (silicone) breast implants, which is a significant factor in women requesting removal of their implants.22,30 This fear may be stoked by the widespread (social) media attention the subject receives.31,32 It may explain why women with saline-filled implants were spared the development of BII in this study. Removal of the implants can reduce anxiety, which potentially causes a relief of symptoms. Any symptom improvement after explantation in this group may therefore be partly explained by a placebo effect.
On the other hand, explantation may have a negative impact on body image and psychological well-being.21 Therefore, alternative reconstructions should be proposed. Few studies have investigated the outcome of reconstruction after explantation. Autologous breast reconstruction after failed implant-based reconstruction was found to be safe and to improve quality of life.33,34 Most women reported the advantage of have softer, more natural feeling breasts and less pain when they compared their autologous reconstruction with their implant-based reconstruction.34 Importantly, reconstruction is only covered by the Dutch health insurance for oncology patients. The results could therefore be biased by selection. In addition, not all women are suitable for autologous reconstructions because there needs to be sufficient tissue for transplantation.35 This point is reflected in the higher BMI found in this subgroup.
Certain limitations need to be acknowledged, for example the study’s retrospective design. It is undetermined whether some symptoms attributed to the implants preexisted the surgery of were a result thereof. The same applies to psychological and physical comorbidity. Only with a prospective design, starting before implantation, can this be determined. Furthermore, during the chart review we noticed missing data regarding implant characteristics, operative reports, and the medical course of self-reported complaints. It has not been sufficiently reported whether capsules were partially or completely removed during explantation and therefore we cannot retrospectively determine this for all cases. This may have affected the clinical outcome. Systemic complaints were not systematically questioned, with limited information recorded in some medical charts, and it is likely this led to an underreporting of implant-related complaints, rather than overreporting. Conversely, in those patients who requested explantation because of suggested BII, a comprehensive documentation of both the symptoms and comorbidities was maintained. This approach of reporting encourages selection bias and should be considered when interpreting these results as well as other studies involving BII. Finally, there may be bias based on our patient population. Our center is a university hospital to which many patients with suggested BII are referred. As a result, the proportion of “systemic complaints” as an indication for implant removal will probably be higher than in a private clinic, where cosmetic reasons, for example, may more often lead to implant removal.
Despite the attention the topic of breast implants attracts, this study has demonstrated that the number of explantation procedures related to this disease is relatively low. Capsular contracture, implant rupture, and pain are common indications for implant removal, however. In women experiencing systemic implant-related complaints, it is difficult to predict whether removal will lead to an improvement of the complaints or to what extent. Nonetheless, with the insights gained here, patients requesting explantation can be provided with more comprehensive information about the expected results. In order to provide patients with the best, evidence-based information about the effects of explantation in case of BII, long-term prospective studies must be conducted in which both physical and psychological symptoms are analyzed pre- and postoperatively. It is recommended that long-term outcomes be measured by means of quality-of-life questionnaires, as these can ultimately determine whether explantation will benefit patients with implant-related complaints.
CONCLUSIONS
A relatively low prevalence of suggested BII exists among women undergoing removal of their breast implant(s); 1 in 9 explanation procedures was performed for this reason. Allergy and implant rupture may increase the likelihood of having BII. The clinical outcomes of explantation are promising: about 60% of BII patients experienced an improvement in their complaints. The same holds for women undergoing autologous breast reconstruction, which appears a good alternative. Prospective studies examining health complaints and quality of life should be performed to confirm the effectiveness of explantation as a therapy for BII.
