Abstract
Economic evaluation of health-related projects requires principles and methods to address the various trade-offs that need to be made between costs and benefits, across sectors and social objectives, and over time. Existing guidelines for economic evaluation in low- and middle-income countries embed implicit assumptions about expected changes in the marginal cost per unit of health produced by the healthcare sector, the consumption value of health and the appropriate discount rates for health and consumption. Separating these evaluation parameters out requires estimates for each country over time, which have hitherto been unavailable. We present a conceptual economic evaluation framework that aims to clarify the distinct roles of these different evaluation parameters in evaluating a health-related project. Estimates for each are obtained for each country and in each time period, based on available empirical evidence. Where existing estimates are not available, for future values of the marginal cost per unit of health produced by the healthcare sector, new estimates are obtained following a practical method for obtaining projected values. The framework is applied to a simple, hypothetical, illustrative example, and the results from our preferred approach are compared against those obtained from other approaches informed by the assumptions implicit within existing guidelines. This exposes the consequences of applying such assumptions, which are not supported by available evidence, in terms of potentially sub-optimal decisions. In general, we find that applying existing guidelines as done in conventional practice likely underestimates the value of health-related projects on account of not allowing for expected growth in the marginal cost per unit of health produced by the healthcare sector.
Keywords: Cost-effectiveness analysis, benefit–cost analysis, global health, economic growth, low-income countries, middle-income countries
Key messages.
Economic evaluation of health-related projects requires principles and methods to address the various trade-offs that need to be made between costs and benefits, across sectors and social objectives, and over time.
Conventional practice in health economics is not always clear on how to analyse these trade-offs and often embeds implicit assumptions about expected changes in resource constraints and societal preferences within the discount rates used to evaluate projects.
One reason for this is that separating these arguments out requires a range of parameter estimates for countries over time that have hitherto been unavailable.
This paper marshals available evidence to inform estimates of evaluation parameters by country and over time to produce a flexible evaluation framework that can inform decision-makers in a transparent manner.
Even with a highly stylized simple health-related project, different assumptions about evaluation parameters for each country over time lead to important differences in results for some countries.
Users of guidelines should think carefully about the appropriateness of implicit assumptions in the context of their own country. Writers of future guidelines should seek to improve the transparency regarding assumptions about evaluation parameters.
Introduction
Economic evaluation of a health-related project (such as a healthcare intervention or a health technology or programme of care for a particular indication) can be used to support decision-making in low- and middle-income countries (LMICs) (Drummond et al., 2015). It is most commonly operationalized through the application of some form of cost-effectiveness analysis (CEA) (WHO, 2003; 2019; Wilkinson et al., 2016) or, less commonly, benefit–cost analysis (BCA) (Robinson et al., 2019b).
The effectiveness of a health-related project is typically denominated in terms of its impact on a generic measure of health such as a disability-adjusted life year (DALY) or a quality-adjusted life year, but other objectives such as consumption, which comprises both the consumption value of health effects and the consumption of non-health goods and services, may also be considered. The adopted perspective of the analysis determines the appropriate scope of which costs are included (Sanders et al., 2016).
Economic evaluation allows for the calculation of the net benefit of a project, which represents its effect net of the opportunity cost (the value of the best alternative use of the resources required for the project). This depends not only on the choice of objective and perspective but also on the assumed source of the resources. Where the healthcare sector budget available for a project is exogenous to the decision, the resources are obtained from elsewhere within the budget, and the marginal cost per unit of health produced by the healthcare sector ( ) may be used to calculate the health opportunity cost (Woods et al., 2016; Ochalek et al., 2018). This can be used to quantify the net health benefit, but for comparisons beyond health, the net health benefit may need to be multiplied by the consumption value of health (
) may be used to calculate the health opportunity cost (Woods et al., 2016; Ochalek et al., 2018). This can be used to quantify the net health benefit, but for comparisons beyond health, the net health benefit may need to be multiplied by the consumption value of health ( ) in order to compare with the consumption of non-health goods and services (Brouwer et al., 2018).
) in order to compare with the consumption of non-health goods and services (Brouwer et al., 2018).
Both  and
and  parameters are therefore vital to economic evaluation of this kind, with
parameters are therefore vital to economic evaluation of this kind, with  used to calculate health opportunity costs and
used to calculate health opportunity costs and  used to convert health into consumption value, but the separate role for these is not explicitly acknowledged within existing guidelines. Instead, CEA typically refers to a cost-effectiveness threshold against which the incremental cost-effectiveness ratio (ICER) of a project is compared. In guidelines, the basis for a cost-effectiveness threshold is not always explicitly given and could reflect
used to convert health into consumption value, but the separate role for these is not explicitly acknowledged within existing guidelines. Instead, CEA typically refers to a cost-effectiveness threshold against which the incremental cost-effectiveness ratio (ICER) of a project is compared. In guidelines, the basis for a cost-effectiveness threshold is not always explicitly given and could reflect  or
or  or it may be arbitrary. Historically, an arbitrary cost-effectiveness threshold range of one to three times gross domestic product (GDP) per capita was advised by the World Health Organization (WHO), and its use is still observed in practice in LMICs (Bertram et al., 2016; Leech et al., 2018). More recent guidelines either do not state the basis of the cost-effectiveness threshold (WHO, 2003; 2019) or recommend the use of
or it may be arbitrary. Historically, an arbitrary cost-effectiveness threshold range of one to three times gross domestic product (GDP) per capita was advised by the World Health Organization (WHO), and its use is still observed in practice in LMICs (Bertram et al., 2016; Leech et al., 2018). More recent guidelines either do not state the basis of the cost-effectiveness threshold (WHO, 2003; 2019) or recommend the use of  (Wilkinson et al., 2016). While guidelines for CEA in LMICs recommend that the choice of cost-effectiveness threshold depends upon the country to which the analysis relates, there is no consideration of how it is likely to evolve over time in each country (resulting in an implicit assumption of constant growth or remaining constant). In contrast, the guideline for BCA in LMICs recommends that health is valued using
(Wilkinson et al., 2016). While guidelines for CEA in LMICs recommend that the choice of cost-effectiveness threshold depends upon the country to which the analysis relates, there is no consideration of how it is likely to evolve over time in each country (resulting in an implicit assumption of constant growth or remaining constant). In contrast, the guideline for BCA in LMICs recommends that health is valued using  , with guidance on how this may change over time but acknowledge no role no for
, with guidance on how this may change over time but acknowledge no role no for  (Robinson et al., 2019b).
(Robinson et al., 2019b).
Also vital is accounting for the timing of costs and effects. This is conventionally done using discount rates where impacts of a project in future years are downweighted compared to the present, often motivated by the literature on positive time preference. In particular, guidelines have often adopted a constant discount rate of 3% per annum for all countries, which is applied to all costs and effects (Weinstein et al., 1996; WHO, 2003; Sanders et al., 2016; Wilkinson et al., 2016; Robinson et al., 2019b). Differential, but still constant, discounting has also been recommended, where costs are discounted using a higher discount rate relative to health effects (WHO, 2019), which can be justified on the basis of expected growth in  or
or  (Claxton et al., 2011). However, recommendations around discount rates are a source of much controversy, with the choice of 3% argued to be inappropriate for fast-growing LMICs in particular and arguably lack coherence with relevant theory and empirics more generally (Haacker et al., 2020).
(Claxton et al., 2011). However, recommendations around discount rates are a source of much controversy, with the choice of 3% argued to be inappropriate for fast-growing LMICs in particular and arguably lack coherence with relevant theory and empirics more generally (Haacker et al., 2020).
