Abstract
To report the relationship of outpatient portal (OPP) use with clinical risk, area social determinants of health (SDoH), and race/ethnicity among pregnant women. Regression models predicting overall and individual portal feature use (main effects and interactions) based on key variables were specified using log files and clinical data. Overall OPP use among non-Hispanic Black women or patients who lived in lower SDoH neighborhoods were significantly less. High-risk pregnancy patients were likely to use the OPP more than those with normal-risk pregnancy. We found similar associations with individual OPP features, like Visit (scheduling) and My Record (test results). We also found significant interactive associations between race/ethnicity, clinical risk, and SDoH. Non-Hispanic Black women and those living in lower SDoH areas used OPP less than non-Hispanic White women from similar or affluent areas. More research must be conducted to learn of OPP use implications for pregnant women with specific clinical diagnoses.
Keywords: patient portals, health information technology, prenatal care, log files, social determinants of health
INTRODUCTION
Pregnancy represents a critical period of care when active health engagement can influence maternal and infant outcomes. Patient portals promote improved patient–provider communication, shared decision-making, and patient engagement.1 Depending on the type of portal, patients can access medication lists, information about recent doctor visits, immunization history, as well as securely message one’s doctor, refill prescriptions, make payments, and schedule non-urgent appointments.2 Patient portals provide patients with the means to learn about their health and participate in their health care. Higher portal use was demonstrated among pregnant women who had access to personalized health information through the portal as compared to those who had general information.3 Few studies examined patterns of portal use in obstetric (OB) patients or specific factors that can influence use among these patients.3–5
Patient portal use has been associated with improved medication adherence, disease awareness, self-management of the disease, and patient satisfaction. Their use has been associated with decreased office visits and improved preventative care.6 Although less studied, patient portals have also shown promise in the improvement of clinical outcomes. For instance, portal use was associated with improved glycemic control.7 Studies have assessed outpatient portal (OPP) use by examining number of logins8 and engagement metrics generated from log file analysis.9–12
The digital divide—the gulf between people who have and do not have access to information technologies13—may exist among patient portal users and further exacerbate health inequities across communities. OPP use was less likely among racial/ethnic minorities and individuals living in high deprivation neighborhoods—a proxy for social determinants of health (SDoH).14 Residential racial segregation is particularly high for African-Americans, perpetuating differences in socioeconomic status (SES) and health disparities.15 Use of patient portals is at the intersection of health status, race/ethnicity, and SDoH. Patient portals may be disproportionately used among specific groups of pregnant women with already better health status and greater likelihood of better health outcomes.16
The primary objective of our work is to report on the relationship of OPP use with maternal clinical risk, SDoH (as measured by an area deprivation index [ADI]), and racial/ethnic identity. We hypothesize that OPP use will be higher among women at greater risk of pregnancy-related complications, lower among women living in deprived neighborhoods, and vary by the race/ethnic identity of patients. We further explore the influence of the intersection of clinical risk, SDoH, and racial identity on OPP use at our Academic Medical Center (AMC). It is important to study how this novel health information technology is used among OB patients to identify areas of improvement to ensure that patient engagement with their health and health care is equitable.
METHODS
This study is a secondary analysis of electronic health records and audit log data on My Chart portal usage for women who received prenatal care at our AMC. The log provides a temporal sequence, through the use of time stamps, of specific actions undertaken by patients on the portal. A retrospective cohort of 17 132 pregnant women seen by the Department of Obstetrics and Gynecology (OB/GYN) and Maternal Fetal Medicine (MFM) Division at our AMC, during the study period of January 1, 2016 to January 8, 2020 were analyzed for their OPP use. This study period reflects a time of stable use post MyChart deployment across our AMC (the MyChart rollout initiated in 2011) and reflects the early stages of the COVID-19 pandemic. These patients had registered MyChart accounts through our AMC and were followed throughout their pregnancy to trace their portal use until delivery.
Ethics
Retrospective data were obtained for patient encounters from our AMC’s Information Warehouse (IW) in accordance with the Honest Broker protocol; this protocol is recognized by the Institutional Review Board (IRB) as means to use de-identified data without requiring formal IRB approval.
