PURPOSE:
COVID-19 challenged medical practice and graduate medical education. Building on previous initiatives, we describe and reflect on the formative process and goals of the Hematology-Oncology Collaborative Videoconferencing Learning Initiative, a trainee-led multi-institutional virtual COVID-19 learning model.
METHODS:
Clinical fellows and faculty from 13 US training institutions developed consensus needs, goals, and objectives, recruited presenters, and generated a multidisciplinary COVID-19 curriculum. Weekly Zoom conferences consisted of two trainee-led instructional segments and a trainee-moderated faculty Q&A panel. Hematology-oncology training program faculty and trainees were the targeted audience. Leadership evaluations consisted of anonymized baseline and concluding mixed methods surveys. Presenter evaluations consisted of session debriefs and two structured focus groups. Conference evaluations consisted of attendance, demographics, and pre- or postmultiple-choice questions on topic learning objectives.
RESULTS:
In 6 weeks, the initiative produced five conferences: antivirals, anticoagulation, pulmonology, provider resilience, and resource scarcity ethics. The average attendance was 100 (range 57-185). Among attendees providing both pre- and postconference data, group-level knowledge appeared to increase: antiviral (n = 46) pre-/postcorrect 82.6%/97.8% and incorrect 10.9%/2.2%, anticoagulation (n = 60) pre-/postcorrect 75%/93.3% and incorrect 15%/6.7%, and pulmonary (n = 21) pre-/postcorrect 66.7%/95.2% and incorrect 33.3%/4.8%. Although pulmonary management comfort appeared to increase, comfort managing of antivirals and anticoagulation was unchanged. At the conclusion of the pilot, leadership trainees reported improved self-confidence organizing multi-institutional collaborations, median (interquartile range) 58.5 (50-64) compared with baseline 34 (26-39), but did not report improved confidence in other educational or leadership skills.
CONCLUSION:
During crisis, trainees built a multi-institutional virtual education platform for the purposes of sharing pandemic experiences and knowledge. Accomplishment of initiative goals was mixed. Lessons learned from the process and goals may improve future disaster educational initiatives.
INTRODUCTION
Declared a worldwide pandemic on March 11, 2020, COVID-19 affected all aspects of society, including graduate medical education (GME). As epicenters of disease emerged,1 hospital capacities became overwhelmed,2,3 further compounded by medical supply4,5 and staffing6 shortages. To maintain COVID-19 care, faculty and trainees7 of all disciplines were abruptly pulled from standard duties to fill entirely new roles as emergency, inpatient, and intensive care unit COVID-19 providers.8
Despite a clear alignment of Knowles adult learning principles around COVID-19 learning (ie, motivation, need to know, and application),9 traditional GME methods struggled to overcome the numerous educational barriers imposed by the pandemic.10 To reduce SARS-CoV2 transmission, the Centers for Disease Control and Prevention advised against gatherings of 10 or more people,11 a restriction that significantly impaired in-person conferences.12,13 To ensure that hospitals had adequate COVID-19 emergency staffing protocols, physicians redirected their time and efforts away from educational activities to tasks focused on departmental and programmatic restructuring.14 Regional variations in patient populations, hospital infrastructure, and clinical experiences15-17 obscured cohesive understanding of COVID-19 pathophysiology and evidence-based management. With sparse or contradictory health agency messaging,18 structures historically relied upon to provide clear recommendations and guidelines for disaster response were lacking. In summary, COVID-19 upended traditional learning environments while posing additional challenges of novelty and the absence of clearly defined experts and reliable sources of instruction.
Yet COVID-19 was not the first disaster to temporarily upset medical education. Previous regional, national, and global disasters including outbreaks (SARS, H1/N1 influenza, and Ebola)19-21 and natural (Hurricanes Katrina, Sandy, and Maria)22 or man-made (bioterrorism and military)23 catastrophes each revealed challenges and solutions to continuing medical education. Common challenges presented by these disasters included learning environment disruption, problem novelty, and difficulty in locating reliable sources of instruction. To overcome these challenges, alternative learning environments and curricula were created, often using virtual classrooms24 and emphasizing decentralized, collaborative, and process-oriented learning in place of fact-based learning delivered from an instructive authority to novice learner.25 These solutions were, in turn, based on learning principles of connectivism,26 social constructivism,27 and community capacity28 and used methods such as rapid design thinking29 and a stepwise approach to medical education curriculum development.30
Recognizing similar educational challenges, we created the Hematology-Oncology Collaborative Videoconferencing (H/O CO-VID) Learning Initiative, a multi-institutional trainee-led virtual learning model. The primary aim of this paper is to describe the process of building the H/O CO-VID Learning Initiative. The secondary aims are to report the results for initiative goals and reflect on lessons learned from the process to guide future disaster medical education initiatives.
