Abstract
Background
Non-operative management (NOM) of uncomplicated acute appendicitis (AA) has been introduced as an alternative to appendectomy. This umbrella review aimed to provide an overview of the efficacy and safety of NOM of uncomplicated AA in the published systematic reviews.
Methods
This umbrella review has been reported in line with the PRISMA guidelines and umbrella review approach. Systematic reviews with and without meta-analyses on the efficacy of NOM of AA were analyzed. The quality of the reviews was assessed with the AMSTAR 2 tool. The main outcomes measures were the treatment failure and complication rates of NOM and hospital stay as compared to appendectomy.
Results
Eighteen systematic reviews were included to this umbrella review. Eight reviews documented higher odds of failure with NOM, whereas two reviews revealed similar odds of failure. Six reviews reported lower odds of complications with NOM, six reported similar odds, and one reported lower odds of complications with surgery. Eight reviews reported similar hospital stay between NOM and appendectomy, one reported longer stay with NOM and another reported shorter stay with NOM. Pooled analyses showed that NOM was associated with higher treatment failure overall, in children-only, adults only, and RCTs-only meta-analyses. NOM was associated with lower complications overall, yet children-only and RCTs-only analyses revealed similar complications to surgery. NOM was associated with shorter stay in the overall and adult-only analysis, but not in the children-only analysis.
Conclusions
NOM of AA is associated with higher treatment failure, marginally lower rate of complications and shorter stay than appendectomy.
Introduction
Acute appendicitis (AA) is the most common abdominal and surgical emergency and accounts for more than 40,000 hospital admissions in England with an incidence of 1.1 cases per 1000 people annually [1, 2]. AA commonly affects young and middle-age individuals, but no age is exempt. A male preponderance has been noticed, with a male to female ratio of 1.4:1 [3].
The diagnosis of AA can be made on the basis of clinical data; nonetheless the use of laboratory parameters such as total leukocyte count, scoring systems as Alvarado score, and imaging has been widely adopted [4]. To date, contrast CT scanning is considered the most accurate modality for the definitive diagnosis of AA with a sensitivity and specificity exceeding 90% [5].
Uncomplicated AA is treated with appendectomy which has been considered the gold standard treatment for such a condition for decades. Yet, non-operative management (NOM) of AA with antibiotics has been devised as a viable alternative to surgery [6]. Interestingly, NOM that involves supportive measures such as intravenous fluids and analgesics without antibiotics was found to yield similar treatment failure rates to NOM involving a 4-day course of antibiotics [7].
Large, multicenter randomized controlled trials that compared the outcome of NOM with appendectomy have concluded promising results after NOM. The CODA trial [8] described NOM with antibiotics as non-inferior to appendectomy on the basis of results of a standard health-status measure. However, about 30% of patients who received NOM had to undergo appendectomy by day 90 after ending treatment.
Although several clinical trials and meta-analyses have assessed the efficacy and safety of NOM of acute appendicitis, no consensus has been reached on the role of NOM in AA. The practice management guideline of the Eastern Association of Surgery for Trauma (EAST) could not make a recommendation for or against NOM as primary treatment for uncomplicated AA and found several limitations of the published literature, which necessitates more research on this topic [9].
Umbrella reviews are considered a tertiary level of research that assesses, cumulates and combines published systematic reviews in both quantitative and qualitative manner [10]. Since umbrella reviews compare the outcomes of systematic reviews relevant to the review question, considering only the highest level of evidence, namely other systematic reviews and meta-analyses for inclusion, the findings of umbrella reviews may be relied upon when developing guidelines and making a consensus [11].
The present work is the first umbrella review of NOM of acute appendicitis that aimed to combine the results of published systematic reviews to provide a broad overview of the efficacy and safety of NOM of uncomplicated AA in terms of the pooled rates of failure, recurrence, complications, and stay after NOM and to assess the level of evidence for clinical practice. The hypothesis and objective of this umbrella review was to provide the surgeons and patients with the risks and benefits of each approach (NOM versus appendectomy) to determine the tradeoffs in order to inform decision-making.
Methods
Reporting and registration
The protocol of this umbrella systematic review has been registered a priori in the International prospective register of systematic reviews (PROSPERO) under special identifier CRD42021255006. The reporting guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [12] and Umbrella review approach [11] were followed when reporting this umbrella systematic review.
Strategy of literature search
Databases searched
Two independent investigators (S.E., H.E.) performed an organized literature search of electronic databases including PubMed, Scopus, and Web of Science for published systematic reviews with or without meta-analysis on the outcome of NOM of uncomplicated AA. The databases were searched from their inception through April 2021. To increase the sensitivity of the search process, an Internet-based search using Google Scholar service was conducted.
Search keywords
Keywords used in the search process comprised “appendicitis,” “appendix,” “Uncomplicated,” “treatment,” “management,” “non-operative,” “conservative,” antibiotics,” “systematic review,” “meta-analysis.” In addition, the following medical subject headings (MeSH) terms were included in the literature search: (appendicitis), (conservative treatment), (meta-analysis).
Search strategy
The PubMed function “related articles” was activated to search for other relevant studies. In addition, we hand-searched the reference sections of the studies initially retrieved. A preliminary screening by title and abstract was performed then full-text screening of the studies was followed. The full text of the selected articles was reviewed by two independent investigators to check for eligibility.
Eligibility for inclusion
Studies deemed eligible for inclusion had to fulfill the following PICOS criteria:
P (population): patients with established diagnosis of uncomplicated AA, whether children only, adults only, or both (mixed population).
I (intervention): NOM of AA.
C (comparator): appendectomy, whether by open or laparoscopic approach.
O (outcome): treatment failure, complications, and length of hospital stay.
S (study design): systematic reviews with or without concurrent meta-analysis.
We excluded irrelevant articles, articles of other designs, editorials, and narrative reviews. Only articles published in English were included to this review.
Assessment of methodologic quality and risk of BIAS
The quality of each study was assessed by two authors independently using the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2) tool [13]. The AMSTAR 2 tool is a 16-item checklist used to critically rate the quality of an individual systematic review as critically low, low, moderate, or high. (https://amstar.ca/Amstar_Checklist.php). Discrepancies in outcome interpretation were resolved by consensus and adjudication by a third reviewer.
Grading the evidence
The following criteria [14] were used to assess the grade of evidence of the included meta-analyses:
Convincing evidence (class I): > 1000 cases, significant combined associations for random-effects calculation (p < 10–6), no evidence of small-study effects, no evidence of excess of significance, and no large between-study heterogeneity (I2 < 50%)
Highly suggestive evidence (class II): > 1000 cases, significant combined associations for random-effects calculation (p < 10–6), and the largest study with 95%CI excluding the null value.
Suggestive evidence (class III): > 1000 cases and significant combined associations for random-effects calculation (p < 10–3).
Weak evidence (class IV): Other associations with p < 0.05; non-significant associations with p > 0.05.
Data extraction
Two authors reviewed the full-text of the studies included independently and extracted the following data points from each systematic review into a standardized form for data extraction:
Authors and year of publication.
Databases searched and inclusion criteria.
