ABSTRACT
Kidney transplantation (KT) is an increasingly utilized treatment for end-stage kidney disease. Hypertension either as a cause of kidney disease or as a complication of chronic kidney disease is the most frequently encountered comorbidity of KT patients. Hence, the management of hypertension in KT patients is crucial to prolong patient and graft survival. Ambulatory blood pressure monitoring (ABPM) appeared as a promising technique that has superiority over office and home blood pressure (BP) monitoring to correctly diagnose and manage hypertension. A recent meta-analysis by Pisano et al. including 42 studies with 4115 participants provided strong data for the comparison of ABPM with office BP monitoring in KT patients. In addition to the current literature knowledge, the findings of Pisano et al. filled the long-awaited evidence gap to suggest ABPM as a first-line BP monitoring technique for KT patients. Despite its disadvantages, such as patient discomfort, cost–effectiveness and limited availability, ABPM has crucial advantages in the management of hypertension including the detection of abnormal circadian BP patterns, the assessment of effects of physical activity and short-term variability of BP, and the exclusion of masked and white-coat hypertension.
Keywords: ambulatory blood pressure monitoring, hypertension, kidney transplantation, office blood pressure measurement
Pisano et al. conducted a meta-analysis to ascertain the clinical benefit of 24-h ambulatory blood pressure monitoring (ABPM) compared with office blood pressure (BP) recordings for the management of hypertension in kidney transplantation (KT) patients. Pisano et al. reviewed 42 studies including 4115 participants, and concluded that ABPM is more effective for the detection of uncontrolled hypertension, and masked and white-coat hypertension in KT patients than office BP measurements, with a discordance rate of 44% between the office and ABPM measurements for the classification of KT patients with either controlled or uncontrolled hypertensive [1]. The findings of Pisano et al. made us question the current approach in diagnosing and monitoring hypertension of KT patients according to current transplant guidelines [2].
The number of patients with end-stage kidney disease (ESKD) is on the rise due to the ageing population with an increasing prevalence of cardiovascular and metabolic comorbidities. KT is currently the preferred treatment for ESKD, providing longer survival and increased quality of life [3, 4]. In 2019, more than 80 000 KTs were performed, corresponding to only about 10% of the transplant candidates [5]. With the increasing number of KT patients, accurate management of KT patients and their risk factorsis of the utmost importance to prolong graft and patient survival.
Hypertension is a common condition found among KT patients either as a cause of kidney disease or as a complication of chronic kidney disease (CKD) [6]. The prevalence of hypertension increases up to 86% in haemodialysis patients due to the deterioration of kidney function [7]. Hypertension control forms the cornerstone of the management of KT patients as better management of BP is strongly associated with longer term graft and patient survival [6, 8]. Therefore, accurate monitoring of BP for the diagnosis and treatment of hypertension in KT patients is crucial for clinical decisions.
Currently, the available BP monitoring techniques are office (clinic) BP measurement, ABPM and home (self) blood pressure monitoring (HBPM). ABPM provides multiple measurements of BP over 24 h by taking readings every 10–30 min without any interruption via more ergonomic devices thanks to technological improvements [9]. Besides the determination of average BP level, ABPM can provide more information about the diurnal BP variation and short-term variability of BP. By accumulating knowledge gained from ABPM, it was seen that hypertension is not a stable entity but a complex issue in regulating arterial BP with short-/medium-/long-term BP variability. BP variability and its important clinical implications have been extensively discussed in several articles [10–13]. Circadian BP patterns change such that non-dippers and reverse dippers are more common among CKD patients compared with the general population, and are associated with significant renal and cardiovascular risks [14]. Hence, ABPM has a significant advantage over other BP measurement techniques for the evaluation of daily life’s effect and BP variability with the estimation of circadian BP patterns (nocturnal hypertension, dipping/non-dipping) by 24 h follow-up of BP changes [10, 15].
Pisano et al. [1] showed that abnormal circadian BP patterns are common among KT patients by pointing to a 54% average prevalence of non-dipping BP and a higher proportion of patients with a reverse dipping BP compared with the general population. Pisano et al. also found that the proportion of non-dippers reduced with the time after transplantation and observed a higher fall of BP during sleep as time passed. Several studies have pointed out that early morning pressure surges and non-dipping BP patterns are risk factors for cardiovascular events, so KT patients are under more cardiovascular risk, especially immediately after the transplantation [16–18]. Thus, ABPM could be more helpful for KT patients to detect abnormal circadian BP patterns (non-dippers and reverse dippers).
Chronotherapy is another crucial benefit of ABPM over other BP measurement techniques. Accumulating evidence indicates that antihypertensive medications could be more effective when they are taken at a certain time to target non-dipper BP and nocturnal hypertension [19]. The effective coverage of morning BP surges and abnormal circadian BP patterns could be ensured with the help of chronotherapy. Chronotherapy by the individualization of treatment based on patients’ circadian BP profiles can be best provided by the utilization of ABPM.