Taken together, we argue that following existing guidelines for economic evaluation in LMICs will result in sub-optimal decisions. This is particularly important as resources available for healthcare are especially limited in LMICs compared to high-income countries, and projected economic growth can outstrip more mature economies with implications for expected changes in the marginal cost per unit of health produced by the healthcare sector, expected changes in the consumption value of health, and discount rates. What is lacking is 3-fold: clarity regarding the separate role for key parameters  and
and  , guidance as to plausible assumptions about how these parameter values might evolve over time for a given country, and discount rates that reflect these and other country-specific factors.
, guidance as to plausible assumptions about how these parameter values might evolve over time for a given country, and discount rates that reflect these and other country-specific factors.
The paper is structured as follows. The ‘Methods’ section contains two parts. The first part outlines a conceptual economic evaluation framework that aims to clarify the distinct roles of different evaluation parameters in evaluating a project based on Claxton et al. (2019). The second part describes a comparison of alternative evaluation approaches (i.e. first, our preferred approach, which uses parameters based on the conceptual economic evaluation framework, and then approaches parameters implied by the existing guidelines both where the objective is health and where it is consumption) applied to a simple hypothetical project. Correspondingly, the ‘Results’ section first provides estimates for each of these parameters [the marginal cost per unit of health produced by the healthcare sector ( ), the consumption value of health (
), the consumption value of health ( ), the discount rate for health (
), the discount rate for health ( ) and the discount rate for consumption value (
) and the discount rate for consumption value ( )], for each country and in each time period, based on available empirical evidence for both the preferred approach and other approaches inspired by the assumptions from guidelines. Where existing estimates are not available for future values of the marginal cost per unit of health produced by the healthcare sector (
)], for each country and in each time period, based on available empirical evidence for both the preferred approach and other approaches inspired by the assumptions from guidelines. Where existing estimates are not available for future values of the marginal cost per unit of health produced by the healthcare sector ( ), new estimates are obtained following a practical method for obtaining projected values of this parameter for each country over time. The remainder of this paper demonstrates an application of this framework to calculate the estimated net benefit of a hypothetical project across LMICs. This serves to illustrate the sub-optimal consequences of alternative assumptions about key parameters that result from adhering to recommendations from existing guidelines. All parameter values used within this application are provided in the Supplementary material.
), new estimates are obtained following a practical method for obtaining projected values of this parameter for each country over time. The remainder of this paper demonstrates an application of this framework to calculate the estimated net benefit of a hypothetical project across LMICs. This serves to illustrate the sub-optimal consequences of alternative assumptions about key parameters that result from adhering to recommendations from existing guidelines. All parameter values used within this application are provided in the Supplementary material.
Methods
This section first sets out the economic evaluation framework that identifies key parameters for which country- and time-specific estimates are required and data sources for these are identified. This informs our preferred approach. Second, we describe a method to evaluate existing guidelines in order to expose implicit assumptions about these parameters that are embedded within existing guidance through enabling a like-for-like comparison of the approaches implied within current guidelines with our preferred approach. As part of this, a method is outlined for comparing the results from our preferred assumptions to those in existing guidelines both when the objective is to improve health and when it is to improve consumption value.
Framework of evaluation
Where the objective is to improve health, evaluation focuses on the health achieved by the project net of health opportunity costs. In a given year, for a given country, this is calculated as follows:
 |
(1) |
For each country,  , in year
, in year  ,
,  is the total additional cost of the project,
is the total additional cost of the project,  is the total DALYs averted by the project and
is the total DALYs averted by the project and  is the marginal cost per unit of health produced by the healthcare sector. By specifying all of these parameter values as for a given country and year, it is indicated that each may potentially vary by country as well as over time. In Equation (1), all parameters are undiscounted. From the estimated time profile of net health effects,
is the marginal cost per unit of health produced by the healthcare sector. By specifying all of these parameter values as for a given country and year, it is indicated that each may potentially vary by country as well as over time. In Equation (1), all parameters are undiscounted. From the estimated time profile of net health effects,  , a net present value can be calculated for each country using the discount rate for health (
, a net present value can be calculated for each country using the discount rate for health ( ):
):
 |
(2) |
 and
and  represent the first and final years within the time horizon of the economic evaluation, respectively. The discount rate itself is allowed to vary for each country and over time.
represent the first and final years within the time horizon of the economic evaluation, respectively. The discount rate itself is allowed to vary for each country and over time.
Where the objective is to increase consumption, for each time period, for a given country, it is necessary to evaluate the consumption value of the net health benefits of the project:1
 |
(3) |
 |
(4) |
For each country,  , in year
, in year  ,
,  is the consumption value of a DALY. A net present value can be calculated for each country from the time profile of equivalent consumption effects using the discount rate for consumption (
is the consumption value of a DALY. A net present value can be calculated for each country from the time profile of equivalent consumption effects using the discount rate for consumption ( ).
).
Marginal cost per unit of health produced by the healthcare sector, 
We use estimates of cost per DALY averted from 2015 that reflect  based on two similar studies (Ochalek et al., 2018; Ochalek and Lomas, 2020). There is a considerable variation exhibited among LMICs, ranging between $59 and $17 058 per DALY averted (2017 USD) in Guinea-Bissau and Costa Rica, respectively (Ochalek et al., 2018).2 However, no published estimates of future values of
based on two similar studies (Ochalek et al., 2018; Ochalek and Lomas, 2020). There is a considerable variation exhibited among LMICs, ranging between $59 and $17 058 per DALY averted (2017 USD) in Guinea-Bissau and Costa Rica, respectively (Ochalek et al., 2018).2 However, no published estimates of future values of  are available. Changes in
are available. Changes in  over time depend on many factors, which makes future values difficult to anticipate (Paulden et al., 2017). This paper offers a practical method for obtaining future projections of
over time depend on many factors, which makes future values difficult to anticipate (Paulden et al., 2017). This paper offers a practical method for obtaining future projections of  by analysing the relationship3 between estimates of
by analysing the relationship3 between estimates of  and GDP per capita as well as total fertility rate, for both of which projected values exist (Dieleman et al., 2017), across countries, and sub-groups of countries.4 Using this relationship, we are able to project annual estimates of
and GDP per capita as well as total fertility rate, for both of which projected values exist (Dieleman et al., 2017), across countries, and sub-groups of countries.4 Using this relationship, we are able to project annual estimates of  for 97 LMICs from 2015 to 2040. Employing these values avoids relying on simplifying assumptions such as
for 97 LMICs from 2015 to 2040. Employing these values avoids relying on simplifying assumptions such as  remaining constant over time or growing at a constant rate (see Supplementary Appendix A).
remaining constant over time or growing at a constant rate (see Supplementary Appendix A).
Consumption value of health, 
Although not the only way to obtain a consumption value of health, here, we use recently published estimates of the value of a statistical life (VSL) in 2015, which are available for 95 LMICs based on extrapolation of an estimate for USA using gross national income per capita (Robinson et al., 2019a). For application to net health effects denominated in DALYs, it is advised to calculate the value of a statistical life year (VSLY), which can then form the basis of estimates of  (Robinson et al., 2019a). Following Robinson et al. (2019a),
(Robinson et al., 2019a). Following Robinson et al. (2019a),  is calculated by dividing VSL by the conditional life expectancy at the age equal to half of the life expectancy at birth to obtain VSLY.5
is calculated by dividing VSL by the conditional life expectancy at the age equal to half of the life expectancy at birth to obtain VSLY.5
There is a related literature that analyses the income elasticity of  , which can be drawn upon to provide estimates of
, which can be drawn upon to provide estimates of  for 2015–40, given the availability of projected estimates of GDP per capita (Hammitt and Robinson, 2011; Viscusi and Masterman, 2017; Masterman and Viscusi, 2018; Robinson et al., 2019). In this paper, following Claxton et al. (2019a), we consider two different values for the income elasticity of
for 2015–40, given the availability of projected estimates of GDP per capita (Hammitt and Robinson, 2011; Viscusi and Masterman, 2017; Masterman and Viscusi, 2018; Robinson et al., 2019). In this paper, following Claxton et al. (2019a), we consider two different values for the income elasticity of  : 1 and 1.5 (with our preferred approach using an elasticity of 1). An elasticity of 1 reflects that
: 1 and 1.5 (with our preferred approach using an elasticity of 1). An elasticity of 1 reflects that  increases by the same proportion as GDP per capita, while an elasticity >1 reflects that health is a luxury good, with
increases by the same proportion as GDP per capita, while an elasticity >1 reflects that health is a luxury good, with  increasing by a greater proportion than the increase in GDP per capita.
increasing by a greater proportion than the increase in GDP per capita.
