Abstract
Background:
Excessive alcohol use is a risk factor for injury-related deaths. Postmortem blood samples are commonly used to approximate antemortem blood alcohol concentration (BAC) levels.
Objectives:
To assess differences between antemortem and postmortem BACs among fatally injured adults admitted to one shock trauma center (STC).
Method:
Fifty-two adult decedents (45 male, 7 female) admitted to a STC in Baltimore, Maryland during 2006–2016 were included. STC records were matched with records from Maryland’s Office of the Chief Medical Examiner (OCME). The antemortem and postmortem BAC distributions were compared. After stratifying by antemortem BACs <0.10 versus ≥0.10 g/dL, differences in postmortem and antemortem BACs were plotted as a function of length of hospital stay.
Results:
Among the 52 decedents, 22 died from transportation-related injuries, 20 died by homicide or intentional assault, and 10 died from other injuries. The median BAC antemortem was 0.10 g/dL and postmortem was 0.06 g/dL. Thirty-one (59.6%) decedents had antemortem BACs ≥0.08 g/dL versus 22 (42.3%) decedents using postmortem BACs. Postmortem BACs were lower than the antemortem BACs for 42 decedents, by an average of 0.07 g/dL. Postmortem BACs were higher than the antemortem BACs for 10 decedents, by an average of 0.06 g/dL.
Conclusion:
Postmortem BACs were generally lower than antemortem BACs for the fatally injured decedents in this study, though not consistently. More routine antemortem BAC testing, when possible, would improve the surveillance of alcohol involvement in injuries. The findings emphasize the usefulness of routine testing and recording of BACs in acute care facilities.
Keywords: Alcohol, binge drinking, blood alcohol concentration (BAC), injury, deaths
Introduction
Excessive alcohol use is responsible for an average of 88,000 deaths each year in the United States and about 1,300 deaths each year in Maryland (1). Approximately half of these deaths are due to binge drinking (1). Binge drinking is defined as consuming 4 or more drinks on an occasion for women or 5 or more drinks on an occasion for men (with 14 grams of alcohol in a standard drink) (2). Consuming this amount of alcohol on an occasion—usually defined as about 2 to 3 hours—generally raises a person’s blood alcohol concentration (BAC) to ≥0.08 g/dL. A BAC of ≥0.08 g/dL is used to define alcohol-impaired driving in all states except Utah, which recently lowered the BAC limit for defining alcohol-impaired driving to ≥0.05 g/dL (3–4). Excessive alcohol consumption, particularly binge drinking, is a risk factor for fatal injuries, including those from motor vehicle crashes, falls, violence, homicide, and suicide (5–8). A dose-response relationship exists between alcohol consumption and injury severity, and the chance of injury-related death generally increases as the level of alcohol consumption increases (9).
Some studies have used postmortem BAC information to draw conclusions about antemortem BACs or the amount of alcohol consumed before an injury-related death (7–10). However, it is unclear whether postmortem BACs are a valid indicator for these conclusions. Antemortem and postmortem BACs might differ because of the metabolism of alcohol and other biological reasons (11), measurement issues and circumstances surrounding a death (e.g., environmental conditions and time elapsed between death and autopsy) (12), and administration of intravenous fluids and blood transfusions during trauma care (13).
Few studies have assessed differences in postmortem and antemortem BACs among injured decedents. One such retrospective study of 39 decedents who were admitted to a hospital and examined by the San Diego County Medical Examiner’s Office and who tested positive for alcohol found a high correlation between antemortem and postmortem BACs (14). The same antemortem blood sample was used to test each person’s BAC at two separate times—in the hospital before death and then by the medical examiner’s office after death. When antemortem blood samples were tested for BAC after death, levels were an average of 14% lower than the initial levels. In that study, data were collected from multiple hospital laboratories, introducing the potential for differences in antemortem BAC measurement methods and reducing standardization across decedents that would facilitate comparisons of changes in postmortem BACs relative to antemortem BACs.
When assessing the difference between postmortem and antemortem BACs, the likelihood of differences being attributable to having varying blood sampling collection methods would be decreased if blood samples were collected from a single facility. Furthermore, less is known about how BAC levels change when toxicology tests are conducted on two different blood samples from the same decedent before and after death. Therefore, this study sought to assess differences between antemortem and postmortem BACs among fatally injured adults admitted to one shock trauma center (STC) in Maryland. It was hypothesized that postmortem BACs would generally be lower than antemortem BACs.
