Abstract
Background:
Exercise intolerance was prevalent in people with chronic obstructive pulmonary disease (COPD) and had a detrimental effect on the quality of life. We aimed to evaluate the efficacy and safety of nitrate supplementation in exercise tolerance of people with COPD.
Methods:
We searched medical databases including Cochrane Library, EMBASE, and PubMed from inception to October 2020 for randomized control trials in treating COPD with nitrate supplementation.
Results:
Nine trials were identified. Compared with placebo, nitrate supplementation has no significant effect on the following variables: exercise endurance time (standard mean difference [SMD]: 0.06; 95% confidence interval [CI]: –0.39 to 0.52; P = .79), exercise capacity (SMD: 0.30; 95% CI: –0.21 to 0.80; P = .25), oxygen consumption (SMD: –0.04; 95% CI: –0.33 to 0.25; P = .80), resting systolic blood pressure (MD: –2.84; 95% CI: –8.46 to 2.78; P = .32), systolic blood pressure after exercise (MD: –4.66; 95% CI –15.66 to 6.34; P = .41), resting diastolic blood pressure (MD: 0.89; 95% CI: –4.41 to 6.19; P = .74), diastolic blood pressure after exercise (MD: –0.21; 95% CI: –5.51 to 5.10; P = .94), heart rate (MD: –2.52; 95% CI: –7.76 to 2.73; P = .35), and arterial oxygen saturation (MD: –0.44; 95% CI: –2.38 to 1.49; P = .65). No severe adverse effects from nitrate supplementation were reported in the included trails.
Conclusion:
Current evidence suggests that nitrate supplementation may be safe but ineffective for improving exercise tolerance in people with COPD.
Keywords: chronic obstructive pulmonary disease, exercise tolerance, nitrate
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a worldwide disease with a global prevalence of 11.7%, causing a great burden to the global medical system with annual death of 3 million.[1,2] People with COPD experience persistent respiratory symptoms such as breathlessness and dyspnea. Dyspnea occurs when there is a mismatch between increased inspiratory neural drive (IND) and inadequate mechanical response of the respiratory system.[3] Airflow limitation caused by destruction and remodeling of the lung tissue, as well as skeletal muscle dysfunction, contribute to inadequate mechanical response of the respiratory system when gas exchange abnormality caused by pulmonary blood flow shunting contribute to increased IND.[4,5] Dyspnea results in fatigue and exercise intolerance, lowering the quality of life in people with COPD.[6] Promoting exercise tolerance has always been a therapeutic priority in COPD therapy guidelines.[7]
Nitric oxide (NO) has been used to improve exercise tolerance in people with COPD. NO is a potent arterial vasodilator and plays a vital role in the relaxation of smooth muscle cells in blood vessel walls.[8] Inhaled or oral vasodilator therapy may improve pulmonary blood flow, improve ventilation-perfusion mismatch, and reduce IND.[9] As a result, NO may relieve dyspnea in people with COPD. Moreover, NO holds a significant function in skeletal muscle contraction and mitochondrial oxidative phosphorylation efficiency,[10,11] which may promote mechanical efficiency. Several studies revealed that nitrate supplementation, which converts into NO through entero-salivary pathway in vivo,[12] could improve exercise tolerance in people with COPD. Berry et al[13] found that acute dietary nitrate supplementation improved exercise performance and reduced blood pressure in people with COPD. Curtis et al[14] found that nitrate-rich beetroot juice caused reduced oxygen consumption (VO2) at isotime. However, other researchers made different results. Beijers et al[15] discovered that sodium nitrate supplementation did not modulate mechanical efficiency in people with COPD. Leong et al[16] stated that dietary nitrate supplementation as beetroot juice did not enhance exercise endurance in people with COPD. The contradictory results make it difficult to determine the efficacy of nitrate supplementation on exercise tolerance in people with COPD.
We wonder whether nitrate supplementation may improve exercise tolerance in people with COPD. Herein, we systematically review the evidence and perform a meta-analysis on efficacy and safety of nitrate supplementation in COPD to establish a reference for clinical practice.
2. Materials and methods
This study was performed according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.[17]
2.1. Literature search
We searched medical databases including Cochrane Library, EMBASE, and PubMed from inception until October 2020. The details of search strategy are included in Figure S1, Supplemental Digital Content for the details of the search strategy in databases including Cochrane Library, EMBASE, and PubMed. Additionally, we reviewed the references of included studies to prevent missing any eligible studies and increase the recall ratio.
2.2. Inclusion criteria
-
(1)
People with COPD diagnosed with international guidelines.[7]
-
(2)
Comparison of nitrate supplementation with control.
-
(3)
Randomized controlled trials (RCTs).
-
(4)
Full-text papers published in peer-reviewed journals.
-
(5)
Studies published in English language.
2.3. Exclusion criteria
-
(1)
Protocols or conference abstracts.
-
(2)
Data could not be extracted from articles for meta-analysis.