Discount rate for health, 
Where the objective is to improve health, Paulden and Claxton (2012) argue that net health should be discounted at a rate,  , that reflects the interest rate faced by the payer,
, that reflects the interest rate faced by the payer,  , minus the growth rate of
, minus the growth rate of  ,
,  :
:
 |
(5) |
The growth rate of  ,
,  , can be derived from estimates of
, can be derived from estimates of  . Without estimates for
. Without estimates for  , we are required to make an assumption to obtain a suitable proxy based on the compound annual growth rate (CAGR) of GDP per capita from the projected estimates of GDP per capita (
, we are required to make an assumption to obtain a suitable proxy based on the compound annual growth rate (CAGR) of GDP per capita from the projected estimates of GDP per capita ( ). The rationale for this is that as
). The rationale for this is that as  , where
, where  and
and  , we are effectively proxying
, we are effectively proxying  with
with  , which is the mirror image of the assumption made by the Council of Economic Advisers in 2017 who proxy
, which is the mirror image of the assumption made by the Council of Economic Advisers in 2017 who proxy  with
with  (Council of Economic Advisers, 2017).
(Council of Economic Advisers, 2017).
Discount rate for consumption value, 
Where the objective is to improve consumption, the discount rate,  , reflects the social time preference rate for consumption and can be based on the Ramsey Rule that comprises a pure time preference rate,
, reflects the social time preference rate for consumption and can be based on the Ramsey Rule that comprises a pure time preference rate,  , and a wealth effect that is the product of the growth rate of future consumption (
, and a wealth effect that is the product of the growth rate of future consumption ( ) and the weight that ought to be attached to it (
) and the weight that ought to be attached to it ( ),
),  :
:
 |
(6) |
There is a consensus that pure time preference rate,  , is most appropriately considered to be small or zero for social decision-making (Drupp et al., 2018). The wealth effect requires consideration of the appropriate basis and value for
, is most appropriately considered to be small or zero for social decision-making (Drupp et al., 2018). The wealth effect requires consideration of the appropriate basis and value for  . In the context of social decision-making, empirical estimates of social inequality aversion have been used to infer values for
. In the context of social decision-making, empirical estimates of social inequality aversion have been used to infer values for  , which suggest
, which suggest  (Groom and Maddison, 2019). According to this basis for
(Groom and Maddison, 2019). According to this basis for  , discount rates should be higher in countries with higher expected economic growth, and therefore, the commonplace usage of 3% per annum may be too low for fast-growing LMICs (Haacker et al., 2020). Our preferred approach employs a value of
, discount rates should be higher in countries with higher expected economic growth, and therefore, the commonplace usage of 3% per annum may be too low for fast-growing LMICs (Haacker et al., 2020). Our preferred approach employs a value of  equal to 0 and
equal to 0 and  equal to 1.
equal to 1.
Evaluating existing guidelines for economic evaluation
To illustrate the importance of different assumptions and estimates when applying this flexible evaluation framework to a project, we compare our preferred approach to other approaches inspired by existing guidelines. The comparison is undertaken for two different types of analysis: one where the objective is to improve health and the other to improve consumption.
A simple hypothetical health-related project
For all countries analysed, we assume that a project affects 10% of each country’s population in 2015. The additional costs and DALYs averted per affected individual are $25 (2017 USD) prices and 0.1, respectively, each year for the period 2015–40. It is assumed that the project occurs throughout the 2015–40 period or not at all. This example is highly stylized with its ICER being invariant to the discount rate so long as the same discount rate is used for healthcare costs and health gains ($250 per DALY averted, which is similar to the median value of  among low- and lower-middle-income countries of $307 per DALY averted).
among low- and lower-middle-income countries of $307 per DALY averted).
Enabling like-for-like comparison across guidelines
When the objective is to improve health, our framework of evaluation requires values for  in order to calculate the time profile of net health effects [Equation (1)] for each country and
in order to calculate the time profile of net health effects [Equation (1)] for each country and  to convert this into a net present value [Equation (2)]. When the objective is to improve consumption, our framework instead requires values for both
to convert this into a net present value [Equation (2)]. When the objective is to improve consumption, our framework instead requires values for both  and
and  in order to calculate the time profile of net consumption effects [Equation (3)] and
in order to calculate the time profile of net consumption effects [Equation (3)] and  to convert this into a net present value [Equation (4)].
to convert this into a net present value [Equation (4)].
This differs from what is conventionally done in economic evaluation, which means that a like-for-like comparison of the estimates of net health and net consumption benefit that result from the application of existing guidelines for economic evaluation in LMICs requires inferring assumptions implied about the growth rates of  or
or  , which can be revealed from the recommended discount rates using Claxton et al.’s (2011) framework (although it is important to note that the resulting inferred assumptions do not necessarily reflect the intention of the authors).
, which can be revealed from the recommended discount rates using Claxton et al.’s (2011) framework (although it is important to note that the resulting inferred assumptions do not necessarily reflect the intention of the authors).
Claxton et al. (2011) argue that the cost-effectiveness threshold most appropriately represents  when the objective is to improve health, given an exogenous budget constraint. Their framework shows that, in this context, the discount rate for healthcare costs is given by
when the objective is to improve health, given an exogenous budget constraint. Their framework shows that, in this context, the discount rate for healthcare costs is given by  . This implies that a choice of differential discounting in guidelines with a lower discount rate for health indicates an expectation of growth in
. This implies that a choice of differential discounting in guidelines with a lower discount rate for health indicates an expectation of growth in  , while applying the same discount rate to health and healthcare reveals an implicit assumption that
, while applying the same discount rate to health and healthcare reveals an implicit assumption that  will remain constant in real terms.
will remain constant in real terms.
Using this method, we were able to parameterize two evaluation approaches with the objective of improving health based on the iDSI (Wilkinson et al., 2016) ‘iDSI_H’ and WHO immunization (WHO, 2019b) ‘WHOi_H’ guidelines to compare against our preferred approach ‘Preferred_H’.
Where the objective is to increase consumption, there can be up to three separate discount rates for consumption ( ), health gains (
), health gains ( ), and healthcare costs (
), and healthcare costs ( ), which are characterized in existing guidelines as uniform across countries and constant over time. The discount rate for health gains is found to be
), which are characterized in existing guidelines as uniform across countries and constant over time. The discount rate for health gains is found to be  , which indicates that if
, which indicates that if  is expected to grow, then relatively more weight should be given to future health than should future consumption. If the budget is considered exogenous, the discount rate for healthcare costs is given by
is expected to grow, then relatively more weight should be given to future health than should future consumption. If the budget is considered exogenous, the discount rate for healthcare costs is given by  , which implies that in this context
, which implies that in this context  . Again, a difference between the recommended discount rates for health and healthcare costs indicates an implicit assumption about the growth of
. Again, a difference between the recommended discount rates for health and healthcare costs indicates an implicit assumption about the growth of  . In this context, the assumption regarding the growth rate of
. In this context, the assumption regarding the growth rate of  is revealed by differences between the discount rate for consumption and the other recommended discount rates. If the budget is considered endogenous, then the discount rates for healthcare costs and consumption are the same (
is revealed by differences between the discount rate for consumption and the other recommended discount rates. If the budget is considered endogenous, then the discount rates for healthcare costs and consumption are the same ( ) and a lower discount rate for health implies an expectation of growth in
) and a lower discount rate for health implies an expectation of growth in  .
