ABSTRACT
Purpose
To map the current literature on functional neuroimaging use in medical education research as a novel measurement modality for neurocognitive engagement, learning, and expertise development.
Method
We searched PubMed, Embase, Cochrane, ERIC, and Web of Science, and hand-searched reference lists of relevant articles on April 4, 2019, and updated the search on July 7, 2020. Two authors screened the abstracts and then full-text articles for eligibility based on inclusion criteria. The data were then charted, synthesized, and analyzed descriptively.
Results
Sixty-seven articles published between 2007 and 2020 were included in this scoping review. These studies used three main neuroimaging modalities: functional magnetic resonance imaging, functional near-infrared spectroscopy, and electroencephalography. Most of the publications (90%, n = 60) were from the last 10 years (2011–2020). Although these studies were conducted in 16 countries, 68.7% (n = 46) were from three countries: the USA (n = 21), UK (n = 15), and Canada (n = 10). These studies were mainly non-experimental (74.6%, n = 50). Most used neuroimaging techniques to examine psychomotor skill development (57%, n = 38), but several investigated neurocognitive correlates of clinical reasoning skills (22%, n = 15).
Conclusion
This scoping review maps the available literature on functional neuroimaging use in medical education. Despite the heterogeneity in research questions, study designs, and outcome measures, we identified a few common themes. Included studies are encouraging of the potential for neuroimaging to complement commonly used measures in education research and may help validate/challenge established theoretical assumptions and provide insight into training methods. This review highlighted several areas for further research. The use of these emerging technologies appears ripe for developing precision education, establishing viable study protocols for realistic operational settings, examining team dynamics, and exploring applications for real-time monitoring/intervention during critical clinical tasks.
KEYWORDS: Electroencephalography, functional magnetic resonance imaging, functional near-infrared spectroscopy, health professions education, medical education, neurocognitive engagement, neuroimaging
Introduction
Learning in medicine is a complex process with many competing demands on trainees’ time and cognitive resources. The burden is further compounded by the high stakes that hinge on a trainee’s clinical performance. Research that could improve upon the current state of health professions education will require multimodal evidence to be impactful. The abundance of health professions education resources and their financial cost further necessitate scientific inquiry and validation of what exactly constitutes an appropriate medical education.
Historically, evidence based on self-report, multiple choice examinations, and behavioral observation dominated education research. More recently, neuroscience has made remarkable strides in helping us to understand neurocognitive processes [1]. Indeed, neuroimaging technology offers significant opportunities for health professions education research, but adoption of neurocognitive evidence in such research has lagged behind that for kindergarten-12 and higher education. Comprehensive reviews have been published to evaluate neuroimaging use with those learner groups [1]. In contrast, except for a few brief descriptive literature reviews limited in scope and specific to surgery [2–6], health professions education lacks such a robust review. Given that we were not able to find a comprehensive review of the general health professions education research on this emerging topic, we decided to use a scoping review methodology to explore the breadth and depth of this literature [7].
Our aim in conducting this review was to carefully map the literature on functional neuroimaging use in health professions education as an emerging, novel measurement modality for neurocognitive engagement, learning, and expertise development. This review has the potential to serve as a useful resource that will frame the current state of emerging evidence for health professions education researchers, while also identifying future directions for this exciting, novel approach.
Materials and methods
We used a rigorous scoping review methodology that followed the recommendations provided by previous publications [7–9]. Scoping reviews, unlike systematic reviews, are not restricted to a specific set of questions and allow for a broader approach to examining the breadth, depth, and nature of research activity on an emerging research topic [8,10]. This type of review can help map a wide-ranging and heterogeneous literature base in order to summarize the current findings, identify the gaps, and inform future research endeavors [8].
Based on previous publications that provided guidance on scoping review methodology [7–9], our scoping review included five stages: (1) identifying the focused research question; (2) identifying the relevant studies; (3) selecting the studies to include; (4) charting the data; and (5) collating and reporting the results. Additionally, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews (PRISMA-ScR) guidelines [11] were used for reporting this study.
Research question
We posed the following focused question to guide this scoping review: How has functional neuroimaging technology been used in health professions education to measure neurocognitive engagement, learning, and expertise development? Because a large literature base exists on diagnostic and clinical applications of functional neuroimaging, we intentionally kept the research question focused on learning and expertise development. However, this question was broadly inclusive of a wide spectrum of health professions learners from diverse clinical roles, disciplines, specialties, medical tasks, and settings. Our goal was not to summarize the rigor of existing research but to characterize the body of work on this emergent topic.
Data sources and search strategy
One of the authors (J.N., a clinical informationist) developed the search strategy in collaboration with the rest of the team. The initial search was carried out on 4 April 2019, and then updated on 7 July 2020, in the following databases: Medline (PubMed), Embase (Embase.com), The Cochrane Library (Cochrane Database of Systematic Reviews), Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Methodology Register, ERIC (EbscoHost), and Web of Science (Science and Social Science Citation Index). When designing the search strategies for Medline (PubMed), the Cochrane Library, ERIC, and Embase, we identified controlled vocabulary terms for each concept and combined them with keyword synonyms. Web of Science was searched using keyword terms only.
Only articles in English were included owing to constraints related to resources for translating studies published in languages other than English (see Appendix 1 for exact search strategy). We also searched reference lists of review papers [2–6] and gray literature and identified six additional records from this process. We did not limit the results by publication date, as this is a rather new and emerging topic in health professions education.
Screening and selecting the studies
Retrieved references were uploaded into the systematic review software Covidence (Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org), which was used to remove duplicates and facilitate title, abstract, and full-text screening. Two of the authors (S.T. and D.S.) independently screened all of the retrieved titles and abstracts (a total of 1,524 records after duplicate removal) to determine their relevance for the research question and subsequent eligibility for full-text review. After screening the first 100 records, these authors met to discuss the discrepancies (only 11 at this point) and calibrate the screening process. The same two investigators independently completed the title and abstract screening with the remaining records. All of the disagreements (overall kappa 0.63) were resolved by consensus.
At the full-text screening stage, two authors (S.T. and D.S.) independently read all of the articles included for review and applied clear inclusion/exclusion criteria to determine eligibility. We included all English-language research and review articles that were published in peer-reviewed journals and considered the use of functional neuroimaging such as positron emission tomography (PET), electroencephalography (EEG), functional magnetic resonance imaging (fMRI), and functional near-infrared spectroscopy (fNIRS) in health professions education to measure neurocognitive engagement (e.g., attention, cognitive load), learning, and skill and expertise development. Studies were excluded based on the following criteria: focused on the clinical/diagnostic use of neuroimaging; involved patients in the use of neuroimaging; did not use neuroimaging for measuring some aspect of learning or skill development; did not involve medical trainees and/or health professionals. We also excluded editorials, commentaries, meeting abstracts, and articles published in a language other than English. The same two researchers reviewed any disagreements and reached a consensus on the final list of studies to be included in this review. As explained in the next stage, information from the included studies was recorded and summarized with a data charting template.
Charting the data
The use of functional neuroimaging techniques to measure learning, neurocognitive engagement, or expertise development is an emerging research method in health professions education. The existing literature base is small and heterogeneous, making it challenging to draw specific comparisons between the different studies. Providing a brief summary for each of the records may not have much utility for informing future research either. Thus, we adopted a descriptive-analytical approach [8] by consistently applying a common analytical template to all included studies. This approach provided a useful framework for charting the pertinent information on research context and process.
We created a data entry template in Microsoft Excel 2016 (Redmond, Washington) to chart the key information from the studies included in this review. We sifted and sorted the pertinent information to help summarize and interpret the results, systematically charting the records in the process [8]. We then iteratively developed the data extraction sheet to capture relevant and consistent information from each study. Two of the authors (D.H. and J.M.) used this template independently to chart information from 10 randomly selected studies. During a meeting, the team went over these records and refined the template. Remaining articles were divided equally between the same two investigators to extract and chart data based on refined template criteria. To ensure completeness and accuracy, two additional investigators (S.T. and D.S.) divided all included studies equally and reviewed full-text articles against the charted records. The full team resolved any disagreements regarding the charted information by consensus. The extraction template included the following information
Authors
Year of publication
Study location
Study design
Study aims
Study population
Tasks/intervention and duration
Skill of interest (psychomotor, clinical reasoning, etc.)
Neuroimaging modality
Data acquisition, processing, and analysis
Outcome measures
Medical specialty
Major findings
Collating and summarizing the results
Charted data served as the basis for the numerical analysis of the range and nature of the included studies as well as for thematic outline of the findings. We organized the data to create a descriptive summary that encompassed the overall number of studies included; year of publication; country of origin; types of study design; medical specialty and/or study populations; skill(s) of interest; and types of neuroimaging modalities. To ensure appropriateness for interpretation, we also reorganized and further identified various themes that emerged from the extracted data to report common techniques used for neuroimaging data acquisition, processing, and analysis; neuroimaging modality use by year; skill of interest by use of neuroimaging modality; and skill of interest by medical specialty.
Results
We retrieved 1,525 nonduplicate records for title and abstract screening; 119 met the eligibility criteria for full-text screening, and 67 met the final criteria as shown in Figure 1.
Figure 1.
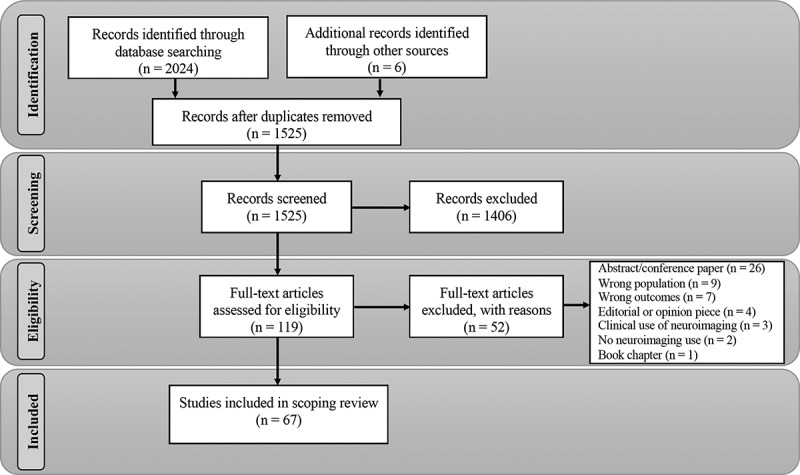
PRISMA flow diagram.