2.4. Quality assessment
The qualities of included randomized studies were evaluated for the risk of bias by the Cochrane Collaboration's tool.[18]
2.5. Data extraction
Two authors, HY and SH, independently screened the literature and extracted data. Different opinions from the 2 authors were resolved through consensus or consultation with a third author, FC. Information in the included studies such as study design, sample size, age, sex ratio, intervention, control, and outcome was extracted with a pre-set data extract table piloted by Kun Zhao.
2.6. Data synthesis and analysis
Review Manager 5.3 software (Cochrane Collaboration, Oxford, UK) was employed for statistical analysis. Statistical heterogeneity in studies was assessed using I2 method, with I2 > 50% or P < .1, suggesting significant heterogeneity. The results were expressed as standardized mean difference (SMD) or mean difference (MD) with a corresponding 95% confidence interval (CI). P < .05 was considered statistically significant. Sensitivity analysis was performed to determine the robustness of results by excluding any single study. Subgroup analysis was conducted to evaluate efficacy of nitrate supplementation on resting systolic blood pressure and systolic blood pressure after exercise, as well as resting diastolic blood pressure and after exercise.
3. Ethical statement
This study did not require ethical approval because it is based on previously conducted studies and does not contain any studies with human participants or animals performed by any author.
4. Results
4.1. Literature search
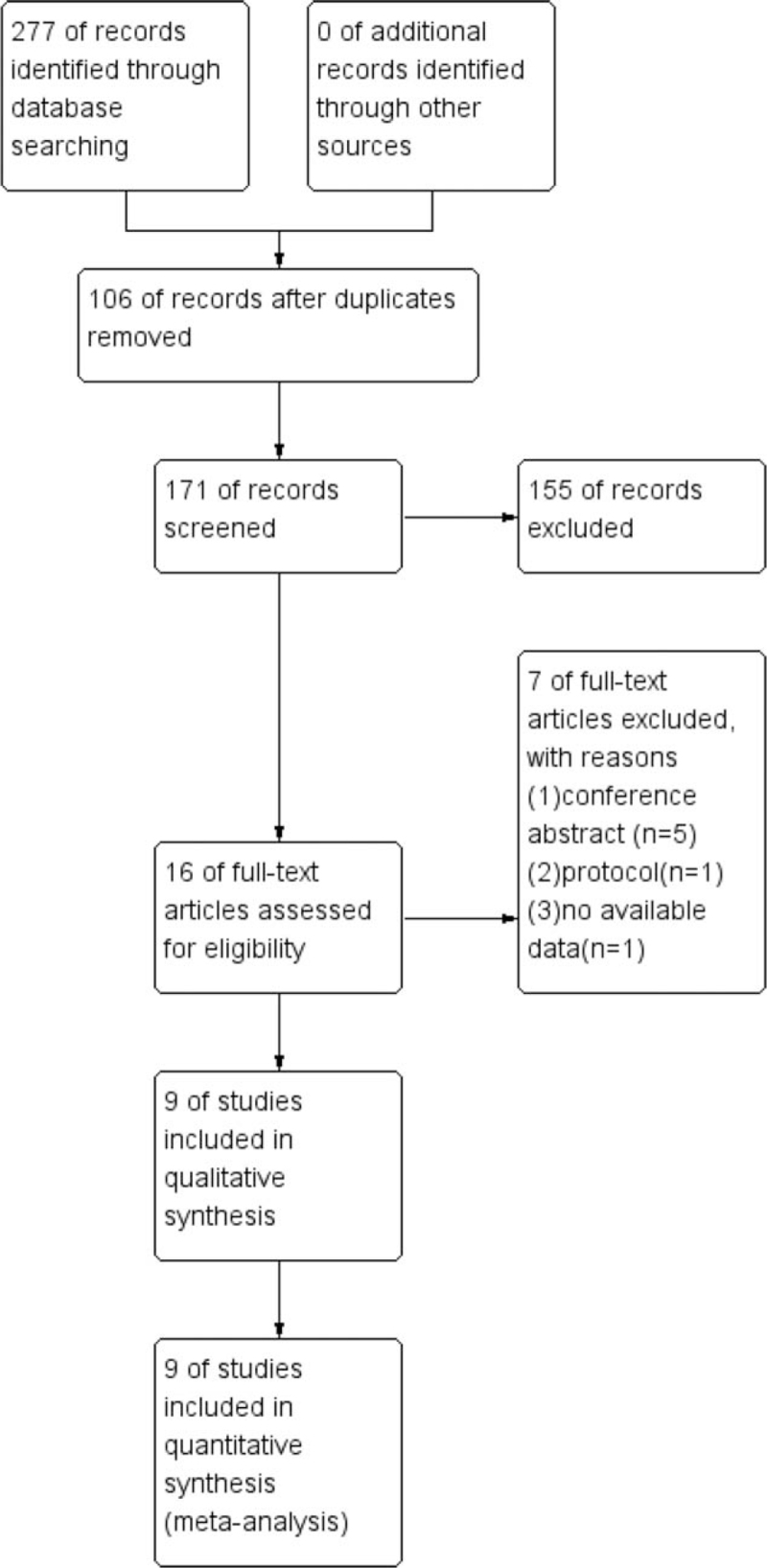
After searching databases, 277 studies were obtained. After removing duplicates and studies that did not match inclusion criteria, 16 were reserved for full-text review. Finally, we identified 9 studies after excluding studies including conference abstracts, protocols, or studies that lack available data. The process of literature search is depicted in Fig. 1.