.
Using this method, we are able to parameterize three evaluation approaches with the objective of improving consumption based on the WHO Generalized CEA (GCEA) (WHO, 2003) ‘WHO_C’, WHO immunization (WHO, 2019) ‘WHOi_C’ and BCA (Robinson et al., 2019b) ‘BCA_C’ guidelines to compare against our preferred approach ‘Preferred_C’.
Results
This section first presents the results of parameterizing the different evaluation approaches, our preferred approach and the approaches inspired by existing guidelines and then presents the results of an application of each to the economic evaluation of a hypothetical project.
Parameterizing the evaluation approaches
Preferred approach
Estimates for  are based on Dieleman et al. (2017) and enable calculation of values for evaluation parameters
are based on Dieleman et al. (2017) and enable calculation of values for evaluation parameters  ,
,  ,
,  and
and  for 95 LMICs. These results are provided in full in Supplementary Appendix B and are summarized below for two countries chosen for illustrative purposes: Bangladesh and Yemen.
for 95 LMICs. These results are provided in full in Supplementary Appendix B and are summarized below for two countries chosen for illustrative purposes: Bangladesh and Yemen.
In 2015, both countries are lower-middle-income countries that are eligible for GAVI support. Bangladesh is estimated to have a  in 2015 of $142 per DALY compared to $241 per DALY for Yemen (2017 USD) (Ochalek et al., 2018). The estimated
in 2015 of $142 per DALY compared to $241 per DALY for Yemen (2017 USD) (Ochalek et al., 2018). The estimated  in 2015 is $1272 for Bangladesh and $1090 for Yemen (2017 USD) (Robinson et al., 2019a).
in 2015 is $1272 for Bangladesh and $1090 for Yemen (2017 USD) (Robinson et al., 2019a).
Analysis of the two countries over time reveals some differences. Both countries are projected to have decreases in total fertility rate with a CAGR of −0.8% in Bangladesh and −1.9% in Yemen. The major difference between these two countries lies in the forecasted trajectories of economic growth where Bangladesh is expected to grow at a CAGR of 4.6% over the period 2015–40, while Yemen is expected to experience a CAGR of −0.2% (Yemen’s annual growth rate is negative until 2020 and positive thereafter).
In our preferred approach with the objective of improving health, ‘Preferred_H’, these projected changes lead to differences in the trajectories of the evaluation parameters  and
and  over time. In Yemen,
over time. In Yemen,  is projected to initially fall and then rise, with a CAGR over the whole period of 0.7% (
is projected to initially fall and then rise, with a CAGR over the whole period of 0.7% ( for Yemen in 2040 is projected to be $286 per DALY in 2017 USD). In contrast, in Bangladesh,
for Yemen in 2040 is projected to be $286 per DALY in 2017 USD). In contrast, in Bangladesh,  is projected to increase throughout with a CAGR of 4.7% (
is projected to increase throughout with a CAGR of 4.7% ( for Bangladesh in 2040 is projected to be $443 per DALY in 2017 USD). Negative values for
for Bangladesh in 2040 is projected to be $443 per DALY in 2017 USD). Negative values for  are estimated for Bangladesh and Yemen throughout, with the magnitude falling between 2016 (−0.6% for Bangladesh and −1.7% for Yemen) and 2040 (−0.1% for Bangladesh and −0.9% for Yemen).
are estimated for Bangladesh and Yemen throughout, with the magnitude falling between 2016 (−0.6% for Bangladesh and −1.7% for Yemen) and 2040 (−0.1% for Bangladesh and −0.9% for Yemen).
The differences in projected changes over time also impact upon the trajectories of  and
and  , which are required for our preferred approach with the objective of improving consumption ‘Preferred_C’. With the assumptions of the income elasticity of
, which are required for our preferred approach with the objective of improving consumption ‘Preferred_C’. With the assumptions of the income elasticity of  and
and  equal to 1, these trajectories exactly mirror that projected for economic growth. This means that
equal to 1, these trajectories exactly mirror that projected for economic growth. This means that  grows with a CAGR of 4.6% in Bangladesh (
grows with a CAGR of 4.6% in Bangladesh ( for Bangladesh in 2040 is projected to be $3898 in 2017 USD) but falls with a CAGR of −0.2% in Yemen (
for Bangladesh in 2040 is projected to be $3898 in 2017 USD) but falls with a CAGR of −0.2% in Yemen ( for Yemen in 2040 is projected to be $1033 in 2017 USD). Yemen has negative values for
for Yemen in 2040 is projected to be $1033 in 2017 USD). Yemen has negative values for  throughout the period analysed falling in magnitude from −11.7% in 2016 to −0.2% in 2040. In contrast, Bangladesh has positive values throughout falling from 6.1% in 2016 to 4.6% in 2040.
throughout the period analysed falling in magnitude from −11.7% in 2016 to −0.2% in 2040. In contrast, Bangladesh has positive values throughout falling from 6.1% in 2016 to 4.6% in 2040.
Assumptions implicit within existing guidelines
‘iDSI_H’
The results from this section are summarized in Tables 1 and 2 with more detail given below. The iDSI reference case (Wilkinson et al., 2016) recommends that an ICER is calculated using a discount rate of 3% for both healthcare costs and health gains and that this is compared to a cost-effectiveness threshold that reflects  . This closely relates to our evaluation framework when the objective is to maximize health. The use of the same discount rate for healthcare costs and health gains therefore implies an assumption of no growth in
. This closely relates to our evaluation framework when the objective is to maximize health. The use of the same discount rate for healthcare costs and health gains therefore implies an assumption of no growth in  (i.e.
(i.e.  and
and  ).
).
Table 1.
Approaches to analysis where the objective is to improve health
| Analysis | Values for 
|
Values for 
|
|---|---|---|
| iDSI_H |

|
3% |
| WHOi_H |
|
0% |
| Preferred_H |

|
|
Table 2.
Approaches to analysis where the objective is to improve consumptiona
| Analysis | Values for 
|
Values for 
|
Values for 
|
|---|---|---|---|
| WHO_C |

|

|
3% |
| WHOi_C |
|
|
3% |
| BCA_C |

|
 (income elasticity = 1.5)
(income elasticity = 1.5) |
3% |
| Preferred_C |

|
 (income elasticity = 1)
(income elasticity = 1) |

|
Our preferred approach (‘Preferred_C’) takes assumptions for the income elasticity of  and
and  from the ‘conservative scenario’ in Claxton et al. (2019). We present the results of an additional three analyses using different assumptions suggested in Claxton et al. (2019) in Supplementary Appendix C.
from the ‘conservative scenario’ in Claxton et al. (2019). We present the results of an additional three analyses using different assumptions suggested in Claxton et al. (2019) in Supplementary Appendix C.
‘WHO_C’
The WHO GCEA guide (WHO, 2003) recommends a similar approach, with discount rates of 3% for both healthcare costs and health gains, but argues that the objective ought to be consumption and that the budget for health should not be considered exogenous. In this context, the lack of divergence between the discount rates for healthcare costs and health gains implies an assumption of  remaining constant in real terms (i.e.
remaining constant in real terms (i.e.  and
and  ). We construct an analysis where the objective is to improve consumption but allow for consideration of an exogenous budget constraint in order to fit within our framework.
