Abstract
Volumetric-modulated arc therapy (VMAT) is a novel treatment strategy that protects normal tissues and enhances target volume coverage during radiotherapy.
This study aimed to clarify whether VMAT is superior to intensity-modulated radiotherapy (IMRT) in treatment planning for left-sided breast cancer patients after modified radical mastectomy.
Left-sided breast cancer patients treated with modified radical mastectomy were eligible for analysis. The dose distribution of both planning target volume and organs at risk were analyzed by using dose volume histograms.
Twenty-four patients were eligible for analysis. Both VMAT and IMRT plans were sufficient in planning target volume coverage. In terms of conformity, VMAT was superior to IMRT (P = .034). Dmean, V5, and V10 of the heart were significantly decreased in VMAT plans when compared with IMRT plans. VMAT was as effective as IMRT plans in sparing of other normal tissues. In addition, both the mean number of monitor units and treatment time were significantly reduced when VMAT was compared with IMRT.
VMAT plans was equivalent or superior to IMRT plans in dose distribution, and was associated with slightly advantage in sparing of the heart and coronary arteries. Our analyses suggested VMAT as a preferred option in left-sided breast cancer patients treated with modified radical mastectomy.
Keywords: breast cancer, dosimetry characteristics, intensity modulated radiotherapy, organs at risk, volumetric modulated arc radiotherapy
1. Introduction
Breast cancer remains the most common cancer and the second leading cause of cancer-related death in the world, the incidence and mortality is also increasing in China.[1,2] Over the last few decades, dramatic changes have been noted in the management of breast cancer. Several publications indicated survival benefits with the application of adjuvant therapies, including polychemotherapy regimens and radiotherapy.[3–5]
Radiotherapy has demonstrated efficacy in patients with operable breast cancer, and it is associated with improved treatment outcomes.[6] For early-stage patients treated with breast-conserving surgery, radiotherapy could decreases local recurrence rates; in node-positive individuals who have undergone mastectomy, radiotherapy improves cancer-specific survival.[7] Recently, partial breast radiotherapy is increasingly acceptable in early-stage patients treated with breast-conserving surgery, and this strategy needs to be evaluated in the long-term clinical outcomes.[8] Currently, whole breast irradiation remains the gold standard for early-stage breast cancer patients after breast-conserving surgery.[9] However, in breast cancer patients treated with thoracic radiotherapy, a challenge emerged as the proximity of dose-limiting to critical structures in the left-sided diseases, which inevitably resulted in increased the side effects and decreased tolerance.[10] For patients with breast tumor, late side effects including new tumors were often observed in the contralateral breast cancer after thoracic radiotherapy, this is the most common secondary cancer in female patients and accounting for approximately 50% of the total second cancers.[11] After radiotherapy, cardiac toxicity including arrhythmias, pericarditis, congestive heart disease, ischemic heart disease (myocardial infarctions), and valvular disease may occur.[10] Over the past few decades, radiotherapy has been optimized with the advances in technology. Compared with conventional therapies such as 2-dimensional radiotherapy technique with anterior–posterior opposed fields, intensity-modulated radiotherapy (IMRT) has been widely investigated in the management of breast cancer. This technique was used to minimize radiation damage to normal tissues and increases the geometrical accuracy in radiation delivery.[12] Volumetric-modulated arc therapy (VMAT), as an advanced radiotherapy technique and a rotational form of IMRT, has been applied to clinical practice in various solid tumors.[13–15] The comparisons between VMAT and IMRT plans have been extensively investigated in breast cancer, especially in treatment planning of breast cancer patients with breast-conserving surgery.[16,17] Due to the difficult in delineation, studies focusing on the comparison of coronary artery sparing is rare. In current analysis, we retrospectively analyzed the treatment planning of left-sided breast cancer patients treated with modified radical mastectomy, moreover, we evaluated the dosimetric parameters of target-volume coverage and organs at risk (OARs) sparing between VMAT plans and IMRT plans.
2. Methods
2.1. Patients selection, target volume, and OAR delineation
This retrospective analysis was performed from March 2013 to May 2015, A total of 24 left-sided breast cancer patients treated with modified radical mastectomy was investigated. The median age was 58 years (range, 38–85 years), all patients were staged according to the American Joint Committee on Cancer 2010 staging system. Most of the patients had stage III breast cancer, and the rest 37.5% patients had stage II and IV diseases. The present analysis was approved by the local Hospital Ethics Committee, and the written informed consent was obtained from each patient prior to treatment.