METHODS
Initiative Inception
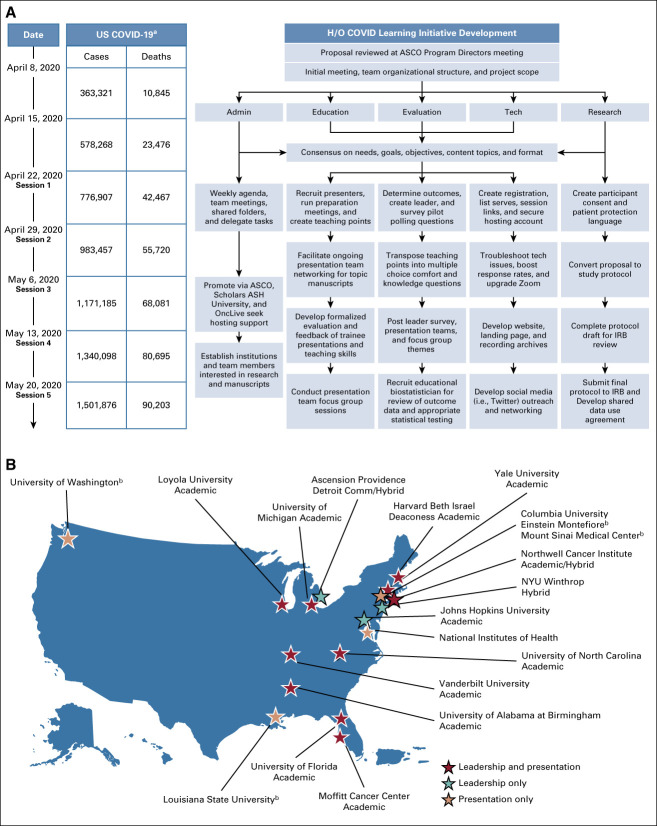
On April 2, 2020, a problem-based proposal was shared at an ASCO Program Directors meeting and through ASCO Connections. Interested institutions joined an e-mail list and attended a Zoom meeting to discuss the proposal. After two meetings, the group created a Microsoft Office 365 e-mail list-serve, adopted a BOX HIPAA compliant online collaborative workspace, planned weekly meetings, and structured trainee-led subcommittees (Fig 1).
FIG 1.
(A) From left to right: Weekly timeline from initial H/O COVID Leadership Meeting through completion of final virtual educational session. Cumulative US COVID-19 cases and deaths as reported by WHO on corresponding dates. Flowchart of H/O CO-VID Development, demonstrating key tasks performed in parallel by subcommittee working groups. (B) Participating US Training Programs (institution name and type). n = 10 institutions (blue star) were involved in both leadership and presentation teams. n = 3 institutions (yellow star) were involved in leadership team only. n = 4 institutions (red star) were involved in presentation teams only. aWHO.35 bProvided guest faculty only. ASH, American Society of Hematology; H/O CO-VID, Hematology-Oncology Collaborative Videoconferencing; IRB, institutional review board.
Initiative Participants and Organizational Structure
The study population primarily consisted of clinical fellows and faculty from US Hematology-Oncology training programs. From this population, three distinct groups were program leadership, presentation teams, and session attendees.
Program leadership consisted of one faculty and one to three trainees from initially responding institutions. Presentation teams consisted of three to five faculties and two to three trainees from leadership and nonleadership institutions, including non–Hematology-Oncology disciplines. Leadership faculty and trainees identified candidate presenters who were recruited through standardized e-mail invitations. Session attendees consisted of the remaining Hematology-Oncology faculty and trainees from all participating institutions, as well as faculty and trainees from guest presenter institutions. Other medical disciplines (infectious disease, pulmonology, critical care, and psychiatry) were invited to enhance cross-disciplinary perspectives and knowledge sharing. Medical students and residents were invited to conferences and encouraged to participate but were excluded from research.