Descriptive summary
The included articles (n = 67) were published between 2007 and 2020 [2–6,12–73]. Ninety percent of these publications (n = 60) were published in the last 10 years (2011–2020) [3–5,17–73], and 70% (n = 47), were published in the last 6 years (2015–2020) [3–5,30–73]. Although these studies were conducted in 16 different countries, the majority (68.7%, n = 46) were from three countries: USA (31.3%, n = 21), UK (22.4%, n = 15), and Canada (15%, n = 10). These publications came from 35 unique institutions (based on primary author affiliations). A total of 10 institutions had two or more articles, which represented 63% (n = 42) of all included articles.
Most of the articles were non-experimental (74.6%, n = 50) and were mainly exploratory in nature (feasibility, pilot, or proof-of-concept studies). The remaining articles were randomized controlled trials (11.9%, n = 8), review articles (7.5%, n = 5), randomized cross-over studies (3%, n = 2), and non-randomized controlled studies (3%, n = 2). Half of the non-experimental studies examined task and/or training effect in cohorts of novice learners (50%, n = 25/50), and a third used a between-subjects design to examine differences in the brain activation patterns either between novices under different conditions or between novices and experts (34%, n = 17/50). Some of the non-experimental studies were proof of concept (8%, n = 4/50), involving small numbers of participants, and others were cross-sectional (6%, n = 3/50). One study used a mixed-design approach by comparing different groups longitudinally (2%, n = 1/50).
As for the sample sizes of the included articles, several were feasibility studies and had five or fewer participants (n = 7), and the largest sample size was 62. Most of the included articles had 20 or fewer participants (54.8%, n = 34/62), whereas 21% (n = 13) had 21 to 30 and 24.2% (n = 15) had more than 31.
Most of the included studies were in surgery or surgical subspecialties (61.2%, n = 41). Other disciplines or learner groups included internal medicine (10.4%, n = 7), medical students (10.4%, n = 7), and gastroenterology (4.5%, n = 3). Four studies (6%) focused on various health sciences learners that did not fit into a single, specific learner group or specialty. There were also five single studies (each representing 1.5% of the total studies) in the following clinical specialties: anesthesiology, cardiology and pulmonology, pediatrics, psychiatry, and radiation oncology.
Most studies represented in this review investigated psychomotor skill development (57%, n = 38) and were conducted in the surgery specialties [13–15,17,20,21,23,28,30,33,34,36,38,39,43,48,49,51,55–58,61,63–67,70,71,74–76], but several (22%, n = 15) looked at neurocognitive correlates of clinical reasoning and diagnostic thinking [18,22,25,26,29,31,32,42,45–47,50,52,53,68]. A smaller number of studies (6%, n = 4) examined visuospatial expertise development [12,19,35,37]; declarative clinical knowledge [40,41,59,62] (6%, n = 4); and correlates of fatigue, well-being, and burnout [16,44,54,60] (6%, n = 4). Also, individual studies used neurocognitive imaging to examine cognitive and emotional control [27] (1.5%, n = 1), and crisis event management team skills [69] (1.5%, n = 1).
Included studies used three main neuroimaging modalities: fMRI (32.8%, n = 22), fNIRS (29.9%, n = 20), and EEG (26.8%, n = 18). The five review articles mentioned use of all these modalities. Summary characteristics for the included articles are shown in Table 1. Also, see Appendix 2 – Summary table listing the first author, publication year, country, primary author institution, study design, neuroimaging modality, specialty, and skill of interest for all included articles.
Table 1.
Characteristics of articles included in the scoping review
| Characteristic | N | Percent |
|---|---|---|
| Year of publication | ||
| 2007 to 2014 | 20 | 30 |
| 2015 to 2020 | 47 | 70 |
| Country of origin | ||
| Brazil | 1 | 1.5 |
| Canada | 10 | 15.0 |
| China | 3 | 4.5 |
| Denmark | 1 | 1.5 |
| Germany | 1 | 1.5 |
| Hong Kong | 1 | 1.5 |
| Ireland | 2 | 3.0 |
| Italy | 2 | 3.0 |
| Japan | 4 | 6.0 |
| Korea | 1 | 1.5 |
| Netherlands | 2 | 3 |
| Singapore | 1 | 1.5 |
| Spain | 1 | 1.5 |
| Turkey | 1 | 1.5 |
| UK | 15 | 22.4 |
| USA | 21 | 31.3 |
| Study design | ||
| Non-experimental | 50 | 74.6 |
| Non-randomized controlled | 2 | 3.0 |
| Randomized crossover | 2 | 3.0 |
| Randomized controlled trial | 8 | 11.9 |
| Review | 5 | 7.5 |
| Specialty/learner group | ||
| Anesthesiology | 1 | 1.5 |
| Cardiology & pulmonology | 1 | 1.5 |
| Gastroenterology | 3 | 4.5 |
| Internal medicine | 7 | 10.4 |
| Medical students | 7 | 10.4 |
| Health sciences learners | 4 | 6.0 |
| Pediatrics | 1 | 1.5 |
| Psychiatry | 1 | 1.5 |
| Radiation oncology | 1 | 1.5 |
| Surgery | 41 | 61.2 |
| Skill of interest | ||
| Clinical reasoning | 15 | 22.0 |
| Cognitive/emotional control | 1 | 1.5 |
| Crisis event management | 1 | 1.5 |
| Clinical knowledge | 4 | 6.0 |
| Fatigue | 2 | 3.0 |
| Psychomotor skills | 38 | 57.0 |
| Well-being, stress, burnout | 2 | 3.0 |
| Visuospatial development | 4 | 6.0 |
| Neuroimaging modality | ||
| EEG | 18 | 26.8 |
| fMRI | 22 | 32.8 |
| fNIRS/OT | 20 | 29.9 |
| Review – NA | 5 | 7.5 |
| Other* | 2 | 3.0 |
EEG, electroencephalogram; fMRI, functional magnetic resonance imaging; fNIRS, functional near-infrared spectroscopy; NA, not applicable; OT, optical topography.
Data acquisition, processing, and analysis
A detailed account of technical and methodological considerations for neuroimaging data acquisition and processing is beyond the scope of this review. Therefore, we briefly review some common steps involved in using this type of modality in health professions education research. Included research studies used various technology and software applications to acquire and process neuroimaging data based on the modality used (i.e., EEG, fMRI, fNIRS). The majority of the technologies used to acquire data were commercially available products, and few were developed at the researchers’ institution.
If researchers are going to use neuroimaging data as a continuous measure of task-related brain activation patterns, they must also ensure data quality and integrity when addressing the specific research question. For instance, some observed changes in brain activation patterns may be attributable to environmental factors or activities unrelated to the task in question. Thus, all of the studies used at least one software package along with filtering and classification techniques to remove noise and signal artifacts such as environmental or muscle and eye movement. The following are some of the software packages reported by the included research studies for neuroimaging data preprocessing and transformation: Analysis of Functional Neuroimages (AFNI) [77], fMRI Expert Analysis Tool (FEAT) [78,79], or FLIRT/MCFLIRT (Motion Correction FMRIB’s Linear Image Registration Tool) [80] for fMRI; HOMER2 [81], Functional optical signal analysis (fOSA) [82], or Imperial College Neuroimaging Analysis (ICNA) [83] or now known as Imperial College Near Infrared Spectroscopy Neuroimaging Analysis (ICNNA) [84] for fNIRS; and EEG lab [85] or Brain Vision Analyzer (Brain Products GmbH, Gilching, Germany) for EEG.
Once the results were filtered, processed, and transformed into a quantitative format, researchers used mainly general linear model approaches to examine the neuroimaging data. Correlation coefficients (Pearson or Spearman’s rank) and nonparametric tests were also used to analyze these data. A few studies (n = 4) specifically mentioned the use of machine learning algorithms [39,58,67,69].
Neuroimaging modality use by year
As described above, most of the research studies included in this review (97%, n = 60/62 [excluding review papers, n = 5]) used one of the three main neuroimaging modalities: fMRI, fNIRS, or EEG. Figure 2 shows the cumulative number of studies that used these three neuroimaging modalities across years. The number of published studies that used fMRI increased steadily between 2007 and 2016, but that increase has since slowed. In comparison, the number of fNIRS- and EEG-based studies has been stea7dily increasing since 2014.
Figure 2.
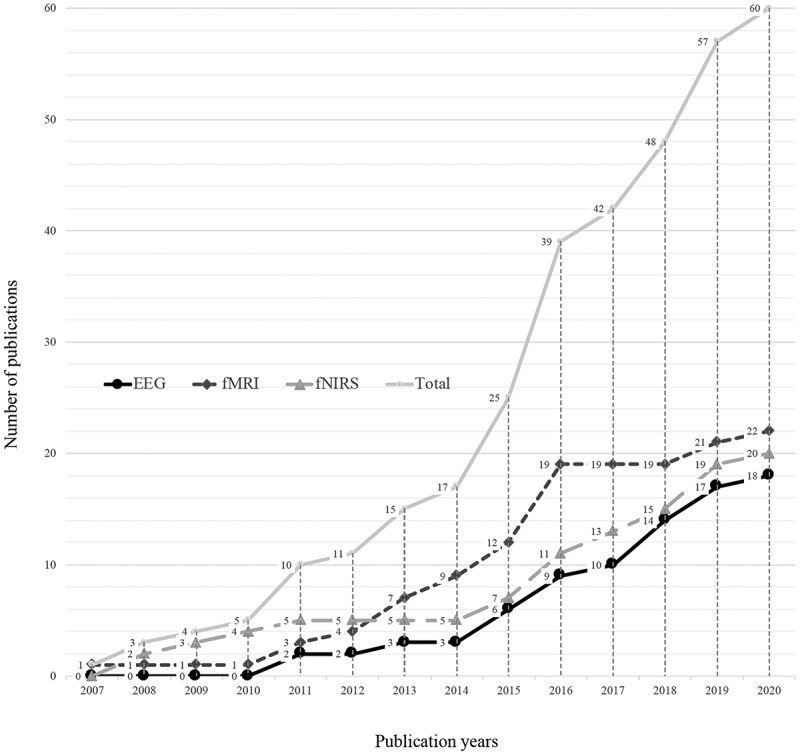
Cumulative number of studies that used each of the three main neuroimaging modalities by year. fMRI, functional magnetic resonance imaging; fNIRS, functional near-infrared spectroscopy; EEG, electroencephalography.