Individuals were immobilized in a supine position with arms overhead using breast board immobilization. A helical scanner (Siemens Somatom, Sensation Open Computed Tomography) was used for treatment-planning computed tomography (CT) scans, the parameters were as following: range, 6 cm superior to the clavicle to 8 cm inferior to breast tissue with 3 mm thick slices. Intravenous contrast is not necessary and the entire lung must be included. All the images were transferred from CT workstation to treatment planning system (TPS, Eclipse version 10.0, Varian Medical Systems, Palo Alto, CA) for delineation.
Regions included the chest wall, ipsilateral supraclavicular lymph nodes, ipsilateral level I–III axillary lymph nodes, ipsilateral interpectoral lymph nodes, and ipsilateral internal mammary lymph nodes were contoured on CT scan to generate the clinical target volume (CTV). The planning target volume (PTV) was generated by using a 7-mm uniform expansion of the CTV in all direction without the skin surface. The breast cancer CTV and PTV delineations were according to the recommendation of the International Committee for Radiological Units (ICRU) report #83.[18] The PTV was designed to account for daily setup error and motion. The normal structures and OARs including heart, left anterior descending artery (LAD), right coronary artery (RCA), contralateral breast, ipsilateral lungs, and contralateral lungs were contoured by several experienced radiation oncologist, and then confirmed by a radiologist.
2.2. Planning techniques and dose constraints
Each treatment plan was designed to deliver 50 Gy in 25 fractions to the PTV using the Varian linear accelerators (TureBeam, Varian) operating at 6 MV photons. All treatment plans aimed to reducing the irradiation to OARs as much as possible while encompass at least 95% of PTV by 95% of the prescribed dose. The OARs dose constraints were defined as the following: the volume to 30 Gy (V30) is below 3% of the heart, the volume to 20 Gy (V20) is less than 20% of the ipsilateral lung.
2.3. VMAT and IMRT plans
In order to optimize the VMAT plan, progressive resolution optimizer (Version 10.0) was utilized. Dose calculation was performed by using the Anisotropic Analytical Algorithm (Version 10.0). For VMAT, a dual arc of 254° with opposite rotation was set up as the following: an arc rotating clockwise with a gantry angle of 273° to 167°, and a second arc rotating anticlockwise from the gantry angle of 167° to 273°. To avoid tongue-and-groove effects, the couch was set to 0°, and the collimator angle was set to 30° (or 330°).
The dose-volume optimizer was used to optimize IMRT plans, and the Anisotropic Analytical Algorithm was utilized for dose calculation. It employs 5 coplanar fields (5F) using a dynamic sliding window multileaf collimator with 6-MV photos from a Varian linear accelerator, with gantry angles (26°, 100°, 140°, 322°, 288°). Each treatment field constituted beam geometry. Times of radiotherapy delivery and numbers of Mus were recorded.
2.4. Evaluation tools
The dose volume histograms was applied to quantitative evaluation of the treatment plans, including PTV, heart, RCA, LCA, and other critical normal tissues (lungs and contralateral breast). The evaluated parameters of PTV including the maximum and minimum dose, D95% (the dose to 95% of the volume), D5% (the dose to 5% of the volume), and V107% (more than 107% of the prescribed dose was received in the volume), were compared between the VMAT and IMRT plans for every individual. The conformity index (CI) was calculated as PTV100%/PTV∗ PTV100%/V100%, and target dose conformity to PTV was measured by using CI. The CI ranges from 0 to 1, and 1 suggested the best value. PTV indicated the PTV volume, the PTV100% demonstrated the PTV volume was covered by the 100% isodose, and the V100% means the volume was covered with 100% isodose. According to the ICRU 83 report, the homogeneous index (HI) of dose distribution was calculated as (D2%-D98%)/D50%. D2%, D50%, and D98% meant the doses of 2%, 50%, and 98% volume of the PTV. When the values of HI was decreasing, a better dose homogeneity was acquired.
For OAR, the evaluation parameters including: Dmean, V5, V10, V30, and V45 of the heart; Dmean and D5 of the LAD and the RCA; Dmean, V5, V10, and V20 of the ipsilateral lung; Dmean and V5 of the contralateral lung; Dmean and V5 of the contralateral breast. Thereinto, Vx was defined as the percentage of organ volumes that receiving the least dose. The treatment time and the number of MU were also recorded and compared in both VMAT and IMRT plans.