White-coat hypertension and masked hypertension are also common in KT patients [14, 20]. In the study by Pisano et al. [1], the average prevalence of masked hypertension and white-coat hypertension was reported as 26 and 10%, respectively [1]. ABPM also helps to detect patients with resistant, white-coat and masked hypertension and provides better data to follow-up renal and cardiovascular risks compared with office BP measurements [8, 21]. A previous systemic review of Pisano et al., including 22 studies with 2078 participants, concluded that ABPM is superior to assess target organ damage compared with office BP monitoring [22].
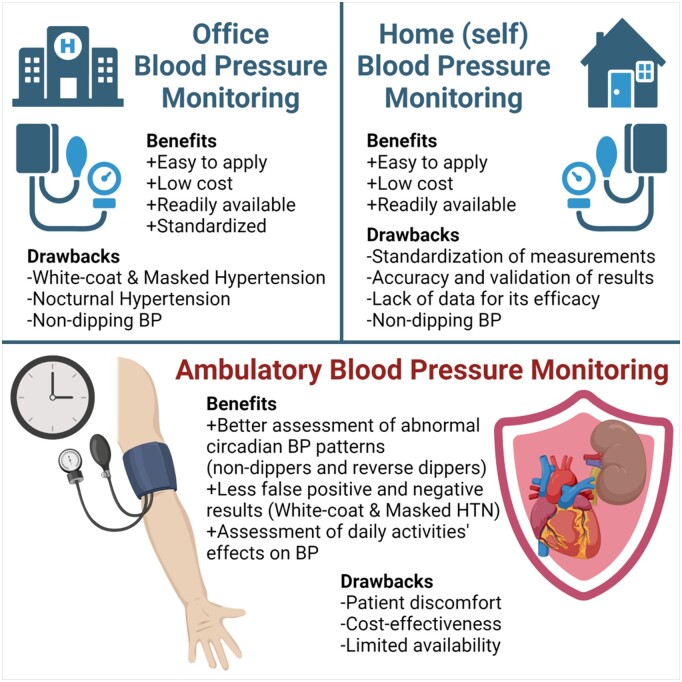
Even though the current literature and the study by Pisano et al. provide beneficial data for comparing ABPM and office BP measurements, there is a lack of data for comparing HBPM and ABPM. The main limitation of the study by Pisano et al. is that only 4 out of 42 studies provided data for the comparison of ABPM and home BP measurements. HBPM seems more readily available, comfortable and cheaper than ABPM; however, validation and accuracy of HBPM for reproducibility of measurements are important issues (Figure 1). Also, patients could not measure their BP while sleeping, so HBPM also has weakness for the determination of circadian BP patterns. On the other hand, a recent review on HBPM suggested that home BP measurements could promote patients’ adherence and lead to better BP control than office BP measurements [23]. Because ABPM has some disadvantages, such as patient discomfort, practicality, cost–effectiveness and limited availability, HBPM could be an important alternative to ABPM [15]. Future studies should be conducted to compare HBPM with ABPM and office BP monitoring.
FIGURE 1:
Benefits and drawbacks of BP monitoring techniques. HTN, hypertension.
While there is enough evidence to suggest ABPM as a first-line modality for the monitoring of BP in the general population, if available, ABPM should be utilized in the management of hypertension for all KT patients as they can benefit significantly more than the general population. As KT patients are generally followed by comprehensive transplantation teams in well-equipped specialized centres, the availability and cost of ABPM should not be an important issue for the utilization of ABPM in this population. Considering the aforementioned superiority of ABPM over office BP monitoring, clinical decisions for the management of hypertension in KT patients must be based on BP data from ABPM. With the current literature and the recent findings of the meta-analysis by Pisano et al. [1], what else do we need to change current guidelines for suggesting ABPM as the first-line modality in the management of hypertension in KT patients?
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
FUNDING
This study was not funded by any grant.
ETHICAL APPROVAL
This article does not contain any studies with human participants or animals performed by any of the authors.
DATA AVAILABILITY STATEMENT
No new data were generated or analysed in support of this research.
ACKNOWLEDGEMENTS
M.K. gratefully acknowledges the use of services and facilities of the Koc University Research Center for Translational Medicine (KUTTAM), funded by the Presidency of Turkey, Presidency of Strategy and Budget. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Presidency of Strategy and Budget
CONFLICT OF INTEREST STATEMENT
M.K. is a Member of the CKJ Editorial Board.
Contributor Information
Atalay Demiray, Department of Medicine, Koc University School of Medicine, Istanbul, Turkey.
Mehmet Kanbay, Department of Medicine, Division of Nephrology, Koc University School of Medicine, Istanbul, Turkey.