Figure 1.
The process of literature search.
4.2. Study characteristics and quality assessment
The study characteristics are detailed in Table 1.
Table 1.
Characteristics of the included studies.
| Author | Year | Study design | Sample size (n) | Age, yr | Gender (M/F) | Intervention | Control | Duration | Outcome |
| Shepherd[23] | 2015 | Crossover study | 13 | 64.7 ± 7.7 | NA | 70 mL beetroot juice (6.77 mmol nitrate) | Placebo | Twice a day for 2.5 days | No difference in VO2, 6MWTD, SBP, DBP. |
| Leong[16] | 2015 | Crossover study | 19 | 67 ± 7.9 | 5/14 | 70 mL beetroot juice (4.8 mmol nitrate) | Placebo | Twice a day for 3.5 days | No difference in ESWTD, ESWTT. Decreased resting SBP. |
| Kerley[22] | 2018 | Crossover study | 8 | 62.9 ± 7.1 | 5/3 | 140 mL beetroot juice (12.9 mmol nitrate) | Placebo | Once a day for 14 days | Increased ISWTD. |
| Kerley[21] | 2015 | Crossover study | 11 | 69 ± 7 | 5/6 | 140 mL beetroot juice (12.9 mmol nitrate) | Placebo | Once a day for 1 day | Decreased SBP, DBP. Increased ISWTD. No difference in HR, SaO2. |
| Friis[20] | 2017 | Crossover study | 15 | 63 ± 13 | 9/6 | 140 mL beetroot juice (600 mg nitrate) | Placebo | Twice daily for 7 days | No difference in VO2, 6MWTD, HR, SBP. Decreased DBP. |
| Curtis[14] | 2015 | Crossover study | 21 | 68 ± 7 | 16/5 | 140 mL beetroot juice (0.8 g or 12.9 mmol nitrate) | Placebo | Once a day for 1 day | No difference in HR, SaO2. Decreased DBP, VO2. |
| Berry[13] | 2014 | Crossover study | 15 | 69.6 ± 8.5 | 12/3 | 140 mL beetroot juice (7.58 mmol of NO3−) | Placebo | Once a day for 1 day | No difference in HR, VO2, SaO2. Decreased DBP, resting SBP. |
| Beijers[15] | 2017 | Crossover study | 18 | 66.6 ± 7.5 | 13/5 | 140 mL water with 680 mg NaNO3 (496 mg or 8 mmol nitrate) | Placebo | Once a day for 7 days | No difference in VO2, Cycling time, SBP, DBP, HR. |
| Behnia[19] | 2018 | Parallel group study | Nitrate (n = 12) placebo (n = 13) | Nitrate 67 ± 8 placebo 68 ± 10 | Nitrate 6/6 placebo 7/6 | 250 mL juice (made of 70 mL of beetroot juice plus 180 mL of black currant juice). | Placebo | Once a day for 8 days | No difference in VO2, HR, DBP. Decreased SBP. |
6MWTD = six-minute walk test distance, DBP = diastolic blood pressure, ESWTD = endurance shuttle walk test distance, ESWTT = endurance shuttle walk test time, HR = heart rate, ISWTD = incremental shuttle walk test distance, NA = not available, SaO2 = arterial O2 saturation, SBP = systolic blood pressure, VO2 = oxygen consumption.