2.5. Statistical analysis
The statistical package for social sciences software (version 17.0, Chicago, IL) was applied for statistical analysis. The Wilcoxon matched-pair signed-rank test was used to compare the VMAT plans with the IMRT plans. The level considered statistically significant was set to 5% (P < .05).
3. Results
The dosimetric comparison of VMAT and IMRT were performed, dosimetric parameters of including the mean values of D5%, D95%, and V107% were presented in Table 1. The mean CI for the PTV was 0.77 (0.73–0.81) for IMRT, and 0.82 (0.79–0.84) for VMAT with a significant difference (P = .034). The mean HI was 0.21 (0.19–0.22) for IMRT, and 0.20 (0.19–0.21) for VMAT, and there was insignificant difference when VMAT compared with IMRT (P = .613). The mean number of MU was 527.21 (range, 476.03–610.79) for VMAT plan compared with 1132.85 (range, 1026.09–1358.14) for IMRT plan. For VMAT plan, the mean delivery time was 3.62 minutes (range, 2.98–4.27 minutes), significantly less than that of IMRT plan (8.74, range from 7.88 to 9.42).
Table 1.
Comparisons of the dosimetric parameters of the PTV. (The Wilcoxon matched-pair signed-rank test was utilized for the calculation of statistical difference.).
| IMRT | VMAT | P-value | |
| Minimal dose (%) | 83.12 (76.8–91.5) | 79.24 (72.6–83.1) | .076 |
| Maximum dose (%) | 108.2 (106. 9–110.2) | 108.7 (105.9–109.7) | .528 |
| CI | 0.77 (0.73–0.81) | 0.82 (0.79–0.84) | .034 |
| D95% (%) | 87.8 (82.3–93.2) | 89.4 (84.5–97.1) | .059 |
| D5% (%) | 105.3 (103.9–107.6) | 104.1 (103.2–106.8) | .125 |
