Abstract
Penetrating orbital injury with a foreign body is a complex problem that requires an interdisciplinary therapeutic approach. Conventionally, an external approach using either transconjuntival or transseptal entry is used by an ophthalmologist. However, there is a risk of damage to the optic nerve and orbital tissue using only the traditional approach. This study concerns a 36-year-old male who has an intra-orbital foreign body (OrbFB). Timely three-dimensional reconstruction computed tomography scan demonstrated an 8-cm-long intra-OrbFB adjacent to the optic nerve penetrating to the contralateral nasal cavity. Endoscopic inspection confirmed a chopstick fragment. Assisted by transnasal endoscopy, the chopstick penetrating from the orbit to the nasal cavity was smoothly removed. Nasal endoscopy is useful for an ophthalmologist in removing foreign body in the orbit.
Keywords: External and endoscopic approach, intra-orbital foreign body, transnasal endoscopic orbital surgery
Introduction
Incidence of penetrating injury due to a retained intra-orbital foreign body (OrbFB) varies from 6% to 50% in traumatic orbital injury or maxillofacial bone injury cases.[1] It may be ignored if the history of the trauma is obscure and the foreign body is not seen in the wound. If the penetration goes through the lamina papyracea into the nasal cavity, inspection from the nose is mandatory to determine the nature of OrbFB. The nature and shape of OrbFBs along with the force or mechanism of penetration determine the depth and extent of injury. Pens and pencils are common OrbFBs and other penetrating objects include umbrellas, knives, chopsticks, eyeglasses, fern, toilet brush handles, forks, keys, knitting needles, and shelving bars.[2] Falls, suicide attempts, and assaults are the three main causes of injury due to orbital penetration.[3]
The diagnosis and management of intra-OrbFB is challenging and requires a multidisciplinary approach. Surgical removal by a traditional orbitotomy often results in visual impairment, severe tissue loss, a long recovery process, or permanent neurological defects. As a minimally invasive procedure, transnasal endoscopic surgery offers another route of entry that allows better visualization of the lesion. This study reports on a individual who had an intra-orbital chopstick penetrating across the orbit to the contralateral nasal cavity. An external approach using transnasal endoscopy is used to successfully locate and remove the intra-OrbFB.
Case Report
A 36-year-old, Asian, heavily drunken male was sent to the emergency department (ED) and presented with a significant swelling to the ecchymosed right eye after an altercation. At the ED, a 3-cm laceration at the right eyebrow area was noted and sutured by the ED staff [Figure 1]. After a few hours, the patient sobered up and an ophthalmologist was consulted. The patient's past ocular history and past medical and surgical history were unremarkable.
Figure 1.
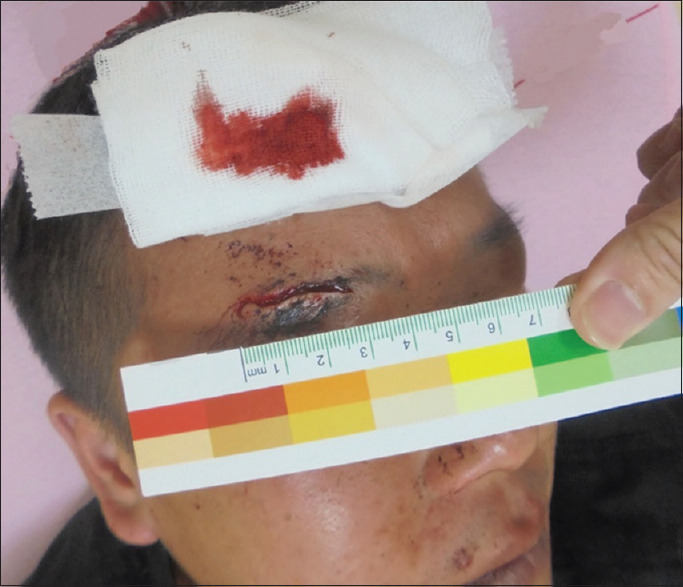
Clinical photograph showing a 3-cm laceration wound with no foreign body protrusion
Ocular examination demonstrated a best-corrected visual acuity of 20/50 in the right eye and 20/25 in the left eye. The eyeball was intact. The pupils and confrontation visual fields were grossly normal. Extraocular motility of the right eye was 75% limited in all the nine cardinal directions, except downward (only about 25%). An anterior segment examination revealed severe subconjunctival hemorrhage and chemosis but no signs of inflammation. A dilated fundus examination showed an attached retina and no vitreous hemorrhage.