Study population
The study population included information on women who had (1) visited the AMC OB/GYN or MFM for prenatal care at least once; (2) were registered users of the AMC MyChart portal; (3) were at least 18 years of age. Outpatient visits for each patient are recorded using unique account identifiers, while Medical Record Numbers (MRNs) are used to link these visits to outpatient portal sessions. Portal activities for 20 788 unique pregnancy episodes from our AMC were retrieved from our Information Warehouse, out of which complete information was available on 9664 patient episodes. Episode number refers to every unique pregnancy for which care was received at the AMC. Nearly 40% of the pregnant patients seen at the AMC OB/GYN or MFM division live in urban neighborhoods wherein for women, 60% have at least a high-school degree, 31% represent a community of color, 7% are uninsured, and 18% live below the Federal Poverty Line.
My Chart patient portal
Our AMC’s MyChart (Epic Systems: Verona, Wisconsin) portal is a free, personalized, and secure electronic system that is tethered to a patient’s personal medical record. It is designed to facilitate patient-provider communication through features including electronic message exchange, appointment scheduling, availability of test results, billing, and more. Outpatient portal use was defined as the number of times a MyChart feature was used for patients with an active account. We considered an active account as any registered MyChart account during pregnancy. We calculated the frequency of use of each of the nine MyChart features and the total frequency of use of all nine MyChart features over a pregnancy episode.
Data processing
Our analytical data set was generated from the outpatient encounters and portal sessions for patients with activated portal accounts. It included information on time and duration of portal use, features accessed, user agent information, test results, and demographic information. These data were processed using the data mining technique described by Di Tosto et al10 to examine patient engagement based on patient interaction with the portal tool. Based on their prescribed methodology, the portal features were grouped into nine areas summarized in Table 1.
Table 1.
Outpatient portal features and their descriptions
| Portal feature group | Description |
|---|---|
| Messaging | Links to messaging center, letters to the patient, prescription refill option |
| Visits | List of past and upcoming visits |
| My record | List of medications, allergies; medical history, immunizations; test results and health summary; and preventive care and a summary of plan of care |
| Medical tools | Share medical records with other services; participate in research studies; and connect tracking devices |
| Billing | Account summary, payment |
| Resources | Terms and conditions; patient education; and frequently asked questions |
| Proxy | Request or renew proxy |
| Preferences | Personal and security settings; and notification preferences |
| Custom | Miscellaneous (eg, send document to personal health record) |
Data analysis
We used a negative binomial regression model specification to account for the overly dispersed portal use variables. Variables in the model were chosen based on existing literature that recommend the use of socio-demographic and clinical characteristics to examine difference in portal use among pregnant women.4,17,18 The model is offset by weeks of pregnancy because portal use could vary among patients based on the duration of prenatal care. Our fully-adjusted models include episode of pregnancy, age at first clinical encounter, Charlson Comorbidity Index (CCI), an area SDoH rank based on ZIP Code,19 pregnancy risk status (normal/high), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and Other Race/Ethnicity), insurance status (Private, Medicaid, and Others) at time of delivery, body mass index at the initial encounter (Non-obese vs Obese) and proportion of household within a tract with internet access as obtained from the American Community Survey.20 Births covered by commercial insurance were categorized into the Private category, while those covered by Medicaid were categorized into the Medicaid category, and the remaining others including self-pay were classified as Others.
The area SDoH rank is the ADI that represents rankings of neighborhoods within the AMC’s state. We converted the ADI to quantiles such that higher quantiles indicated more disadvantaged Zip Codes. The measure was retrieved from the Neighborhood Atlas.19 High-risk pregnancy included women with multiple pregnancies, diabetes, high blood pressure, genetic conditions, history of premature birth, preeclampsia, advanced maternal age, or any condition requiring high-risk care or fetal treatment. We report the estimated incidence rate ratios (IRRs) from fully adjusted models along with corresponding 95% confidence intervals (CIs). We tested the interaction between race/ethnicity, risk status, and ADI. We also performed a sensitivity analysis to see if our results differed due to the COVID-19 pandemic by excluding any pregnancies with births after December 2019.
RESULTS
Demographic information of our sample are presented in Table 2. Based on our total analytical sample, 89% had normal pregnancy-related risks, while 11% had high pregnancy-related risks. Within our sample, 77% of patients received care for only one pregnancy episode at the AMC. A majority of these episodes were from women identified as non-Hispanic Whites (67%), followed by non-Hispanic Blacks, Other Race/Ethnicity, and Hispanics. Nearly 50% of the sample resided in lesser deprived neighborhoods (Q1 and Q2), while 32% resided in areas with relatively higher deprivation (Q4 and Q5). In almost 67% of the episodes, women visited their obstetrician within their first trimester of initiation of prenatal care, and nearly 75% of the births were covered by private insurance companies. This pattern was consistent across different risk groups, as indicated in Table 2.