The studies were performed from 2014 to 2018 and in different countries, including Netherlands (n = 1), USA (n = 2), UK (n = 4), Denmark (n = 1), and Australia (n = 1).[13–16,19–23] The sample sizes in studies ranged from 8 to 25 subjects with 145 subjects in total. Most studies were crossover trials except for 1 study, which was a parallel group trial.[19] Most studies used beetroot juice for nitrate supplementation except 1 study, which used inorganic sodium nitrate.[15]
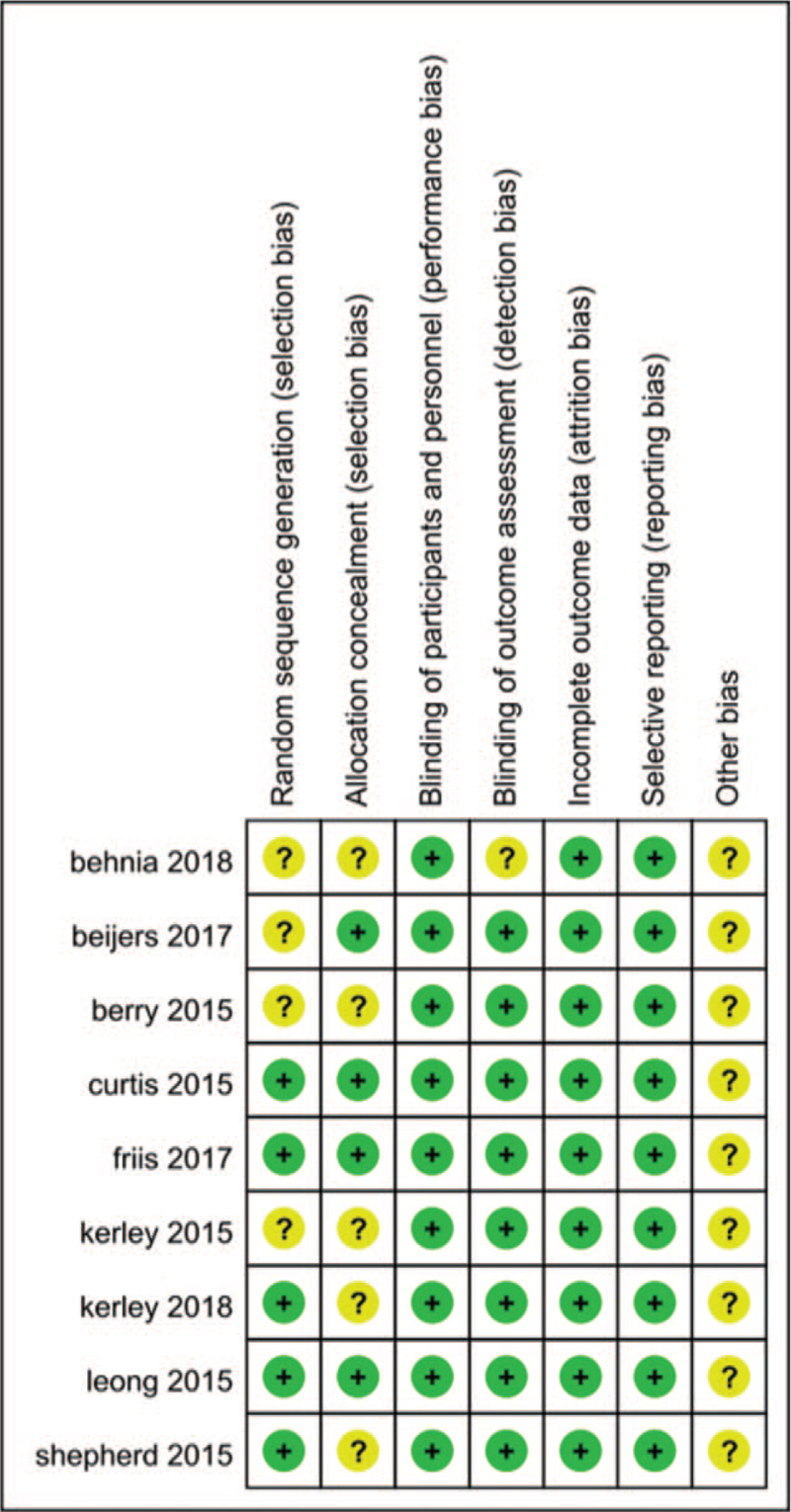
The quality assessment is detailed in Fig. 2.
Figure 2.
Risk of bias summary.
5. Efficacy
5.1. Exercise endurance time
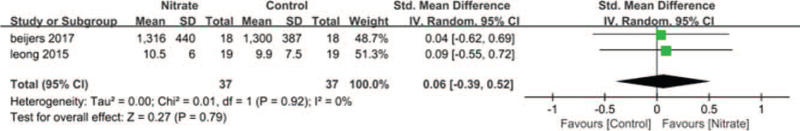
Two RCTs,[15,16] involving 74 subjects, evaluated exercise endurance time in nitrate supplementation and control groups, indicating low heterogeneity (P = .92, I2 = 0%). SMD was employed in these 2 studies since cycling time and endurance shuttle walk test time were used. In overall analysis, nitrate did not significantly increase endurance time (SMD: 0.06; 95% CI: –0.39 to 0.52; P = .79, Fig. 3).
Figure 3.
Forest plot of exercise endurance time.
5.2. Exercise capacity
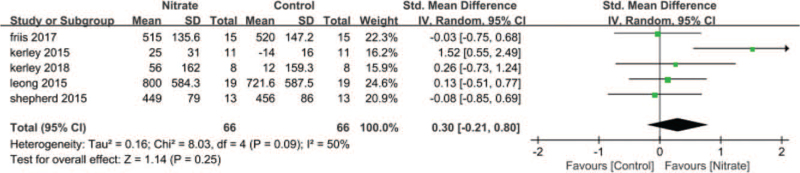
Five RCTs,[16,20–23] involving 132 subjects, evaluated exercise capacity in nitrate intervention and control groups, demonstrating high heterogeneity (P = .09, I2 = 50%). SMD was employed in these studies since 6-minute walk test distance, endurance shuttle walk test distance, and incremental shuttle walk test distance were utilized. In overall analysis, nitrate did not significantly increase exercise capacity (SMD: 0.30; 95% CI: –0.21 to 0.80; P = .25, Fig. 4).