Number and type of studies included in each systematic review.
Total number of patients, number who had NOM, and number who had appendectomy.
Failure rate of NOM.
Complications after NOM and appendectomy.
Length of hospital stay in days.
Effect estimates for failure, complications, and hospital stay.
Outcomes
The primary outcome of this umbrella review was the failure rate of NOM defined as the need for appendectomy either within the index admission or after discharge for increasing or persistent symptoms or development of serious complications such as perforation warranting surgery. Recurrence of AA was defined as an episode of appendicitis being diagnosed again after completion of the initial NOM and discharge of patient. Secondary outcomes were the complication rate of NOM and of appendectomy and length of hospital stay.
Data analysis
Continuous variables were expressed as mean ± standard deviation (SD), or median and normal range. Categorical variables were expressed as numbers and proportions. Review Manager 5.4 was used for pooling of the effect estimate of treatment failure, complications, and hospital stay in the published meta-analyses. The summary (pooled) effect estimates and 95%confidence interval (CI) for each outcome were calculated by combining the effect estimates reported in previously published meta-analyses using the DerSimonian–Laird random-effect model. The summary effect estimates were expressed as risk ratio (RR) for failure and complications and standardized mean difference (SMD) for hospital stay.
Stratified and subgroup analyses were performed, with estimates summarized by patient population (adults only, children only, mixed population) and type of studies included (meta-analyses of RCTs).
Statistical heterogeneity was assessed by the p value of the Higgins inconsistency (I2) statistics and the χ2-based Cochran’s Q test. Heterogeneity was considered low if I2 < 25%, moderate if I2 was 25–75%, and high if I2 > 75%. P values less than 0.05 were considered significant.
Excess statistical significance was assessed using The Ioannidis’ excess significance test [15]. The number of the observed (O) positive studies (p < 0.05) in each meta-analysis was compared to the expected number of studies with significant results (E). The expected number of studies with significant results (E) was calculated by summation of the statistical power estimates for each study in a meta-analysis. To estimate the statistical power of each individual study, we used the effect size of the largest study that had the smallest standard error in each included meta-analysis [16]. Excess statistical significance was determined for each meta-analysis when O was greater than E with a two-sided p < 0.10.
Publication bias and small-study effect were assessed using a funnel plot of the standard error of each outcome against the rate of the outcome in the studies reviewed. A straight vertical line in the plot indicates the zone in which 95% of studies should be if there were no publication biases. Furthermore, Egger’s regression test was used to investigate for small-study effect where smaller studies tend to provide larger effect estimates than larger studies. In random-effects meta-analysis, p < 0.1 indicated the presence of small-study effects.
A random-effect meta-regression model was used weighing the studies by their within-study variance and the degree of heterogeneity. The inter-study heterogeneity was assessed in terms of differences in patients’ age, sex, type of population (children vs adult vs mixed), total leucocyte count, follow-up duration, and quality of the study. The statistical significance of each examined variable was expressed using slope coefficient (SE) and p value. P value < 0.1 was considered statistically significant.
Results
Characteristics of the reviews included
After screening of 487 non-duplicate articles, 18 systematic reviews with or without meta-analysis [17–34] published between 2011 and 2021 were included to the present umbrella review. The PRISMA flowchart for study selection is shown in Fig. 1.
Fig. 1.
PRISMA flowchart for study selection and inclusion
Databases searched: PubMed/MEDLINE were searched in all (100%) systematic reviews, Embase in 13 (72.2%) reviews, Cochrane central register/library in 11 (61.1%) reviews, Scopus in three reviews (16.7%), and Web of Science in three reviews (16.7%).
Number and type of studies included: The median number of studies included in each review was 6 (range, 4–21). Eight systematic reviews included RCTs only and ten included both RCTs and cohort studies.
Patient population: Six (33.3%) systematic reviews involved adults only, four (22.2%) involved children only, and eight (44.4%) included both adults and children. The median number of patients included to the reviews was 1430 (range, 320–67,688) patients. The median percentage of patients who had NOM was 48.2% (range, 8.5%–69.5%).
Appraisal of quality and level of evidence: Overall, ten systematic reviews were of low quality, five of moderate quality, two of high quality and one of critically low quality. Regarding the level of evidence, 10 studies entailed weak evidence, six entailed suggestive evidence, and two entailed highly suggestive evidence.
The databases searched, inclusion criteria, number and types of studies included, patient population, and quality of the published systematic reviews are summarized in Tables 1 and 2.
Table 1.
Inclusion period, databases searched, inclusion criteria, and quality of the published systematic reviews
| Studies | Inclusion period | Databases searched | Inclusion criteria | AMSTAR2 | Level of evidence |
|---|---|---|---|---|---|
| Emile SH et al. [17] | Inception-Nov 2020 | PubMed, Scopus, EMBASE, and Web of Science | Single-arm case series, cohort, and comparative studies that compared the outcome of NOM with appendectomy with at least five patients, in the setting of COVID-19 | Low | Suggestive |
| Maita S et al. [18] | Inception-May 2019 | PubMed, Embase, Cochrane and Web of Science | All studies focusing on the initial NOM and comparing antibiotic treatment with appendectomy for acute nonperforated appendicitis in children | Critically low | Weak |
| Prechal et al. [19] | Nov 1965 to Jan 2016 | PubMed, Cochrane Library, Web of Science, trial registries | RCTs including patients ≥ 18 years with acute uncomplicated appendicitis which compared NOM with any form of appendectomy | Low | Suggestive |
| Podda et al. [20] | Inception-Aug 2018 | MEDLINE (via PubMed), the Cochrane, EMBASE | RCTs, prospective and retrospective cohort studies comparing NOM and appendectomy for acute uncomplicated appendicitis in adults and children | Moderate | Suggestive |
| Poprom et al. [21] | Inception-July 2017 | Medline and Scopus | RCTs comparing NOM and appendectomy for acute uncomplicated appendicitis in adults and children reporting one of: success, complications, recurrence, and length of stay | Moderate | Suggestive |
| Kessler et al. [22] | 1950–2017 | MEDLINE (via PubMed), Ovid Embase, the Cochrane library | Studies that assessed both appendicectomy and the NOM of acute uncomplicated appendicitis in children of less than 18 years of age | Low | Weak |
| Talutis et al. [23] | 1996–2017 | PubMed | Prospective studies and trials that compared operative and antibiotic management of acute appendicitis in adults and pediatric populations | Low | Weak |
| Xu et al. [24] | 1946–2016 | MEDLINE, Embase | All studies focusing on the NOM of acute uncomplicated appendicitis in children | Low | Weak |
| Gorter et al. [25] | Inception-Jan 2017 | MEDLINE, Embase | All studies investigating initial nonoperative treatment strategy for Uncomplicated appendicitis in patients younger than eighteen years (children) | Low | Weak |
| Sakran et al. [26] | Inception-Jan 2017 | PubMed, Cochrane, and Scopus | RCTs that compared NOM and appendectomy in adult patients with uncomplicated acute appendicitis | Low | Highly suggestive |
| Podda et al. [27] | Inception-May 2016 | PubMed, EMBASE, Medline, Google Scholar and Cochrane Central Register | RCTs comparing NOM and surgical treatment as primary treatment for uncomplicated acute appendicitis in adults irrespective of language and publication status | Low | Suggestive |
| Findlay et al. [28] | Inception-May 2016 | PubMed, EMBASE, Cochrane Central Register of Controlled Trials | RCTs randomizing patients > 16 years to NOM or appendectomy for uncomplicated acute appendicitis | Low | Weak |
| Harnoss et al. [29] | Inception-Jan 2015 | MEDLINE (via PubMed), EMBASE, the Cochrane Library | RCTs and nonrandomized cohort studies assessing NOM versus surgical treatment for uncomplicated acute appendicitis in adults | High | Highly suggestive |
| Ehlers et al. [30] | Inception-June 2015 | PubMed (Medline) and EMBASE | RCTs that compared antibiotics with appendectomy for acute appendicitis | Moderate | Weak |
| Sallinen et al. [31] | Jan 2011-Dec 2015 | MEDLINE, Embase and the Cochrane Central Register of Controlled Trials | RCTs that compared antibiotic treatment with appendicectomy in patients with suspected acute non-perforated appendicitis | Moderate | Weak |
| Wilms et al. [32] | Inception-June 2011 | MEDLINE, Embase and the Cochrane Central Register of Controlled Trials, Prospective trial registries | RCTs and Quasi RCT that compared NOM antibiotic treatment with appendectomy in patients with suspected acute appendicitis | High | Weak |
| Liu et al. [33] | 1970–2009 | MEDLINE | Studies that compared NOM with appendectomy in patients with acute uncomplicated appendicitis | Low | Suggestive |
| Ansaloni et al. [34] | 1966–2009 | MEDLINE, Embase and the Cochrane Central Register of Controlled Trials, Cochrane Library | RCTs comparing surgery with NOM antibiotic therapies for the treatment of adult patients with acute appendicitis | Moderate | Weak |
*NOM = non-operative management *RCTs = randomized controlled trials
Table 2.