Supplementary Material
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1. Van Slyke AC, Carr M, Carr NJ. Not all breast implants are equal: a 13-year review of implant longevity and reasons for explantation. Plast Reconstr Surg. 2018;142(3):281e-289e. [DOI] [PubMed] [Google Scholar]
- 2. Magnusson MR, Cooter RD, Rakhorst H, McGuire PA, AdamsWP, Jr., Deva AK. Breast implant illness: a way forward. Plast Reconstr Surg. 2019;143(3S A Review of Breast Implant-Associated Anaplastic Large Cell Lymphoma):74s-81s. [DOI] [PubMed] [Google Scholar]
- 3. Watad A, Quaresma M, Bragazzi NL, et al. The autoimmune/inflammatory syndrome induced by adjuvants (ASIA)/Shoenfeld’s syndrome: descriptive analysis of 300 patients from the international ASIA syndrome registry. Clin Rheumatol. 2018;37(2):483-493. [DOI] [PubMed] [Google Scholar]
- 4. Colaris MJL, de Boer M, van der Hulst RR, Cohen Tervaert JW. Two hundreds cases of ASIA syndrome following silicone implants: a comparative study of 30 years and a review of current literature. Immunol Res. 2017;65(1):120-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Balk EM, Earley A, Avendano EA, Raman G. Long-term health outcomes in women with silicone gel breast implants: a systematic review. Ann Intern Med. 2016;164(3):164-175. [DOI] [PubMed] [Google Scholar]
- 6. Coroneos CJ, Selber JC, OffodileAC, 2nd, Butler CE, Clemens MW. US FDA breast implant postapproval studies: long-term outcomes in 99,993 patients. Ann Surg. 2019;269(1):30-36. [DOI] [PubMed] [Google Scholar]
- 7. Godfrey PM, Godfrey NV. Response of locoregional and systemic symptoms to breast implant replacement with autologous tissues: experience in 37 consecutive patients. Plast Reconstr Surg. 1996;97(1):110-116. [DOI] [PubMed] [Google Scholar]
- 8. Melmed EP. A review of explantation in 240 symptomatic women: a description of explantation and capsulectomy with reconstruction using a periareolar technique. Plast Reconstr Surg. 1998;101(5):1364-1373. [DOI] [PubMed] [Google Scholar]
- 9. Rohrich RJ, Kenkel JM, Adams WP, Beran S, Conner WC. A prospective analysis of patients undergoing silicone breast implant explantation. Plast Reconstr Surg. 2000;105(7):2529-2537; discussion 2538-2543. [DOI] [PubMed] [Google Scholar]
- 10. de Boer M, Colaris M, van der Hulst R, Cohen Tervaert JW. Is explantation of silicone breast implants useful in patients with complaints? Immunol Res. 2017;65(1):25-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kulmala I, McLaughlin JK, Pakkanen M, et al. Local complications after cosmetic breast implant surgery in Finland. Ann Plast Surg. 2004;53(5):413-419. [DOI] [PubMed] [Google Scholar]
- 12. Somogyi RB, Brown MH. Outcomes in primary breast augmentation: a single surgeon’s review of 1539 consecutive cases. Plast Reconstr Surg. 2015;135(1):87-97. [DOI] [PubMed] [Google Scholar]
- 13. Pool SMW, Wolthuizen R, Moues-Vink CM. Silicone breast prostheses: a cohort study of complaints, complications, and explantations between 2003 and 2015. J Plast Reconstr Aesthet Surg. 2018;71(11):1563-1569. [DOI] [PubMed] [Google Scholar]
- 14. Marano AA, Cohen MH, Ascherman JA. Resolution of systemic rheumatologic symptoms following breast implant removal. Plast Reconstr Surg Glob Open. 2020;8(5):e2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pavlov-Dolijanovic S, Vujasinovic Stupar N. Women with silicone breast implants and autoimmune inflammatory syndrome induced by adjuvants: description of three patients and a critical review of the literature. Rheumatol Int. 2017;37(8):1405-1411. [DOI] [PubMed] [Google Scholar]
- 16. Schierbeck J, Davidsen JR, Grindsted Nielsen S, Bille C. Silicone implant incompatibility syndrome (SIIS) in a 57-year-old woman with unilateral silicone breast implant. BMJ Case Rep. 2017;2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cohen Tervaert JW, Kappel RM. Silicone implant incompatibility syndrome (SIIS): a frequent cause of ASIA (Shoenfeld’s syndrome). Immunol Res. 2013;56(2-3):293-298. [DOI] [PubMed] [Google Scholar]