Figure 4.
Forest plot of exercise capacity.
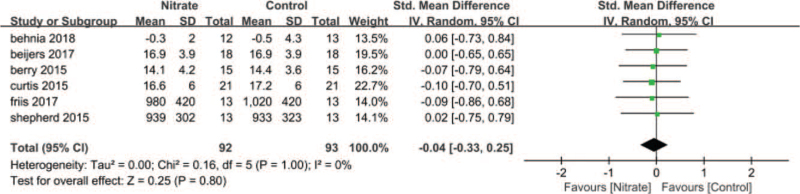
5.3. Oxygen consumption
Six RCTs,[13–15,19,20,23] including 185 subjects, evaluated VO2 in the nitrate intervention and control groups, revealing low heterogeneity (P = 1.00, I2 = 0%). SMD was employed in these studies since different measure units (mL/min or mL/kg/min) were utilized. In overall analysis, nitrate did not significantly decrease VO2 (SMD: –0.04; 95% CI: –0.33 to 0.25; P = .80, Fig. 5).
Figure 5.
Forest plot of oxygen consumption.
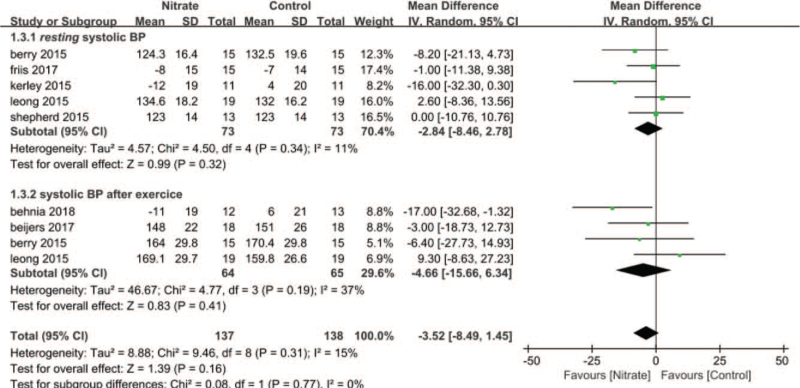
5.4. Systolic blood pressure
Preset subgroup analysis was performed for systolic blood pressure (SBP). Five RCTs,[13,16,20,21,23] involving 146 subjects, evaluated resting SBP in nitrate intervention and control groups, demonstrating low heterogeneity (P = .34, I2 = 11%). In overall analysis, nitrate did not significantly decrease resting SBP (MD: –2.84; 95% CI: –8.46 to 2.78; P = .32, Fig. 6). Four RCTs,[13,15,19] including 129 subjects, evaluated SBP after exercise in nitrate intervention and control groups, revealing low heterogeneity (P = .19, I2 = 37%). In overall analysis, nitrate did not significantly decrease SBP after exercise (MD: –4.66; 95% CI: –15.66 to 6.34; P = .41, Fig. 6).
Figure 6.
Forest plot of systolic blood pressure.
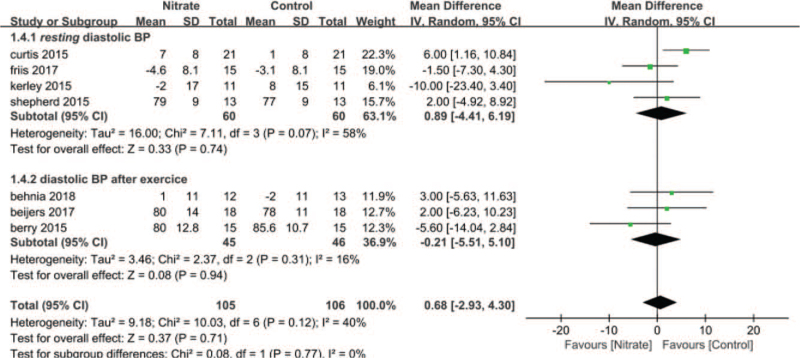
5.5. Diastolic blood pressure
Preset subgroup analysis was performed for diastolic blood pressure (DBP). Four RCTs,[14,20,21,23] involving 120 subjects, evaluated the resting DBP in the nitrate intervention and control groups, revealing high heterogeneity (P = .07, I2 = 58%). In overall analysis, nitrate did not significantly decrease resting DBP (MD: 0.89; 95% CI: –4.41 to 6.19; P = .74, Fig. 7). Three RCTs,[13,15,19] including 91 subjects, evaluated DBP after exercise in nitrate intervention and control groups, manifesting low heterogeneity (P = .31, I2 = 16%). In overall analysis, nitrate did not significantly decrease DBP after exercise (MD: –0.21; 95% CI: –5.51 to 5.10; P = .94, Fig. 7).
Figure 7.
Forest plot of diastolic blood pressure.