Skill of interest and modality
Most studies on psychomotor skill development used EEG (34%, n = 13/38) or fNIRS (32%, n = 12/38), and few used fMRI (16%, n = 6/38). In contrast, most of the studies that investigated clinical reasoning skills utilized fMRI technology (73.4%, n = 11/15). See Table 2 for the breakdown of studies in terms of skill of interest and neuroimaging modality.
Table 2.
Skill of interest and modality
| Skill | Modality |
Total | ||||
|---|---|---|---|---|---|---|
| EEG | fMRI | fNIRS | Other* | Review | ||
| Psychomotor skills | 13 (34) | 6 (16) | 12 (32) | 2 (5) | 5 (13) | 38 |
| Clinical reasoning | 2 (13.3) | 11 (73.4) | 2 (13.3) | – | – | 15 |
| Declarative clinical knowledge | 2 (50) | 2 (50) | – | – | – | 4 |
| Visuospatial skills | – | 1 (25) | 3 (75) | – | – | 4 |
| Fatigue | – | – | 2 (100) | – | – | 2 |
| Well-being | 1 (50) | 1 (50) | – | – | – | 2 |
| Cognitive/emotional control | – | 1 (100) | – | – | – | 1 |
| Crisis event management | – | – | 1 (100) | – | – | 1 |
All data are shown as n (%).
Abbreviations: EEG, electroencephalogram; fMRI, functional magnetic resonance imaging; fNIRS, functional near-infrared spectroscopy.
Skill of interest by specialty
Studies that examined psychomotor skill development and visuospatial skills were conducted predominantly in surgery or surgical subspecialties (95%, n = 36/38; 75%, n = 3/4, respectively), whereas those focused on clinical reasoning were conducted mainly in internal medicine (47%, n = 7/15). Studies that examined declarative clinical knowledge utilized medical and health sciences students (100%, n = 4).
Discussion
The purpose of this scoping review was to assess the existing literature related to functional neuroimaging of neurocognitive engagement in health professions education. Since the focus in this review was on the use of neuroimaging to study learning, we did not include interventional applications of neuroimaging such as neurofeedback. We also did not include studies that used EEG primarily as a measure of fatigue or sleep deprivation. However, if a study question focused on the effect of EEG measured sleep deprivation on learning, we did include the study. This review is the first to map the relevant literature on this topic. Synthesizing the research findings and indicating the untapped potentials of neuroimaging use could raise awareness, inform future efforts in this line of inquiry, and stimulate more interest in conducting such research in health professions education.
Our findings show increasing reports of studies, especially in the last 5 years, and likely enhanced momentum, as medical educators recognize the opportunities to provide objective evidence. The rapid development of user-friendly technologies, such as wireless EEG and fNIRS headsets, and increased access to fMRI scanners also likely contributes to the increased pace. Recognizing the accessibility of these new technologies and their applications for learning may pave the way for future studies.
Our results show patterns of use that are related to either date of study or study question. The earlier studies, 2007–2014, primarily utilized fMRI, and the later studies, 2015–2020, show increasing use of EEG and fNIRS. We believe that this progression is due to the increased availability of easier-to-use wireless headsets and software for data acquisition and analysis. These changes also coincided with the rapid expansion of large-database use in medical science. Each of the imaging modalities creates massive amounts of data. Therefore, current and future considerations for regular use of neuroimaging in assessment of learning must include plans for data storage, data management, and accuracy of software algorithms.
Notably, research questions can lend themselves to one imaging modality or another. Both fMRI and fNIRS are brain mapping techniques that rely on hemodynamic response for capturing neurocognitive processes. fMRI provides high spatial resolution for exploring activation patterns of specific brain regions associated with various cognitive tasks. When the study goal is to look for temporal effects, fNIRS is better than fMRI. However, both have relatively low temporal resolution compared to EEG, which offers temporal resolution on the order of milliseconds for examining task-related brain activation patterns. See Table 3 for more comparisons between neuroimaging modalities. Some groups have explored options of combining measurement modalities to optimize temporal and spatial resolution however logistical impediments remain an important barrier.
Table 3.
Characteristics of neuroimaging modalities
| Modality | How it works | Best applications | Advantages [86] | Disadvantages [86] |
|---|---|---|---|---|
| fMRI | Captures hemodynamic response/regional activated neuroanatomy |
|
|
|
| fNIRS | Captures hemodynamic response through optical intensity/regional brain blood flow |
|
|
|
| EEG | Electrical activity of the brain showing wavelength and areas of activation Event-related potentials |
|
|
|
Abbreviations: EEG, electroencephalogram; fMRI, functional magnetic resonance imaging; fNIRS, functional near-infrared spectroscopy.
Our results show that the literature base on this topic is still emerging and that the majority of the studies are exploratory (feasibility, pilot, or proof-of-concept). The heterogeneity of the target learner populations, research questions, study designs, targeted skills, interventions, outcome measures, and neuroimaging modalities used makes it impractical to systematically compare outcomes across studies. However, our review of the main results identified a few common themes within the included studies. The researchers either stated explicitly or indicated implicitly (by the study design) that they adopted information processing, neural efficiency, and/or dual processing theory to inform their research.
These frameworks within the context of these studies help explain differences in the brain activation patterns between novices and experts. Evidence from cognitive neuroscience has shown that the frontal cortex is a major hub for storage and executive processes [87]. Individuals are thought to better regulate their working memory resources and exhibit significantly less brain activation in the prefrontal cortex (PFC) while performing tasks within their area of expertise [88]. Similarly, dual processing theory suggests that with experience and proficiency, slow, analytical decision-making evolves into less-effortful, intuitive judgements [89].
Overall, included research studies that used functional neuroimaging technology during technical skill performance indicated that experts and novices show distinct brain activation patterns. Experts show significantly lower activation, especially in the PFC, than do novices. One study with a longitudinal component found that after repeated practice, novices still showed persistent engagement in the PFC even after they demonstrated expert level performance based on observational measures [51]. This finding may in fact have some implications for clinical educators and hint that demonstrated competency in a controlled educational environment may not necessarily translate into complex clinical settings.
Complex procedural skills that require coordination of multiple sensorimotor functions or pathways may not be detected clearly enough in the brain activation patterns to distinguish skill levels. For instance, one included study hypothesized that functional connectivity data within sensorimotor and associative networks may be a better measure to appreciate differences in surgeon skill levels [39]. This group applied machine learning algorithms to functional brain connectivity data and was able to classify surgeon skill levels with good accuracy. Their findings are still in line with other included studies that reported increased PFC activation in the novices but also adds that novices showed stronger interaction between prefrontal and motor-related regions than did experts.
Although high levels of brain activation in the PFC could hinder performance, low levels of activation might indicate lack of attention and concentration. For example, one group examined the effect of temporal pressure on laparoscopic suturing performance and on the neurocognitive correlates of task load (Modi et al., 2018). Performance scores decreased for all trainees under time-pressure conditions when compared to self-pacing. All trainees reported greater task load under time pressure and showed decreased PFC activity, especially junior trainees. In a subsequent study, this group used fNIRS to examine brain activation differences between trainees who maintained a stable performance under time pressure and those who did not [65]. Resilient trainees showed greater bilateral ventral PFC activation, suggesting better attentional control and vigilance. Interestingly, researchers found that stress sensitivity and performance degradation were unrelated to experience level and were not captured by the heart-rate variability or self-report work-load measures (Surgical-TLX). The current literature base does not provide clear markers for the optimal PFC engagement levels, which may be dependent on the context, task, and individual.
Similarly, studies examining clinical reasoning or decision-making indicated that experts and novices show different brain activation patterns, especially, in the PFC. Additionally, the nature of the task seems to modulate the brain activation patterns, as several studies showed that problem-solving tasks or difficult cases induced significantly higher brain activation than did simple recall or routine clinical cases [25,42,46,52,68]. Several of these clinical decision-making studies specifically examined whether dual processing theory could be verified by the use of functional brain imaging [46,47,68]. A few studies also looked at the changes in brain activation patterns as a function of learning or based on high or low performance [18,22,27,40,45]. For example, one group showed that incorrect answers induced higher PFC activation than did correct answers [22].
This review also indicates a few areas ripe for further research efforts. One such area is the establishment of a viable study design and research methods for operational settings. Though researchers attempted to approximate real-life tasks, studies embedded in operational settings with realistic clinical tasks are scarce. For environmental validity, future research endeavors may use real-world settings, perhaps by integrating functional neuroimaging within simulated clinical environments. For example, one study included in this review explored the use of functional neuroimaging to examine team functioning [69] during high-fidelity simulation-based training for crisis event management in the operating rooms. This group showed that it was feasible to use wireless functional neuroimaging technology to measure workload and team engagement in simulated clinical settings. Their results suggested that deoxyhemoglobin in the PFC was a good indicator of workload for individuals but that oxyhemoglobin neural synchrony was more sensitive to scenario difficulty levels. The teams that participated in that study showed greater neural synchrony during teamwork. These findings are encouraging; however, team dynamics in fluid clinical settings are quite complex, and more work is needed to continue building evidence for reliability and validity for capturing neurocognitive correlates of team experience.