Table 2.
Descriptive statistics for study sample
| Patient characteristics | Total (N = 9664) | Normal risk (N = 8581) | High risk (N = 1083) |
|---|---|---|---|
| Age (mean, SD) | 30 (5) | 30 (5) | 31 (5) |
| Race/ethnicity (n, %) | |||
| Non-Hispanic White | 6462 (66.87%) | 5763 (67.16%) | 699 (64.54%) |
| Non-Hispanic Black | 1841 (19.05%) | 1648 (19.21%) | 193 (17.82%) |
| Hispanic | 314 (3.25%) | 276 (3.22%) | 38 (3.51%) |
| Other Race/Ethnicity | 1047 (10.83%) | 894 (10.42%) | 153(14.31%) |
| Episode number (n, %) | |||
| 1 | 7461 (77.20%) | 6638 (77.36%) | 823 (75.99%) |
| 2 | 1902 (19.68%) | 1675 (19.52%) | 227 (20.96%) |
| 3 | 274 (2.84%) | 243 (2.83%) | 31 (2.86%) |
| 4 | 25 (0.26%) | 24 (0.28%) | 1 (0.09%) |
| 5 | 2 (0.02%) | 1 (0.01%) | 1 (0.09%) |
| Area SDoH ranka (n, %) | |||
| Quantile 1 | 2452 (25.37%) | 2202 (25.66%) | 250 (23.08%) |
| Quantile 2 | 2178 (22.54%) | 1965 (22.90%) | 213 (19.67%) |
| Quantile 3 | 1897 (19.63%) | 1659 (19.33%) | 238 (21.98%) |
| Quantile 4 | 1851 (19.15%) | 1617 (18.84%) | 234 (21.61%) |
| Quantile 5 | 1286 (13.31%) | 1138 (13.26%) | 148 (13.67%) |
| Gestational age at initiation of care at AMC (n, %) | |||
| 1st Trimester | 6432 (66.56%) | 5752 (67.03%) | 680 (62.79%) |
| 2nd Trimester | 2517 (26.05%) | 2173 (25.33%) | 344 (31.76%) |
| 3rd Trimester | 715 (7.40 %) | 656 (7.64%) | 59 (5.45%) |
| Clinical risk (n, %) | |||
| Normal | 8581 (88.79%) | — | — |
| High | 1083 (11.21%) | — | — |
| Insurance status (n, %) | |||
| Private | 7182 (74.32%) | 6355 (74.06%) | 827 (76.36%) |
| Medicaid | 720 (7.45%) | 655 (7.63%) | 65 (6.00%) |
| Others | 1762 (18.23%) | 1571 (18.31%) | 191 (17.64%) |
| BMI (kg/m2) (n, %) | |||
| Normal (<30) | 6880 (71.19%) | 6251 (72.85%) | 629 (58.08%) |
| Obese (≥30) | 2784 (28.81%) | 2330 (27.15%) | 455 (41.92%) |
Note: High-risk pregnancy includes women with either multiple pregnancies, diabetes, high blood pressure, genetic conditions, history of premature birth, preeclampsia, advanced maternal age, or any condition requiring high-risk care or fetal treatment.
BMI: body mass index; SDoH: social determinants of health.
Higher quantile indicate more disadvantaged Zip Codes.
Among the registered users, 59 women did not access the portal during their pregnancy and were classified as non-users. We compared characteristics of users and non-users for any underlying differences. Within the non-user group, the average age (in years) was slightly lower (non-user vs user) (28.86 vs 29.97), and fewer had high pregnancy-related risk (8.47% vs 11.22%) compared to the users. The percentage of non-Hispanic White was smaller (44.07% vs 66.98%), but the percentage of non-Hispanic Black (38.98% vs 18.96%), and Other Race/Ethnicity (13.56% vs 10.82%) was higher in the non-user group compared to the OPP users. The percentage of Hispanics did not vary much between the two groups (3.39% vs 3.25%).