| V107% (%) | 2.1 (1.7–2.4) | 1.8 (1.5–2.1) | .063 |
| MU | 1132.85 (1026.09–1358.14) | 527.21 (476.03–610.79) | .837 |
| HI | 0.21 (0.19–0.22) | 0.20 (0.19–0.21) | .613 |
| Time | 8.74 (7.88–9.42) | 3.62 (2.98–4.27) | .341 |
CI = conformity index, HI = homogeneous index, IMRT = intensity-modulated radiotherapy, MU = monitor units, VMAT = volumetric-modulated arc therapy.
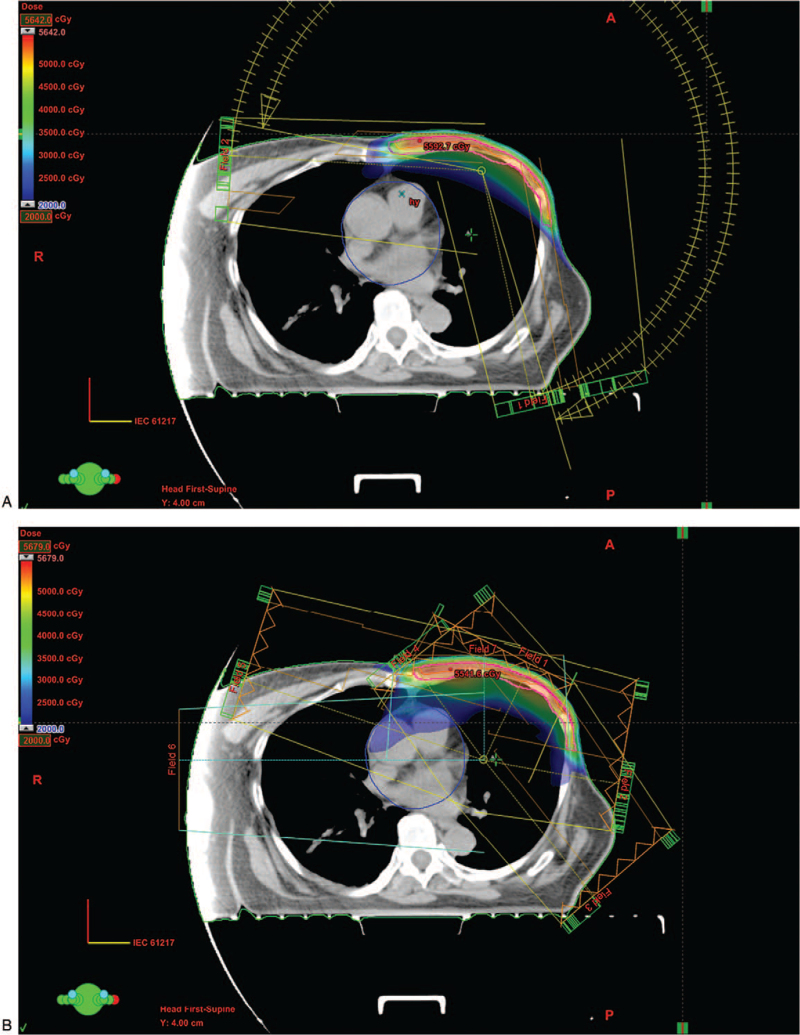
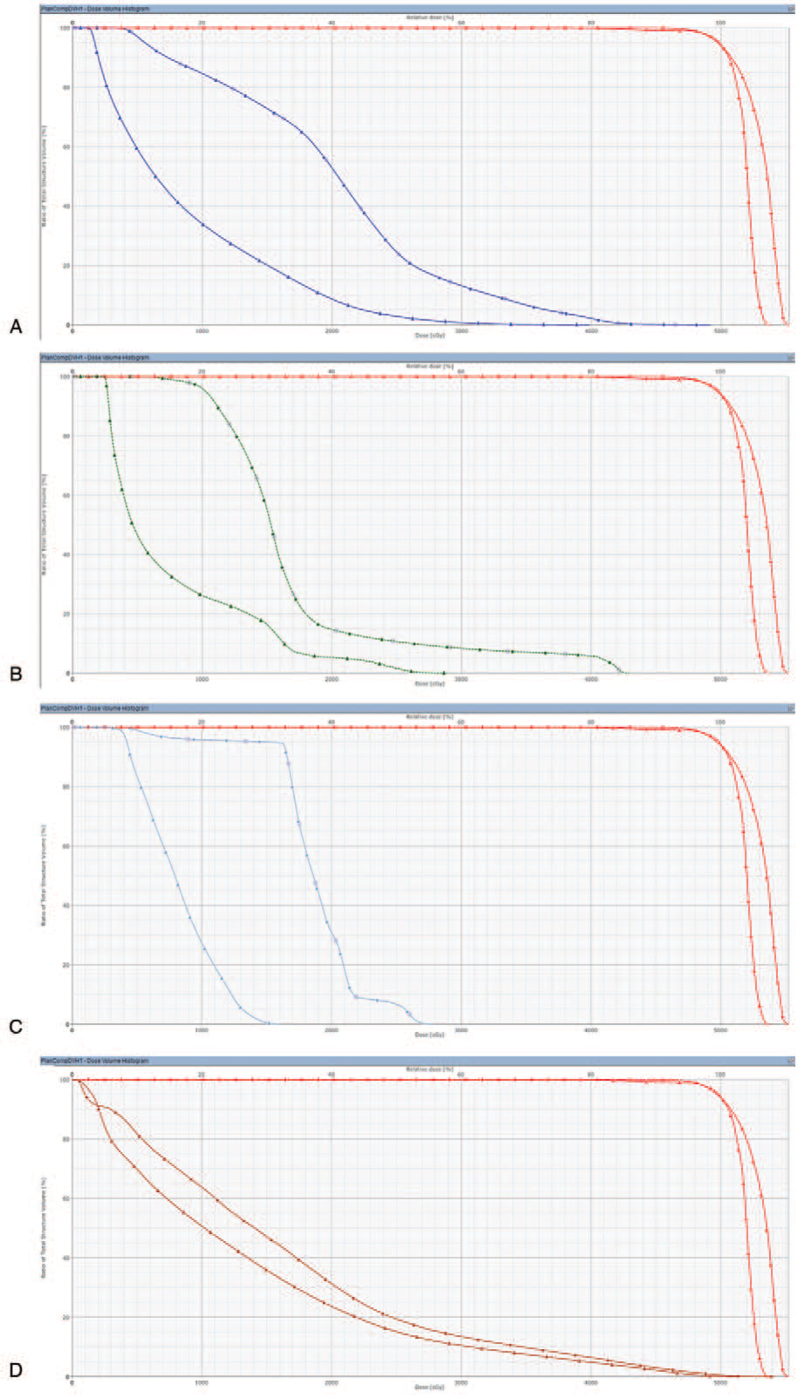
The VMAT plans was associated with slightly advantages of OARs sparing when compared with IMRT, and the detailed dosimetric parameters of OARs were shown in Table 2. Figure 1 represented the contours of PTV, heart, LAD, RCA, both lungs and contralateral breast for both VMAT and IMRT plans in a patient. In VMAT plans, the mean value of radiation dose to heart was 10.7 Gy (range, 9.5–11.6 Gy), which was lower than the dose in IMRT plans (11.5 Gy, range from 10.3 to 12.7 Gy, P = .043, Fig. 2A). These favorable outcomes were partly due to the decrease of volume receiving the low doses (V5 and V10), however, in terms of high doses irradiation to heart volume (V30 and V45), insignificant differences were observed (P > .05). In addition, for the LAD sparing, the mean dose reduced in VMAT plans and IMRT plans were 26.1, 29.3 Gy; respectively, (P = .037, Fig. 2B). For the RCA sparing, the mean dose decreased in VMAT plans and IMRT plans were 5.2, 9.5 Gy; respectively, (P = .023, Fig. 2C). VMAT showed certain advantages in both the LAD and RCA sparing.