Our review did not identify a strong literature base within the health professions education for real-time monitoring of tasks that require vigilance and sustained attention. One group examined the effect of fatigue on clinical reasoning skills across two separate pilot studies as internal medicine physicians answered and reflected on multiple-choice questions from the US medical licensing and/or maintenance of certification exams [29,32]. The results were consistent with those of other studies outside medical education, which have shown that fatigue and sleep quantity are associated with significant changes in brain activation patterns, especially in the medial and/or lateral PFC and other working memory-related areas. Although the exact nature of this relationship was not clear, these preliminary findings emphasize the importance of examining how fatigue and sleep deprivation might regulate neurocognitive engagement. The interplay among various factors such as expertise level, task, cognitive load, attention, and medical errors presents critical research opportunities for functional neuroimaging studies. Numerous studies in other fields could offer guidance for such efforts in health professions education. This type of research can have significant implications for real-time monitoring, and potentially intervention, during critical clinical tasks.
Several studies have used learning curves to visualize learning/competency development in various clinical skills as a function of effort and accuracy/achievement plotted across multiple data points [90]. However, studies that use functional neuroimaging to track and verify the expertise development process are lacking. Future longitudinal studies that examine changes in the brain activation patterns of learners could be invaluable to understanding the learning process at a more individual level and for potentially devising ways to individualize and optimize health professions training. These research opportunities are vast, and the impact of this approach to health professions education is important, as it may provide novel and complementary measures of learning and perhaps additional insights into competency development from a neurocognitive perspective.
Another question ripe for study is whether gender differences in brain activation patterns appear in studies of this type. Two articles [24,71] specifically mentioned comparing brain activation patterns between male and female participants. Both studies examined laparoscopic skill development. Bocci et al. (2013) used EEG to measure the differences in hemispheric connectivity in surgeons using either laparoscopic or robotic surgery for the same motor task. This study did not find any significant differences between males and females performing the same task in neither hemispheres [24]. The second study [71], a randomized controlled trial, used fNIRS to assess the effects of standardized laparoscopic workshops on medical students’ prefrontal cortex activation (PFCA) patterns. Overall, trained individuals showed left PFCA attenuation for precision cutting task. Subgroup analyses indicated that trained female students had significantly greater PFCA attenuation compared to untrained female students for peg transfer and precision cutting tasks whereas no difference was noted between trained and untrained males. The researchers concluded that female students were better able to focus and thus benefitted from focused laparoscopic training. However, these differences in PFCA were not reflected in objective performance scores.
We currently do not have efficient methods for gaining a full understanding of the neurocognitive engagement of learners. Educational efficacy could be markedly augmented if one were able to recognize when cognitive load increases enough to impair attention, when situational awareness is impaired, or when fatigue reduces attention. Understanding such neurocognitive engagement of the learner in the classroom and particularly at the bedside may facilitate learning and possibly enhance patient safety. In an age when learner-centered approaches, much like patient-centered medicine, have recognized value, we must develop efficient and comprehensive measures of learning success across various classroom and clinical educational settings. Recognition of impaired learning may help programs make adjustments to instructional design, learning environment, pace, or repetition.
Finally, we were not able to find strong presence of power and sample size considerations in the included studies. As reported earlier, most of the studies had considerably small sample sizes. The fact that neuroimaging provides rich data may allow for the detection of meaningful differences in the brain activation patterns. However, as this research matures, it will be important to provide robust methodology for sample size considerations with respect to the research question. This field of study will be optimally developed with more longitudinal, comprehensive and hypothesis-driven investigations. We need to learn more about brain dynamics in both learners and experts and how neuroimaging modalities can capture those differences. Additionally, technological development of sophisticated and affordable wearable devices should improve the possibilities of using neuroimaging in live, patient care environments.
Limitations to reviews of this nature include the possibility of bias in selection of the published articles. We limited our selection committee to two investigators after establishing our research question and search methods and conducted a calibration exercise at the beginning of screening. Each investigator screened the candidate studies for inclusion, and discrepancies were discussed and resolved. PRISMA-ScR guidelines were followed in an attempt to generate a transparent report of the available literature.
Conclusions
This scoping review provides an overview of the available literature on the topic of neuroimaging use for health professions educational research. Neuroimaging has the potential to help validate/challenge established theoretical assumptions, lay foundations for new theory development, and provide insight into more efficient and efficacious training methods in health professions education. The use of these emerging technologies and databases appears ripe for the development of precision education and for understanding the learning curve of each individual learner in specific skills or cognitive engagement. Opportunities may also exist for establishing objective measures of competence.
Acknowledgments
The authors wish to thank Claire Levine, MS, ELS, Scientific Editor, Department of Anesthesiology and Critical Care Medicine, Johns Hopkins University, for her expert editing of the manuscript.
AppendicesAppendix 1- Search Strategy conducted on 4/4/2019 and updated on 7/7/2020.
| PubMed | |
| #1 | (‘Neuroimaging’[Mesh] OR ‘Electroencephalography’[Mesh] OR FMRI[tiab] OR EEG[tiab] OR ERP[tiab] OR fnirs[tiab] OR neuroimag*[tiab] OR ‘brain imaging’[tiab] OR ‘functional mri’[tiab] OR ‘functional magnetic resonance spectroscopy’[tiab] OR electroencephalography[tiab] OR ‘event related potentials’[tiab] OR ‘functional neuroimaging’[tiab] OR ‘Functional near infrared spectroscopy’[tiab]) |
| #2 | (‘Clinical Competence’[Mesh] OR ‘Psychomotor Performance’[Mesh] OR ‘Burnout, Psychological’[Mesh] OR ‘Burnout, Professional’[Mesh] OR ‘Sleepiness’[Mesh] OR ‘cognitive load’[tiab] OR clinical skill*[tiab] OR ‘clinical expertise’[tiab] OR ‘skills learning’[tiab] OR ‘skill acquisition’[tiab] OR surgical skill*[tiab] OR ‘clinical reasoning’[tiab] OR psychomotor skill*[tiab] OR procedural skill*[tiab] OR technical skill*[tiab] OR ‘diagnostic thinking’[tiab] OR ‘diagnostic reasoning’[tiab] OR ‘visual expertise’[tiab] OR burnout[tiab] OR sleepiness[tiab] OR fatigue[tiab] OR performance[tiab] OR competenc*[tiab] OR ‘mental workload’[tiab] OR memory[tiab] OR ‘problem solving’[tiab] OR medical error*[tiab] OR ‘patient safety’[tiab]) |