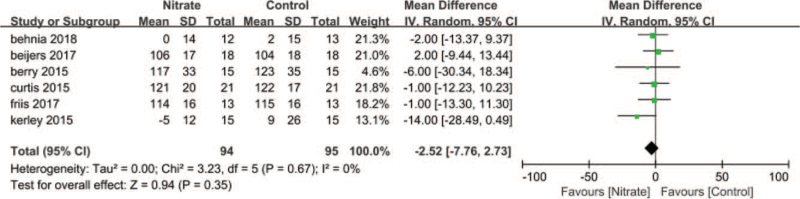
5.6. Heart rate
Six RCTs,[13–15,19–21] involving 189 subjects, evaluated the heart rate (HR) in nitrate intervention and control groups, indicating low heterogeneity (P = .67, I2 = 0%). In overall analysis, nitrate did not significantly decrease HR (MD: –2.52; 95% CI: –7.76 to 2.73; P = .35, Fig. 8).
Figure 8.
Forest plot of heart rate.
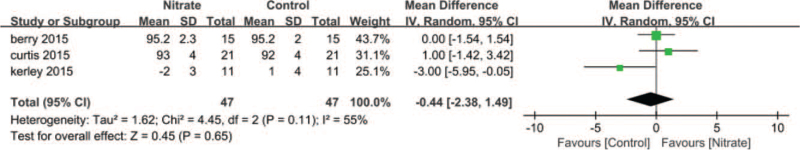
5.7. Arterial O2 saturation
Three RCTs,[13,14,21] including 94 subjects, evaluated arterial O2 saturation (SaO2) in nitrate intervention and control groups, revealing high heterogeneity (P = .11, I2 = 55%). In overall analysis, nitrate did not significantly decrease SaO2 (MD: –0.44; 95% CI: –2.38 to 1.49; P = .65, Fig. 9).
Figure 9.
Forest plot of arterial oxygen saturation.
5.8. Safety
No severe adverse effects from nitrate supplementation were reported in included trials. The adverse effects are shown in Table 2.
Table 2.
Adverse effect of the nitrate supplementation in patients with COPD.
| Author | Adverse effect |
| Curtis[14] | Beeturia |
| Shepherd[23] | Red stools and beeturia |
| Friis[20] | Nausea |
| Kerley[22] | Intolerance to beetroots juice taste/texture |
COPD = chronic obstructive pulmonary disease.
5.9. Sensitivity analysis
For exercise capacity, heterogeneity disappeared when a study from Kerley was omitted, but statistical significance remained the same.[21] For resting DBP, heterogeneity disappeared when a study from Kerley or Curtis was excluded, but statistical significance remained unchanged.[14,21] For SaO2, heterogeneity disappeared when a study from Kerley was omitted, but statistical significance remained the same.[21]
6. Discussion
Our study aimed to evaluate the efficacy and safety of nitrate supplementation on exercise tolerance in people with COPD. We found that nitrate supplementation may be safe but does not significantly affect exercise capacity, exercise endurance time, oxygen cost, blood pressure, oxygen saturation, or HR in people with COPD.
Dyspnoea is a symptom of COPD which contributes to exercise intolerance in patients with COPD. Dyspnea has been shown to result from disruption of normal relationship between IND to breathe and the dynamic response of the respiratory system.[3] Nitrate acquired from beetroots juice or sodium nitrate consumption can be converted into NO in vivo, which is an important regulator of vascular blood flow, mitochondrial function, skeletal muscle contractility, and calcium handling.[24] It has been postulated that nitrate supplementation may improve pulmonary blood flow, improve ventilation-perfusion mismatch, and reduce IND.[9] As a result, NO can relieve dyspnea in people with COPD. In our study, nitrate supplementation did not induce any effects on exercise tolerance in COPD. We speculate that, may be nitrate supplementation did not affect respiratory mechanics. The study by Behnia et al[19] included in this review found that nitrate supplementation did not affect markers of ventilation/perfusion matching (i.e., ventilation relative to carbon dioxide production, VE/VCO2 ratio) nor ventilation during exercise in people with COPD, although it increased the level of exhaled NO by 200%. This phenomenon may explain why nitrate supplementation did not have any effect on COPD. A recent study done by Phillips et al[25] showed that inhaled NO increased peak oxygen uptake, secondary to reduced ventilation relative to carbon dioxide production (VE/VCO2) and dyspnoea, which improved exercise capacity in people with mild COPD. The differences in these findings may result from the nature of subjects included. In the study by Phillips et al, the subjects had mild COPD whereas subjects included in the studies involved in our review had moderate to severe COPD. The progression of COPD is accompanied by damage to the pulmonary capillaries due to emphysema as well as pulmonary vasoconstriction caused by hyoxemia. In people with moderate to severe COPD, application of pulmonary vasodilators may regulate hypoxic pulmonary vasoconstriction and redirect perfusion to poorly ventilated alveoli. This will cause low ventilation–perfusion ratio and negatively affect pulmonary gas exchange.[26,27] This may partly explain the results reported by Phillips et al.[25]
Our meta-analysis revealed no decrease in SBP or DBP. A meta-analysis revealed that vascular aging might reduce tissue-specific responses to nitrate supplementation and the capacity to convert inorganic nitrate into nitrite,[28] which may partly explain why nitrate supplementation is ineffective in lowering blood pressure, given that included subjects in our meta-analysis were elderly. Another possible explanation may be using anti-hypertensive medication in included subjects in clinical trials. Numerous studies found no significant reduction in blood pressure in older hypertension subjects receiving anti-hypertensive medication.[29,30] It was supposed that anti-hypertensive agents might mitigate NO-mediated reduction in blood pressure by an unknown mechanism. In our meta-analysis, people with COPD receive anti-hypertensive medication, which may cause anti-hypertensive agents to mitigate NO-mediated reduction in blood pressure.