We also compared the racial distributions between our study sample and the overall pregnant population seen at the AMC, regardless of portal account. Our study sample had greater proportions of women identified as non-Hispanic Whites (study sample vs overall population at AMC) (66.87% vs 58.36%) and Other Race/Ethnicity (10.83% vs 8.92%), and fewer proportions of non-Hispanic Blacks (19.05% vs 24.65%) and Hispanics (3.25% vs 8.06%), as compared to the overall population. We also compared the racial distribution of our sample with a national study sample assessing portal use.21 Based on these reported values our study had fewer women from the non-Hispanic White (study sample vs national distribution) (66.87% vs 71.3%) and Hispanic (3.25% vs 9.1%) race /ethnicity, and more from non-Hispanic Blacks (19.05% vs 10.7%) and Other Race/Ethnicity groups (10.83% vs 8.8%).22,23
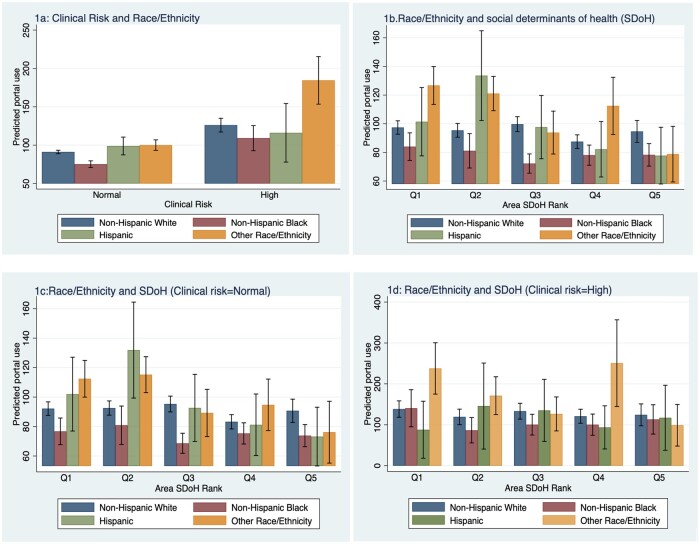
Estimated IRRs for overall portal use and individual features are presented in Table 3. We found that non-Hispanic Black women used the portal (IRR: 0.833; 95% CI: 0.789–0.880) significantly less than non-Hispanic White women (Figure 1A). Women with high-risk pregnancies used the portal 45% more (IRR: 1.446; 95% CI: 1.360–1.537) than those with normal pregnancy risks. Area SDoH conditions also played a significant role in portal use. Though no differences were reported in portal use for those living in quantile five, women living in quantile four used the portal significantly less, up to 10% less, than those living in quantile 1 (IRR 0.906; CI: 0.852–0.963 (Q4)). Also, there was a significant trend in portal use based on area SDoH (p < .001 based on a trend test, results not shown), which indicated that portal use increased as deprivation decreased.
Table 3.
Rate ratios for outpatient portal use outcomes and key study variables
| Outcome (N = 9664) | Overall portal use | Messaging | Visits | My record | Medical tools | Billing | Proxy | Preferences | Custom |
|---|---|---|---|---|---|---|---|---|---|
| Episode number | 1.119*** | 0.740*** | 1.290*** | 1.073*** | 1.018 | 1.084** | 1.230*** | 0.884** | 1.085 |
| (1.078–1.162) | (0.705–0.777) | (1.226–1.357) | (1.036–1.111) | (0.934–1.110) | (1.031–1.140) | (1.097–1.378) | (0.822–0.952) | (0.995–1.183) | |
| Charlson co-morbidity index | 1.030* | 1.083*** | 1.025 | 1.052*** | 0.963 | 0.960* | 1.167** | 0.973 | 1.016 |
| (1.000–1.061) | (1.041–1.127) | (0.985–1.065) | (1.023–1.081) | (0.900–1.031) | (0.924–0.998) | (1.050–1.297) | (0.920–1.029) | (0.951–1.085) | |
| SDoH ranking (Reference: Quantile 1) | |||||||||
| Quantile 2 | 0.994 | 1.039 | 0.979 | 0.999 | 1.214** | 0.986 | 0.882 | 0.947 | 1.04 |
| (0.941–1.051) | (0.966–1.117) | (0.909–1.054) | (0.948–1.052) | (1.070–1.378) | (0.916–1.060) | (0.742–1.047) | (0.851–1.052) | (0.913–1.185) | |
| Quantile 3 | 0.964 | 1.01 | 0.955 | 0.971 | 1.102 | 0.953 | 1.028 | 0.886* | 0.921 |