| #3 | (‘Surgeons’[MeSH] OR ‘Physicians’[MeSH] OR ‘Students, Medical’[Mesh] OR ‘Internship and Residency’[Mesh] OR ‘Clinical Clerkship’[Mesh] OR ‘premedical’[tiab] OR ‘pre-medical’[tiab] OR ‘clinical clerkship’[tiab] OR ‘resident’[tiab] OR ‘residents’[tiab] OR ‘residency’[tiab] OR PGY*[tiab] OR ‘post graduate year’[tiab] OR ‘postgraduate year’[tiab] OR ‘trainee’[tiab] OR ‘intern’[tiab] OR ‘interns’[tiab] OR ‘internship’[tiab] OR ‘house officer’[tiab] OR ‘house officers’[tiab] OR ‘houseofficer’[tiab] OR ‘house staff’[tiab] OR ‘housestaff’[tiab] OR ‘fellowship’[tiab] OR ‘fellow’[tiab] OR ‘fellows’[tiab] OR ‘undergraduate medical’[tiab] OR ‘medical student’[tiab] OR ‘medical students’[tiab] OR ‘Schools, Medical’[Mesh] OR medical school*[tiab] OR health science*[tiab] OR clinician*[tiab] OR surgeon*[tiab] OR physician[tiab] OR physicians[tiab] OR ‘health profession’[tiab] OR ‘health professionals’[tiab] OR ‘health professions’[tiab] OR doctor[tiab] OR doctors[tiab]) |
| #4 | (‘Education, Medical’[Mesh] OR ‘Education’[Mesh] OR educate[tiab] or education[tiab] OR educated[tiab] OR educational[tiab] OR curricula*[tiab] OR curriculum[tiab] OR train*[tiab] OR teach*[tiab] OR instruct*[tiab] OR mentor*[tiab] OR program*[tiab] OR pedagog*[tiab] OR workshop*[tiab] OR initiative*[tiab] OR seminar*[tiab] OR electives[tiab] OR ‘CME’[tiab] OR ‘faculty development’[tiab]) |
| #5 | #1 AND #2 AND #3 AND #4 |
| Cochrane | |
| #1 | (‘Neuroimaging’[Mesh] OR ‘Electroencephalography’[Mesh] OR FMRI OR EEG OR ERP OR fnirs OR neuroimag* OR ‘brain imaging’ OR ‘functional mri’ OR ‘functional magnetic resonance spectroscopy’ OR electroencephalography OR ‘event related potentials’ OR ‘functional neuroimaging’ OR ‘Functional near infrared spectroscopy’) |
| #2 | (‘Clinical Competence’[Mesh] OR ‘Psychomotor Performance’[Mesh] OR ‘Burnout, Psychological’[Mesh] OR ‘Burnout, Professional’[Mesh] OR ‘Sleepiness’[Mesh] OR ‘cognitive load’ OR clinical skill* OR ‘clinical expertise’ OR ‘skills learning’ OR ‘skill acquisition’ OR surgical skill* OR ‘clinical reasoning’ OR psychomotor skill* OR procedural skill* OR technical skill* OR ‘diagnostic thinking’ OR ‘diagnostic reasoning’ OR ‘visual expertise’ OR burnout OR sleepiness OR fatigue OR performance OR competenc* OR ‘mental workload’ OR memory OR ‘problem solving’ OR medical error* OR ‘patient safety’) |
| #3 | (‘Surgeons’[MeSH] OR ‘Physicians’[MeSH] OR ‘Students, Medical’[Mesh] OR ‘Internship and Residency’[Mesh] OR ‘Clinical Clerkship’[Mesh] OR ‘premedical’ OR ‘pre-medical’ OR ‘clinical clerkship’ OR ‘resident’ OR ‘residents’ OR ‘residency’ OR PGY* OR ‘post graduate year’ OR ‘postgraduate year’ OR ‘trainee’ OR ‘intern’ OR ‘interns’ OR ‘internship’ OR ‘house officer’ OR ‘house officers’ OR ‘houseofficer’ OR ‘house staff’ OR ‘housestaff’ OR ‘fellowship’ OR ‘fellow’ OR ‘fellows’ OR ‘undergraduate medical’ OR ‘medical student’ OR ‘medical students’ OR ‘Schools, Medical’[Mesh] OR medical school* OR health science* OR clinician* OR surgeon* OR physician OR physicians OR ‘health profession’ OR ‘health professionals’ OR ‘health professions’ OR doctor OR doctors) |
| #4 | (‘Education, Medical’[Mesh] OR ‘Education’[Mesh] OR educate or education OR educated OR educational OR curricula* OR curriculum OR train* OR teach* OR instruct* OR mentor* OR program* OR pedagog* OR workshop* OR initiative* OR seminar* OR electives OR ‘CME’ OR ‘faculty development’) |
| #5 | #1 AND #2 AND #3 AND #4 |
| Web of Science | |
| #1 | TS = (FMRI OR EEG OR ERP OR fnirs OR neuroimag* OR ‘brain imaging’ OR ‘functional mri’ OR ‘functional magnetic resonance spectroscopy’ OR electroencephalography OR ‘event related potentials’ OR ‘functional neuroimaging’ OR ‘Functional near infrared spectroscopy’) |
| #2 | TS = (‘cognitive load’ OR clinical skill* OR ‘clinical expertise’ OR ‘skills learning’ OR ‘skill acquisition’ OR surgical skill* OR ‘clinical reasoning’ OR psychomotor skill* OR procedural skill* OR technical skill* OR ‘diagnostic thinking’ OR ‘diagnostic reasoning’ OR ‘visual expertise’ OR burnout OR sleepiness OR fatigue OR performance OR competenc* OR ‘mental workload’ OR memory OR ‘problem solving’ OR medical error* OR ‘patient safety’) |
| #3 | TS = (‘premedical’ OR ‘pre-medical’ OR ‘clinical clerkship’ OR ‘resident’ OR ‘residents’ OR ‘residency’ OR PGY* OR ‘post graduate year’ OR ‘postgraduate year’ OR ‘trainee’ OR ‘intern’ OR ‘interns’ OR ‘internship’ OR ‘house officer’ OR ‘house officers’ OR ‘houseofficer’ OR ‘house staff’ OR ‘housestaff’ OR ‘fellowship’ OR ‘fellow’ OR ‘fellows’ OR ‘undergraduate medical’ OR ‘medical student’ OR ‘medical students’ OR ‘medical school*’ OR ‘health science*’ OR clinician* OR surgeon* OR physician OR physicians OR ‘health profession’ OR ‘health professionals’ OR ‘health professions’ OR doctor OR doctors) |
| #4 | TS = (educate OR education OR educated OR educational OR curricula* OR curriculum OR train* OR teach* OR instruct* OR mentor* OR program* OR pedagog* OR workshop* OR initiative* OR seminar* OR electives OR CME OR ‘faculty development’) |
| #5 | #1 AND #2 AND #3 AND #4 |
| Embase | |
| #1 | ‘neuroimaging’/exp OR ‘electroencephalography’/exp OR (FMRI OR EEG OR ERP OR fnirs OR neuroimag* OR ‘brain imaging’ OR ‘functional mri’ OR ‘functional magnetic resonance spectroscopy’ OR electroencephalography OR ‘event related potentials’ OR ‘functional neuroimaging’ OR ‘Functional near infrared spectroscopy’):ti,ab |
| #2 | ‘clinical competence’/exp OR ‘psychomotor performance’/exp OR ‘burnout’/exp OR (‘cognitive load’ OR ‘clinical skill*’ OR ‘clinical expertise’ OR ‘skills learning’ OR ‘skill acquisition’ OR ‘surgical skill*’ OR ‘clinical reasoning’ OR ‘psychomotor skill*’ OR ‘procedural skill*’ OR ‘technical skill*’ OR ‘diagnostic thinking’ OR ‘diagnostic reasoning’ OR ‘visual expertise’ OR burnout OR sleepiness OR fatigue OR performance OR competenc* OR ‘mental workload’ OR memory OR ‘problem solving’ OR ‘medical error*’ OR ‘patient safety’):ti,ab |
| #3 | ‘medical education’/exp OR ‘surgeon’/exp OR ‘physician’/exp OR ‘health student’/exp OR ‘resident’/exp OR (premedical OR pre-medical OR ‘clinical clerkship’ OR resident OR residents OR residency OR PGY* OR ‘post graduate year’ OR ‘postgraduate year’ OR trainee OR intern OR interns OR internship OR ‘house officer’ OR ‘house officers’ OR ‘houseofficer’ OR ‘house staff’ OR housestaff OR fellowship OR fellow OR fellows OR ‘undergraduate medical’ OR ‘medical student’ OR ‘medical students’ OR ‘medical school*’ OR ‘health science*’ OR clinician* OR surgeon* OR physician OR physicians OR ‘health profession’ OR ‘health professionals’ OR ‘health professions’ OR doctor OR doctors):ti,ab |
| #4 | ‘medical education’/exp OR ‘education’/exp OR (educate OR education OR educated OR educational OR curricula* OR curriculum OR train* OR teach* OR instruct* OR mentor* OR program* OR pedagog* OR workshop* OR initiative* OR seminar* OR electives OR CME OR ‘faculty development’):ti,ab |
| #5 | #1 AND #2 AND #3 AND #4 |
| ERIC | |
| #1 | (FMRI OR EEG OR ERP OR fnirs OR neuroimag* OR ‘brain imaging’ OR ‘functional mri’ OR ‘functional magnetic resonance spectroscopy’ OR electroencephalography OR ‘event related potentials’ OR ‘functional neuroimaging’ OR ‘Functional near infrared spectroscopy’) |
| #2 | (DE ‘Medical Evaluation’) OR (DE ‘Psychomotor Skills’) OR (DE ‘Burnout’) OR ‘cognitive load’ OR ‘clinical skill*’ OR ‘clinical expertise’ OR ‘skills learning’ OR ‘skill acquisition’ OR ‘surgical skill*’ OR ‘clinical reasoning’ OR ‘psychomotor skill*’ OR ‘procedural skill*’ OR ‘technical skill*’ OR ‘diagnostic thinking’ OR ‘diagnostic reasoning’ OR ‘visual expertise’ OR burnout OR sleepiness OR fatigue OR performance OR competenc* OR ‘mental workload’ OR memory OR ‘problem solving’ OR ‘medical error*’ OR ‘patient safety’) |
| #3 | (DE ‘Medical Education’) OR (DE ‘Medical Schools’) OR (DE ‘Physicians’) OR (DE ‘Medical Students’) OR ‘premedical’ OR ‘pre-medical’ OR ‘clinical clerkship’ OR resident OR residents OR residency OR PGY* OR ‘post graduate year’ OR ‘postgraduate year’ OR trainee OR intern OR interns OR internship OR ‘house officer’ OR ‘house officers’ OR houseofficer OR ‘house staff’ OR housestaff OR fellowship OR fellow OR fellows OR ‘undergraduate medical’ OR ‘medical student’ OR ‘medical students’ OR ‘medical school*’ OR ‘health science*’ OR clinician* OR surgeon* OR physician OR physicians OR ‘health profession’ OR ‘health professionals’ OR ‘health professions’ OR doctor OR doctors) |
| #4 | (DE ‘Medical Education’) OR (DE ‘Education’) OR educate or education OR educated OR educational OR curricula* OR curriculum OR train* OR teach* OR instruct* OR mentor* OR program* OR pedagog* OR workshop* OR initiative* OR seminar* OR electives OR ‘CME’ OR ‘faculty development’) |
| #5 | #1 AND #2 AND #3 AND #4 |
Appendix 2: Summary table for included studies in alphabetical order by first author.