). We construct an analysis where the objective is to improve consumption but allow for consideration of an exogenous budget constraint in order to fit within our framework.
‘WHOi_H’ and ‘WHOi_C’
More recently, WHO has released separate guidelines for evaluating immunizations (WHO, 2019). These guidelines differ in two important ways for our purposes. First, the guidelines refer to the use of a cost-effectiveness threshold but do not state the appropriate basis for this. Second, they propose differential discounting with a discount rate for health gains equal to 0% with discount rates of 3% for healthcare costs and consumption ( ,
,  and
and  ). The use of differential discounting in this way implies an assumption of 3% annual growth in both
). The use of differential discounting in this way implies an assumption of 3% annual growth in both  and
and  (i.e.
(i.e.  and
and  ) when viewed through the lens of Claxton et al.’s (2011) framework.
) when viewed through the lens of Claxton et al.’s (2011) framework.
‘BCA_C’
Finally, the BCA guidelines (Robinson et al., 2019a) differ from other guidelines in that its recommendations are not based on the conventional practice of CEA. Instead, it is recommended that health gains are converted into their consumption value and that  is adjusted for expected growth in GDP per capita using an income elasticity of the consumption value of health of 1.5. No role is acknowledged for an exogenous budget constraint, but this is required for our framework. As such we assume the same principle of projecting
is adjusted for expected growth in GDP per capita using an income elasticity of the consumption value of health of 1.5. No role is acknowledged for an exogenous budget constraint, but this is required for our framework. As such we assume the same principle of projecting  where possible. These guidelines recommend a constant discount rate of 3% for all countries (i.e.
where possible. These guidelines recommend a constant discount rate of 3% for all countries (i.e.  ).
).
Comparing the results from the evaluation approaches when applied to the simple hypothetical health-related project
The proportion of countries where a positive net present value of net health benefits is estimated varies according to the evaluation approach that is taken. This is summarized in Table 3.
Table 3.
Proportion of countries where a positive net health benefit is estimated by income category by evaluation approach
| Proportion of countries where a positive net health benefit is estimated | |||
|---|---|---|---|
| Groups of countries | iDSI_H (%) | WHOi_H (%) | Preferred_H (%) |
| Low-income | 25 | 42 | 42 |
| Lower-middle-income | 81 | 92 | 89 |
| Upper-middle-income | 100 | 100 | 100 |
| LMICs (all) | 74 | 82 | 81 |
Positive net health benefits are generated in all upper-middle-income countries and in most lower-middle-income countries and negative net health benefits in the majority of low-income countries regardless of approach. This is because  tends to be lower in low-income countries than in lower-middle-income countries, which are in turn lower than in upper-middle-income countries.
tends to be lower in low-income countries than in lower-middle-income countries, which are in turn lower than in upper-middle-income countries.
The observed differences in the sign of the net health benefit across approaches summarized in Table 3 are driven by the different assumptions about the projected trajectory of  over time. Assuming that
over time. Assuming that  is constant in real terms over time (as in ‘iDSI_H’) generally underestimates its growth compared to using our projected values of
is constant in real terms over time (as in ‘iDSI_H’) generally underestimates its growth compared to using our projected values of  (as in ‘Preferred_H’). In contrast, the assumption of 3% annual growth (as in ‘WHOi_H’) may underestimate or overestimate depending on the actual growth rate in each year in each country. Results by country are reported in Supplementary Appendix C, Table C2. Yemen provides an interesting case with the sign of its estimated net health benefit differing between evaluation approaches. In the case of Yemen, the 3% annual growth rate in
(as in ‘Preferred_H’). In contrast, the assumption of 3% annual growth (as in ‘WHOi_H’) may underestimate or overestimate depending on the actual growth rate in each year in each country. Results by country are reported in Supplementary Appendix C, Table C2. Yemen provides an interesting case with the sign of its estimated net health benefit differing between evaluation approaches. In the case of Yemen, the 3% annual growth rate in  represents an overestimate compared to our projected estimates, which forecasts 0.7% CAGR. This has an impact on the estimated sign of the net health benefit, with only the ‘WHOi_H’ approach giving a positive net health benefit.
represents an overestimate compared to our projected estimates, which forecasts 0.7% CAGR. This has an impact on the estimated sign of the net health benefit, with only the ‘WHOi_H’ approach giving a positive net health benefit.
Differences are also observed between the results of the three approaches for each country when we consider the estimated net health benefit itself (and not just its sign). The results by country in Supplementary Appendix C, Table C2 are summarized in Figure 1.
Figure 1.
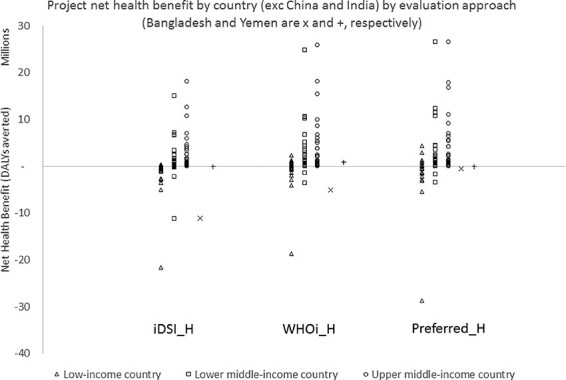
Net health benefit by country by evaluation approach
Moving from considering the sign of net health benefit to its magnitude, the value of the project in terms of the net present value of net health benefit is higher for each country when analysed according to ‘WHOi_H’ compared to ‘iDSI_H’ for two reasons. First, as explained above, assuming that  is constant (as in ‘iDSI_H’) results in lower estimated net health benefits compared to when it is assumed to grow at 3% per year in ‘WHOi_H’. Second, this is compounded by the lower discount rate applied to net health benefit in ‘WHOi_H’, which means that there is a higher weight attached to future values of net health benefit where
is constant (as in ‘iDSI_H’) results in lower estimated net health benefits compared to when it is assumed to grow at 3% per year in ‘WHOi_H’. Second, this is compounded by the lower discount rate applied to net health benefit in ‘WHOi_H’, which means that there is a higher weight attached to future values of net health benefit where  is highest. The results for ‘Preferred_H’ are more similar to ‘WHOi_H’, because the assumption of 3% growth in
is highest. The results for ‘Preferred_H’ are more similar to ‘WHOi_H’, because the assumption of 3% growth in  implied by ‘WHOi_H’ is not far off the unweighted CAGR across countries of 2.3% from our projected estimates. However, this masks considerable variation in the forecasts (range: −0.5% to 6%, see Supplementary Appendix A, Table A3), meaning that for some countries the ‘WHOi_H’ will result in an underestimate of the net present value of net health benefit, while for others, it will result in an overestimate. With respect to the discount rate adopted, the country-specific discounting in ‘Preferred_H’ applies a discount rate to net health close to 0% (0% is also applied in ‘WHOi_H’) for all countries because
implied by ‘WHOi_H’ is not far off the unweighted CAGR across countries of 2.3% from our projected estimates. However, this masks considerable variation in the forecasts (range: −0.5% to 6%, see Supplementary Appendix A, Table A3), meaning that for some countries the ‘WHOi_H’ will result in an underestimate of the net present value of net health benefit, while for others, it will result in an overestimate. With respect to the discount rate adopted, the country-specific discounting in ‘Preferred_H’ applies a discount rate to net health close to 0% (0% is also applied in ‘WHOi_H’) for all countries because  and
and  almost exactly offset. This is an artefact of how they are both calculated as a function of projected growth in GDP per capita (see Supplementary Appendix A, careful inspection finds that the country-specific discounting in ‘Preferred_H’ often indicates a small negative discount rate where
almost exactly offset. This is an artefact of how they are both calculated as a function of projected growth in GDP per capita (see Supplementary Appendix A, careful inspection finds that the country-specific discounting in ‘Preferred_H’ often indicates a small negative discount rate where  ).