Number and type of studies and patient population in the published systematic reviews
| Studies | Number of studies | Type of studies | Population | Total number of patients | % NOM | Follow up in months |
|---|---|---|---|---|---|---|
| Emile SH et al. [17] | 14 | 8 Retrospective and 6 Prospective | Mixed | 2140 | 44.8 | 30 |
| Maita S et al. [18] | 21 | 8 Retrospective and 13 Prospective | Children | 67,688 | 8.5 | 14 |
| Prechal et al. [19] | 5 | 5 RCTs | Adults | 1430 | 50.8 | 13.2 |
| Podda et al. [20] | 20 | 8 RCT, 4 Retrospective, 8 Prospective | Mixed | 3618 | 48.2 | 12 |
| Poprom et al. [21] | 9 | 9 RCTs | Mixed | 2108 | Not reported | 12 |
| Kessler et al. [22] | 5 | 1 RCT, 1 Retrospective, 3 Prospective | Children | 442 | 42.8 | 12–48 |
| Talutis et al. [23] | 11 | 4 RCTs, 7 Prospective | Mixed | 2422 | 50.4 | 12–24 |
| Xu et al. [24] | 15 | 1 RCT, 4 Retrospective, 8 Prospective | Children | 1163 | 69.4 | 12 |
| Gorter et al. [25] | 5 | 1 RCT, 2 Retrospective, 2 Prospective | Children | 320 | 45.9 | 12 |
| Sakran et al. [26] | 5 | 5 RCTs | Adults | 1430 | 50.8 | 12 |
| Podda et al. [27] | 5 | 5 RCTs | Adults | 1351 | 46.8 | 18.5 |
| Findlay et al. [28] | 6 | 6 RCTs | Adults | 1724 | 48.5 | 12 |
| Harnoss et al. [29] | 8 | 4 RCTs, 4 Cohort | Adults | 2551 | 51.4 | 12 |
| Ehlers et al. [30] | 6 | 6 RCTs | Mixed | 1720 | 48.5 | 12 |
| Sallinen et al. [31] | 5 | 5 RCTs | Mixed | 1072 | 47.6 | 12 |
| Wilms et al. [32] | 5 | 5 RCTS and Quasi RCTs | Mixed | 901 | 46.1 | 1–12 |
| Liu et al. [33] | 6 | 4 RCTs, 1 Prospective, 1 Retrospective | Mixed | 1201 | 36.1 | 14.5 |
| Ansaloni et al. [34] | 4 | 4 RCTs | Adults | 741 | 52.6 | 12 |
*NOM = non-operative management *RCTs = randomized controlled trials
Outcome of NOM
Efficacy of treatment: The median failure rate of NOM across the systematic reviews was 25% (range, 6.9%–37.4%). Recurrence of symptoms within one year after NOM occurred in a median of 18.3% of patients (range, 10.8–26.5%). Eight reviews documented higher odds of failure with NOM as compared to appendectomy, whereas two systematic reviews revealed similar odds of failure. The median follow-up across the systematic reviews ranged from 12 to 48 months.
Complications: The median complication rate after NOM was 6.9% (range, 1–32.6%) and the median complication rate after appendectomy was 10.5% (range, 2–27%). Six reviews reported lower odds of complications with NOM as compared to surgery, six reported similar odds, and one reported lower odds of complications with surgery.
Hospital stay: Eight reviews reported similar hospital stay between NOM and appendectomy, one reported longer stay with NOM and another reported shorter stay with NOM.
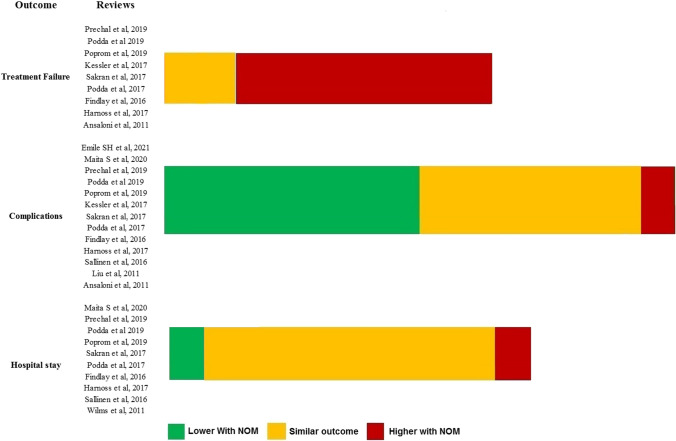
A summary of the effect estimates used for treatment failure, complications, and hospital stay in each systematic review is shown in Table 3. The quantitative outcomes of the systematic reviews that compared NOM with appendectomy are summarized in Table 4. Figure 2 shows a visual representation of the outcome of the published systematic reviews.
Table 3.