Methods
Setting and Study Population
The R Adams Cowley Shock Trauma Center, located at the University of Maryland in Baltimore, has approximately 8,000 admissions per year and conducts BAC tests on at least 95% of these admissions. The state’s Office of the Chief Medical Examiner (OCME) investigates unattended deaths (i.e., when a person dies alone) that occur in the state, as well as deaths that occur after a person arrives at an acute care facility if the underlying cause of death has not been determined by medical professionals. Eligible decedents for this study were adults age ≥18 years who were admitted to the STC during 2006–2016, died within 48 hours of arriving at the STC, and had toxicology data in their records. Because BACs measured from urine or vitreous are not comparable with BACs measured using blood samples, decedents with a recorded BAC from only urine or vitreous samples were not included in this analysis (15). Decedents’ STC records were matched with the associated OCME records, using a unique identification number for each decedent. The study was exempted from local Institutional Review Board approval because the study involved secondary data analysis of existing data, documents, records and specimens.
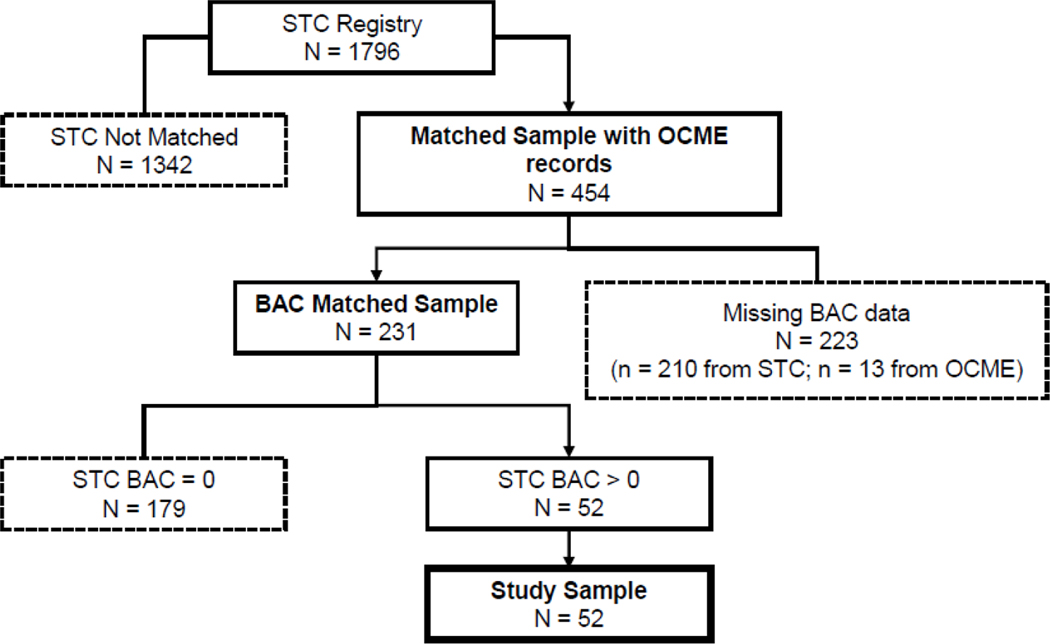
Among the 1,796 decedents identified through the STC records, 454 were matched with the OCME records (Figure 1). Common reasons for not matching included the decedent not having a case number reported from the OCME to the STC; the OCME not receiving records from the STC, so a unique identification number could not be assigned for linking the STC and OCME records; or the OCME declining to do a complete death investigation (such as if medical records were sufficient to identify cause of death). Among the 454 decedents in both the STC and the OCME records, 231 had BAC data recorded from both sources. Among those with recorded antemortem and postmortem BACs, 179 tested negative for alcohol (BAC=0.00 g/dL) and were excluded from the study. The final study sample included 52 decedents with a positive BAC (>0.00 g/dL) recorded in the STC record and a matched OCME record.
Fig. 1.
Process for deriving study sample of fatally injured adult decedents with reported blood alcohol concentration (BAC) data from the R Adams Cowley Shock Trauma Center (STC) and Maryland’s Office of the Chief Medical Examiner (OCME) in Baltimore, Maryland, 2006–2016.
Measures
Individual characteristics of the decedents (age, sex, race), length of hospital stay before death (hours), and cause of injury codes were extracted from the STC electronic medical record. The length of hospital stay before death is used as an approximate indicator of time elapsed between the antemortem blood sample and death because other data to inform the timing of the blood sample collections were not available. Causes of injury were categorized into three groups, using only the ICD-9-CM or ICD-10-CM codes in the decedents’ STC records that were applicable to the injuries incurred by the decedents in the study sample. The following three cause of injury groups were created: 1) “transport-related injuries,” including injuries related to motor vehicles (traffic and nontraffic), pedestrians, and bicyclists (ICD-9-CM: E810–E819 and E820–E825 or ICD-10-CM: V00–V09, V10–V19, V20–V29, V40–V49); 2) “homicide and intentional assault” (ICD-9-CM: E960–E969 or ICD-10-CM: X92–Y09); and 3) “other,” including intentional self-harm or suicide (ICD-9-CM: E950–E959 or ICD-10-CM: X71–X83), unintentional falls (ICD-9-CM: E880–E888 and ICD-10-CM: W10.8–W13.9), and undetermined intent (ICD-9-CM: E980–E989). The study period overlaps the transition from use of ICD-9-CM to ICD-10-CM, which occurred in the fourth quarter of 2015 (16). As a result, 36 decedents were coded using ICD-9-CM codes only, 10 were coded using ICD-10-CM codes only, and 6 were coded using both ICD-9-CM and ICD-10-CM codes. For the 6 decedents coded with both coding systems, ICD-9-CM codes were used to categorize their injury cause because these codes were likely more reliable during the transition period.