| Authors | Year | Country | Primary Author Institution | Design | Neuroimaging Modality | Specialty | Skill |
|---|---|---|---|---|---|---|---|
| Aggarwal et al. | 2008 | UK | Department of Biosurgery & Surgical Technology, Imperial College London | Review | N/A | surgery | REVIEW psychomotor skill |
| Akimoto et al. | 2015 | Japan | Center for Advanced Medical Initiatives, Kyushu University | Non-experimental | Other * | surgery | psychomotor skill |
| Aksoy et al. | 2019 | Turkey | Department of Biomedical Device Technology, Acıbadem Mehmet Ali Aydınlar University | Non-experimental | fNIRS | healthcare professionals | psychomotor skill |
| Anderson et al. | 2019 | Canada | Department of Community Health Sciences, Cumming School of Medicine, University of Calgary | RCT | EEG | health sciences students | declarative clinical knowledge |
| Andreu-Perez et al. | 2016 | UK | The Hamlyn Centre, Imperial College London | Non-experimental | fNIRS/OT | surgery | psychomotor skill |
| Bahrami et al. | 2014 | Canada | Institute of Biomaterials and Biomedical Engineering, University of Toronto | Non-experimental | fMRI | surgery | psychomotor skill |
| Bahrami et al. | 2011 | Canada | Institute of Biomaterials and Biomedical Engineering, University of Toronto, and Keenan Research Centre of the Li Ka Shing Knowledge Institute at St. Michael’s Hospital, Toronto | Non-experimental | fMRI | surgery | psychomotor skill |
| Bernier et al. | 2016 | Canada | Sherbrooke University Hospital Center (CHUS) | Non-experimental | fMRI | medical students | declarative clinical knowledge |
| Bhatt et al. | 2016 | Ireland | Department of Surgery, University of Dublin, Trinity College, at the Adelaide and Meath Hospital | Review | N/A | surgery | REVIEW effects of aging on surgeons |
| Bocci et al. | 2013 | Italy | Department of Neuroscience, Unit of Neurology, Pisa University Medical School | Non-experimental | EEG | surgery | psychomotor skill |
| Brod et al. | 2016 | Germany | The Center for Lifespan Psychology, Max Planck Institute for Human Development | Non-experimental | fMRI | medical students | declarative clinical knowledge |
| Chang et al. | 2016 | South Korea | Department of Medical Humanities, Korea University College of Medicine | Non-experimental | fMRI | medical students | clinical reasoning |
| Ciechanski et al. | 2019 | Canada | Faculty of Medicine and Dentistry, University of Alberta | RCT | EEG | surgery | psychomotor skill |
| Crewther et al. | 2016 | UK | The Hamlyn Centre for Robotic Surgery, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill |
| De Andrade et al. | 2016 | Brazil | Faculty of Medicine, Department of Paediatric, University of Sao Paulo | Non-experimental | fMRI | pediatrics | well-being |
| Downar et al. | 2011 | USA | Human Neuroimaging Laboratory, Virginia Tech Carilion Research Institute and Department of Physics, Virginia Tech | Non-experimental | fMRI | non-surgical physicians | clinical reasoning |
| Durning et al. | 2013 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2014 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2015 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2016 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2013 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2012 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Durning et al. | 2015 | USA | Department of Medicine, Uniformed Services University of the Health Sciences | Non-experimental | fMRI | internal medicine | clinical reasoning |
| Duty et al. | 2012 | USA | Institute for Urology and Center of Neurosciences, Feinstein Institute for Medical Research North Shore–Long Island Jewish Health System | Non-experimental | PET | surgery | psychomotor skill |
| Garbens et al. | 2019 | Canada | Department of Surgery, St. Michael’s Hospital, University of Toronto | Non-experimental | fMRI | surgery | psychomotor skill |
| Guru et al. | 2015 | USA | Department of Urology, Roswell Park Cancer Institute, Brain Computer Interface Laboratory, Department of Mechanical & Aerospace Engineering, University at Buffalo | Non-experimental | EEG | surgery | psychomotor skill |
| Guru et al. | 2015 | USA | Department of Urology, Applied Technology Laboratory for Advanced Surgery (ATLAS) Program at Roswell Park Cancer Institute | Non-experimental | EEG | surgery | psychomotor skill |
| Hruska et al. | 2015 | Canada | Department of Community Health Sciences, Cumming School of Medicine, University of Calgary | Non-experimental | fMRI | gastroenterology | diagnostic thinking |
| Hruska et al. | 2015 | Canada | Department of Community Health Sciences, Cumming School of Medicine, University of Calgary | Non-experimental | fMRI | gastroenterology | diagnostic thinking |
| Hussein et al. | 2016 | USA | Applied Technology Laboratory for Advanced Surgery (ATLAS) Program, Roswell Park Cancer Institute, Buffalo | Non-experimental | EEG | surgery | psychomotor skill |
| James et al. | 2011 | UK | Department of Surgery and Cancer & Hamlyn Centre for Robotic Surgery, Imperial College | Non-experimental | fNIRS | gastroenterology | visuospatial skill |
| Kahol et al. | 2011 | USA | Human Machine Symbiosis Laboratory, School of Biological and Health Systems Engineering, Arizona State University | Non-experimental | EEG | surgery | psychomotor skill |
| Karabanov et al. | 2019 | Denmark | Danish Research Centre for Magnetic Resonance, Centre for Functional and Diagnostic Imaging and Research, Copenhagen University Hospital | RCT | fMRI | surgery | psychomotor skill |
| Khoe et al. | 2020 | Singapore | Yong Loo Lin School of Medicine, National University of Singapore | RCT | fNIRS | surgery | psychomotor skill |
| Leff et al. | 2008 | UK | Royal Wolfson Image Computing Laboratory and Department of Biosurgery and Surgical Technology, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill |
| Leff et al. | 2015 | UK | Hamlyn Centre for Robotic Surgery, Imperial College London | Randomized crossover | fNIRS/OT | surgery | visuospatial skill |
| Leff et al. | 2008 | UK | Royal Wolfson Image Computing Laboratory and Department of Biosurgery and Surgical Technology, Imperial College London | Review | N/A | surgery | REVIEW psychomotor skill |
| Leff et al. | 2008 | UK | Royal Wolfson Image Computing Laboratory and Department of Biosurgery and Surgical Technology, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill |
| Leff et al. | 2010 | UK | Royal Wolfson Image Computing Laboratory and Department of Biosurgery and Surgical Technology, Imperial College London | Non-experimental | fNIRS | surgery | fatigue |
| Leff et al. | 2017 | UK | Hamlyn Centre for Robotic Surgery, Department of Biosurgery and Surgical Technology, Imperial College London | Non-experimental | fNIRS/OT | surgery | clinical reasoning |
| Li et al. | 2020 | China | Spinal Division of Orthopedic and Traumatology Center, Affiliated Hospital of Guangdong Medical University | Non-experimental | EEG | surgery | psychomotor skill |
| Maddox et al. | 2015 | USA | Department of Urology, Tulane University School of Medicine | Non-experimental | EEG | surgery | psychomotor skill |
| Mazur et al. | 2017 | USA | Department of Radiation Oncology, University of North Carolina | Non-experimental | EEG | radiation oncology | clinical reasoning |
| Mazur et al. | 2016 | USA | Department of Radiation Oncology, University of North Carolina | Non-experimental | EEG | medical trainees | psychomotor skill |
| Miura et al. | 2015 | Japan | Department of Modern Mechanical Engineering, Waseda University | Non-experimental | fNIRS | surgery | visuospatial skill |
| Modi et al. | 2019 | UK | Department of Surgery and Cancer & Hamlyn Centre for Robotic Surgery, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill |
| Modi et al. | 2018 | UK | Department of Surgery and Cancer & Hamlyn Centre for Robotic Surgery, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill |
| Modi et al. | 2017 | UK | Department of Surgery and Cancer & Hamlyn Centre for Robotic Surgery, Imperial College London | Review | N/A | surgery | REVIEW psychomotor skill |
| Modi et al. | 2017 | UK | Department of Surgery and Cancer & Hamlyn Centre for Robotic Surgery, Imperial College London | Review | N/A | surgery | REVIEW psychomotor skill |
| Morales et al. | 2019 | Spain | Mind, Brain, and Behavior Research Center, University of Granada | Non-experimental | EEG | surgery | psychomotor skill |
| Morris et al. | 2015 | Ireland | Education Division and Department of Surgery, School of Medicine, Trinity College | Non-experimental | fMRI | surgery | psychomotor skill |
| Ndaro et al. | 2018 | China | Department of Biomedical Engineering, School of Medical Instrument and Food Engineering, University of Shanghai for Science and Technology | Non-experimental | EEG | surgery | psychomotor skill |
| Nemani et al. | 2018 | USA | Rensselaer Polytechnic Institute | RCT | fNIRS | surgery | psychomotor skill |
| Nishida et al. | 2017 | Japan | Department of Psychiatry, Jichi Medical University & Faculty of Sports Science, Waseda University | Randomized crossover | fNIRS | psychiatry | fatigue |
| Ohuchida et al. | 2009 | Japan | Department of Advanced Medical Initiatives, Faculty of Medical Sciences, Kyushu University | Non-experimental | fNIRS | surgery | psychomotor skill |
| Pelizzo et al. | 2020 | Italy | Department of Pediatric Surgery, ‘Vittore Buzzi’ Children’s Hospital, University of Milano | RCT | fMRI | surgery | psychomotor skill |
| Rotgans et al. | 2019 | Netherlands | Institute of Medical Education Research Rotterdam, Erasmus Medical Center, Rotterdam | Non-experimental | fNIRS | medical students – | clinical reasoning |
| Rourke et al. | 2016 | Canada | Department of Medicine, University of Alberta | Non-randomized controlled |
EEG | cardiology and pulmonology | clinical reasoning |
| Shafiei et al. | 2018 | USA | Department of Urology, Applied Technology Laboratory for Advanced Surgery (ATLAS) Program at Roswell Park Cancer Institute | Non-experimental | EEG | surgery | psychomotor skill |
| Shetty et al. | 2016 | UK | Hamlyn Centre for Robotic Surgery, Imperial College London | Non-experimental | fNIRS | surgery | psychomotor skill development |
| Shewokis et al. | 2017 | USA | Nutrition Sciences Department, College of Nursing and Health Professions, School of Biomedical Engineering, Science and Health Systems, Drexel University | RCT | fNIRS | surgery | psychomotor skill |
| Turk et al. | 2018 | USA | VA Boston Healthcare System & Boston University School of Medicine |
Non-experimental | EEG | medical students | declarative clinical knowledge |
| Veroude et al. | 2013 | Netherlands | Department of Educational Neuroscience, Faculty of Psychology and Education VU University Amsterdam | Non-experimental | fMRI | medical students | cognitive/emotional control |
| Wanzel et al. | 2007 | Canada | Department of Surgery, University of Toronto | Non-experimental | fMRI | surgery | visuospatial skill |
| Xu et al. | 2018 | China | Department of Military Psychology, Army Medical University, Chongqing, China. | RCT | EEG | medical students | well-being |
| Xu et al. | 2019 | USA | Center for Research and Innovation in Systems Safety, Vanderbilt University Medical Center | Non-experimental | fNIRS | anesthesiology | crisis event management team skills |
| Zhu et al. | 2011 | Hong Kong | Institute of Human Performance, The University of Hong Kong | Non-randomized controlled |
EEG | surgery | psychomotor skill |
EEG, electroencephalogram; fMRI, functional magnetic resonance imaging; fNIRS, functional near-infrared spectroscopy; NA, not applicable; OT, optical topography; RCT, randomized controlled trial.