Effect estimates of treatment failure, complications, and hospital stay in the published systematic reviews
| Studies | Treatment failure | Complications | Hospital stay |
|---|---|---|---|
| Emile SH et al. [17] | NA |
Lower with NOM (OR = 0.36, 95%CI: 0.14–0.93, p = 0.03, I2 = 57.9%) |
NA |
| Maita S et al. [18] | NA |
Similar (OR = 0.64, 95%CI: 0.29- 1.39) |
Similar (MD = 0.07, 95%CI:—0.8–0.66) |
| Prechal et al. [19] | Lower failure with surgery (RR = 0.65, 0.55–0.76, I2 = 85%) |
Similar (RR = 0.98, 0.82–1.18, I2 = 82%) |
Similar (MD = 0.11, 95%CI: -0.22–0.43, I2 = 68%) |
| Podda et al. [20] | Lower failure with surgery (OR = 0.12, 0.06–0.24, I2 = 81%) |
Lower after NOM (OR = 0.41; 95% CI 0.22–0.77; P = 0.006; I2 = 68%) |
Similar (SMD = 0.55; 95%CI:1.49–0.39; P: 0.25; I2: 99%) |
| Poprom et al. [21] |
Similar (OR = 0.70; 95%CI: 0.49–1.01) |
Lower with NOM 0.39 (95%CI: 0.22, 0.70) |
Similar (MD = 0.17, 95%CI: -0.23, 0.56) |
| Kessler et al. [22] | Lower with surgery (RR = 0.77, 95% CI: 0.71- 0.84; p < 0.001) |
Similar (RR 1.07, 95% CI 0.26—4.46) |
NA |
| Xu et al. [24] | Similar (OR = 1.5; 95%CI = 0.38–5.9, p = 0.56, I2 = 39.2%) | NA | NA |
| Sakran et al. [26] |
Lower with surgery (RR = 0.68; 95% CI: 0.60–0.77; p < 0.001, I2 = 77.5%) |
Lower with NOM (RR = 0.32; 95% CI: 0.24–0.43; p < 0.001, I2 = 34%) |
Similar (WMD = 0.20; 95% CI: − 0.16–0.56; p = 0.285, I2 = 70.5%) |
| Podda et al. [27] |
Lower with surgery (OR = 0.07, 95% CI: 0.02–0.24, P < 0.0001, I2 = 70% |
Similar (RR = 0.51, 95% CI: 0.13–1.95, p = 0.32; I2 = 84%) |
Similar (SMD = 1.54, 95% CI: 0.47–3.54; P = 0.13, I2 = 99%) |
| Findlay et al. [28] |
Lower with surgery (RR = 0.92; 95% CI 0.87- 0.97; p = 0.002, I2 = 30%) |
Similar (RR = 0.41, 95%CI: 0.13–1.3%, p = 0.13, I2 = 76%) |
Longer with NOM (MD = 0.48, 95%CI: 0.1–0.85, p = 0.01, I2 = 52%) |
| Harnoss et al. [29] |
Lower with surgery (RR 0.75; 95% CI 0.70–0.79; P = 0.00001; I2: 62%) |
Lower with surgery (RR: 0.78; 95% CI 0.72–0.83; P < 0.00001; I2:16.2%) |
Similar (RR-0.73; 95% CI-2.69–1.23; P = 0.47; I2 = 0%) |
| Sallinen et al. [31] | NA | Similar (RD = – 2·6; 95%CI: 6·3, 1·1, p = 0.16, I2 = 26%) | Similar (MD = –3·58; 95%CI: 8·27, 1·11, p = 0.13, I2 = 95%) |
| Wilms et al. [32] | NA | NA | Shorter with NOM (OR = 0.66; 95% CI: 0.44–0.87, p < 0.001, I2 = 33%) |
| Liu et al. [33] | NA | Lower with NOM (OR = 0.31, 95%CI:0.19- 0.49, p = 0.001) | NA |
| Ansaloni et al. [34] |
Higher with NOM (OR = 6.01, 95% CI = 4.2–8.4) |
Higher with surgery (OR = 1.92; 95%CI: 1.30–2.85) | NA |
*RR = risk ratio *OR = odds ratio *MD = mean difference *NOM = non-operative management
Table 4.
Tabular representation of the quantitative outcomes of the systematic reviews
| Outcome | Systematic review | Studies/patients | Findings | ES | Upper CI | Lower CI | P value | Heterogeneity |
|---|---|---|---|---|---|---|---|---|
| Treatment failure | Prechal et al. [19] | 5/1430 | Lower with surgery | RR = 0.65 | 0.55 | 0.76 | < 0.0001 | I2 = 85% |
| Podda et al. [20] | 30/3618 | Lower with surgery |
OR = 0.12 |
0.06 | 0.24 | < 0.0001 | I2 = 81% | |
| Poprom et al. [21] | 9/2108 | Similar | OR = 0.70 | 0.49 | 1.01 | NA | NA | |
| Kessler et al. [22] | 5/422 | Lower with surgery | RR = 0.77 | 0.71 | 0.84 | < 0.0001 | NA | |
| Xu et al. [24] | 15/1163 | Similar |
OR = 1.5 |
0.38 | 5.9 | 0.56 | 39.2% | |
| Sakran et al. [26] | 5/1430 | Lower with surgery | RR = 0.68 | 0.60 | 0.77 | < 0.0001 | I2 = 77.5% | |
| Podda et al. [27] | 5/1351 | Lower with surgery | OR = 0.07 | 0.02 | 0.24 | < 0.0001 | I2 = 70% | |
| Findlay et al. [28] | 6/1724 | Lower with surgery | RR = 0.92 | 0.87 | 0.97 | 0.002 | I2 = 30% | |
| Harnoss et al. [29] | 8/2551 | Lower with surgery | RR 0.75 | 0.70 | 0.79 | 0.00001 | I2 = 62% | |
| Ansaloni et al. [34] | 4/741 | Higher with NOM | OR = 6.01 | 4.2 | 8.4 | NA | NA | |
| Complications | Emile SH et al. [17] | 14/2140 | Lower with NOM | OR = 0.36 | 0.14 | 0.93 | 0.03 | I2 = 57.9% |
| Maita S et al. [18] | 21/67688 | Similar | OR = 0.64 | 0.29 | 1.39 | NA | NA | |
| Prechal et al. [19] | 5/1430 | Similar | RR = 0.98 | 0.82 | 1.18 | 0.16 | I2 = 82% | |
| Podda et al. [20] | 30/3618 | Lower with NOM | OR = 0.41 | 0.22 | 0.77 | 0.006 | I2 = 68% | |
| Poprom et al. [21] | 9/2108 | Lower with NOM |
OR = 0.39 |
0.22 | 0.7 | NA | NA | |
| Kessler et al. [22] | 5/422 | Similar | RR 1.07 | 0.26 | 4.46 | NA | NA | |