| (0.910–1.022) | (0.934–1.091) | (0.883–1.033) | (0.919–1.026) | (0.961–1.263) | (0.882–1.030) | (0.860–1.229) | (0.792–0.992) | (0.803–1.055) | |
| Quantile 4 | 0.906** | 0.903* | 0.884** | 0.945 | 1.086 | 0.905* | 0.853 | 0.833** | 0.944 |
| (0.852–0.963) | (0.832–0.980) | (0.814–0.961) | (0.892–1.002) | (0.939–1.257) | (0.834–0.983) | (0.708–1.027) | (0.739–0.939) | (0.818–1.088) | |
| Quantile 5 | 0.937 | 0.907 | 0.941 | 0.986 | 1.097 | 0.806*** | 1.01 | 0.907 | 0.841 |
| (0.864–1.017) | (0.812–1.013) | (0.842–1.050) | (0.913–1.065) | (0.900–1.336) | (0.722–0.898) | (0.787–1.297) | (0.776–1.060) | (0.698–1.013) | |
| Race (Reference: Non-Hispanic White) | |||||||||
| Non-Hispanic Black | 0.833*** | 0.778*** | 0.902** | 0.823*** | 0.762*** | 0.636*** | 0.791** | 1.02 | 0.96 |
| (0.789–0.880) | (0.722–0.837) | (0.838–0.972) | (0.782–0.867) | (0.669–0.867) | (0.591–0.685) | (0.667–0.938) | (0.920–1.132) | (0.845–1.089) | |
| Hispanic | 1.051 | 0.827** | 1.173* | 0.969 | 1.123 | 1.117 | 0.849 | 1.162 | 1.267 |
| (0.943–1.171) | (0.716–0.955) | (1.013–1.357) | (0.875–1.073) | (0.881–1.432) | (0.967–1.290) | (0.607–1.187) | (0.948–1.424) | (0.992–1.617) | |
| Other Race/Ethnicity | 1.192*** | 1.046 | 1.205*** | 1.162*** | 1.091 | 1.369*** | 1.145 | 1.283*** | 1.329*** |
| Risk (Reference: Normal) | 1.446*** | 1.322*** | 1.546*** | 1.453*** | 1.308*** | 1.262*** | 1.714*** | 1.046 | 1.236** |
| (1.360–1.537) | (1.220–1.432) | (1.424–1.678) | (1.372–1.538) | (1.143–1.497) | (1.164–1.369) | (1.420–2.068) | (0.931–1.175) | (1.075–1.422) | |
| Age at first gestational encounter | 0.997 | 1.008** | 0.993* | 0.997 | 1.001 | 1.005 | 1 | 0.987** | 0.960*** |
| (0.993–1.001) | (1.003–1.014) | (0.988–0.999) | (0.993–1.001) | (0.991–1.011) | (0.999–1.010) | (0.987–1.014) | (0.979–0.995) | (0.951–0.970) | |
| BMI (Reference: Non-obese (body mass index <30 kg/m2) | 1.095*** | 1.052 | 1.124*** | 1.092*** | 1.029 | 1.034 | 1.251** | 1.005 | 1.049 |
| (1.048–1.143) | (0.992–1.114) | (1.060–1.192) | (1.048–1.137) | (0.930–1.138) | (0.975–1.096) | (1.094–1.431) | (0.925–1.092) | (0.948–1.161) | |
| Insurance status (Reference: Private) | |||||||||
| Medicaid | 0.652*** | 0.579*** | 0.691*** | 0.744*** | 0.679*** | 0.298*** | 0.724** | 0.991 | 0.819* |
| (0.603–0.705) | (0.521–0.644) | (0.622–0.767) | (0.692–0.801) | (0.564–0.818) | (0.267–0.333) | (0.569–0.920) | (0.855–1.148) | (0.683–0.982) | |
| Other | 0.690*** | 0.674*** | 0.693*** | 0.774*** | 0.681*** | 0.429*** | 0.781** | 0.982 | 0.934 |
| (0.653–0.729) | (0.626–0.725) | (0.643–0.746) | (0.735–0.816) | (0.598–0.776) | (0.399–0.461) | (0.656–0.929) | (0.885–1.089) | (0.823–1.059) | |
| Internet access | 1.271 | 0.968 | 1.076 | 1.554* | 2.032 | 2.017** | 0.799 | 0.734 | 0.415* |
| (0.875–1.848) | (0.581–1.611) | (0.648–1.787) | (1.094–2.208) | (0.819–5.044) | (1.230–3.307) | (0.262–2.434) | (0.358–1.505) | (0.178–0.969) |
Note: Incidence rate ratio (95% confidence intervals). p < 0.1;
p < 0.05;
p < 0.001.