Our study also examined the safety of nitrate supplementation. Generally speaking, nitrate supplementation in the form of beetroot was well-tolerated with no reports of severe adverse effects. Specific investigations revealed gastrointestinal reactions such as nausea and color change in defecation.[14,20,22,23] The only study which utilized inorganic sodium nitrate for nitrate supplementation did not mention any adverse effect.[15]
Our study has some strengths. As far as we know, this study is the first meta-analysis evaluating efficacy and safety of nitrate supplementation on exercise tolerance in people with COPD. The included studies were all RCTs with relatively high quality of evidence. The meta-analysis was strictly conducted according to PRISMA guidelines. However, there were also some limitations. First, due to limited resources, only studies written in English were included in our meta-analysis, which may cause omission of some studies written in other languages. Second, most included studies employed a commercial beetroots juice in one company for nitrate supplementation (only 1 study used sodium nitrate). This could result in a bias due to the dosage form and its manufacturers. Third, the publication bias evaluation was unable to perform because included studies are <10.
7. Conclusions
Current evidence suggests that nitrate supplementation may be safe but ineffective for improving exercise tolerance in people with COPD. The underlying mechanism is required for investigation, as is the subtype of people with COPD who benefit from nitrate supplementation.
Acknowledgments
The authors sincerely acknowledge Kun Zhao from Zhejiang University for his advice in the study design and literature research.
Author contributions
Conceptualization: Hongkuan Yang.
Data curation: Hongkuan Yang, Shuifeng He, Fang Chen.
Formal analysis: Shuifeng He, Fang Chen.
Investigation: Junjie Pan.
Methodology: Hongkuan Yang, Fang Chen, Junjie Pan.
Project administration: Hongkuan Yang.
Software: Linbao Liang.
Supervision: Hongkuan Yang.
Writing – original draft: Hongkuan Yang.
Writing – review & editing: Linbao Liang, Junjie Pan.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, COPD = chronic obstructive pulmonary disease, DBP = diastolic blood pressure, HR = heart rate, IND = inspiratory neural drive, ISWTD = incremental shuttle walk test distance, MD = mean difference, NA = not available, NO = nitric oxide, RCTs = randomized control trials, SaO2 = arterial oxygen saturation, SBP = systolic blood pressure, SMD = standard mean difference, VE/VCO2 = ventilation relative to carbon dioxide production, VO2 = oxygen consumption.
How to cite this article: Yang H, He S, Chen F, Liang L, Pan J. Efficacy and safety of nitrate supplementation on exercise tolerance in chronic obstructive pulmonary disease: a systematic review and meta-analysis. Medicine. 2022;101:2(e28578).
This study was supported by Zhejiang Provincial Natural Science Foundation of China under Grant Number: LQ20H290004 and Zhejiang Provincial Chinese Medicine Research Program of China under Grant Number: 2020ZQ039.
The authors have no conflicts of interest to disclose.