).
For approaches to evaluation where the objective is to increase consumption, we find a similar pattern in terms of the sign of the estimated net consumption benefit across countries as was found when considering net health benefit. This is summarized in Table 4.
Table 4.
Proportion of countries where a positive net consumption benefit is estimated by income category by evaluation approach
| Proportion of countries where a positive net consumption benefit is estimated | ||||
|---|---|---|---|---|
| Groups of countries | WHO_C (%) | WHOi_C (%) | BCA_C (%) | Preferred_C (%) |
| Low-income | 25 | 42 | 42 | 42 |
| Lower-middle-income | 81 | 92 | 92 | 89 |
| Upper-middle-income | 100 | 100 | 100 | 100 |
| LMICs (all) | 74 | 82 | 82 | 81 |
This project generates positive net consumption benefits in the majority of middle-income countries (in all upper-middle-income countries and in most lower-middle-income countries) and negative net consumption benefits in the majority of low-income countries. The reason for this finding is again because of the different values of  that are generally found across income categories as it is
that are generally found across income categories as it is  that determines if (and when) a net health benefit is achieved. With this project, there are no wider effects beyond health and so calculating net consumption benefit effectively only involves re-scaling these net health benefits. The proportion of countries where a positive net health benefit is estimated is therefore lowest according to ‘WHO_C’, which illustrates the effect of assuming no real terms changes in
that determines if (and when) a net health benefit is achieved. With this project, there are no wider effects beyond health and so calculating net consumption benefit effectively only involves re-scaling these net health benefits. The proportion of countries where a positive net health benefit is estimated is therefore lowest according to ‘WHO_C’, which illustrates the effect of assuming no real terms changes in  . The differences between the results from the other approaches presented here are more subtle. As with the analysis with the objective of improving health, Yemen is only found to have a positive estimated net consumption benefit according to ‘WHOi_C’. Again, this illustrates that the assumed growth rate of 3% for
. The differences between the results from the other approaches presented here are more subtle. As with the analysis with the objective of improving health, Yemen is only found to have a positive estimated net consumption benefit according to ‘WHOi_C’. Again, this illustrates that the assumed growth rate of 3% for  and
and  is likely to be an overestimate for some countries such as Yemen. Another interesting case is that a positive net consumption benefit is estimated for Bangladesh with the ‘BCA_C’ approach but not with any of the other approaches presented here. To help to understand this finding, we have presented the cumulative net present value of net consumption benefit over time for Bangladesh in Figure 2.
is likely to be an overestimate for some countries such as Yemen. Another interesting case is that a positive net consumption benefit is estimated for Bangladesh with the ‘BCA_C’ approach but not with any of the other approaches presented here. To help to understand this finding, we have presented the cumulative net present value of net consumption benefit over time for Bangladesh in Figure 2.
Figure 2.
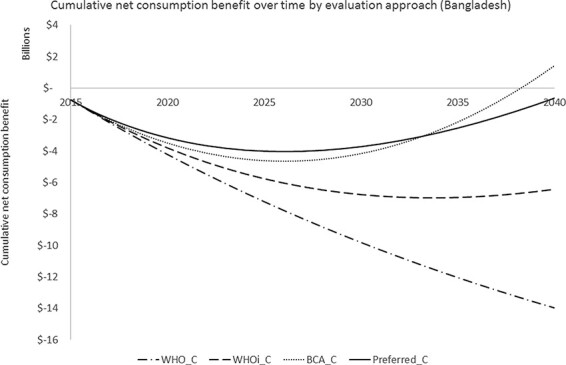
Cumulative net present value of net consumption benefit over time for Bangladesh according to different evaluation approaches
In the ‘BCA_C’ analysis, country-specific projections of  are applied (where it is found to grow at a CAGR of 4.7%), which results in net consumption benefits being generated from 2027 onwards (the turning point for ‘BCA_C’ and also ‘Preferred_C’ in Figure 2). In addition,
are applied (where it is found to grow at a CAGR of 4.7%), which results in net consumption benefits being generated from 2027 onwards (the turning point for ‘BCA_C’ and also ‘Preferred_C’ in Figure 2). In addition,  is assumed to grow to a disproportionately high extent with GDP growth (with an income elasticity of health of 1.5), where Bangladesh is forecasted to experience a high growth in GDP over the period under consideration (CAGR of 4.6%). Finally, the uniform discount rate of 3% applied in ‘BCA_C’ is relatively low compared to when based on Bangladesh’s high forecasted GDP growth (e.g. ‘Preferred_C’). Taken together, the ‘BCA_C’ analysis results in net health benefits from 2027, which is the same as in ‘Preferred_C’, that are valued more highly and discounted less than in ‘Preferred_C’.
is assumed to grow to a disproportionately high extent with GDP growth (with an income elasticity of health of 1.5), where Bangladesh is forecasted to experience a high growth in GDP over the period under consideration (CAGR of 4.6%). Finally, the uniform discount rate of 3% applied in ‘BCA_C’ is relatively low compared to when based on Bangladesh’s high forecasted GDP growth (e.g. ‘Preferred_C’). Taken together, the ‘BCA_C’ analysis results in net health benefits from 2027, which is the same as in ‘Preferred_C’, that are valued more highly and discounted less than in ‘Preferred_C’.
We can also compare the estimated levels of net consumption benefit by country, which is shown in Figure 3.
Figure 3.
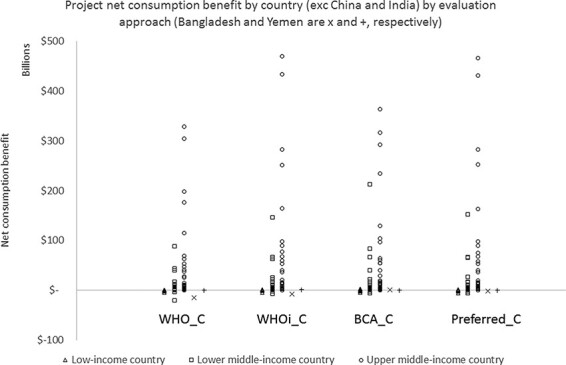
Net consumption benefit by country by evaluation approach
The discounting strategy is the same for all of ‘WHO_C’, ‘WHOi_C’ and ‘BCA_C’ and so differences in the estimated net consumption benefit are entirely driven by different assumptions about how  and
and  might be expected to change over time. As a result, in almost all countries, the magnitude of net consumption benefit is lowest in ‘WHO_C’, which assumes no temporal change in these evaluation parameters. The net consumption benefit appears similar when estimated using ‘WHOi_C’ and ‘BCA_C’, since both involve growing values for
might be expected to change over time. As a result, in almost all countries, the magnitude of net consumption benefit is lowest in ‘WHO_C’, which assumes no temporal change in these evaluation parameters. The net consumption benefit appears similar when estimated using ‘WHOi_C’ and ‘BCA_C’, since both involve growing values for  and
and  for most countries. The same is also true for ‘Preferred_C’, but a slightly different pattern is observed because the effect of growing values for
for most countries. The same is also true for ‘Preferred_C’, but a slightly different pattern is observed because the effect of growing values for  and
and  is offset by higher discount rates in ‘Preferred_C’ (and conversely slower growth in these values offset by lower discount rates).
is offset by higher discount rates in ‘Preferred_C’ (and conversely slower growth in these values offset by lower discount rates).