Initiative Curriculum
Needs, goals, and objectives.
Using Kern's six-step approach,30 the leadership team engaged in consensus discussions to formulate a problem statement, identify general learning needs around this problem, refine general learning needs into targeted needs addressable by the initiative, and finally, translate targeted needs into potentially measurable initiative goals and objectives. Individual learners also completed voluntary surveys on personal learning needs and motivations.
Session learning objectives were selected through collaboration between presenters, the education subcommittee, and the evaluation subcommittee. Subcommittees presented updates at weekly meetings to allow for full team feedback, realign tasks with initiative goals, and clarify next steps.
Content.
Content was conceived around the immediate care of COVID-19 patients and providers and included five sessions correlating with targeted needs: (1) antiviral and immunology therapies, (2) coagulation disorders and anticoagulation management, (3) pulmonary complications and ventilation management, (4) provider resilience, and (5) Ethical Decision-Making During Resource Scarcity. Content was created by presentation teams who were introduced through Zoom. Roles, responsibilities, and expectations were reviewed, along with steps to ensure that all members had access and proficiency in using Box. Trainees developed coordinated slide sets and guided faculty in using online workspaces. Presentation and education subcommittee faculty assisted trainees in finding publications and provided presentation feedback during a preconference rehearsal session. Trainees and faculty debriefed following their presentations to provide future teams with clearer roles, responsibilities, and expectations.31
Implementation.
Eligible attendees were sent a registration e-mail for each session, complete with information on the topic, learning objectives, presenters, confidentiality, and research consent statement. Additional outreach efforts included creating a web page and Twitter account. Using an institutional Zoom Enterprise account, live virtual sessions consisted of a pretest and demographics introduction, two 20-minute Microsoft Powerpoint instructional segments led by trainees, and a 20-minute faculty Q&A panel moderated by a trainee and concluded with a post-test. A technology subcommittee facilitated recordings for on-demand access. Poll Everywhere polling questions and word clouds were incorporated into presentations to enhance interactivity. Q&A encouraged panelists to compare their respective institutional and multidisciplinary experiences and protocols and discuss the underlying reasoning behind their institutionally adopted care decisions.
Evaluation.
Evaluation tools were developed and overseen by the evaluation tools subcommittee. Leadership evaluations occurred through pre- and postmixed methods surveys and weekly meetings with feedback for continuing improvement. Surveys were created using the Research Electronic Data Capture (REDCap)32 and included sections on demographics, previous leadership or education experiences, self-assessed confidence fulfilling educational leadership roles, and open-ended questions on adult learning principles. Presentation team evaluations consisted of postconference debriefs and two structured focus group sessions at the conclusion of the pilot. Session evaluations consisted of attendance, demographics, and pre- or postmultiple-choice polling questions related to session learning objectives. Session knowledge and comfort were independently assessed to capture the distinct needs of knowing how to provide effective care while feeling competent. Knowledge questions included the option not sure to foster a culture of inquiry. Comfort questions such as “I feel comfortable managing noninvasive ventilation in patients with COVID-19” were based on a Likert scale from 1 = very uncomfortable to 5 = very comfortable. Provider resilience and ethics conferences used word clouds and open-ended responses to foster shared learning through interactive experiences.
Data Collection and Analysis
Data collected from REDCap and Poll Everywhere were exported as .csv files and uploaded into STATA v16.0 (StataCorp LLC, College Station, TX) for analysis. Descriptive statistics were performed on demographics, leadership experience, session attendance, and changes in group level session knowledge and comfort. Other statistical tests were exploratory for the purpose of internal program evaluation and continuing improvement. Pearson's chi square test for proportions evaluated differences in leadership team demographics. The Wilcoxon Rank-Sum test evaluated differences between pre- and postpilot self-assessed leadership skills, whereas the Wilcoxon Signed Rank test evaluated for differences between trainees and faculty. The McNemar test of nonparametric paired nominal data evaluated individual attendee changes in matched data from pre- to postconference knowledge answers. Similarly, the Wilcoxon Rank-Sum test evaluated individual attendee changes in matched data from pre- to postconference comfort with learning objectives.
Institutional Review
The project underwent full review and approval by the Institutional Review Board (20-0931, 20-1760). All participation was strictly voluntary. All participants were informed that participation implied consent as a research subject. No patient identifying information was included or discussed.