REFERENCES
- 1. Pisano AM, D’Arrigo G, Bolignano D et al. Assessment of hypertension in kidney transplantation by ambulatory blood pressure monitoring: a systematic review and meta-analysis. Clin Kidney J 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheung AK, Chang TI, Cushman WC et al. Executive summary of the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int 2021; 99: 559–569 [DOI] [PubMed] [Google Scholar]
- 3. Lorent M, Foucher Y, Kerleau K et al. ; EKiTE Consortium. The EKiTE network (epidemiology in kidney transplantation - a European validated database): an initiative epidemiological and translational European collaborative research. BMC Nephrol 2019; 20: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tonelli M, Wiebe N, Knoll G et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 2011; 11: 2093–2109 [DOI] [PubMed] [Google Scholar]
- 5. WHO-ONT Global Observatory on Donation and Transplantation. http://www.transplant-observatory.org/uses-of-dataquoting-data/
- 6. Sarafidis PA, Persu A, Agarwal R et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH). Nephrol Dial Transplant 2017; 32: 620–640 [DOI] [PubMed] [Google Scholar]
- 7. Agarwal R, Nissenson AR, Batlle D et al. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med 2003; 115: 291–297 [DOI] [PubMed] [Google Scholar]
- 8. Parati G, Ochoa JE, Bilo G et al. ; European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association–European Dialysis Transplantation Association (ERA-EDTA). Hypertension in chronic kidney disease part 1: out-of-office blood pressure monitoring: methods, thresholds, and patterns. Hypertension 2016; 67: 1093–1101 [DOI] [PubMed] [Google Scholar]
- 9. Kanbay M, Turkmen K, Ecder T et al. Ambulatory blood pressure monitoring: from old concepts to novel insights. Int Urol Nephrol 2012; 44: 173–182 [DOI] [PubMed] [Google Scholar]
- 10. Parati G, Ochoa JE, Bilo G et al. ; European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis Transplantation Association (ERA-EDTA). Hypertension in chronic kidney disease part 2: role of ambulatory and home blood pressure monitoring for assessing alterations in blood pressure variability and blood pressure profiles. Hypertension 2016; 67: 1102–1110 [DOI] [PubMed] [Google Scholar]
- 11. Zhang Y, Li JJ, Wang AJ et al. Effects of intensive blood pressure control on mortality and cardiorenal function in chronic kidney disease patients. Ren Fail 2021; 43: 811–820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Çağlı K, Turak O, Canpolat U et al. Association of serum uric acid level with blood pressure variability in newly diagnosed essential hypertension. J Clin Hypertens 2015; 17: 929–935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kanbay M, Turgut F, Uyar ME et al. Causes and mechanisms of nondipping hypertension. Clin Exp Hypertens 2008; 30: 585–597 [DOI] [PubMed] [Google Scholar]
- 14. Mzingeli L, Jones E, Barday Z et al. The relevance of performing 24-hour ambulatory blood pressure and pulse wave analysis in kidney transplant recipients. Clin Nephrol 2021; 95: 240–246 [DOI] [PubMed] [Google Scholar]
- 15. Solak Y, Kario K, Covic A et al. Clinical value of ambulatory blood pressure: Is it time to recommend for all patients with hypertension? Clin Exp Nephrol 2016; 20: 14–22 [DOI] [PubMed] [Google Scholar]
- 16. Turak O, Afsar B, Ozcan F et al. Relationship between elevated morning blood pressure surge, uric acid, and cardiovascular outcomes in hypertensive patients. J Clin Hypertens 2014; 16: 530–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hermida RC, Mojon A, Fernandez JR et al. Elevated asleep blood pressure and non-dipper 24h patterning best predict risk for heart failure that can be averted by bedtime hypertension chronotherapy: A review of the published literature. Chronobiol Int 2021; 1–20. 10.1080/07420528.2021.1939367 [DOI] [PubMed] [Google Scholar]
- 18. Lo L, Hung SWS, Chan SSW et al. Prognostic value of nocturnal blood pressure dipping on cardiovascular outcomes in Chinese patients with hypertension in primary care. J Clin Hypertens (Greenwich) 2021; 23: 1291–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carriazo S, Ramos AM, Sanz AB et al. Chronodisruption: a poorly recognized feature of CKD. Toxins (Basel) 2020; 12: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Loutradis C, Sarafidis P, Marinaki S et al. Role of hypertension in kidney transplant recipients. J Hum Hypertens 2021 [DOI] [PubMed] [Google Scholar]
- 21. Halimi JM, Ortiz A, Sarafidis PA et al. Hypertension in kidney transplantation: a consensus statement of the ‘hypertension and the kidney’ working group of the European Society of Hypertension. J Hypertens 2021; 39: 1513–1521 [DOI] [PubMed] [Google Scholar]
- 22. Pisano A, Mallamaci F, DArrigo G et al. Blood pressure monitoring in kidney transplantation: a systematic review on hypertension and target organ damage. Nephrol Dial Transplant 2021; 36: 1326–1346. doi: 10.1093/ndt/gfab076 [DOI] [PubMed] [Google Scholar]
- 23. Mengden T, Weisser B. Monitoring of treatment for arterial hypertension-the role of office, home, and 24 h ambulatory blood pressure measurement. Dtsch Arztebl Int 2021; 118: 473–478 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.