Table 2.
Plan evaluation parameters of IMRT and VMAT plans. (The Wilcoxon matched-pair signed-rank test was applied for the statistical analysis.).
| IMRT | VMAT | P-value | |
| Heart | |||
| Mean dose (Gy) | 11.5 (10.3–12.7) | 10.7 (9.5–11.6) | .043 |
| V5 (%) | 100.0 (99.91–100) | 93.6 (87.2–98.1) | .021 |
| V10 (%) | 57.3 (48.2–65.9) | 44.8 (37.3–56.4) | .265 |
| V30 (%) | 3.1 (2.8–3.5) | 2.8 (2.4–3.2) | .087 |
| V45 (%) | 0.25 (0.22–0.31) | 0.27 (0.23–0.3) | .172 |
| LAD | |||
| Mean dose (Gy) | 29.3 (24.2–33.6) | 26.1 (21.6–31.8) | .037 |
| D5 (Gy) | 40.27 | 37.5 | .128 |
| RCA | |||
| Mean dose (Gy) | 9.5 (7.6–10.8) | 5.2 (4.5–5.7) | .023 |
| D5 (Gy) | 20.9 | 16.8 | .146 |
| Ipsilateral lung | |||
| Mean dose (Gy) | 14.1 (12.3–15.1) | 13.6 (11.9–14.7) | .069 |
| V5 (%) | 54.7 (47.6–62.1) | 53.8 (49.2–60.3) | .071 |
| V10 (%) | 38.9 (36.2–42.5) | 40.3 (37.8–41.7) | .206 |
| V20 (%) | 27.6 (23.9–31.6) | 26.4 (23.1–30.8) | .194 |
| Contralateral lung | |||
| Mean dose (Gy) | 5.4 (4.8–5.9) | 5.3 (4.9–5.7) | .057 |
| V5 (%) | 28.3 (24.6–33.1) | 25.7 (20.4–31.6) | .105 |
| Contralateral breast | |||
| Mean dose (Gy) | 3.2 (2.9–3.5) | 3.4 (3.1–3.8) | .056 |
| V5 (%) | 9.4 (8.7–10.2) | 8.6 (7.9–9.1) | .143 |
IMRT = intensity-modulated radiotherapy, LAD = left anterior descending artery, RCA = right coronary artery, VMAT = volumetric-modulated arc therapy.
Figure 1.
Treatment planning in 1 representative patient. (A) VMAT. (B) IMRT. IMRT = intensity-modulated radiotherapy, VMAT = volumetric-modulated arc therapy.
Figure 2.
Dose-volume graph of a representative patient for VMAT and IMRT. (A) Heart. (B) LAD. (C) RCA. (D) Lung. IMRT = intensity-modulated radiotherapy, LAD = left anterior descending artery, RCA = right coronary artery, VMAT = volumetric-modulated arc therapy.
VMAT and IMRT plans were comparable in other normal tissues sparing. For ipsilateral lung, the mean dose was 13.2 Gy (range, 11.9–14.7 Gy) in VMAT and 13.8 Gy (range, 12.3–15.1 Gy) in IMRT (P = .069), and there was insignificant difference in the comparison of V5, V10, and V20 between the 2 plans (P > .05, Fig. 2D). In terms of Dmean and V5 of contralateral lung, insignificant advantage was observed when VMAT plans compared with IMRT (P > .05). Additionally, Dmean and V5 of contralateral breast were slightly decreased in VMAT plans when compared with IMRT plans, and insignificant differences was achieved (P > .05).