Antemortem BACs were extracted from STC records. Postmortem BACs were extracted from OCME toxicology records. BACs were measured differently in the two settings. The STC measures BAC using plasma samples, while the OCME uses whole blood. Plasma generally has a higher BAC than whole blood because of properties such as higher water content (17–20). The results from the STC plasma samples were divided by 1.14, following a standard approach for comparing plasma and whole blood samples that uses a 14% conversion factor (20). For some decedents, OCME records had multiple BACs depending on the body location from which the blood was extracted. Because BACs can vary in different parts of the body, an a priori clinical decision was made to use the following priority order of blood sample locations to assess the antemortem BACs in this analysis: heart, subclavian, femoral, subdural, and cavity (21).
Analysis
Descriptive statistics for decedent characteristics, cause of injury, and BAC level were calculated using SPSS Statistics version 26 (IBM Corp., Armonk, NY; 2019). To explore the overall distributions of BACs taken before death at the STC and after death at the OCME, all decedents’ BACs were placed into 0.05 g/dL interval bins. The number of decedents within each bin was calculated separately according to antemortem or postmortem BAC records. To examine whether the magnitude of antemortem BACs and length of hospital stay before death affected differences in postmortem BACs compared with antemortem BACs (referred to as “BAC difference”), decedents were stratified into two groups based on the median antemortem BAC of the sample (0.10 g/dL). There were 26 decedents with an antemortem BAC <0.10 g/dL and 26 decedents with an antemortem BAC ≥0.10 g/dL, and individual-level BAC differences were plotted as a function of length of hospital stay. The two groups of decedents, stratified at the median antemortem BAC level, are presented in two figures to show that the individual-level BAC differences (after death compared with before death) as a function of length of hospital stay occurred among decedents with antemortem BAC levels across the full spectrum of alcohol use (that is, among decedents with an antemortem BAC <0.10 g/dL as well as among decedents with an antemortem BAC ≥0.10 g/dL).
Results
Of the 52 fatally injured adult decedents who presented at one STC in Baltimore, Maryland in 2006–2016 and stayed ≤48 hours before dying, 45 (86.5%) decedents were male, and the average age was 42 years (standard deviation: 15.2) (Table 1). Thirty decedents were black (57.7%), 20 (38.5%) were white, and 2 (3.9%) were of other races. The median hospital stay was 2.2 hours, ranging from less than 1 hour to 44.5 hours (interquartile range: 3.1 hours). Twenty-two (42.3%) decedents suffered transportation-related injuries, either in a motor vehicle crash or as a pedestrian. Twenty (38.5%) decedents died by homicide or intentional assault; 13 of which were by gunshots. Ten (19.2%) decedents died by another cause, including intentional self-harm or suicide, accidental fall, or undetermined intent.
Table 1.
Characteristics of fatally injured adult decedents in study sample, Baltimore, Maryland
| Decedents’ Characteristics | n | Mean (SD), Median, or Percent |
|---|---|---|
| Age (years) | 52 | 42 (SD = 15.2) |
| Sex (Male) | 45 | 86.3% |
| Race | ||
| Black | 30 | 57.7% |
| White | 20 | 38.5% |
| Other Race | 2 | 3.8% |
| Length of Hospital Stay | 52 | 2.2 hours |
| Cause of Injury a | ||
| Transport-related (including motor vehicles and pedestrians) | 22 | 42.3% |
| Homicide or intentional assault | 20 | 38.5% |
| Other | 10 | 19.2% |
| BAC ≥ 0.08 g/dL | ||
| Antemortem BAC from Shock Trauma Center | 31 | 59.6% |
| Postmortem BAC from Maryland Office of Chief Medical Examiner | 22 | 42.3% |
| Median BAC | ||
| Antemortem BAC from Shock Trauma Center | 52 | 0.10 g/dL |
| Postmortem BAC from Maryland Office of Chief Medical Examiner | 52 | 0.06 g/dL |
BAC: blood alcohol concentration; SD: standard deviation.