RESULTS
Initiative Needs, Goals, and Objectives
Framed around the problem of urgent learning barriers imposed by the pandemic, general needs included maintaining a learning and scholarship environment, maintaining a sense of medical community, feeling competent providing COVID-19 patient care, keeping up-to-date with evolving knowledge, and building self-efficacy and resilience. From these general needs, targeted needs were identified and subsequently transposed into the following initiative goals:
Produce weekly content to meet urgency;
Ensure trainees develop professionally, by leading in all aspects of the initiative and collaborating on scholastic COVID-19 works;
Grow a diverse community of participants, disciplines, and institutions;
Encourage sharing of COVID-19 feelings, experiences, and concerns;
Promote multidisciplinary learning from best available evidence and domain experts;
Acknowledge that ethical dilemmas and burnout and ensure trainee voices are valued and incorporated.
Leadership Team
Demographics.
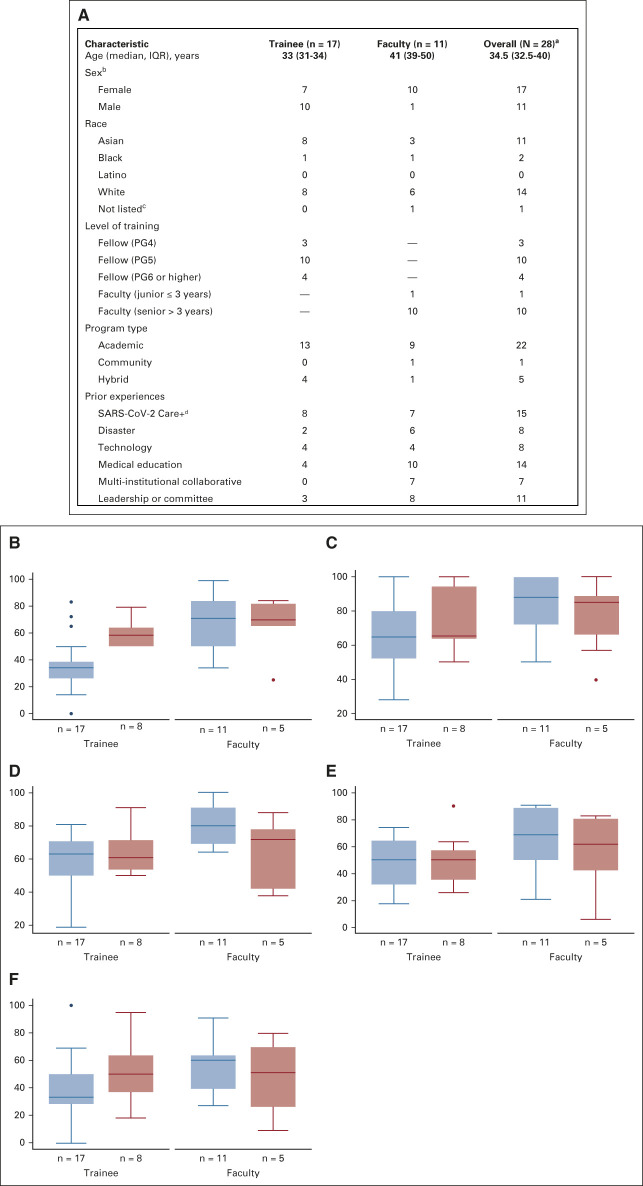
The leadership team was composed of clinical fellows (n = 17) and faculty (n = 11) from 13 US Hematology-Oncology training institutions (Fig 2). Sex was equally represented among trainees, whereas faculty members were predominantly female. Most leadership members identified as White or Asian. The majority worked at academic institutions, with hybrid and community institutions also represented. Compared with faculty, trainees were significantly less likely to have previous multi-institutional collaboration, committee leadership, or educational research experiences (Pearson's chi-square P < .01).
FIG 2.