4. Discussion
Radiotherapy served as a vital tool in the management of breast cancer. Radiotherapy for left-side breast cancer is really a challenge in escalating doses to primary tumor and limiting doses to normal tissue. Compared with the 2-dimensional technique, IMRT reduces the damage to normal tissues, creates high geometrical accuracy, and provides highly conformal dose distributions. Meanwhile, improved radiotherapy techniques further reduce the damage to OARs. VMAT is a new technology developed from IMRT, it uses a single gantry rotation and delivers an optimized 3-dimensional dose distribution. However, when VMAT compared with IMRT in treating breast cancer, the conclusions regarding to the plan quality were unclear. In the present study, we examined the efficacy of VMAT planning in sparing the critical normal tissues in left-sided breast cancer patients treated with modified radical mastectomy, the results indicated slightly advantages in heart and coronary arteries sparing by this novel technique when compared with IMRT. Furthermore, we compared the dosimetric parameters between VMAT and IMRT plans and revealed that VMRT plans significantly reduced treatment time and MU number.
The difference between VMAT and IMRT has been investigated before. Jin et al evaluated the radiotherapy plans of breast cancer patients after breast-conserving surgery, and the outcomes demonstrated that the CI of target volume within VMAT was decreased when compared with tangential field IMRT, moreover, the HI was even worse.[19] In the present analysis, we found that both VMAT and IMRT plans were sufficient to the clinical required PTV coverage. In terms of CI, VMAT acquired a better dose conformity than IMRT technique. However, there was insignificant difference in terms of HI. This discrepancy might be depended on factors including the operational manner or the target irradiated, and further investigation were needed.
Cardiac toxicity as a severe sequela after breast radiotherapy has been increasingly recognized among patients with left-sided disease.[10] Radiation-induced damage to endothelial cell and microvasculature resulted in the progressive dysfunction of pericardium, myocardium, heart valves, and coronary arteries.[20,21] Patients treated with thoracic radiotherapy were associated with a moderate or severe radiation-related endocardial fibrosis, nonischemic myocardial fibrosis, and valvular dysfunction.[22] There were advantages in OARs sparing with an increased utilization of IMRT technique in breast cancer, the heart exposed dosage has been significantly reduced. Kole et al evaluated 19 distal esophageal cancer patients and found that 3-dimensional conformal radiotherapy treatment planning significantly increased the radiation exposure to heart and RCA when compared with IMRT.[23] Several studies also compared the dosimetric advantages of VMAT and IMRT plans in breast cancer patients treated with breast-conserving surgery, and indicated that IMRT was superior to VMAT in the OARs dose distribution.[24] For patients with left breast carcinoma after mastectomy, VMAT showed better target coverage, HI, CI, and OARs sparing than IMRT plans.[25] In the current study, we compared VMAT with IMRT planning in left-sided breast cancer patients treated with modified radical mastectomy, the results demonstrated that VMAT was slightly superior to IMRT in sparing of heart and coronary arteries, but insignificant differences were observed in other normal tissues. Although the advanced radiotherapy techniques were able to reduce the irradiation dose to heart, breast radiotherapy still increases the risk of cardiovascular diseases. Therefore, VMAT may be a preferred modality in OARs sparing in left-sided breast cancer patients, especially for heart and coronary arteries during radiotherapy.
To date, several studies have shown that low dose irradiation could increase the risk of subsequent malignancy, especially for the contralateral breast.[26,27] Stovall et al reported that the risk of developing a second primary breast cancer was inverse correlated with the age at exposure.[28] Women younger than 40 years who received more than 1.0 Gy radiation doses to the contralateral breast would have an increased long-term risk of second cancer. For the women older than 40 years, there was no evidence of increased risk of contralateral breast cancer. Pasler et al compared the dose exposure to right breast between VMAT and IMRT plans, final results demonstrated a preferred OARs sparing in VMAT and the volume of contralateral structures receiving high dose were similar or even smaller in VMAT plans than IMRT plans.[29] In the present study, the application of VMAT was associated with similar contralateral breast sparing when compared with IMRT.
There were several limitations in the present study. Firstly, the sample size was really small and large patient population studies are really needed. Secondly, because the absence of a cone beam CT in our hospital, patient positioning was not monitored; moreover, intra-fraction organ motion may be ignored and slight difference of the dose delivered to tumor target and OARs may be existed. Nevertheless, this analysis provided novel insights for the application of VMAT in patients of left-sided breast cancer after modified radical mastectomy.