A noncontrast computed tomography (CT) study showed a linear structure extending from the right orbital to the left nasal cavity, suggesting a foreign body [Figure 2a-c]. This foreign body was hyperdense, relative to normal parenchyma. The Hounsfield unit scale from the CT of the foreign body was around 500–550, which suggests that the material was plastic. A CT scan with three-dimensional (3D) reconstruction showed detail of the route. The retained foreign body stretched from the supraorbital rim region, penetrating the orbital medial wall and the nasal septum, to the left nasal cavity [Figure 3]. A portable fiberscope was passed through the nasal route and the foreign body was identified as a chopstick fragment.
Figure 2.
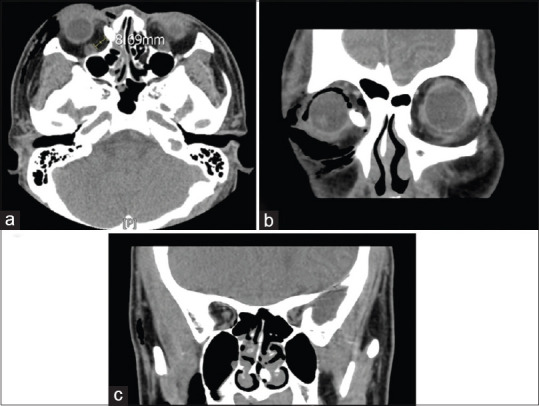
(a) Axial computed tomography showing a hyperdense foreign body in the right orbit with approximate attenuation values of 500–550 Hounsfield units. This is 8 mm from the optic nerve. (b) Computed tomography coronal section showing orbital foreign body penetrating the medial wall to the nasal cavity. (c) Computed tomography coronal section showing orbital foreign body penetrating the nasal septum to the contralateral nasal cavity
Figure 3.
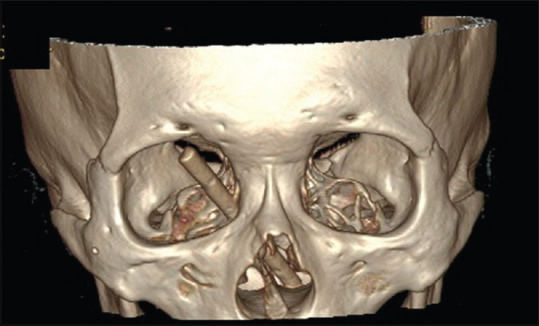
Computed tomography scan using three-dimensional reconstruction to demonstrate the foreign body in the orbital and nasal cavities
The diagnosis of the intraorbital chopstick fragment indicated a need for emergent surgery for extraction to avoid complication and permanent damage. A transorbital approach was chosen. A new 5-mm incision wound, where the tip of the foreign body under skin was palpable, was made beside the original penetrating wound. A blunt and gentle dissection was made from the new incision to explore the tip of the chopstick fragment.
A transnasal endoscope was used to increase safety. An endoscope of 0° angle (Karl Storz) with a high-definition camera and a standard light source were used. Through the endoscope, the chopstick could be visualized clearly from the nasal side [Figure 4]. When pulling the fragments through the new incision, the extraction route was followed all the way into the orbit using direct and simultaneous visualization. A proper angle was chosen and adjusted during the extraction to avoid touching the optic nerve. When the foreign body was removed, a second look was achieved using endoscopy over the entire tract to ensure that no fragments remained. The surgery was smooth without intraoperative bleeding or damage to the periocular structures.
Figure 4.