(A) Baseline characteristics of program leadership members. (B-F) Baseline (blue: trainee n = 17 and faculty n = 11) and postpilot (red: trainee n = 8 and faculty n = 5) box plots of self-assessed confidence 100-point scale (0 = very uncomfortable and 100 = very comfortable). Median (IQR): (B) leading a multi-institutional collaborative: trainee 34 (26-39) and 58.5 (50-64) and faculty 71 (50-84) and 70 (65-82), (C) serving as active member of committee or leadership team: trainee 65 (52-80) and 65 (63.5-94.5) and faculty 88 (72-100) and 85 (66-89), (D) creating an educational curriculum: trainee 63 (50-71) and 61 (53.5-71.5) and faculty 79 (69-91) and 72 (42-78), (E) conducting educational research: trainee 50 (32-65) and 50 (35.5-57) and faculty 69 (50-89) and 62 (42-81), and (F) creating and analyzing mixed methods data: trainee 33 (28-50) and 50 (37-64) and faculty 60 (39-64) and 51 (26-70). aThirteen US training programs were represented. bOptions: nonbinary and prefer not to answer had no responses. cOptions: Pacific Islander and Native American had no responses. Middle Eastern or North African option was not provided. dOptions included 11 clinical COVID-19–focused experiences: screening, general care (oncology and nononcology), intensive care (oncology and nononcology), ventilator management, chemotherapy alteration, telehealth, goals of care discussion, emergency department, and others. IQR, interquartile range; PG, program year.
Self-assessed leadership confidence.
At project onset, n = 17 trainees reported generally lower confidence serving in educational leadership roles compared with n = 11 faculties. In leading a multi-institutional collaborative, trainees rated themselves a median 34 of 100 (interquartile range [IQR] 26-39) compared with a faculty median 71 (IQR 50-84; Wilcoxon Rank-sum P < .01), and in serving as an active member of a committee or leadership team, trainees rated themselves a median 65 (IQR 52-80) versus a faculty median 88 [(IQR 72-100) (P = .01)].
At the conclusion of the pilot, n = 8 trainees reported higher confidence in leading a multi-institutional collaborative, median 58.5 (IQR 50-64) compared with their individually matched baseline (Wilcoxon Signed Rank P = .04). No other significant changes in educational leadership skills confidence were observed in either trainees or faculty.
Session Outcomes
Demographics and attendance.
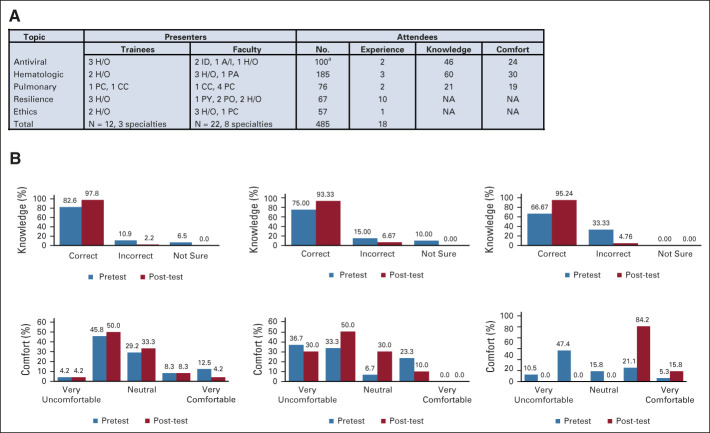
In 6 weeks, the H/O CO-VID Learning Initiative recruited 12 trainees and 22 faculties, representing 17 institutions and eight medical specialties, to produce five, hour-long teleconferences (Fig 3). Session attendance was 100 (antiviral), 185 (hematologic), 76 (pulmonary), 67 (provider resilience), and 57 (ethical decision making). The initial conference was capped at 100 because of Zoom Pro restrictions.
FIG 3.
(A) Characteristics of session presenters and attendees. Experience: previous experience in managing topic-related complications in patients with COVID-19. Number of participants providing both pre- and post-test polling data for knowledge and comfort questions. (B) Group-level knowledge and comfort changes among attendees providing both pre- and postconference polling data. Among n = 46 antiviral knowledge respondents, preconference answers were 82.6% correct, 10.9% incorrect, and 6.5% not sure compared with postconference answers in which 97.8% correct, 2.2% incorrect, and 0% not sure. Similar trends were observed for anticoagulation (n = 60) and pulmonary (n = 21) conferences. Among n = 24 antiviral comfort respondents, preconference answers were 4.2% very uncomfortable, 45.8% uncomfortable, 29.2% neutral, 8.3% comfortable, and 12.5% very comfortable. A similar distribution was observed in antiviral comfort postconference answers. For anticoagulation (n = 30), postconference answers appeared to consolidate around uncomfortable or neutral compared with preconference. For pulmonary (n = 19), answers shifted from a roughly equal preconference distribution to 84.2% comfortable and 15.8% very comfortable postconference. aEntry capped at 100 because of limitations of ZoomProTM. A/I, allergy or immunology; CC, cardiology critical care; ID, infectious disease; H/O, hematology-oncology; NA, not available; PA, pathology; PC, pulmonology critical care; PO, psychology; PY, psychiatry.