BMI: body mass index; SDoH: social determinants of health.
Figure 1.
Interactive plots for overall outpatient portal use by race, area social determinants of health, and clinical risk for pregnant women. (A) Interaction plot for risk and race/ethnicity. (B) Interaction plot for race/ethnicity and area SDoH rank (Q1: best and Q5: worst). (C) Interaction plot for race/ethnicity and area SDoH rank when clinical risk is normal. (D) Interaction plot for race/ethnicity and area SDoH rank when clinical risk is high.
Based on counts of individual features, the Visit feature, which involved scheduling information, was used most, followed by My Record, which helped patients manage their medication and test results (results not shown). Similar to our results for overall portal use, we found that these top features were used less among non-Hispanic Black women in comparison to non-Hispanic White women. Women living in deprived neighborhoods used these features less than women living in least deprived neighborhoods. We observed similar patterns between race and several other features. As the episode number increased the use of Messaging and Preferences features decreased, while other features increased. No activity was observed for the Resources feature across any patients because the external functions accessed with this feature are not captured by the AMC log data.
Two and three-way interactions between race/ethnicity, clinical risk, and area SDoH were also examined. We found statistically significant interactions displayed in Figure 1 (see Supplementary Table S1 for results from our interaction models). As risk of complications increased, women from the Other Race/Ethnicity group used the portal significantly more than non-Hispanic White women with similar risks (IRR: 1.430; 95% CI: 1.033–1.978), shown in Figure 1A. Women from the Other Race/Ethnicity group, who lived in the least deprived areas used the portal more than non-Hispanic White women living in similar neighborhoods. With increased levels of area SDoH deprivation, however, portal use among women from Other Race/Ethnicity reduced significantly (Figure 1B). This pattern was consistent among women with normal pregnancy-related complications (Figure 1C). No significant interactions were seen between race/ethnicity and ADI within the high-pregnancy related risk group (Figure 1D). Irrespective of risk and ADI, portal use was consistently lower among non-Hispanic Black women compared to women from Other Race/Ethnicity. Similar patterns were observed for the billing feature; portal use was likely to reduce with deprivation (results not shown).
In regard to our sensitivity analysis, we found the pre-COVID estimates to be similar to those from our main analysis (see Supplementary Table S2 for details).
DISCUSSION
We found non-Hispanic Black women to be among the lowest portal users for pre-natal care and this pattern was consistent across different area SDoH and risk levels. Our results suggest that interaction of neighborhood and race impacts portal use. Neighborhood deprivation and race have been significantly associated in the past, with greater proportion of minority population residing in more deprived areas.24–26 The triad between environment (including clinical and social determinants), individual, and behavioral factors, as explained by the Engagement Capacity Framework, can explain patient engagement outcomes such as portal use.27 Moreover, the lack of environmental and individual factors such as health literacy, health technology literacy, and language barriers impact health care utilization in these communities.28
Our results substantiate the persistence of racial inequity within our society that disproportionately impacts the non-Hispanic Black sub-group. Additionally, our results indicate that neighborhood factors impact portal use, especially those living in deprived areas. Though our results do not indicate significant differences in portal use among those living in the most deprived neighborhood in comparison to the least deprived one, the rate ratios suggest a decreased usage with deprivation and further examination with newer samples may be warranted. In addition to individual barriers, structural limitations such as lack of connectivity can negatively impact the outreach of technology and health care. Higher use of technology can pose a risk for intervention generated inequalities by disproportionately supporting more advantaged individuals.29
The concentration of infrastructure development in urban areas and disinvestment plans have increased the poverty rates in deprived neighborhoods.30 A recent study showed that though gentrification efforts have uplifted few neighborhoods, many reported higher levels of poverty.31 The number of high-poverty census tracts in a major city in United States increased from 26 to 50 in 2018 along with an increase in population from 88 812 to 166 530. These area-based expansions further exacerbate health disparities that the affected communities experience.32–34
Prior studies on portal use in low-income populations found disparities by race and SES in OPP use, similar to ours, where higher use was associated with individuals of White race and being insured.32 We found that area deprivation was associated with lower OPP use. Previous evidence suggests that better access to broadband internet14 and smartphones with data35,36 can help bridge health disparities,37–39 including the use of patient portals. Qualitative research suggests that a one-time introduction to OPP is inadequate, especially among low-income pregnant women. Moreover, these women have also expressed a desire for consistent patient education and support that is tailored to their OB histories.18
We observed greater OPP use among women at higher risk of pregnancy complications. Results from our interaction outcomes elucidate the role of socio-demographic variables on portal use. The decision to deploy health information on tools such as portals must incorporate clinical as well as non-clinical factors. A woman of non-Hispanic Black race group, living in a derived neighborhood is less likely to access her health information from the portal which may restrict her health engagement if alternate strategies are not presented.