| Sakran et al. [26] | 5/1430 | Lower with NOM | RR = 0.32 | 0.24 | 0.43 | < 0.0001 | I2 = 34% | |
| Podda et al. [27] | 5/1351 | Similar | RR = 0.51 | 0.13 | 1.95 | 0.32 | I2 = 84% | |
| Findlay et al. [28] | 6/1724 | Similar | RR = 0.41 | 0.13 | 1.3 | 0.13 | I2 = 76%) | |
| Harnoss et al. [29] | 8/2551 | Lower with surgery | RR: 0.78 | 0.72 | 0.83 | < 0.0001 | I2:16.2% | |
| Sallinen et al. [31] | 5/1072 | Similar |
RD = –2.6 |
6.3 | 1.1 | 0.16 | I2 = 26% | |
| Liu et al. [33] | 6/1201 | Lower with NOM | OR = 0.31 | 0.19 | 0.49 | 0.001 | NA | |
| Ansaloni et al. [34] | 4/741 | Higher with surgery | OR = 1.9 | 1.30 | 2.85 | NA | NA | |
| Hospital stay | Maita S et al. [18] | 21/67688 | Similar | MD = 0.07 | .8 | 0.66 | NA | |
| Prechal et al. [19] | 5/1430 | Similar |
MD = 0.11 |
0.22 | 0.43 | 0.53 | I2 = 68% | |
| Podda et al. [20] | 30/3618 | Similar | MD = 0.55 | 1.49 | 0.39 | 0.25 | I2 = 99% | |
| Poprom et al. [21] | 9/2108 | Similar |
MD = 0.17 |
0.23 | 0.56 | NA | NA | |
| Sakran et al. [26] | 5/1430 | Similar |
SMD = 0.20 |
0.16 | 0.56 | 0.285 | I2 = 70.5% | |
| Podda et al. [27] | 5/1351 | Similar |
SMD = 1.54 |
0.47 | 3.54 | 0.13 | I2 = 99% | |
| Findlay et al. [28] | 6/1724 | Shorter with surgery |
MD = 0.48 |
0.10 | 0.85 | 0.01 | I2 = 52% | |
| Harnoss et al. [29] | 8/2551 | Similar | RR = 0.73 | 2.69 | 1.23 | 0.47 | I2 = 0% | |
| Sallinen et al. [31] | 5/1072 | Similar |
MD = 3.58 |
8.27 | 1.11 | 0.13 | I2 = 95% | |
| Wilms et al. [32] | 5/901 | Shorter with NOM |
OR = 0.66 |
0.44 | 0.87 | < 0.0001 | I2 = 33% |
*RR = risk ratio *OR = odds ratio *MD = mean difference *NOM = non-operative management *ES = effect estimate *CI = confidence interval
Fig. 2.
Visual representation of the qualitative outcome of the umbrella review; the longer the colored part of each bar, the higher the number of studies supporting the conclusion
Summary effect estimates for the published meta-analyses with subgroup analyses
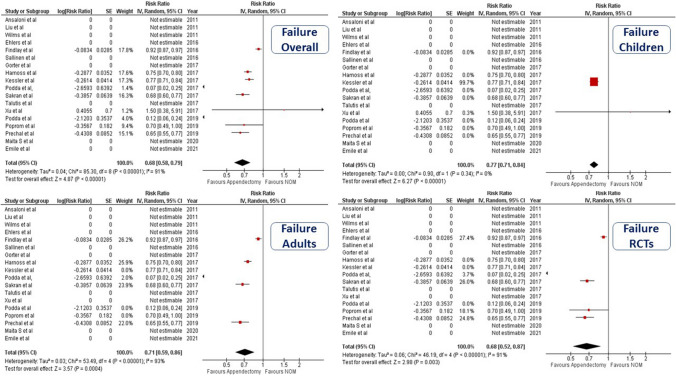
NOM was associated with higher treatment failure on pooling the effect estimates of all published meta-analyses and on subgroup analysis of meta-analyses that included children only, adults only, and RCTs only. (Fig. 3).
Fig. 3.
Forest plot illustrating the risk ratio of treatment failure along with 95% confidence interval and degree of heterogeneity (Overall analysis and subgroup analyses of children-only, adults-only, and RCTs only meta-analyses)
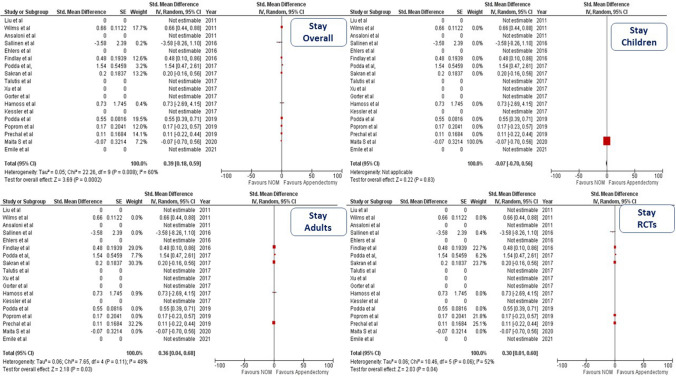
NOM was associated with lower complications on pooling the effect estimates of all published meta-analyses. However, subgroup pooling of meta-analyses including children only and RCTs only revealed similar risk of complications between NOM and appendectomy. (Fig. 4).
Fig. 4.
Forest plot illustrating the risk ratio of complications along with 95% confidence interval and degree of heterogeneity (Overall analysis and subgroup analyses of children-only, adults-only, and RCTs only meta-analyses)
NOM was associated with shorter stay in the overall analysis and subgroup analyses of adults and RCTs, however; the length of stay was similar in the subgroup analysis of children only. (Fig. 5).
Fig. 5.
Forest plot illustrating the standard mean difference in hospital stay along with 95% confidence interval and degree of heterogeneity (Overall analysis and subgroup analyses of children-only, adults-only, and RCTs only meta-analyses)
The inclusion of both children and adult population in the same study or meta-analysis may not be precise. Therefore, we reported the outcomes in terms of the population included, in addition to the overall analysis. As for treatment failure, all analyses showed a lower risk of failure with surgery, however; the degree of heterogeneity was high in the adult-only and overall analyses, whereas the children-only analysis included only one meta-analysis, and thus did not exhibit heterogeneity. While the overall analysis implied a lower risk of complications with NOM, the children-only and adult-only analyses showed similar risk. Again, there was high degree of heterogeneity in the adult-only and overall analysis, while the children-only analysis had no heterogeneity. The overall and adult-only analysis showed shorter stay with NOM, yet the children-only analysis showed similar stay. The degree of heterogeneity of hospital stay was generally moderate, and was not present in the children-only analysis (Table 5).
Table 5.