Causes of injury were categorized into the following three groups, using only the ICD-9-CM or ICD-10-CM codes in the decedents’ medical records that were applicable to the injuries incurred by the decedents in the study sample: 1) “transport-related injuries,” including injuries related to motor vehicles (traffic and nontraffic), pedestrians, and bicyclists (ICD-9-CM: E810-E819 and E820-E825 or ICD-10-CM: V00-V09, V10-V19, V20-V29, and V40-V49); 2) “homicide and intentional assault” (ICD-9-CM E960-E969 or ICD-10-CM: X92-Y09); and 3) “other,” including intentional self-harm or suicide (ICD-9-CM: E950-E959 or ICD-10-CM: X71-X83), unintentional falls (ICD-9-CM: E880-E888 and ICD-10-CM: W10.8-W13.9), and undetermined intent (ICD-9-CM: E980-E989).
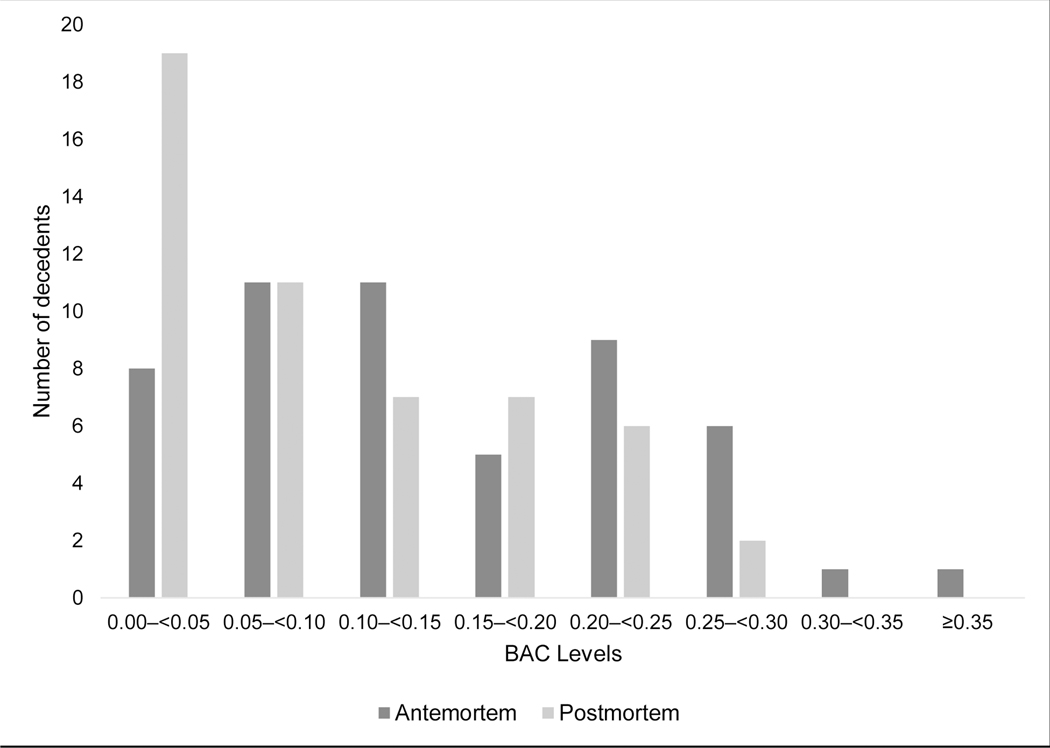
Overall, 31 (59.6%) decedents had antemortem BACs of ≥0.08 g/dL versus 22 (42.3%) decedents when assessed using postmortem BACs (Table 1). The median antemortem BAC was 0.10 g/dL compared with a median postmortem BAC of 0.06 g/dL. The overall distribution of postmortem BACs was lower than the distribution of antemortem BACs, with 19 (36.5%) decedents having a postmortem BAC of 0.00–0.05 g/dL compared with 8 (15.4%) decedents being within this range based on antemortem BACs (Figure 2).
Fig. 2.
Distribution of antemortem and postmortem blood alcohol concentration (BAC) levels among the 52 fatally injured adult decedents in the study sample. The overall distribution of postmortem BACs was lower than the distribution of antemortem BACs, with 19 (36.5%) decedents having a postmortem BAC of 0.00–0.05 g/dL compared with 8 (15.4%) decedents being within this range based on antemortem BACs.