5. Conclusion
In conclusion, the VMAT plans significantly reduced treatment time and MU number when compared with IMRT in patients of left-sided breast cancer after modified radical mastectomy; VMAT were associated with slightly advantage in terms of heart and coronary arteries sparing. Furthermore, similar PTV coverage and sparing of other normal tissues were observed between these 2 techniques. Therefore, VMAT is a promising technique in the treatment of left-sided breast cancer.
Author contributions
Conceptualization: Rui Wang, Jun Zhou.
Data curation: Rui Wang, Jun Zhou.
Formal analysis: Rui Wang, Jun Zhou.
Investigation: Rui Wang, Jun Shen, Huanhuan Yan, Xitao Gao, Tianfu Dong, Shuqin Li, Peishun Wang, Jun Zhou.
Methodology: Rui Wang, Jun Shen, Huanhuan Yan, Xitao Gao, Tianfu Dong, Shuqin Li, Peishun Wang, Jun Zhou.
Resources: Huanhuan Yan, Xitao Gao, Tianfu Dong, Shuqin Li, Peishun Wang.
Software: Xitao Gao, Tianfu Dong, Shuqin Li, Peishun Wang.
Supervision: Jun Zhou.
Validation: Rui Wang, Jun Shen, Jun Zhou.
Visualization: Rui Wang, Jun Zhou.
Writing – original draft: Rui Wang, Jun Zhou.
Writing – review & editing: Jun Zhou.
Footnotes
Abbreviations: CI = conformity index, CTV = clinical target volume, HI = homogeneous index, IMRT = intensity-modulated radiotherapy, LAD = left anterior descending artery, OARs = organs at risk, PTV = planning target volume, RCA = right coronary artery, VMAT = volumetric-modulated arc therapy.
How to cite this article: Wang R, Shen J, Yan H, Gao X, Dong T, Li S, Wang P, Zhou J. Dosimetric comparison between intensity-modulated radiotherapy and volumetric-modulated arc therapy in patients of left-sided breast cancer treated with modified radical mastectomy: CONSORT. Medicine. 2022;101:2(e28427).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:07–30. [DOI] [PubMed] [Google Scholar]
- [2].Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115–32. [DOI] [PubMed] [Google Scholar]
- [3].Eckhoff L, Nielsen M, Moeller S, et al. TAXTOX - a retrospective study regarding the side effects of docetaxel given as part of the adjuvant treatment to patients with primary breast cancer in Denmark from 2007 to 2009. Acta Oncol 2011;50:1075–82. [DOI] [PubMed] [Google Scholar]
- [4].Yang K, Chun M. Radiation recall dermatitis in response to adjuvant capecitabine immediately following postoperative radiotherapy in a patient with breast cancer. Breast J 2019;26:748–51. [DOI] [PubMed] [Google Scholar]
- [5].Shien T, Iwata H. Adjuvant and neoadjuvant therapy for breast cancer. Jpn J Clin Oncol 2020;50:225–9. [DOI] [PubMed] [Google Scholar]
- [6].Haussmann J, Corradini S, Nestle-Kraemling C, et al. Recent advances in radiotherapy of breast cancer. Radiat Oncol 2020;15:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zhou L, Yang P, Zheng Y, et al. Effects of postoperative radiotherapy in early breast cancer patients older than 75 years: a propensity-matched analysis. J Cancer 2019;10:6225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Das M. Promising radiotherapy classifier for early breast cancer. Lancet Oncol 2019;20:e665. [DOI] [PubMed] [Google Scholar]
- [9].Mondal D, Julka PK, Sharma DN, et al. Dual partial arc volumetric-modulated arc therapy: The game changer for accelerated hypofractionated whole-breast radiotherapy with simultaneous integrated tumor cavity boost in early breast cancer - a comparative dosimetric study with single partial arc volumetric-modulated arc therapy. J Cancer Res Ther 2019;15:1005–10. [DOI] [PubMed] [Google Scholar]
- [10].Hufnagle JJ, Goyal A. Radiation Therapy Induced Cardiac Toxicity. Treasure Island, FL: StatPearls Publishing LLC; 2020. [Google Scholar]
- [11].DiMarzio P, Peila R, Dowling O, et al. Smoking and alcohol drinking effect on radiotherapy associated risk of second primary cancer and mortality among breast cancer patients. Cancer Epidemiol 2018;57:97–103. [DOI] [PubMed] [Google Scholar]