Overall and subgroup analysis of summary effect estimates of treatment failure, complications, and hospital stay
| Variable | Overall analysis | Children only | Adults only | RCTs only |
|---|---|---|---|---|
| Treatment failure | Lower with surgery (RR = 0.68, 95%CI: 0.58–0.79, p < 0.0001, I2 = 91%) | Lower with surgery (RR = 0.77, 95%CI: 0.71–0.84, p < 0.0001) | Lower with surgery (RR = 0.71, 95%CI: 0.59- 0.86, p = 0.0004, I2 = 93%) | Lower with surgery (RR = 0.68, 95%CI: 0.52–0.87, p = 0.003, I2 = 91%) |
| Complications | Lower with NOM (RR = 0.59, 95%CI: 0.43–0.81, p < 0.0001, I2 = 88%) | Similar (RR = 0.72, 95%CI: 0.36–1.44, p = 0.36, I2 = 0) | Similar (RR = 0.75, 95%CI: 0.5–1.12, p = 0.16, I2 = 92) | Similar (RR = 0.63, 95%CI: 0.33–1.21, p = 0.17, I2 = 93) |
| Hospital stay | Shorter with NOM (SMD = 0.39, 95%CI = 0.18-0.59, P = 0.0002, I2 = 60%) | Similar (SMD = 0.07, 95%CI: 0.7–0.56, p = 0.83) | Shorter with NOM (SMD = 0.36, 95%CI = 0.04–0.68, P = 0.03, I2 = 48%) | Shorter with NOM (SMD = 0.3, 95%CI = 0.01–0.6, P = 0.04, I2 = 52%) |
*RR = risk ratio *SMD = standardized mean difference *NOM = non-operative management *RCTs = randomized controlled trials
Meta-regression of factors associated with failure and recurrence after NOM
Younger age (SE = 0.198, p = 0.037), male sex (SE = 0.0001, p = 0.06), mixed patient population (SE = 0.172, p < 0.001), and longer follow-up (SE = 0.01, p = 0.07) were associated with higher failure rates, whereas higher leucocyte count (SE = 0.04, p = 0.34) was not associated with failure.
Higher leucocyte count (SE = 0.219, p = 0.019) and male sex (SE = 0.0001, p = 0.004) were associated with higher recurrence rates, whereas younger age (SE = 0.004, p = 0.136), and mixed population (SE = 0.053, p = 0.211) were not associated with recurrence.
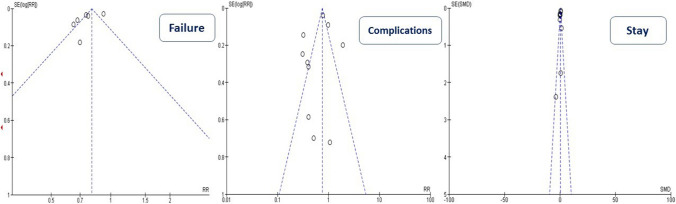
Publication bias and small-study effect
As shown in Fig. 6, there was significant publication bias in regards to “Treatment failure” (Egger’s intercept = 1.34, 95%CI: 1.91– 0.77, p = 0.001), whereas there was no publication bias in regards to the outcomes “Hospital stay” (Egger’s intercept = 0.76, 95%CI: 0.22–1.74, p = 0.11) and “Complications” (Egger’s intercept = 25, 95%CI: 1.9– 1.39, p = 0.73).
Fig. 6.
Funnel plot for assessment of publication bias in the three study outcomes
Table 6 illustrates the results of the test for excess significance for each outcome. Overall, 18 out of 31 total associations had a greater number of observed positive studies than the number of expected positive studies, yet only one association (complication, Emile et al.) had statistical evidence (p < 0.1) of excess statistical significance.
Table 6.
Test for excess significance and small-study effect in each meta-analysis
| Outcome | Systematic review | Total number of studies | Observed positive studies | Expected positive studies | P for TES | Small Study |
|---|---|---|---|---|---|---|
| Treatment failure | Prechal et al. [19] | 5 | 5 | 4.21 | 0.99 | No |
| Podda et al. [20] | 30 | 10 | 4.82 | 0.23 | No | |
| Poprom et al. [21] | 9 | 3 | 2.13 | 0.99 | No | |
| Kessler et al. [22] | 5 | 4 | 2.99 | 0.99 | Yes | |
| Sakran et al. [26] | 5 | 4 | 2.69 | 0.5 | No | |
| Podda et al. [27] | 5 | 4 | 0.33 | 0.2 | No | |
| Findlay et al. [28] | 6 | 6 | 4.09 | 0.45 | Yes | |
| Harnoss et al. [29] | 8 | 8 | 5.85 | 0.47 | Yes | |
| Ansaloni et al. [34] | 4 | 3 | 1.77 | 0.99 | No | |
| Complications | Emile SH et al. [17] | 14 | 6 | 0.39 | 0.07 | No |
| Maita S et al. [18] | 21 | 0 | 6.1 | NP | No | |
| Prechal et al. [19] | 5 | 3 | 5.45 | NP | No | |
| Podda et al. [20] | 30 | 4 | 4.82 | NP | No | |
| Poprom et al. [21] | 9 | 1 | 1.07 | NP | No | |
| Kessler et al. [22] | 5 | 0 | 7.62 | NP | No | |
| Sakran et al. [26] | 5 | 3 | 1.98 | 0.99 | Yes | |
| Findlay et al. [28] | 6 | 2 | 3.27 | NP | No | |
| Harnoss et al. [29] | 8 | 8 | 6.08 | 0.47 | No | |
| Sallinen et al. [31] | 5 | 0 | 17.8 | NP | No | |
| Liu et al. [33] | 6 | NA | NA | NA | No | |
| Ansaloni et al. [34] | 4 | 1 | 1.2 | NP | Yes | |
| Hospital stay | Maita S et al. [18] | 21 | 1 | 5 | NP | No |
| Prechal et al. [19] | 5 | 1 | 0.7 | 0.99 | No | |
| Podda et al. [20] | 30 | 3 | 0.91 | 0.61 | No | |
| Poprom et al. [21] | 9 | 1 | 0.1 | 0.99 | No | |
| Sakran et al. [26] | 5 | 1 | 1.02 | NP | No | |
| Podda et al. [27] | 5 | 2 | 6.16 | NP | No | |
| Findlay et al. [28] | 6 | 1 | 1.72 | NP | No | |
| Harnoss et al. [29] | 8 | 6 | 5.04 | NP | No | |
| Sallinen et al. [31] | 5 | 4 | 1.97 | 0.52 | No | |
| Wilms et al. [32] | 6 | 2 | 1.76 | 0.99 | No |
*TES = test for excess significance
Discussion
The present umbrella review aimed to provide an overview of the current evidence on the efficacy and safety of NOM for uncomplicated AA. Over the span of 10 years, 18 systematic reviews were published with a median of six studies per review. This observation reflects the increasing interest in NOM as an alternative to appendectomy, perhaps to avoid the adverse effects of surgery and to preserve the immune function of the appendix [35]. It was notable that PubMed/MEDLINE and Embase were the most commonly searched databases in the systematic reviews included, whereas a few reviews searched Scopus, despite being the largest abstract and citation database of peer-reviewed literature [36].
Less than half of the systematic reviews included level I evidence of RCTs only, whereas 10 systematic reviews included both RCTs and cohort studies which may not be statistically reliable. Overall, more than 50% of the systematic reviews on NOM for AA were of low quality and entailed weak evidence. Only two reviews were of high quality and two were credible and entailed highly suggestive evidence. This calls for higher quality future trials on the role of NOM of AA to avoid the shortcomings of the present trials.
NOM of AA is suggested as an alternative to appendectomy that can be similarly effective in controlling the symptoms, yet associated with less complications [37]. Therefore, the main outcomes of this umbrella review were treatment effectiveness and complications of NOM. The median rate of treatment failure of NOM was 25% and can reach up to 37.4% [19]. Almost all meta-analyses documented a higher likelihood of failure with NOM, as compared to appendectomy. The exception was a network meta-analysis [21] that reported similar odds of failure between NOM and surgery and this difference may be explained by the small number of studies included in the direct meta-analysis of failure of NOM (n = 3).