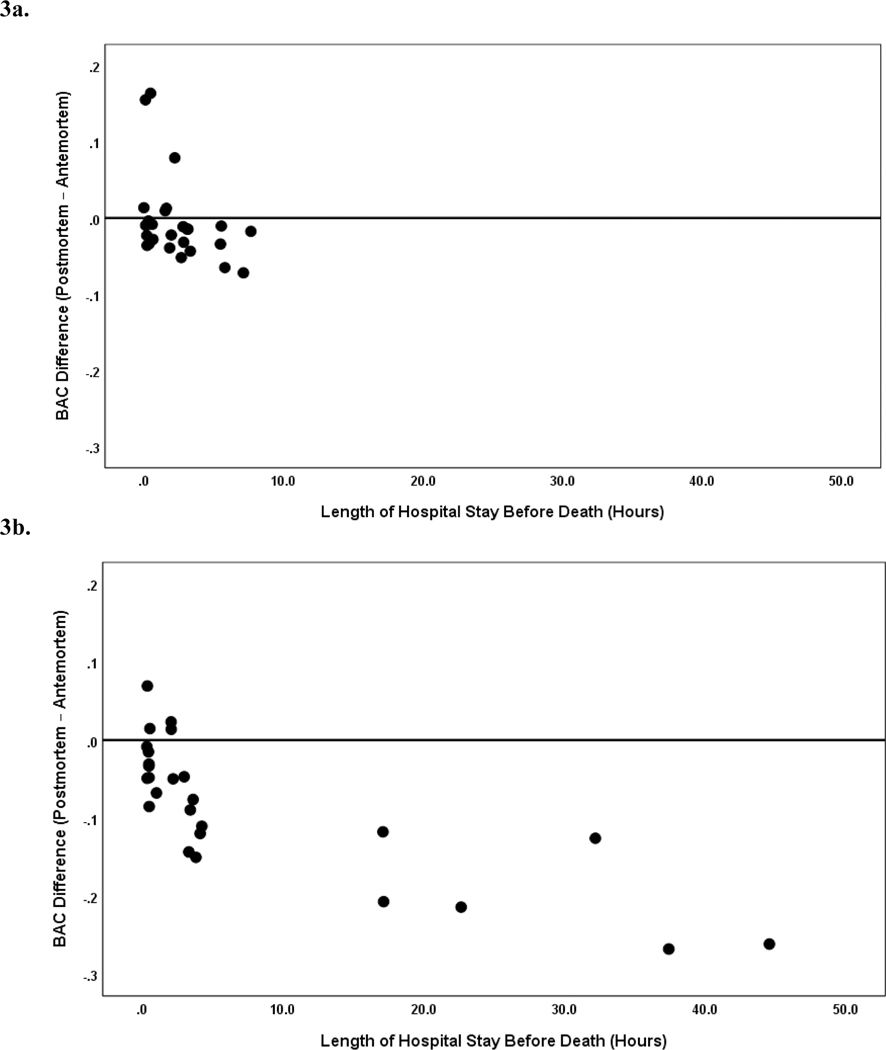
Among decedents with an antemortem BAC <0.10 g/dL (Figure 3a) and decedents with an antemortem BAC ≥0.10 g/dL (Figure 3b), decedents with a longer length of hospital stay had a greater BAC difference postmortem relative to antemortem. For 42 (80.8%) decedents, postmortem BACs were lower than the antemortem BACs by an average of 0.07 g/dL, ranging from a BAC difference with a reduction of 0.004 g/dL to 0.27 g/dL. For 10 (19.2%) decedents, the BAC difference was positive such that the postmortem BACs were higher than the antemortem BACs by an average of 0.06 g/dL, ranging from a BAC difference of an increase of 0.01 g/dL to 0.16 g/dL. Among these 10 decedents with a positive BAC difference, 6 of them had antemortem BACs of <0.10 g/dL (Figure 3a) and 4 had antemortem BACs of ≥ 0.10 g/dL (Figure 3b). The median length of hospital stay before death for those 10 decedents with a positive BAC difference was 1.1 hours, ranging from less than 1 hour to 2.2 hours. Furthermore, all decedents in the matched sample had positive antemortem BACs >0.00 g/dL. However, 10 decedents had postmortem BACs of 0.00 g/dL; among them, the antemortem BACs ranged from 0.01 g/dL 0.26 g/dL. Among those 10 decedents with no alcohol detected postmortem, the median length of hospital stay before death was 7.4 hours, ranging from 0.1 hours to 44.5 hours.
Fig. 3.
Individual level differences in postmortem blood alcohol concentration (BAC) relative to antemortem BAC among the fatally injured adult decedents in the study sample. Among decedents with an antemortem BAC <0.10 g/dL (n = 26) (Figure 3a) and decedents with an antemortem BAC ≥0.10 g/dL (n = 26) (Figure 3b), decedents with a longer length of hospital stay had a greater BAC difference postmortem relative to antemortem.