Discussion
Assessing the value of a new health-related project requires information about the project itself, the additional costs it imposes and DALYs averted, but it also requires other information in the form of evaluation parameters. Evaluation parameters are required in order to account for the resource constraints of the healthcare system, preferences of the population served by the decision-maker and the timing of costs and effects. Good examples of conventional practice may use the latest recommendations for evaluation parameters, but they rarely explicitly consider whether these are reasonable, given the country context and the timing of effects of the decision. In particular, conventional practice embeds assumptions about expectations of changes in  and
and  over time within discount rates. In part, this has been the approach taken due to the absence of evidence that might inform values for these evaluation parameters for each country over time. However, it has also stifled debate as to whether the implicit assumptions are appropriate for a country at a given point in time, or, indeed, broadly appropriate for LMICs. For example, the widespread use and recommendation of a 3% discount rate are thought to derive from experience with high-income countries and may not be appropriate for LMICs where projected economic growth outstrips more mature economies (Haacker et al., 2020). This paper provides estimates for all of the relevant evaluation parameters for 95 LMICs between 2015 and 2040 and applies them within a formal evaluation framework. A highly stylized hypothetical health-related project is analysed to assess the appropriateness of assumptions implied by recent economic evaluation guidelines.
over time within discount rates. In part, this has been the approach taken due to the absence of evidence that might inform values for these evaluation parameters for each country over time. However, it has also stifled debate as to whether the implicit assumptions are appropriate for a country at a given point in time, or, indeed, broadly appropriate for LMICs. For example, the widespread use and recommendation of a 3% discount rate are thought to derive from experience with high-income countries and may not be appropriate for LMICs where projected economic growth outstrips more mature economies (Haacker et al., 2020). This paper provides estimates for all of the relevant evaluation parameters for 95 LMICs between 2015 and 2040 and applies them within a formal evaluation framework. A highly stylized hypothetical health-related project is analysed to assess the appropriateness of assumptions implied by recent economic evaluation guidelines.
We reflect conventional practice drawing upon three sources of commonly used guidance: iDSI, WHO and BCA. With the exception of BCA, these approaches adopt uniform assumptions across countries about the growth rate of  and
and  , and without exception, they advise uniform and constant discount rates (in the absence of existing country guidance).
, and without exception, they advise uniform and constant discount rates (in the absence of existing country guidance).
Empirically derived values for  and
and  are available, but projected values of
are available, but projected values of  and
and  over time have not been available prior to this paper. However, this does not justify assumptions of constancy (or some uniform growth rate across countries) over time when available data can be used to inform estimates of how these might evolve in the future. We apply this principle to estimating
over time have not been available prior to this paper. However, this does not justify assumptions of constancy (or some uniform growth rate across countries) over time when available data can be used to inform estimates of how these might evolve in the future. We apply this principle to estimating  in Supplementary Appendix A. We find that allowing
in Supplementary Appendix A. We find that allowing  and
and  to vary, typically growing, over time shows that the assumption of constancy is likely to underestimate the value of new projects. In analyses devised to inform objectives of improving health and consumption, approaches that allow
to vary, typically growing, over time shows that the assumption of constancy is likely to underestimate the value of new projects. In analyses devised to inform objectives of improving health and consumption, approaches that allow  and
and  to vary with time are found to produce higher estimates of net health and net consumption effects, with the sign changing from negative to positive in 7–8% of countries analysed using our hypothetical project. The hypothetical project analysed is highly stylized and simplistic; it is likely that the effect of different assumptions about evaluation parameters would be greater in the case of projects such as vaccines where results are particularly sensitive to the handling of the timing of costs and effects (WHO, 2019).
to vary with time are found to produce higher estimates of net health and net consumption effects, with the sign changing from negative to positive in 7–8% of countries analysed using our hypothetical project. The hypothetical project analysed is highly stylized and simplistic; it is likely that the effect of different assumptions about evaluation parameters would be greater in the case of projects such as vaccines where results are particularly sensitive to the handling of the timing of costs and effects (WHO, 2019).
The country- and time-specific values we have used for  ,
,  ,
,  and
and  are available in Supplementary Appendix B. A number of assumptions pertain to these values with our method for projecting
are available in Supplementary Appendix B. A number of assumptions pertain to these values with our method for projecting  detailed in Supplementary Appendix A. We have also assumed that the projected growth in GDP per capita can be used as a proxy for
detailed in Supplementary Appendix A. We have also assumed that the projected growth in GDP per capita can be used as a proxy for  when calculating
when calculating  . Another assumption concerns the use of the Ramsey Rule to calculate values for
. Another assumption concerns the use of the Ramsey Rule to calculate values for  . The Ramsey Rule is well-established in economics, with its basis founded on society’s preferences, but there is no guarantee that these will be reflected in the ability of decision-makers to allocate resources inter-temporally (i.e. it is not guaranteed that
. The Ramsey Rule is well-established in economics, with its basis founded on society’s preferences, but there is no guarantee that these will be reflected in the ability of decision-makers to allocate resources inter-temporally (i.e. it is not guaranteed that  ). Other considerations highlighted in Claxton et al. (2019) concerning factors to be incorporated in discounting, such as the time horizon under consideration, the relationship between macro-economic risk and project-specific risk and uncertainty around projected growth rates in real income and effects on
). Other considerations highlighted in Claxton et al. (2019) concerning factors to be incorporated in discounting, such as the time horizon under consideration, the relationship between macro-economic risk and project-specific risk and uncertainty around projected growth rates in real income and effects on  , are not considered but are important areas for further research. Parameter uncertainty, more generally, particularly in future values, is not incorporated within this analysis, but it is likely to be considerable and may be of relevance to decision-makers.
, are not considered but are important areas for further research. Parameter uncertainty, more generally, particularly in future values, is not incorporated within this analysis, but it is likely to be considerable and may be of relevance to decision-makers.
Conclusion
Conventional practice in health economics often embeds implicit assumptions about expected changes in resource constraints and societal preferences within the discount rates used to evaluate projects resulting in a lack of clarity and transparency. In addition, the assumptions made may not be appropriate for a country at a given point in time or for LMICs in general. Separating out these arguments and marshalling available evidence to inform estimates of evaluation parameters by country and over time can produce a flexible evaluation framework that can inform decision-makers in a more transparent and appropriate manner.
This paper provides such a framework and demonstrates (and provides the required parameter values for) the application of this framework. Even when applied to a simple hypothetical example, this framework with preferred assumptions about evaluation parameters gives important differences in results compared to the application of existing guidelines. The implication is that analysts need to consider critically the appropriateness of existing guidelines for economic evaluation in the context of their country. In addition, looking ahead, future guidelines for economic evaluation in LMICs should ensure that assumptions about evaluation parameters are clearly and explicitly stated and are founded on the best available evidence.
Supplementary Material
Acknowledgements
We are grateful to Joseph Dieleman for generously sharing with us projections of GDP for the countries analysed between 2015 and 2040. We thank the anonymous referees for their comments that have greatly improved this paper.
Endnotes
For simplicity, in this example, there are no non-health effects to consider, but in general, they would be incorporated here (Claxton et al., 2019; Walker et al., 2019).
Woods et al. (2016) provide estimates for a range of countries (including LMICs) based on extrapolation of the Claxton, Martin, et al. (2015) estimate for the UK. Estimates for some (mainly high-income) countries exist that use bespoke within-country analysis (Claxton et al., 2015; Edney et al., 2018; Vallejo-Torres et al., 2018; Siverskog and Henriksson, 2019; Stadhouders et al., 2019; van Baal et al., 2019; Edoka and Stacey, 2020; Ochalek et al., 2020).
We tested for structural breaks in the relationship between  and GDP per capita by categorizing countries according to eligibility for support funding from different institutions: GAVI, IMF and Global Fund. We ultimately derive a satisfactory model that differs for GAVI-eligible countries (see Supplementary Appendix A). These countries are those that have access to GAVI-negotiated prices for vaccines.
and GDP per capita by categorizing countries according to eligibility for support funding from different institutions: GAVI, IMF and Global Fund. We ultimately derive a satisfactory model that differs for GAVI-eligible countries (see Supplementary Appendix A). These countries are those that have access to GAVI-negotiated prices for vaccines.