The higher likelihood of failure of NOM compared to surgery was further ascertained on subgroup analyses of meta-analyses that included pediatric population only, adult population only, and RCTs alone. This finding does make sense, because surgery effectively removes the inflamed appendix altogether, and thus eradicates the source of symptoms. On the other hand, NOM tends to resolve the acute inflammation in the appendix, however; the retained appendix may still exhibit some degree of inflammation and thus symptoms may persist or recur and moreover some complications such as appendicular mass may develop.
Having a median treatment failure rate of 25% and a median recurrence of symptoms rate of 18%, NOM may not be the optimal definitive treatment of AA. Nonetheless, NOM can be considered as a short-term treatment of AA in certain conditions where access to well-equipped operation theaters is not feasible or when the patient is not considered fit for surgery. Recently, another setting where NOM of AA may be a feasible treatment option has emerged, the COVID-19 pandemic. The role of NOM of AA during the pandemic was discussed in one meta-analysis [17] that concluded that NOM of AA may be a safe, short-term alternative to surgery in the setting of COVID-19.
As regards to the complication rates, the median complication rate of NOM was approximately 7% as compared to 10.5% after appendectomy. While some meta-analyses concluded lower complications after NOM, an equal number concluded similar odds of complications after both treatment modalities. One novel finding of this umbrella review is that while the risk ratio of complications in the overall analysis of all meta-analyses was lower with NOM, the subgroup analyses of children-only, adults-only, and RCTs-only meta-analyses found similar risk of complications. This interesting finding may be explained that the lower complication risk in the overall analysis was only marginal and thus when specifically analyzed for each population this marginal effect disappeared and the risk was similar between NOM and surgery. However, this finding should be interpreted with caution given the high level of statistical heterogeneity among the reviews included.
It should be noted that even when the complication rate of NOM is similar or lower than appendectomy, the type and severity of complications may quite differ. Complications of surgery usually involve mild morbidities such as wound-related complications (infection, seroma, dehiscence), ileus, and pelvic collection. On the other hand, complications of NOM may involve formation of appendicular mass or abscess or sometimes perforation and peritonitis which is more serious and warrants interventional or surgical management. However, it should be noted that NOM for uncomplicated AA does not statistically increase the perforation rate in adult patients [37].
Another outcome of interest is hospital stay after NOM and surgery. It may be expected that NOM is associated with longer stay than appendectomy owing to the time required for the antibiotic treatment and for frequent observation of the patient to document improvement in symptoms with NOM. However, most meta-analyses documented similar stay with both treatment methods, except one [29] that concluded longer stay with NOM and another [32] that found longer stay with surgery. Interestingly, the summary effect estimate of hospital stay was significantly shorter with NOM overall, in adult-only population and in meta-analyses of RCTs alone, whereas meta-analyses entailing children only showed similar stay. Nevertheless, it is noteworthy that the difference in hospital stay between NOM and surgery groups was only a few hours which may not be clinically important.
Despite the high degree of heterogeneity observed in the present umbrella review, some findings may aid in the clinical decision-making on AA. Given the higher failure rate of NOM, it should be reserved for the cases when appendectomy cannot be performed either due to lack of operative facilities or with patients at high risk for anesthesia and surgery. The potential advantages offered by NOM by having lower complication rate and shorter stay do not seem consistent among the published meta-analyses. Given the low heterogeneity of all outcomes in the children-only population, the conclusions on the outcome of NOM may be more reliable. With similar complication and stay, yet higher failure of NOM in children, surgery might be the optimal treatment option for children presenting with AA.
The primary findings of this umbrella review that can help advance the understanding of the role of NOM of AA can be summarized as: (1) NOM was followed by a significantly higher failure rate (median rate 25%) than appendectomy and this was consistent on subgroup analysis of children only, adults only, RCTs only; (2) Studies that entailed younger patients, more male patients, mixed population, and had longer follow-up were more likely to report higher failure/recurrence rates of NOM; (3) The complication rate of NOM (median 6.9%) was similar to surgery on analysis of meta-analyses of RCTs only to exclude selection bias; (4) Although stay of NOM was shorter than that after surgery in adults, this was not reproduced in children; (5) There was significant publication bias of the outcome “failure of NOM” implying that some negative studies reporting high failure of NOM were not published. Therefore, the actual failure rate of NOM might be higher than that reported.
Some systematic reviews included to this umbrella review may have included similar set of primary studies. However, each meta-analysis was handled and analyzed separately, knowing that some meta-analyses may have included similar set of primary studies, yet the study protocol, inclusion criteria, and statistical analysis methods of each meta-analysis would differ, and thus may lead to different conclusions. For example, using fixed-effect and random-effect models may yield different results. That is why the systematic reviews included had different weight and risk ratios as demonstrated in the forest plots, even if some included similar primary studies.
Limitations of the present study include the remarkable heterogeneity of the systematic reviews included. About half of the reviews entailed a mixed population of adults and children which did not allow for separate analysis of each subgroup. Moreover, 55% of the systematic reviews included both RCTs and observational studies in the same analysis which may compromise the accuracy of the final outcomes. That is why we conducted dedicated subgroup analyses of the pediatric population, adult population, and RCTs separately. Finally, most systematic reviews were of low quality and the level of evidence inferred was rather weak.
Conclusions
Based on the umbrella review and collective analysis of systematic reviews and meta-analyses, NOM of AA is associated with higher treatment failure, marginally lower rate of complications, and shorter hospital stay to appendectomy. The potential benefits of NOM of AA were not apparent on subgroup analysis of the meta-analyses that included pediatric population only. These results reinforce the concept that the success of the NOM approach requires careful patient selection and close observation.
Authors’ contribution
Sameh Emile designed the study. Sameh Emile, Ahmad Sakr, Mostafa Shalaby and Hossam Elfeki contributed to data collection and interpretation. Sameh Emile wrote the manuscript. Ahmad Sakr, Mostafa Shalaby and Hossam Elfeki reviewed and edited the final manuscript.
Declarations
Conflict of interest
None to be disclosed by the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sameh Hany Emile, Email: sameh200@hotmail.com.
Ahmad Sakr, Email: ahmadsakr1987@gmail.com.
Mostafa Shalaby, Email: mostafashalaby@mans.edu.eg.
Hossam Elfeki, Email: hossamelfeki@gmail.com.
References
- 1.Hospital Episode Statistics. Primary diagnosis: summary. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=202.