Discussion
Using data from Maryland, which has a centralized medical investigator system with highly trained forensic pathologists, this study found that postmortem BACs from the OCME for fatally injured adult decedents were generally lower than antemortem BACs from the STC. However, this finding was not consistent, with 10 of the 52 decedents having higher postmortem BACs than antemortem BACs. These differences in antemortem and postmortem BACs were found after applying a standard conversion factor of 14% to account for differences in the type of blood sample used for conducting BAC tests at the STC and the OCME (20). Other studies have used an 11% conversion factor (19), but this study used the 14% standard to be conservative. In addition, approaches that use postmortem BAC information to model antemortem BACs (e.g., the Widmark approach) have been developed, but these models require information that is not often available, such as time since ingestion of alcohol and grams of alcohol in the beverage consumed (15). Therefore, postmortem blood samples will likely continue to be used to make assumptions about individual’s alcohol use and BAC before death.
A public health related consequence of differences in postmortem BACs compared with antemortem BACs is the underestimation of alcohol involvement in injury-related deaths. For example, for 10 of the 52 decedents in this study, their antemortem BACs were positive while their postmortem BACs were negative, substantial variations in the antemortem BACs and lengths of hospital stay for those decedents, indicating variability in how these factors influence changes in BACs. Alcohol use, even at low levels, increases the risk for overdose when used concurrently with certain types of other drugs (e.g., opioids, benzodiazepines) because it leads to pharmacodynamic interactions that depress breathing (22–24). Therefore, failing to detect alcohol in postmortem toxicology testing could be especially problematic in drug overdose investigations and result in alcohol being missed as a contributing cause of death. The involvement of alcohol in drug overdose deaths could be underestimated if postmortem blood samples are used, however, in reality, antemortem blood samples are often not available because people may not receive medical attention before dying from overdoses or other injury-related causes.
Furthermore, this study found that a greater number of decedents had BACs ≥0.08 g/dL, which equates to binge drinking, when measured antemortem compared with postmortem. This suggests that use of postmortem blood alcohol samples to assess alcohol involvement in injury-related deaths may lead to conservative estimates at the population level, which has potential legal implications. For example, during investigations of fatal injuries resulting from motor vehicle crashes, BAC testing is used to determine whether a driver was alcohol-impaired. The findings from this study suggest that fewer deceased drivers would have BACs above the maximum legal BAC limit for driving if alcohol testing was conducted using postmortem blood samples rather than antemortem samples. This would be particularly likely for people who die after an extended length of time following the crash, as there would be more time for the metabolism of alcohol before death.
The situations in which postmortem BACs are higher than antemortem BACs can be highly variable and unpredictable (21). For 10 decedents in this study, postmortem BACs were higher than the antemortem BACs, including some decedents with BACs <0.10 g/dL and others with BAC ≥0.10 g/dL. The decedents who had a higher BAC after death than before death each had a short hospital stay of about 2 hours or less. This finding may be a result of alcohol production after death because of the presence of certain microbes or factors such as the time between alcohol consumption, death, and the postmortem BAC test (21). For example, it is possible for an individual to consume alcohol close to the time of an injury event, so the metabolism of the alcohol would continue after blood being drawn at the STC for the antemortem BAC test. With a larger sample population, future research could assess decedents’ characteristics and circumstances of the injury event that are associated with varying magnitudes and direction of differences between postmortem and antemortem BAC levels.
This study has limitations that are important to consider when interpreting its findings. First, despite the inclusion of data from 11 years, our study sample has only 52 fatally injured adults with a positive BAC level recorded in the STC records and an associated OCME record with toxicology data. The small sample size can be partially explained by missing BAC data in either the STC records, the OCME records, or both. For some fatally injured decedents, the OCME might use a decedent’s BAC as reported by the STC in the death investigation records. In these cases, decedents would not have both an antemortem and postmortem BAC recorded and could not be included in this study. Second, the matched sample for this study was drawn from one trauma center out of nine adult trauma centers in the state; therefore, the findings might not be generalizable to other parts of Maryland or to other states where admission procedures and testing rates might differ. The findings of this study also might not be generalizable to jurisdictions that do not have a centralized medical system because consistent procedures might not be used to conduct postmortem BAC tests. Third, almost half of the STC decedents who had an associated OCME record were missing antemortem BAC values (210 of 454 matched decedents). It is unknown whether the missing BAC values in the STC records were due to these patients not being tested for alcohol; whether they were tested for alcohol, but the BACs were not recorded; or a combination of both. Finally, the BAC data from both the STC and the OCME are subject to potential measurement and recording errors.
Given the differences in BACs when tested using postmortem blood samples from the OCME compared with the antemortem BACs from the STC, more routine alcohol testing in acute care facilities, and recording of this information in medical records, could improve surveillance of alcohol-related nonfatal and fatal injuries (25). This testing can provide useful information about risk factors associated with both nonfatal and fatal injuries.