* Other: Brain electric activity monitoring system designed by the researchers
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Antonenko PD, van Gog T, Paas F.. Implications of neuroimaging for educational research, in Handbook of research on educational communications and technology. New York, NY: Springer; 2014. 51–63. [Google Scholar]
- [2].Aggarwal R, Leong J, Leff D, et al. New technologies for the surgical curriculum. World J Surg. 2008;32(2):213–18. [DOI] [PubMed] [Google Scholar]
- [3].Bhatt N, Morris M, O’Neil A, et al. When should surgeons retire? Br J Surg. 2016;103(1):35–42. [DOI] [PubMed] [Google Scholar]
- [4].Modi HN, Singh H, Yang G-Z, et al. A decade of imaging surgeons’ brain function (part I): terminology, techniques, and clinical translation. Surgery. 2017;162(5):1121–1130. [DOI] [PubMed] [Google Scholar]
- [5].Modi HN, Singh H, Yang GZ, et al. A decade of imaging surgeons’ brain function (part II): a systematic review of applications for technical and nontechnical skills assessment. Surgery (USA). 2017;162(5):1130–1139. [DOI] [PubMed] [Google Scholar]
- [6].Leff DR, Leong JJH, Aggarwal R, et al. Could variations in technical skills acquisition in surgery be explained by differences in cortical plasticity? Ann Surg. 2008;247(3):540–543. [DOI] [PubMed] [Google Scholar]
- [7].Thomas A, Lubarsky S, Varpio L, et al. Scoping reviews in health professions education: challenges, considerations and lessons learned about epistemology and methodology. Adv Health Sci Educ. 2019;24(1):1–14. [DOI] [PubMed] [Google Scholar]
- [8].Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- [9].Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Peters Md, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146. [DOI] [PubMed] [Google Scholar]
- [11].Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. [DOI] [PubMed] [Google Scholar]
- [12].Wanzel KR, Anastakis DJ, McAndrews MP, et al. Visual-spatial ability and fMRI cortical activation in surgery residents. Am J Surg. 2007;193(4):507–510. [DOI] [PubMed] [Google Scholar]
- [13].Leff DR, Elwell CE, Orihuela-Espina F, et al. Changes in prefrontal cortical behaviour depend upon familiarity on a bimanual co-ordination task: an fNIRS study. Neuroimage. 2008;39(2):805–813. [DOI] [PubMed] [Google Scholar]
- [14].Leff DR, Orihuela-Espina F, Atallah L, et al. Functional prefrontal reorganization accompanies learning-associated refinements in surgery: a manifold embedding approach. Comput Aided Surg. 2008;13(6):325–339. [DOI] [PubMed] [Google Scholar]
- [15].Ohuchida K, Kenmotsu H, Yamamoto A, et al. The frontal cortex is activated during learning of endoscopic procedures. Surg Endosc. 2009;23(10):2296–2301. [DOI] [PubMed] [Google Scholar]
- [16].Leff DR, Orihuela-Espina F, Athanasiou T, et al. “Circadian cortical compensation”: a longitudinal study of brain function during technical and cognitive skills in acutely sleep-deprived surgical residents. Ann Surg. 2010;252(6):1082–1090. [DOI] [PubMed] [Google Scholar]
- [17].Bahrami P, Schweizer TA, Tam F, et al. Functional MRI-compatible laparoscopic surgery training simulator. Magn Reson Med. 2011;65(3):873–881. [DOI] [PubMed] [Google Scholar]
- [18].Downar J, Bhatt M, Montague PR. Neural correlates of effective learning in experienced medical decision-makers. PLoS One. 2011;6(11):e27768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].James DR, Orihuela-Espina F, Leff DR, et al. The ergonomics of natural orifice translumenal endoscopic surgery (NOTES) navigation in terms of performance, stress, and cognitive behavior. Surgery. 2011;149(4):525–533. [DOI] [PubMed] [Google Scholar]
- [20].Kahol K, Smith M, Brandenberger J, et al. Impact of fatigue on neurophysiologic measures of surgical residents. J Am Coll Surg. 2011;213(1):29–34. discussion 34. 10.1016/j.jamcollsurg.2011.03.028. [DOI] [PubMed] [Google Scholar]
- [21].Zhu FF, Poolton JM, Wilson MR, et al. Implicit motor learning promotes neural efficiency during laparoscopy. Surg Endosc. 2011;25(9):2950–2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Durning SJ, Graner J, Artino AR, et al. Using functional neuroimaging combined with a think-aloud protocol to explore clinical reasoning expertise in internal medicine. Mil Med. 2012;177(9 Suppl):72–78. [DOI] [PubMed] [Google Scholar]
- [23].Duty B, Andonian S, Ma Y, et al. Correlation of laparoscopic experience with differential functional brain activation: a positron emission tomography study with oxygen 15–labeled water. Arch Surg. 2012;147(7):627–632. [DOI] [PubMed] [Google Scholar]
- [24].Bocci T, Moretto C, Tognazzi S, et al. How does a surgeon’s brain buzz? An EEG coherence study on the interaction between humans and robot. Behavioral and Brain Functions. 2013;9(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Durning SJ, Artino Jr AR, Beckman TJ, et al. Does the think-aloud protocol reflect thinking? Exploring functional neuroimaging differences with thinking (answering multiple choice questions) versus thinking aloud. Med Teach. 2013;35(9):720–726. [DOI] [PubMed] [Google Scholar]
- [26].Durning SJ, Costanzo M, Artino AR, et al. Functional neuroimaging correlates of burnout among internal medicine residents and faculty members. Front Psychiatry. 2013;4:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Veroude K, Jolles J, Knežević M, et al. Anterior cingulate activation during cognitive control relates to academic performance in medical students. Trends in Neuroscience and Education. 2013;2(3–4):100–106. [Google Scholar]
- [28].Bahrami P, Graham SJ, Grantcharov TP, et al. Neuroanatomical correlates of laparoscopic surgery training. Surg Endosc. 2014;28(7):2189–2198. [DOI] [PubMed] [Google Scholar]
- [29].Durning SJ, Capaldi II VF, Artino AR, et al. A pilot study exploring the relationship between internists’ self-reported sleepiness, performance on multiple-choice exam items and prefrontal cortex activity. Med Teach. 2014;36(5):434–440. [DOI] [PubMed] [Google Scholar]
- [30].Akimoto S, Ohdaira T, Nakamura S, et al. The efficiency of a modified real-time wireless brain electric activity calculator to reveal the subliminal psychological instability of surgeons that possibly leads to errors in surgical procedures. Surg Technol Int. 2015;26:25–30. [PubMed] [Google Scholar]
- [31].Durning SJ, Costanzo ME, Artino AR, et al. Neural basis of nonanalytical reasoning expertise during clinical evaluation. Brain Behav. 2015;5(3):e00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Durning SJ, Kelly W, Costanzo ME, et al. Relationship of neuroimaging to typical sleep times during a clinical reasoning task: a pilot study. Mil Med. 2015;180(4 Suppl):129–135. [DOI] [PubMed] [Google Scholar]
- [33].Guru KA, et al. Cognitive skills assessment during robot‐assisted surgery: separating the wheat from the chaff. BJU Int. 2015;115(1):166–174. [DOI] [PubMed] [Google Scholar]
- [34].Guru KA, Shafiei SB, Khan A, et al. Understanding cognitive performance during robot-assisted surgery. Urology. 2015;86(4):751–757. [DOI] [PubMed] [Google Scholar]
- [35].Leff DR, James DRC, Orihuela-Espina F, et al. The impact of expert visual guidance on trainee visual search strategy, visual attention and motor skills. Front Hum Neurosci. 2015;9:526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Maddox MM, Lopez A, Mandava SH, et al. Electroencephalographic monitoring of brain wave activity during laparoscopic surgical simulation to measure surgeon concentration and stress: can the student become the master? J Endourol. 2015;29(12):1329–1333. [DOI] [PubMed] [Google Scholar]
- [37].Miura S, Kobayashi Y, Kawamura K, et al. Brain activation in parietal area during manipulation with a surgical robot simulator. Int J Comput Assist Radiol Surg. 2015;10(6):783–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Morris MC, Frodl T, D’Souza A, et al. Assessment of competence in surgical skills using functional magnetic resonance imaging: a feasibility study. J Surg Educ. 2015;72(2):198–204. [DOI] [PubMed] [Google Scholar]
- [39].Andreu-Perez J, Leff DR, Shetty K, et al. Disparity in frontal lobe connectivity on a complex bimanual motor task aids in classification of operator skill level. Brain Connect. 2016;6(5):375–388. [DOI] [PubMed] [Google Scholar]
- [40].Bernier M, Gauvreau C, Theriault D, et al. Increased BOLD activation in the left parahippocampal cortex after 1 year of medical school: an association with cumulative verbal memory learning. Neuroreport. 2016;27(1):45–49. [DOI] [PubMed] [Google Scholar]
- [41].Brod G, Lindenberger U, Wagner AD, et al. Knowledge acquisition during exam preparation improves memory and modulates memory formation. J Neurosci. 2016;36(31):8103–8111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Chang HJ, Kang J, Ham B-J, et al. A functional neuroimaging study of the clinical reasoning of medical students. Adv Health Sci Educ Theory Pract. 2016;21(5):969–982. [DOI] [PubMed] [Google Scholar]
- [43].Crewther BT, Shetty K, Jarchi D, et al. Skill acquisition and stress adaptations following laparoscopic surgery training and detraining in novice surgeons. Surg Endosc. 2016;30(7):2961–2968. [DOI] [PubMed] [Google Scholar]
- [44].de Andrade AP, Amaro E, Farhat SCL, et al. Higher burnout scores in paediatric residents are associated with increased brain activity during attentional functional magnetic resonance imaging task. Acta Paediatr. 2016;105(6):705–713. [DOI] [PubMed] [Google Scholar]