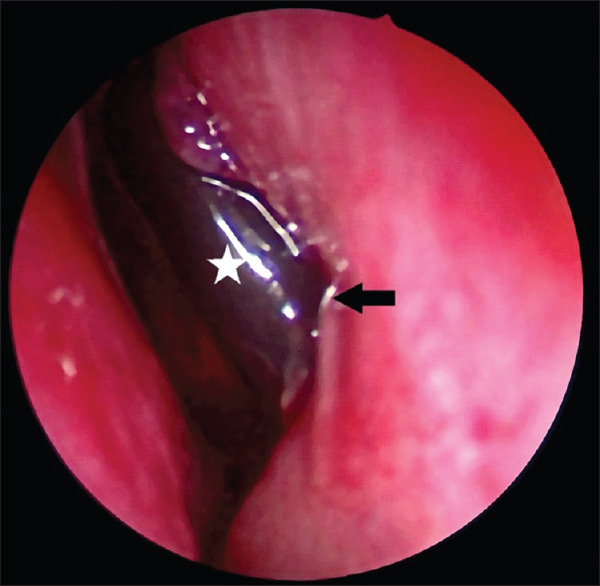
Orbital foreign body seen through the transnasal endoscope. Arrow: Penetrating site at the nasal septum. Star: orbital foreign body
The chopstick was measured to be approximately 8 cm in length [Figure 5]. Postoperative care was uncomplicated. Systemic and topical antibiotics were administered to prevent infection. The patient was discharged uneventfully after 3 days. Following removal of the foreign body, the eyelid hematoma and swelling of the bulbar conjunctiva were significantly reduced. Six days after the operation, visual acuity had improved to 20/25 in the right eye. Extraocular movement also improved with a residual 10% adduction limitation.
Figure 5.

The chopstick was measured to be approximately 8 cm long after complete removal
Discussion
Clinical signs may not be immediately apparent in cases of orbital penetrating injury.[4] This type of injury requires an image study to determine whether there is a retained intra-OrbFB. A full radiological workup must precede removal of the foreign object.[4] Noncontrast CT scanning is the preferred imaging modality. Advances in software and image quality mean that 3D CT offers a clear orientation and shows the extent of tissue injury. In this case, a rod clearly penetrates from the right orbit to the nasal cavity, crossing the nasal septum. A transnasal endoscope was used to evaluate the foreign body in the nasal cavity before and during the operation.
Endoscopic surgery in the orbital area began in the early 1990s.[5] After development in the field of otolaryngology-head-and-neck surgery, it gradually became adopted as a surgical technique for ophthalmology, most often for orbital tumor resection, orbital decompression, and dacryocystorhinostomy. In recent years, a limited number of case series have been published, which describe the use of an endoscope for the removal of a variety of OrbFBs. Endoscopic transnasal surgery, endoscopic transconjunctiva surgery, or combinations of open surgery with an endoscope have been proposed.[6,7,8] Transnasal endoscopy results in minimal morbidity and an early return to normal function. The advantage is that the operator can clearly visualize OrbFB and monitor it during extraction, so there is a lower risk of damage to the surrounding structure and further loss of vision.
The timing of OrbFB removal is controversial and depends on several clinical factors and key conditions, such as the material, the location of the foreign body, and the associated complications. In general, nonorganic foreign bodies, such as metal, nonirritating plastic, and glass, do not require urgent removal unless visual function is heavily impaired or there is uncontrolled inflammation.[9] Copper and iron must be removed immediately because they impose a risk of suppurative inflammation. Organic foreign bodies, such as wood and bamboo, must also be removed as soon as possible because they pose an elevated level of risk for severe and irreversible orbital complications, such as orbital infection and inflammation.[9] In this case, direct inspection of the penetrating material in the nasal cavity showed the nature of the foreign body, which was a plastic chopstick.
Conventionally, open surgery is the most common method for the retrieval of orbital OrbFBs. The route of entry includes transconjunctiva, transseptal, transentry wounds, and a variety of other orbitotomy approaches.[10] Ophthalmologists most often use a conventional transconjuctival approach, but this is of limited utility if the foreign body is situated behind the eyeball or deep into the periorbital tissue. Exploring the intraconal space incurs a risk of damaging the optic nerve and the extraocular muscles. In this case, the chopstick was close to the optic nerve and the extraocular muscles [Figure 2a].
A surgeon must assess the risk and benefit of OrbFB extraction. A transnasal endoscope provides a better surgical view than the traditional method, and it is easy to ensure that all the fragments in visual range along the tract are removed. A new incision is made to create a new angle that is slightly away from the optic nerve, to ensure that there is no damage to the optic nerve during the surgery. If navigation system is used, the procedure is safe and accurate.[11] However, in this case, no navigation system was available.