More routine BAC testing would improve surveillance of alcohol involvement in injuries and could also inform the planning and implementation of strategies to effectively prevent excessive alcohol use and associated harms, including nonfatal and fatal injuries. The US Preventive Services Task Force recommends alcohol screening and brief intervention (SBI) for adults in primary care settings (26). Alcohol SBI can also be administered electronically (“e-SBI”) using computers, tablets, smartphones, and other electronic devices in a variety of settings (e.g., acute care settings, primary care clinics, health departments), as recommended by the US Community Preventive Services Task Force (27). These clinically oriented prevention services can complement evidence-based population level interventions (e.g., increasing alcohol taxes, regulating the density of alcohol outlets, having commercial host liability laws, enforcing maximum BAC laws of ≤0.08 g/dL, expanding use of sobriety checkpoints) (28–31). Increased use of these evidence-based strategies could reduce fatal injuries involving alcohol throughout the US.
Conclusions
The findings from this study suggest that postmortem BACs generally underestimate the magnitude of alcohol involvement in fatal injuries. Therefore, postmortem BACs may not accurately represent a person’s BAC at the time of injury. Nevertheless, for many decedents, death investigations are the only source of information about factors contributing to injury-related deaths, and the death investigations can provide important information to help prevent alcohol-related fatal injuries. However, these efforts may be thwarted when death records do not have BAC data. When possible, more routine alcohol testing in acute care facilities, and recording of this information in medical records, would improve the surveillance of alcohol-related nonfatal and fatal injuries. This would also support further research on the differences between antemortem and postmortem BACs with greater availability of alcohol data. In light of the study findings, medical examiners and coroners could consistently use antemortem blood samples, when available, for alcohol testing as part of death investigations on injured decedents. However, if antemortem blood samples are not available, the reporting of postmortem BACs in death records is still informative to broadly assess the role of alcohol in fatal injuries.
Acknowledgements
The authors would like to acknowledge Maryland’s Office of the Chief Medical Examiner for granting access to some of the data used in this study. This study was partially supported by Cooperative Agreements Numbers 5U48DP005045 for Naomi Greene and NU38OT000203 for Roumen Vesselinov, Timothy Kerns, Kimberly Auman, Margaret Lauerman from the Centers for Disease Control and Prevention. Naomi Greene was also partially supported by NCI National Research Service Award T32 CA009314. Its contents are solely the responsibility of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Disclosure of Interest
Margaret Lauerman reports grants from the National Highway Traffic Safety Association, the Maryland Highway Safety Office and the Surgical Infection Society, outside the submitted work. The authors report no other potential disclosures of interest.
References
- 1.Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis. 2014;11:130293. doi: 10.5888/pcd11.130293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute on Alcohol Abuse and Alcoholism Newsletter. Bethesda, MA: 2004. http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. [Accessed 2020 April 26] [Google Scholar]
- 3.Adult Operators of Noncommercial Motor Vehicles. Alcohol Policy Information System (APIS). https://alcoholpolicy.niaaa.nih.gov/apis-policy-topics/adult-operators-of-noncommercial-motor-vehicles/12. [Accessed 2020 April 26]
- 4.Utah Department of Public Safety. Utah’s 0.5 BAC Law. https://highwaypatrol.utah.gov/frequently-asked-questions/faq-utahs-05-bac-law/. [Accessed 2020 April 26]
- 5.Ertl A, Sheats KJ, Petrosky E, Betz CJ, Yuan K, Fowler KA. Surveillance for Violent Deaths — National Violent Death Reporting System, 32 States, 2016. MMWR Surveill Summ 2019;68(No. SS-9):1–36. doi: 10.15585/mmwr.ss.6809a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: a metaanalysis. Ann Emerg Med. 1999;33(6):659–68. doi: 10.1016/S0196-0644(99)70195-2. [DOI] [PubMed] [Google Scholar]
- 7.Conner KR, Lathrop S, Caetano R, Silenzio V, Nolte KB. Blood alcohol concentrations in suicide and motor vehicle crash decedents ages 18 to 54. Alcohol Clin Exp Res. 2016;40(4):772–5. doi: 10.1111/acer.13002. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Statistics and Analysis. Alcohol-impaired driving: 2017 data. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812630. [Accessed 2020 April 26]