Prior work suggests that use of personal health records was greater among those with chronic conditions.40 Evidence from a study on portal use and glycemic control in prenatal care suggested that secure messaging is higher among those with suboptimal glucose control.5 However, more research is needed to explore the implications of portal use for health outcomes among women with high-risk conditions and whether there are differential effects based on types of clinical diagnoses presented at pregnancy.33 Since grounded in the reality that many of our patients have multiple social identities that influence ways they experience health, screening for clinical and reporting SDoH hurdles must be promulgated. Current programs that target health disparity are designed at the individual level and thus are less effective in bringing changes at the population level. Rather population-based interventions such as providing technical training and assistance programs should be considered.29
Limitations
Our analysis was focused on OB patients in a single health system using an OPP from one particular vendor, thereby limiting the generalizability of our findings. ADI is a proxy for SDoH factors and may not completely capture individual SDoH factors. Lastly, our sample may have under representation of women from extremely deprived neighborhoods because of the previously designed SDoH measure used and because of the uneven distribution of women from such neighborhoods.
CONCLUSION
OB patients interact with the healthcare system for nearly nine to ten months. HIT tools like patient portals can facilitate these interactions. Future studies should further explore how patient portal use based on race/ethnicity, area SDoH, and clinical risk can have differential effects on patient experiences and health outcomes.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
PS, PJ, EM, and NF contributed to the conceptualization and drafting of the analysis. EM, PS, and NF performed data collection and data analysis.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors wish to thank (blinded for peer review) from our AMC Information Warehouse for their assistance with this project.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to information that could compromise the privacy of study subjects.
REFERENCES
- 1. Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc 2013; 20 (3): 519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.What is a patient portal? | HealthIT.gov. https://www.healthit.gov/faq/what-patient-portal Accessed March 26, 2021.
- 3. Shaw E, Howard M, Chan D, et al. Access to web-based personalized antenatal health records for pregnant women: a randomized controlled trial. J Obstet Gynaecol Can 2008; 30 (1): 38–43. [DOI] [PubMed] [Google Scholar]
- 4. Ukoha EP, Feinglass J, Yee LM. Disparities in electronic patient portal use in prenatal care: retrospective cohort study. J Med Internet Res 2019; 21 (9): e14445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holder K, Ukoha E, Feinglass J, et al. Relationship between patient portal utilization and glycemic control outcomes during pregnancy. J Diabetes Sci Technol 2021; 15 (4): 970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res 2015; 17 (2): e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Graetz I, Huang J, Muelly ER, et al. Association of mobile patient portal access with diabetes medication adherence and glycemic levels among adults with diabetes. JAMA Netw Open 2020; 3 (2): e1921429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lau M, Campbell H, Tang T, et al. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes 2014; 38 (1): 17–21. [DOI] [PubMed] [Google Scholar]
- 9. Sieverink F, Kelders S, Poel M, et al. Opening the black box of electronic health: collecting, analyzing, and interpreting log data. JMIR Res Protoc 2017; 6 (8): e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Di Tosto G, McAlearney AS, Fareed N, et al. Metrics for outpatient portal use based on log file analysis: algorithm development. J Med Internet Res 2020; 22 (6): e16849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tsai R, Bell EJ, Woo H, et al. How patients use a patient portal: an institutional case study of demographics and usage patterns. Appl Clin Inform 2019; 10 (1): 96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jones JB, Weiner JP, Shah NR, et al. The wired patient: patterns of electronic patient portal use among patients with cardiac disease or diabetes. J Med Internet Res 2015; 17 (2): e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Dijk J, Hacker K. The digital divide as a complex and dynamic phenomenon. Inf Soc 2003; 19 (4): 315–26. [Google Scholar]
- 14. Perzynski AT, Roach MJ, Shick S, et al. Patient portals and broadband internet inequality. J Am Med Inform Assoc 2017; 24 (5): 927–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001; 116 (5): 404–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brewer LC, Fortuna KL, Jones C, et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth 2020; 8 (1): e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Powell KR. Patient-perceived facilitators of and barriers to electronic portal use: a systematic review. Comput Inform Nurs 2017; 35 (11): 565–73. [DOI] [PubMed] [Google Scholar]
- 18. Kim J, Mathews H, Cortright LM, et al. Factors affecting patient portal use among low-income pregnant women: mixed-methods pilot study. JMIR Form Res 2018; 2 (1): e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med 2018; 378 (26): 2456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Computer and Internet Use. https://www.census.gov/topics/population/computer-internet.html Accessed August 3, 2021.