The compound annual growth rate of GDP per capita between 2015 and 2040 varies considerably among LMICs, ranging between −0.5% (Congo) and 5.3% (China).
This is justified as a pragmatic proxy for what is typically done to calculate VSLY from VSL, which is to divide the estimated VSL by the conditional life expectancy at the average individual included in the study.
Contributor Information
James Lomas, Centre for Health Economics, University of York, York YO10 5DD, UK.
Karl Claxton, Centre for Health Economics, University of York, York YO10 5DD, UK; Department of Economics and Related Studies, University of York, York YO10 5DD, UK.
Jessica Ochalek, Centre for Health Economics, University of York, York YO10 5DD, UK.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
Data availability statement
The data underlying this article are available in the article and in its online supplementary material.
Funding
This study received funding support from the Bill and Melinda Gates Foundation [OPP1165566 to University of York].
Ethical approval.
Ethical approval for this type of study is not required by our institute.
Conflict of interest.
The authors declare that they have no conflict of interest.
References
- Bertram MY, Lauer JA, De Joncheere K et al. 2016. Cost-effectiveness thresholds: pros and cons. Bulletin of the World Health Organization 94: 925–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer W et al. 2018. When is it too expensive? Cost-effectiveness thresholds and health care decision-making. The European Journal of Health Economics 20: 175–80.doi: 10.1007/s10198-018-1000-4. [DOI] [PubMed] [Google Scholar]
- Claxton K, Asaria M, Chansa C et al. 2019. Accounting for timing when assessing health-related policies. Journal of Benefit-Cost Analysis 10: 73–105.doi: 10.1017/bca.2018.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claxton K, Martin S, Soares M et al. 2015. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technology Assessment (Winchester, England) 19.doi: 10.3310/hta19140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claxton K, Paulden M, Gravelle H et al. 2011. Discounting and decision making in the economic evaluation of health-care technologies. Health Economics 20: 2–15. [DOI] [PubMed] [Google Scholar]
- Council of Economic Advisers . 2017. Discounting For Public Policy: Theory and Recent Evidence on the Merits Of Updating the Discount Rate. https://obamawhitehouse.archives.gov/sites/default/files/page/files/201701_cea_discounting_issue_brief.pdf, accessed 3 July 2020.
- Dieleman JL, Campbell M, Chapin A et al. 2017. Future and potential spending on health 2015-40: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. TheLancet 389: 2005–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW 2015. Methods for the Economic Evaluation of Health Care Programmes, 4th ed. Oxford: Oxford University Press. [Google Scholar]
- Drupp MA et al. 2018. Discounting disentangled. American Economic Journal: Economic Policy 10: 109–34. [Google Scholar]
- Edney LC, Haji Ali Afzali H, Cheng TC et al. 2018. Estimating the reference incremental cost-effectiveness ratio for the Australian Health System. PharmacoEconomics 36: 239–52. [DOI] [PubMed] [Google Scholar]
- Edoka IP, Stacey NK 2020. Estimating a cost-effectiveness threshold for health care decision-making in South Africa. Health Policy and Planning 35: 546–55.doi: 10.1093/HEAPOL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groom B, Maddison D. 2019. New estimates of the elasticity of marginal utility for the UK. Environmental and Resource Economics 72: 1155–82. [Google Scholar]
- Haacker M, Hallett TB, Atun R. 2020. On discount rates for economic evaluations in global health. Health Policy and Planning 35: 107–14. [DOI] [PubMed] [Google Scholar]
- Hammitt J, Robinson L. 2011. The income elasticity of the value per statistical life: transferring estimates between high and low income populations. Journal of Benefit-Cost Analysis 2: 1–29. [Google Scholar]
- Leech AA, Kim DD, Cohen JT et al. 2018. Use and misuse of cost-effectiveness analysis thresholds in low- and middle-income countries: trends in cost-per-DALY studies. Value in Health 21: 759–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masterman CJ, Viscusi K. 2018. The income elasticity of global values of a statistical life: stated preference evidence. Journal of Benefit-Cost Analysis 9: 407–34. [Google Scholar]
- Ochalek J, Lomas J. 2020. Reflecting the health opportunity costs of funding decisions within value frameworks: initial estimates and the need for further research. Clinical Therapeutics 42: 1. [DOI] [PubMed] [Google Scholar]
- Ochalek J, Lomas J, Claxton K. 2018. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Global Health 3: e000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochalek J, Wang H, Gu Y et al. 2020. Informing a cost-effectiveness threshold for health technology assessment in China: a marginal productivity approach. PharmacoEconomics 38: 1319–31. [DOI] [PubMed] [Google Scholar]
- Paulden M, Claxton K. 2012. Budget allocation and the revealed social rate of time preference for health. Health Economics 21: 612–8. [DOI] [PubMed] [Google Scholar]
- Paulden M, O’Mahony J, McCabe C. 2017. Determinants of change in the cost-effectiveness threshold. Medical Decision Making 37: 264–76. [DOI] [PubMed] [Google Scholar]
- Robinson L, Hammitt JK, O’Keeffe L. 2019a. Valuing mortality risk reductions in global benefit-cost analysis. Journal of Benefit-Cost Analysis 10: 15–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson LA et al. 2019b. Reference Case Guidelines for Benefit-Cost Analysis in Global Health and Development. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2447/2019/05/BCA-Guidelines-May-2019.pdf, accessed 19 May 2020.
- Sanders GD, Neumann PJ, Basu A et al. 2016. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses. JAMA 316: 1093. [DOI] [PubMed] [Google Scholar]
- Siverskog J, Henriksson M. 2019. Estimating the marginal cost of a life year in Sweden’s public healthcare sector. The European Journal of Health Economics 20: 751–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadhouders N, Koolman X, Dijk C et al. 2019. The marginal benefits of healthcare spending in the Netherlands: estimating cost-effectiveness thresholds using a translog production function. Health Economics 28: 1331–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallejo-Torres L, García-Lorenzo B, Serrano-Aguilar P. 2018. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Economics 27: 746–61. [DOI] [PubMed] [Google Scholar]
- van Baal P, Perry-Duxbury M, Bakx P et al. 2019. A cost-effectiveness threshold based on the marginal returns of cardiovascular hospital spending. Health Economics 28: 87–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscusi WK, Masterman CJ. 2017. Income elasticities and global values of a statistical life. Journal of Benefit-Cost Analysis 8: 226–50. [Google Scholar]
- Walker S, Griffin S, Asaria M et al. 2019. Striving for a societal perspective: a framework for economic evaluations when costs and effects fall on multiple sectors and decision makers. Applied Health Economics and Health Policy 17: 577–90.doi: 10.1007/s40258-019-00481-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein MC et al. 1996. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA: The Journal of the American Medical Association 276: 1253. [PubMed] [Google Scholar]
- WHO . 2003. WHO Guide to Cost-Effectiveness Analysis. Tan-Torres Edejer T et al. (ed.) Geneva: World Health Organization. [Google Scholar]
- WHO . 2019. Immunization, Vaccines and Biologicals WHO Guide For Standardization Of Economic Evaluations Of Immunization Programmes EDITION II. https://www.who.int/immunization/documents/who_ivb_19.10/en/, accessed 19 May 2020.
- Wilkinson T, Sculpher MJ, Claxton K et al. 2016. The international decision support initiative reference case for economic evaluation: an aid to thought. Value in Health 19: 921–8. [DOI] [PubMed] [Google Scholar]
- Woods B, Revill P, Sculpher M et al. 2016. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value in Health 19: 929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.