- 2.Appendicitis. Medscape. Available online at https://emedicine.medscape.com/article/773895-overview#a6. Accessed on May 6, 2021
- 3.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 4.Elsherbiny MW, Emile SH, Abdelnaby M, Khafagy W, Elshobaky A. Assessment of the diagnostic accuracy of alvarado scoring system combined with focused ultrasound in the diagnosis of acute appendicitis. Br J Surg. 2020;107(12):e594–e595. doi: 10.1002/bjs.12037. [DOI] [PubMed] [Google Scholar]
- 5.Al-Khayal KA, Al-Omran MA. Computed tomography and ultrasonography in the diagnosis of equivocal acute appendicitis. Meta-anal Saudi Med J. 2007;28:173–180. [PubMed] [Google Scholar]
- 6.Di Saverio S, Sibilio A, Giorgini E, Biscardi A, Villani S, Coccolini F, Smerieri N, Pisano M, Ansaloni L, Sartelli M, Catena F, Tugnoli G. The NOTA Study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260(1):109–117. doi: 10.1097/SLA.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 7.Park HC, Kim MJ, Lee BH. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg. 2017;104(13):1785–1790. doi: 10.1002/bjs.10660. [DOI] [PubMed] [Google Scholar]
- 8.Collaborative CODA, Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020;383(20):1907–1919. doi: 10.1056/NEJMoa2014320. [DOI] [PubMed] [Google Scholar]
- 9.Rushing A, Bugaev N, Jones C, Como JJ, Fox N, Cripps M, Robinson B, Velopulos C, Haut ER, Narayan M. Management of acute appendicitis in adults: a practice management guideline from the eastern association for the surgery of Trauma. J Trauma Acute Care Surg. 2019;87(1):214–224. doi: 10.1097/TA.0000000000002270. [DOI] [PubMed] [Google Scholar]
- 10.Biondi-Zoccai G, editor. Umbrella Reviews. Evidence Synthesis with Overviews of Reviews and Meta-Epidemiologic Studies. Berlin: Springer International Publishing; 2016. [Google Scholar]
- 11.Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med. 2009;6(6):e1000097. doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 15.Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–253. doi: 10.1177/1740774507079441. [DOI] [PubMed] [Google Scholar]
- 16.Tsilidis KK, Papatheodorou SI, Evangelou E, Ioannidis JP. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J Natl Cancer Inst. 2012;104(24):1867–1878. doi: 10.1093/jnci/djs437. [DOI] [PubMed] [Google Scholar]
- 17.Emile SH, Hamid HKS, Khan SM, Davis GN. Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: systematic review and meta-analysis. J Gastrointest Surg. 2021;26:1–11. doi: 10.1007/s11605-021-04988-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maita S, Andersson B, Svensson JF, Wester T. Nonoperative treatment for nonperforated appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int. 2020;36(3):261–269. doi: 10.1007/s00383-019-04610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prechal D, Damirov F, Grilli M, Ronellenfitsch U. Antibiotic therapy for acute uncomplicated appendicitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2019;34(6):963–971. doi: 10.1007/s00384-019-03296-0. [DOI] [PubMed] [Google Scholar]
- 20.Podda M, Gerardi C, Cillara N, Fearnhead N, Gomes CA, Birindelli A, Mulliri A, Davies RJ, Di Saverio S. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg. 2019;270(6):1028–1040. doi: 10.1097/SLA.0000000000003225. [DOI] [PubMed] [Google Scholar]
- 21.Poprom N, Numthavaj P, Wilasrusmee C, Rattanasiri S, Attia J, McEvoy M, Thakkinstian A. The efficacy of antibiotic treatment versus surgical treatment of uncomplicated acute appendicitis: Systematic review and network meta-analysis of randomized controlled trial. Am J Surg. 2019;218(1):192–200. doi: 10.1016/j.amjsurg.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Kessler U, Mosbahi S, Walker B, Hau EM, Cotton M, Peiry B, Berger S, Egger B. Conservative treatment versus surgery for uncomplicated appendicitis in children: a systematic review and meta-analysis. Arch Dis Child. 2017;102(12):1118–1124. doi: 10.1136/archdischild-2017-313127. [DOI] [PubMed] [Google Scholar]
- 23.Talutis SD, Drake FT. Comparative effectiveness of surgery versus antibiotics in acute appendicitis: a systematic review. J Comp Eff Res. 2017;6(5):471–482. doi: 10.2217/cer-2017-0017. [DOI] [PubMed] [Google Scholar]
- 24.Xu J, Adams S, Liu YC, Karpelowsky J. Nonoperative management in children with early acute appendicitis: a systematic review. J Pediatr Surg. 2017;52(9):1409–1415. doi: 10.1016/j.jpedsurg.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Gorter RR, The SML, Gorter-Stam MAW, Eker HH, Bakx R, van der Lee JH, Heij HA. Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg. 2017;52(8):1219–1227. doi: 10.1016/j.jpedsurg.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Sakran JV, Mylonas KS, Gryparis A, Stawicki SP, Burns CJ, Matar MM, Economopoulos KP. Operation versus antibiotics–The "appendicitis conundrum" continues: a meta-analysis. J Trauma Acute Care Surg. 2017;82(6):1129–1137. doi: 10.1097/TA.0000000000001450. [DOI] [PubMed] [Google Scholar]
- 27.Podda M, Cillara N, Di Saverio S, Lai A, Feroci F, Luridiana G, Agresta F, Vettoretto N, ACOI (Italian Society of Hospital Surgeons) Study Group on Acute Appendicitis Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15(5):303–314. doi: 10.1016/j.surge.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Findlay JM, Kafsi JE, Hammer C, Gilmour J, Gillies RS, Maynard ND. Nonoperative management of appendicitis in adults: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg. 2016;223(6):814–824.e2. doi: 10.1016/j.jamcollsurg.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Harnoss JC, Zelienka I, Probst P, Grummich K, Müller-Lantzsch C, Harnoss JM, Ulrich A, Büchler MW, Diener MK (2017) Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 265(5):889–900. doi: 10.1097/SLA.0000000000002039. [DOI] [PubMed]
- 30.Ehlers AP, Talan DA, Moran GJ, Flum DR, Davidson GH. Evidence for an antibiotics-first strategy for uncomplicated appendicitis in adults: a systematic review and gap analysis. J Am Coll Surg. 2016;222(3):309–314. doi: 10.1016/j.jamcollsurg.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, Agoritsas T, Heels-Ansdell D, Guyatt GH, Tikkinen KA. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656–667. doi: 10.1002/bjs.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD008359.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Liu K, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta-analysis. Surgery. 2011;150(4):673–683. doi: 10.1016/j.surg.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 34.Ansaloni L, Catena F, Coccolini F, Ercolani G, Gazzotti F, Pasqualini E, Pinna AD. Surgery versus conservative antibiotic treatment in acute appendicitis: a systematic review and meta-analysis of randomized controlled trials. Dig Surg. 2011;28(3):210–221. doi: 10.1159/000324595. [DOI] [PubMed] [Google Scholar]
- 35.Kooij IA, Sahami S, Meijer SL, Buskens CJ, Te Velde AA. The immunology of the vermiform appendix: a review of the literature. Clin Exp Immunol. 2016;186(1):1–9. doi: 10.1111/cei.12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andalia R, Rodríguez-Labrada R, Castells MM. Scopus: The largest database of peer-reviewed scientific literature available to underdeveloped countries. Revista Cubana de Información en Ciencias de la Salud (ACIMED) 2010;21(3):270–282. [Google Scholar]
- 37.Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. doi: 10.1186/s13017-020-00306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]