- 21. Winston S. Health information national trends survey (hints.gov). Med Ref Serv Q 2021; 40 (2): 215–23. [DOI] [PubMed] [Google Scholar]
- 22. Anthony DL, Campos-Castillo C, Lim PS. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018; 37 (12): 1948–54. [DOI] [PubMed] [Google Scholar]
- 23. El-Toukhy S, Méndez A, Collins S, Pérez-Stable EJ. Barriers to patient portal access and use: evidence from the health information national trends survey. J Am Board Fam Med 2020; 33 (6): 953–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sharkey P. Spatial segmentation and the black middle class. AJS 2014; 119 (4): 903–54. [DOI] [PubMed] [Google Scholar]
- 25. Darden JT, Bagaka’s JG, Ji SJ. Racial residential segregation and the concentration of low-and high-income households in the 45 largest US metropolitan areas. J Dev Soc 1997; 13 (2): 171–94. [PubMed] [Google Scholar]
- 26. Massey DS, Condran GA, Denton NA. The effect of residential segregation on black social and economic well-being. Social Forces 1987; 66 (1): 29. [Google Scholar]
- 27. Sieck CJ, Walker DM, Retchin S, et al. The patient engagement capacity model: what factors determine a patient’s ability to engage? NEJM Catalyst 2019; 5 (2).
- 28. Douthit N, Kiv S, Dwolatzky T, et al. Exposing some important barriers to health care access in the rural USA. Public Health 2015; 129 (6): 611–20. [DOI] [PubMed] [Google Scholar]
- 29. Grossman LV, Masterson Creber RM, Benda NC, et al. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc 2019; 26 (8-9): 855–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Turner MA, Gourevitch R. How Neighborhoods Affect the Social and Economic Mobility of Their Residents. Washington: US Partnership on Mobility from Poverty.
- 31.The Geography of High-Poverty Neighborhoods—The View from Ohio. Economic Innovation Group. https://eig.org/news/the-geography-of-high-poverty-neighborhoods-the-view-from-ohio Accessed July 27, 2021.
- 32. Ancker JS, Barrón Y, Rockoff ML, et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011; 26 (10): 1117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Veinot TC, Mitchell H, Ancker JS. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc 2018; 25 (8): 1080–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.U.S. Census Bureau. Population Estimates. 2017. https://www.census.gov/programs-surveys/popest.html Accessed January 24, 2020.
- 35.Cell phone ownership hits 91% of adults | Pew Research Center. https://www.pewresearch.org/fact-tank/2013/06/06/cell-phone-ownership-hits-91-of-adults/ Accessed February 23, 2021.
- 36.10% of Americans don’t use the internet | Pew Research Center. https://www.pewresearch.org/fact-tank/2019/04/22/some-americans-dont-use-the-internet-who-are-they/ Accessed January 24, 2020.
- 37. Fareed N, Swoboda CM, Jonnalagadda P, et al. Persistent digital divide in health-related internet use among cancer survivors: findings from the Health Information National Trends Survey, 2003-2018. J Cancer Surviv 2021; 15 (1): 87–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chou W-YS, Liu B, Post S, et al. Health-related Internet use among cancer survivors: data from the Health Information National Trends Survey, 2003-2008. J Cancer Surviv 2011; 5 (3): 263–70. [DOI] [PubMed] [Google Scholar]
- 39. Prestin A, Vieux SN, Chou W-YS. Is online health activity alive and well or flatlining? findings from 10 years of the health information national trends survey. J Health Commun 2015; 20 (7): 790–8. [DOI] [PubMed] [Google Scholar]
- 40. Archer N, Fevrier-Thomas U, Lokker C, et al. Personal health records: a scoping review. J Am Med Inform Assoc 2011; 18 (4): 515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to information that could compromise the privacy of study subjects.