- [12].Arsene-Henry A, Fourquet A, Kirova YM. Evolution of radiation techniques in the treatment of breast cancer (BC) patients: from 3D conformal radiotherapy (3D CRT) to intensity-modulated RT (IMRT) using helical tomotherapy (HT). Radiother Oncol 2017;124:333–4. [DOI] [PubMed] [Google Scholar]
- [13].Ballhausen H, Li M, Ganswindt U, et al. Shorter treatment times reduce the impact of intra-fractional motion: a real-time 4DUS study comparing VMAT vs step-and-shoot IMRT for prostate cancer. Strahlenther Onkol 2018;194:664–74. [DOI] [PubMed] [Google Scholar]
- [14].Sharfo AWM, Stieler F, Kupfer O, et al. Automated VMAT planning for postoperative adjuvant treatment of advanced gastric cancer. Radiat Oncol 2018;13:74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rossi M, Boman E, Kapanen M. Contralateral tissue sparing in lymph node-positive breast cancer radiotherapy with VMAT technique. Med Dosim 2019;44:117–21. [DOI] [PubMed] [Google Scholar]
- [16].Zhao H, He M, Cheng G, et al. A comparative dosimetric study of left sided breast cancer after breast-conserving surgery treated with VMAT and IMRT. Radiat Oncol 2015;10:231–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Huang JH, Wu XX, Lin X, et al. Evaluation of fixed-jaw IMRT and tangential partial-VMAT radiotherapy plans for synchronous bilateral breast cancer irradiation based on a dosimetric study. J Appl Clin Med Phys 2019;20:31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gregoire V, Mackie TR. State of the art on dose prescription, reporting and recording in intensity-modulated radiation therapy (ICRU report No. 83). Cancer Radiother 2011;15:555–9. [DOI] [PubMed] [Google Scholar]
- [19].Jin GH, Chen LX, Deng XW, et al. A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: conventional tangential field, filed-in-filed, tangential-IMRT, multi-beam IMRT and VMAT. Radiat Oncol 2013;8:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Musa AE, Shabeeb D. Radiation-induced heart diseases: protective effects of natural products. Medicina (Kaunas) 2019;55:126–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ramadan R, Vromans E, Anang DC, et al. Connexin43 hemichannel targeting with TAT-Gap19 alleviates radiation-induced endothelial cell damage. Front Pharmacol 2020;11:212–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Šteiner I. Pathology of radiation induced heart disease. Rep Pract Oncol Radiother 2020;25:178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kole TP, Aghayere O, Kwah J, et al. Comparison of heart and coronary artery doses associated with intensity-modulated radiotherapy versus three-dimensional conformal radiotherapy for distal esophageal cancer. Int J Radiat Oncol Biol Phys 2012;83:1580–6. [DOI] [PubMed] [Google Scholar]
- [24].Badakhshi H, Kaul D, Nadobny J, et al. Image-guided volumetric modulated arc therapy for breast cancer: a feasibility study and plan comparison with three-dimensional conformal and intensity-modulated radiotherapy. Br J Radiol 2013;86:15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ekambaram V, Velayudham R, Swaminathan S, et al. Planning aspects of volumetric modulated arc therapy and intensity modulated radio therapy in carcinoma left breast – a comparative study. Asian Pac J Cancer Prev 2015;16:1633–6. [DOI] [PubMed] [Google Scholar]
- [26].Facoetti A, Barcellini A, Valvo F, et al. The role of particle therapy in the risk of radio-induced second tumors: a review of the literature. Anticancer Res 2019;39:4613–7. [DOI] [PubMed] [Google Scholar]
- [27].Xie L, Bao X, Cai T, et al. Elevated risk of radiation therapy-associated second malignant neoplasms in young African-American women survivors of stage I-IIIA breast cancer. Int J Radiat Oncol Biol Phys 2019;105:275–84. [DOI] [PubMed] [Google Scholar]
- [28].Stovall M, Smith SA, Langholz BM, et al. Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study. Int J Radiat Oncol Biol Phys 2008;72:1021–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Pasler M, Georg D, Bartelt S, et al. Node-positive left-sided breast cancer: does VMAT improve treatment plan quality with respect to IMRT? Strahlenther Onkol 2013;189:380–6. [DOI] [PubMed] [Google Scholar]