- 9.Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C. The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110(1–2):108–16. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan MS, Huguet N, McFarland BH, Caetano R, Conner KR, Giesbrecht N. Use of alcohol before suicide in the United States. Ann Epidemiol. 2014;24(8):588–92. doi: 10.1016/j.annepidem.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly AT, Mozayani A. An overview of alcohol testing and interpretation in the 21st century. J Pharm Pract. 2012;25(1):30–6. doi: 10.1177/0897190011431149. [DOI] [PubMed] [Google Scholar]
- 12.Kugelberg FC, Jones AW. Interpreting results of ethanol analysis in postmortem specimens: a review of the literature. Forensic Sci Int. 2007;165(1):10–29. doi: 10.1016/j.forsciint.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Jones AW. Impact of trauma, massive blood loss and administration of resuscitation fluids on a person’s blood-alcohol concentration and rate of ethanol metabolism. Acad Forensic Pathol. 2016;6(1):77–88. doi: 10.23907/2016.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saitman A, Estrada J, Fitzgerald RL, McIntyre IM. Comparative analysis of hospital and forensic laboratory ethanol concentrations: a 15 month investigation of antemortem specimens. J Forensic Leg Med. 2015;33:23–7. doi: 10.1016/j.jflm.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Cowan DM, Maskrey JR, Fung ES, Woods TA, Stabryla LM, Scott PK. Best-practices approach to determination of blood alcohol concentration (BAC) at specific time points: Combination of ante-mortem alcohol pharmacokinetic modeling and post-mortem alcohol generation and transport considerations. Regul Toxicol Pharmacol. 2016;78:24–36. doi: 10.1016/j.yrtph.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. State injury indicators report: instructions for preparing 2015 data. Thomas KE, Johnson RL, editors. Centers for Disease Control and Prevention; 2017. doi: 10.1017/CBO9781107415324.004. [DOI] [Google Scholar]
- 17.American Prosecutors Research Institute. Alcohol toxicology for prosecutors: targeting hardcore impaired drivers. Alexandria, VA: 2003. https://ndaa.org/wp-content/uploads/toxicology_final.pdf. [Accessed 2020 April 26] [Google Scholar]
- 18.Charlebois RC, Corbelt MR, Wigmore JG. Comparison of ethanol concentrations in blood, serum, and blood cells for forensic application. J Anal Toxicol. 1996;20(3):171–8. doi: 10.1093/jat/20.3.171. [DOI] [PubMed] [Google Scholar]
- 19.Hodgson BT, Shajani NK. Distribution of ethanol: plasma to whole blood ratios. Can Soc Forensic Sci J. 1985;18(2):73–7. doi: 10.1080/00085030.1985.10757386. [DOI] [Google Scholar]
- 20.Winek CL, Carfagna M. Comparison of plasma, serum, and whole blood ethanol concentrations. J Anal Toxicol. 1987;11(6):267–8. doi: 10.1093/jat/11.6.267. [DOI] [PubMed] [Google Scholar]
- 21.Ziavrou K, Boumba VA, Vougiouklakis TG. Insights into the origin of postmortem ethanol. Int J Toxicol. 2005;69–77. doi: 10.1080/10915810590936391. [DOI] [PubMed] [Google Scholar]
- 22.Van der Schrier R, Roozekrans M, Olofsen E, Aarts L, van Velzen M, de Jong M, et al. Influence of ethanol on oxycodone-induced respiratory depression: a dose-escalating study in young and elderly individuals. Anesthesiology. 2017;126(3):534–42. doi: 10.1097/ALN.0000000000001505. [DOI] [PubMed] [Google Scholar]
- 23.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA. 2018;319(17):1819–21. doi: 10.1001/jama.2018.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esser MB, Guy GP Jr., Zhang K, Brewer RD Binge drinking and prescription opioid misuse in the U.S., 2012–2014. Am J Prev Med. 2019;57(2):197–208. doi: 10.1016/j.amepre.2019.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osborn M. Guidelines on autopsy practice: autopsy when drugs or poisoning may be involved. London: 2018. https://www.rcpath.org/profession/guidelines/autopsy-guidelines-series.html. [Accessed 2020 April 26] [Google Scholar]
- 26.United States Preventive Services Task Force. Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(18):1899–1909. doi: 10.1001/jama.2018.16789. [DOI] [PubMed] [Google Scholar]
- 27.Tansil KA, Esser MB, Sandhu P, Reynolds JA, Elder RW, Williamson RS. Alcohol electronic screening and brief intervention: A Community Guide systematic review. Am J Prev Med. 2016;51(5):801–11. doi: 10.1016/j.amepre.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elder RW, Lawrence B, Ferguson A, Naimi TS, Brewer RD, Chattopadhyay SK. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 2010;38(2):217–29. doi: 10.1016/j.amepre.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell CA, Hahn RA, Elder R, Brewer R, Chattopadhyay S, Fielding J. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med. 2009;37(6):556–69. doi: 10.1016/j.amepre.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 30.Rammohan V, Hahn RA, Elder R, Brewer R, Fielding J, Naimi TS. Effects of dram shop liability and enhanced overservice law enforcement initiatives on excessive alcohol consumption and related harms: two Community Guide systematic reviews. Am J Prev Med. 2011;41(3):334–43. doi: 10.1016/j.amepre.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 31.The Community Guide. What works: motor vehicle -related injury prevention. https://www.thecommunityguide.org/sites/default/files/assets/What-Works-Factsheet-MotorVehicle.pdf. [Accessed 2020 April 26]