Data Availability: The numeric data supporting this meta-analysis are from previously reported studies, which have been cited. The processed data are available from the corresponding author upon request.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
References
- [1].Adeloye D, Chua S, Lee C, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health 2015;5:020415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Collaborators GMaCoD. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].O’Donnell DE, Milne KM, James MD, de Torres JP, Neder JA. Dyspnea in COPD: new mechanistic insights and management implications. Adv Ther 2020;37:41–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Maltais F, Decramer M, Casaburi R, et al. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014;189:e15–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Marshall BE, Hanson CW, Frasch F, Marshall C. Role of hypoxic pulmonary vasoconstriction in pulmonary gas exchange and blood flow distribution. 2. Pathophysiology. Intensive Care Med 1994;20:379–89. [DOI] [PubMed] [Google Scholar]
- [6].Lee SH, Kim KU, Lee H, Kim YS, Lee MK, Park HK. Factors associated with low-level physical activity in elderly patients with chronic obstructive pulmonary disease. Korean J Intern Med 2018;33:130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 2017;195:557–82. [DOI] [PubMed] [Google Scholar]
- [8].Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A 1987;84:9265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Iyer KS, Newell JD, Jr, Jin D, et al. Quantitative dual-energy computed tomography supports a vascular etiology of smoking-induced inflammatory lung disease. Am J Respir Crit Care Med 2016;193:652–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bailey SJ, Fulford J, Vanhatalo A, et al. Dietary nitrate supplementation enhances muscle contractile efficiency during knee-extensor exercise in humans. J Appl Physiol 2010;109:135–48. [DOI] [PubMed] [Google Scholar]
- [11].Clerc P, Rigoulet M, Leverve X, Fontaine E. Nitric oxide increases oxidative phosphorylation efficiency. J Bioenerg Biomembr 2007;39:158–66. [DOI] [PubMed] [Google Scholar]
- [12].Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov 2008;7:156–67. [DOI] [PubMed] [Google Scholar]
- [13].Berry MJ, Justus NW, Hauser JI, et al. Dietary nitrate supplementation improves exercise performance and decreases blood pressure in COPD patients. Nitric Oxide 2015;48:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Curtis KJ, O’Brien KA, Tanner RJ, et al. Acute dietary nitrate supplementation and exercise performance in copd: a double-blind, placebo-controlled, randomised controlled pilot study. PLoS One 2015;10:e0144504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Beijers R, Huysmans SMD, van de Bool C, et al. The effect of acute and 7-days dietary nitrate on mechanical efficiency, exercise performance and cardiac biomarkers in patients with chronic obstructive pulmonary disease. Clin Nutr 2018;37(6 pt A):1852–61. [DOI] [PubMed] [Google Scholar]
- [16].Leong P, Basham JE, Yong T, et al. A double blind randomized placebo control crossover trial on the effect of dietary nitrate supplementation on exercise tolerance in stable moderate chronic obstructive pulmonary disease. BMC Pulm Med 2015;15:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009;151:W65–94. [DOI] [PubMed] [Google Scholar]
- [18].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Behnia M, Wheatley CM, Avolio A, Johnson BD. Influence of dietary nitrate supplementation on lung function and exercise gas exchange in COPD patients. Nitric Oxide 2018;76:53–61. [DOI] [PubMed] [Google Scholar]
- [20].Friis AL, Steenholt CB, Løkke A, Hansen M. Dietary beetroot juice - effects on physical performance in COPD patients: a randomized controlled crossover trial. Int J Chron Obstruct Pulmon Dis 2017;12:1765–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kerley CP, Cahill K, Bolger K, et al. Dietary nitrate supplementation in COPD: an acute, double-blind, randomized, placebo-controlled, crossover trial. Nitric Oxide 2015;44:105–11. [DOI] [PubMed] [Google Scholar]
- [22].Kerley CP, James PE, McGowan A, Faul J, Cormican L. Dietary nitrate improved exercise capacity in COPD but not blood pressure or pulmonary function: a 2 week, double-blind randomised, placebo-controlled crossover trial. Int J Food Sci Nutr 2019;70:222–31. [DOI] [PubMed] [Google Scholar]
- [23].Shepherd AI, Wilkerson DP, Dobson L, et al. The effect of dietary nitrate supplementation on the oxygen cost of cycling, walking performance and resting blood pressure in individuals with chronic obstructive pulmonary disease: a double blind placebo controlled, randomised control trial. Nitric Oxide 2015;48:31–7. [DOI] [PubMed] [Google Scholar]
- [24].Stamler JS, Meissner G. Physiology of nitric oxide in skeletal muscle. Physiol Rev 2001;81:209–37. [DOI] [PubMed] [Google Scholar]
- [25].Phillips DB, Brotto AR, Ross BA, et al. Inhaled nitric oxide improves ventilatory efficiency and exercise capacity in patients with mild COPD: a randomized-control cross-over trial. J Physiol 2021;599:1665–83. [DOI] [PubMed] [Google Scholar]
- [26].Barberà JA, Roger N, Roca J, Rovira I, Higenbottam TW, Rodriguez-Roisin R. Worsening of pulmonary gas exchange with nitric oxide inhalation in chronic obstructive pulmonary disease. Lancet 1996;347:436–40. [DOI] [PubMed] [Google Scholar]
- [27].Blanco I, Gimeno E, Munoz PA, et al. Hemodynamic and gas exchange effects of sildenafil in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Am J Respir Crit Care Med 2010;181:270–8. [DOI] [PubMed] [Google Scholar]
- [28].Siervo M, Lara J, Jajja A, et al. Ageing modifies the effects of beetroot juice supplementation on 24-hour blood pressure variability: an individual participant meta-analysis. Nitric Oxide 2015;47:97–105. [DOI] [PubMed] [Google Scholar]
- [29].Bondonno CP, Liu AH, Croft KD, et al. Absence of an effect of high nitrate intake from beetroot juice on blood pressure in treated hypertensive individuals: a randomized controlled trial. Am J Clin Nutr 2015;102:368–75. [DOI] [PubMed] [Google Scholar]
- [30].Kerley CP, Dolan E, Cormican L. Nitrate-rich beetroot juice selectively lowers ambulatory pressures and LDL cholesterol in uncontrolled but not controlled hypertension: a pilot study. Ir J Med Sci 2017;186:895–902. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.