- 18. Maijers MC, de Blok CJ, Niessen FB, et al. Women with silicone breast implants and unexplained systemic symptoms: a descriptive cohort study. Neth J Med. 2013;71(10):534-540. [PubMed] [Google Scholar]
- 19. Shoenfeld Y, Agmon-Levin N. ‘ASIA’—autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36(1):4-8. [DOI] [PubMed] [Google Scholar]
- 20. Cohen Tervaert JW, Colaris MJ, van der Hulst RR. Silicone breast implants and autoimmune rheumatic diseases: myth or reality. Curr Opin Rheumatol. 2017;29(4):348-354. [DOI] [PubMed] [Google Scholar]
- 21. Walden KJ, Thompson JK, Wells KE. Body image and psychological sequelae of silicone breast explantation: preliminary findings. Plast Reconstr Surg. 1997;100(5):1299-1306. [DOI] [PubMed] [Google Scholar]
- 22. Wells KE, Roberts C, Daniels SM, et al. Comparison of psychological symptoms of women requesting removal of breast implants with those of breast cancer patients and healthy controls. Plast Reconstr Surg. 1997;99(3):680-685. [DOI] [PubMed] [Google Scholar]
- 23. Roberts C, Wells KE, Daniels S. Outcome study of the psychological changes after silicone breast implant removal. Plast Reconstr Surg. 1997;100(3):595-599. [DOI] [PubMed] [Google Scholar]
- 24. Breiting VB, Hölmich LR, Brandt B, et al. Long-term health status of Danish women with silicone breast implants. Plast Reconstr Surg. 2004;114(1):217-226. [DOI] [PubMed] [Google Scholar]
- 25. Wells KE, Roberts C, Daniels SM, Kearney RE, Cox CE. Psychological and rheumatic symptoms of women requesting silicone breast implant removal. Ann Plast Surg. 1995;34(6):572-577. [DOI] [PubMed] [Google Scholar]
- 26. Dush DM. Breast implants and illness: a model of psychological factors. Ann Rheum Dis. 2001;60(7):653-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wolfe F. “Silicone related symptoms” are common in patients with fibromyalgia: no evidence for a new disease. J Rheumatol. 1999;26(5):1172-1175. [PubMed] [Google Scholar]
- 28. Aggarwal VR, McBeth J, Zakrzewska JM, Lunt M, Macfarlane GJ. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int J Epidemiol. 2006;35(2):468-476. [DOI] [PubMed] [Google Scholar]
- 29. McBeth J, Macfarlane GJ, Benjamin S, Silman AJ. Features of somatization predict the onset of chronic widespread pain: results of a large population-based study. Arthritis Rheum. 2001;44(4):940-946. [DOI] [PubMed] [Google Scholar]
- 30. Slavin SA, Goldwyn RM. Silicone gel implant explantation: reasons, results, and admonitions. Plast Reconstr Surg. 1995;95(1):63-69. [DOI] [PubMed] [Google Scholar]
- 31. Adidharma W, Latack KR, Colohan SM, Morrison SD, Cederna PS. Breast implant illness: are social media and the internet worrying patients sick? Plast Reconstr Surg. 2020;145(1):225e-227e. [DOI] [PubMed] [Google Scholar]
- 32. Tang SY, Israel JS, Afifi AM. Breast implant illness: symptoms, patient concerns, and the power of social media. Plast Reconstr Surg. 2017;140(5):765e-766e. [DOI] [PubMed] [Google Scholar]
- 33. Coriddi M, Shenaq D, Kenworthy E, et al. Autologous breast reconstruction after failed implant-based reconstruction: evaluation of surgical and patient-reported outcomes and quality of life. Plast Reconstr Surg. 2019;143(2):373-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Visser NJ, Damen TH, Timman R, Hofer SO, Mureau MA. Surgical results, aesthetic outcome, and patient satisfaction after microsurgical autologous breast reconstruction following failed implant reconstruction. Plast Reconstr Surg. 2010;126(1):26-36. [DOI] [PubMed] [Google Scholar]
- 35. Bramhall RJ, Hernan I, Harris PA. A single-centre, retrospective proof-of-concept review of salvage of infected or exposed implant breast reconstructions with explantation and one-stage free flap replacement. J Plast Reconstr Aesthet Surg. 2018;71(2):194-200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.