The combination of external and endoscopic approaches allows an effective, safe, and minimally invasive approach to remove foreign bodies that are located in the medial orbit. Surgical removal of intra-orbital foreign bodies is a classic example of an interdisciplinary therapeutic approach, in which the best outcome is usually the result of a team that comprises an ophthalmologist, an otorhinolaryngologist, and a neurosurgeon.[12]
Conclusion
Transnasal endoscopic surgery combined with an external transorbital approach is an effective, safe, and minimally invasive procedure for the treatment of intra-orbital foreign bodies for certain patients. Facial CT with 3D reconstruction gives an effective view and orientation for preoperative planning. Nasal endoscopy is useful to ophthalmologists for orbital surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Gonullu ME, Filinte GT, Cardak NG, Kucuk S, Akoz T. The surgical strategy for the intraorbital foreign bodies. J Craniofac Surg. 2016;27:1785–8. doi: 10.1097/SCS.0000000000002950. [DOI] [PubMed] [Google Scholar]
- 2.Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury: Case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011;114:53–61. doi: 10.3171/2010.8.JNS10301. [DOI] [PubMed] [Google Scholar]
- 3.Mashriqi F, Iwanaga J, Loukas M, D'Antoni AV, Tubbs RS. Penetrating orbital injuries: A review. Cureus. 2017;9:e1725. doi: 10.7759/cureus.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Donoghue GT, Kumar R, Taleb FS. Unsuspected orbitocranial penetrating injury by a plastic pen cartridge: Case report. J Trauma. 2005;58:634–7. doi: 10.1097/01.ta.0000075799.18982.77. [DOI] [PubMed] [Google Scholar]
- 5.Chen J, Shen T, Wu Y, Yan J. Clinical characteristics and surgical treatment of intraorbital foreign bodies in a tertiary eye center. J Craniofac Surg. 2015;26:e486–9. doi: 10.1097/SCS.0000000000001973. [DOI] [PubMed] [Google Scholar]
- 6.Zhao Y, Liu J, Wang Z, Yan Y, Han J, Yang D. Transnasal endoscopic retrieval of a metallic intraorbital intraconal foreign body facilitated by an intraoperative magnetic stick. J Craniofac Surg. 2019;30:e603–e605. doi: 10.1097/SCS.0000000000005622. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy DW, Goodstein ML, Miller NR, Zinreich SJ. Endoscopic transnasal orbital decompression. Arch Otolaryngol Head Neck Surg. 1990;116:275–82. doi: 10.1001/archotol.1990.01870030039006. [DOI] [PubMed] [Google Scholar]
- 8.Łysoń T, Sieskiewicz A, Rogowski M, Mariak Z. Transnasal endoscopic removal of intraorbital wooden foreign body. J Neurol Surg A Cent Eur Neurosurg. 2013;74(Suppl 1):e100–3. doi: 10.1055/s-0032-1326942. [DOI] [PubMed] [Google Scholar]
- 9.Marchioni D, Bertossi D, Soloperto D, Bianconi L, Procacci P, Nocini PF. Traumatic intraconal foreign body: Report of an injury corrected with combined surgical and endoscopic treatment. Oper Neurosurg (Hagerstown) 2016;12:14–8. doi: 10.1227/NEU.0000000000001150. [DOI] [PubMed] [Google Scholar]
- 10.Griffa A, Viterbo S, Boffano P. Endoscopic-assisted removal of an intraorbital dislocated dental implant. Clin Oral Implants Res. 2010;21:778–80. doi: 10.1111/j.1600-0501.2009.01894.x. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Y, Li Y, Li Z, Deng Y. Removal of orbital metallic foreign bodies with image-guided surgical navigation. Ophthalmic Plast Reconstr Surg. 2020;36:305–10. doi: 10.1097/IOP.0000000000001580. [DOI] [PubMed] [Google Scholar]
- 12.Wu X, Li A, Tan J, Ou X. Removal of orbital-maxillary sinus-pterygopalatine fossa foreign body with external and endoscopic combined approach. J Craniofac Surg. 2014;25:1547–9. doi: 10.1097/SCS.0000000000000848. [DOI] [PubMed] [Google Scholar]