- [45].Durning SJ, Costanzo ME, Beckman TJ, et al. Functional neuroimaging correlates of thinking flexibility and knowledge structure in memory: exploring the relationships between clinical reasoning and diagnostic thinking. Med Teach. 2016;38(6):570–577. [DOI] [PubMed] [Google Scholar]
- [46].Hruska P, Hecker KG, Coderre S, et al. Hemispheric activation differences in novice and expert clinicians during clinical decision making. Adv Health Sci Educ Theory Pract. 2016;21(5):921–933. [DOI] [PubMed] [Google Scholar]
- [47].Hruska P, Krigolson O, Coderre S, et al. Working memory, reasoning, and expertise in medicine—insights into their relationship using functional neuroimaging. Adv Health Sci Educ. 2016;21(5):935–952. [DOI] [PubMed] [Google Scholar]
- [48].Hussein AA, Shafiei SB, Sharif M, et al. Technical mentorship during robot-assisted surgery: a cognitive analysis. BJU Int. 2016;118(3):429–436. [DOI] [PubMed] [Google Scholar]
- [49].Mazur LM, Mosaly PR, Moore C, et al. Toward a better understanding of task demands, workload, and performance during physician-computer interactions. J Am Med Inform Assoc. 2016;23(6):1113–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Rourke L, Cruikshank LC, Shapke L, et al. A neural marker of medical visual expertise: implications for training. Adv Health Sci Educ Theory Pract. 2016;21(5):953–966. [DOI] [PubMed] [Google Scholar]
- [51].Shetty K, Leff DR, Orihuela-Espina F, et al. Persistent prefrontal engagement despite improvements in laparoscopic technical skill. JAMA Surg. 2016;151(7):682–684. [DOI] [PubMed] [Google Scholar]
- [52].Leff DR, Yongue G, Vlaev I, et al. “Contemplating the next maneuver”: functional neuroimaging reveals intraoperative decision-making strategies. Ann Surg. 2017;265(2):320–330. [DOI] [PubMed] [Google Scholar]
- [53].Mazur LM, Campbell A, Comitz E, et al. Positive effects of neurofeedback intervention on radiation oncology physicians’ workload during go/no-go performance test. Le travail humain. 2017;80(1):113–132. [Google Scholar]
- [54].Nishida M, Kikuchi S, Miwakeichi F, et al. Night duty and decreased brain activity of medical residents: a wearable optical topography study. Med Educ Online. 2017;22(1):1379345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Shewokis PA, Shariff FU, Liu Y, et al. Acquisition, retention and transfer of simulated laparoscopic tasks using fNIR and a contextual interference paradigm. Am J Surg. 2017;213(2):336–345. [DOI] [PubMed] [Google Scholar]
- [56].Modi HN, Singh H, Orihuela-Espina F, et al. Temporal stress in the operating room: brain engagement promotes “Coping” and disengagement prompts “Choking”. Ann Surg. 2018;267(4):683–691. [DOI] [PubMed] [Google Scholar]
- [57].Ndaro NZ, Wang SY. Effects of fatigue based on electroencephalography signal during laparoscopic surgical simulation. Minim Invasive Surg. 2018;2018:2389158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Shafiei SB, Hussein AA, Muldoon SF, et al. Functional brain states measure mentor-trainee trust during robot-assisted surgery. Sci Rep. 2018;8(1):3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Turk KW, Elshaar AA, Deason RG, et al. Late positive component event-related potential amplitude predicts long-term classroom-based learning. J Cogn Neurosci. 2018;30(9):1323–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Xu YY, Feng Z-Q, Xie Y-J, et al. Frontal alpha EEG asymmetry before and after positive psychological interventions for medical students. Front Psychiatry. 2018;9:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Aksoy E, Izzetoglu K, Baysoy E, et al. performance monitoring via functional near infrared spectroscopy for virtual reality based basic life support training. Front Neurosci. 2019;13:1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Anderson SJ, Jamniczky HA, Krigolson OE, et al. Quantifying two-dimensional and three-dimensional stereoscopic learning in anatomy using electroencephalography. NPJ Sci Learn. 2019;4(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Ciechanski P, Kirton A, Wilson B, et al. Electroencephalography correlates of transcranial direct-current stimulation enhanced surgical skill learning: a replication and extension study. Brain Res. 2019;1725:146445. [DOI] [PubMed] [Google Scholar]
- [64].Karabanov AN, Irmen F, Madsen KH, et al. Getting to grips with endoscopy - learning endoscopic surgical skills induces bi-hemispheric plasticity of the grasping network. Neuroimage. 2019;189:32–44. [DOI] [PubMed] [Google Scholar]
- [65].Modi HN, Singh H, Fiorentino F, et al. Association of residents’ neural signatures with stress resilience during surgery. JAMA Surg. 2019;154(10):e192552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Morales JM, Ruiz-Rabelo JF, Diaz-Piedra C, et al. Detecting mental workload in surgical teams using a wearable single-channel electroencephalographic device. J Surg Educ. 2019;76(4):1107–1115. [DOI] [PubMed] [Google Scholar]
- [67].Nemani A, Kruger U, Cooper CA, et al. Objective assessment of surgical skill transfer using non-invasive brain imaging. Surg Endosc. 2019;33(8):2485–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Rotgans JI, Schmidt HG, Rosby LV, et al. Evidence supporting dual-process theory of medical diagnosis: a functional near-infrared spectroscopy study. Med Educ. 2019;53(2):143–152. [DOI] [PubMed] [Google Scholar]
- [69].Xu J, Slagle JM, Banerjee A, et al. Use of a portable functional near-infrared spectroscopy (fnirs) system to examine team experience during crisis event management in clinical simulations. Front Hum Neurosci. 2019;13:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Garbens A, Armstrong BA, Louridas M, et al. Brain activation during laparoscopic tasks in high- and low-performing medical students: a pilot fMRI study. Surg Endosc. 2020;34(11):4837–4845. [DOI] [PubMed] [Google Scholar]
- [71].Khoe HCH, Low JW, Wijerathne S, et al. Use of prefrontal cortex activity as a measure of learning curve in surgical novices: results of a single blind randomised controlled trial. Surg Endosc. 2020;34(12):5604–5615. [DOI] [PubMed] [Google Scholar]
- [72].Pelizzo G, Cardinali L, Bonanno L, et al. Training skills in minimally invasive, robotic and open surgery: brain activation as an opportunity for learning. Eur Surg Res. 2020;61(1):34–50. [DOI] [PubMed] [Google Scholar]
- [73].Li G, Li H, Pu J, et al. Effect of brain alpha oscillation on the performance in laparoscopic skills simulator training. Surg Endosc. 2021;35(2):584–592. [DOI] [PubMed] [Google Scholar]
- [74].Bocci T, Moretto C, Tognazzi S, et al. How does a surgeon’s brain buzz? An EEG coherence study on the interaction between humans and robot. Behav Brain Funct. 2013;9(1):14. 10.1186/1744-9081-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Li G, Li H, Pu J, et al. Effect of brain alpha oscillation on the performance in laparoscopic skills simulator training. Surg Endosc. 2020. [DOI] [PubMed] [Google Scholar]
- [76].Pelizzo G, Cardinali L, Bonanno L, et al. Training skills in minimally invasive, robotic and open surgery: brain activation as an opportunity for learning. Eur Surg Res. 2020;1–16. [DOI] [PubMed] [Google Scholar]
- [77].Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comp Biomed Res. 1996;29(3):162–173. [DOI] [PubMed] [Google Scholar]
- [78].Woolrich MW, Ripley BD, Brady M, et al. Temporal autocorrelation in univariate linear modeling of FMRI data. Neuroimage. 2001;14(6):1370–1386. [DOI] [PubMed] [Google Scholar]
- [79].Woolrich MW, Behrens TEJ, Beckmann CF, et al. Multilevel linear modelling for FMRI group analysis using Bayesian inference. Neuroimage. 2004;21(4):1732–1747. [DOI] [PubMed] [Google Scholar]
- [80].Jenkinson M, Bannister P, Brady M, et al. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. 2002;17(2):825–841. [DOI] [PubMed] [Google Scholar]
- [81].Huppert TJ, Diamond SG, Franceschini MA, et al. HomER: a review of time-series analysis methods for near-infrared spectroscopy of the brain. Appl Opt. 2009;48(10):D280–D298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Koh PH, Glaser DE, Flandin G, et al. Functional optical signal analysis: a software tool for near-infrared spectroscopy data processing incorporating statistical parametric mapping. J Biomed Opt. 2007;12(6):64010. [DOI] [PubMed] [Google Scholar]
- [83].Orihuela-Espina F, Leff DR, James DA, et al. ICNA: a software tool for manifold embedded based analysis of functional near infrared spectroscopy data. Neuroimage. 2009;47(47):S59. [Google Scholar]
- [84].Orihuela-Espina F, Leff DR, James DRC, et al. Imperial college near infrared spectroscopy neuroimaging analysis framework. Neurophotonics. 2017;5(1):11011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Delorme A, Makeig S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods. 2004;134(1):9–21. [DOI] [PubMed] [Google Scholar]
- [86].Glover GH. Overview of functional magnetic resonance imaging. Neurosurg Clinics. 2011;22(2):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Smith EE, Jonides J. Storage and executive processes in the frontal lobes. Science. 1999;283(5408):1657–1661. [DOI] [PubMed] [Google Scholar]
- [88].Neubauer AC, Fink A. Intelligence and neural efficiency. Neurosci Biobehav Rev. 2009;33(7):1004–1023. [DOI] [PubMed] [Google Scholar]
- [89].Kahneman D, Frederick S. Representativeness revisited: attribute substitution in intuitive judgment. Heuristics and biases: the psychology of intuitive judgment. 2002;49:81. [Google Scholar]
- [90].Pusic MV, Boutis K, Pecaric MR, et al. A primer on the statistical modelling of learning curves in health professions education. Adv Health Sci Educ. 2017;22(3):741–759. [DOI] [PubMed] [Google Scholar]