Attendee response rates ranged approximately 20%-30%. Among the 100 antiviral session attendees, 31 provided demographic data, in which there were four faculties, 26 fellows, and one resident or student. Two had previous experience in prescribing antivirals or immunologic therapies for patients with COVID-19. Other sessions were similar, with low overall response rates preventing reporting on demographics other than level of training, and few attendees citing previous topic-related COVID-19 experience.
Knowledge and comfort.
Among attendees providing both pre- and postdata, antiviral (n = 46) group preconference knowledge was 82.6% correct, 10.9% incorrect, and 6.5% not sure compared with postconference 97.8% correct, 2.2% incorrect, and 0% not sure. Similar group trends were observed for anticoagulation and pulmonary conferences. Evaluating paired individual answers, attendees appeared more likely to gain knowledge in the anticoagulation (McNemar P < .01) and pulmonary lectures (P = .03), but not in the antiviral lecture (P = .13). Provider resilience and ethics sessions focused on reflective group and personal experiences through word clouds (data not shown).
Regarding comfort with session learning objectives, for prescribing immunologic therapies (n = 24), group preconference responses were 4.2% very uncomfortable, 45.8% uncomfortable, 29.2% neutral, 8.3% comfortable, and 12.5% very comfortable. Group postconference responses were similar in distribution. Group pre- and postsession comfort navigating evidence-based anticoagulation protocols (n = 30) and managing noninvasive and invasive ventilation (n = 19) is shown in Figure 3B. Evaluating paired individual answers, for the antiviral and anticoagulation sessions, most attendees maintained the same level of comfort, 62.9% and 63.3%, respectively, but overall, attendees were more likely to increase rather than decrease comfort, 37.1% increase vs. 0% decrease in the antiviral session (Wilcoxan Signed Rank P < .05) and 26.6% increase vs. 10% decrease in the anticoagulation session (P = .07). For the pulmonary session, 78.9% gained comfort, whereas 21.1% remained at the same comfort level and 0% lost comfort (P < .01).
DISCUSSION
The H/O CO-VID Learning initiative accomplished its primary purpose of developing a trainee-led multi-institutional, multidisciplinary, and virtual learning environment for the purposes of sharing COVID-19 experiences and knowledge. The secondary purpose of accomplishing initiative goals produced mixed results. Lessons learned from this process, including reflections on the appropriateness and accomplishment or underperformance of goals, will help guide future efforts to sustain medical education during disasters.
Having no baseline infrastructure, funding, or trainees experienced in educational programming, the H/O CO-VID Learning Initiative built a multi-institutional virtual learning environment reaching 19 institutions and hundreds of trainees and faculty in 6 weeks. The subcommittee structure allowed trainees to select areas of interest, work closely with other trainees and faculty, provide clear expectations, and allow for parallel workflows. ASCO-affiliated networks provided early outreach, but a lack of additional networks and funding hindered greater outreach. Reliance on free versions of virtual tools led to several problems, including caps on meeting duration and attendance, requirements for attendees to create accounts before participating in polling, and inconsistency in data formatting. After acquiring greater institutional support, many of these issues were improved or corrected by the end of the pilot.
Applying Kern's stepwise approach, the initiative rapidly put together a five-session curriculum on the basis of a sequential selection of learning needs, goals, and objectives. This manuscript focused on the process of creating goals. Information on individual reasons or motivations behind goals is provided in the companion literature.34 Early adoption of this approach prospectively revealed needs to address ethical dilemmas and burnout, needs that were retroactively identified in previous disaster educational initiatives.24 On the other hand, because Kern's approach was not designed for disaster curricula, several evaluations were not well-suited for initiative goals.
The goal of producing weekly output stemmed from the initial sense of urgency around COVID-19 and is unlikely to translate to standard medical learning.
The initiative brought together a diverse community of 19 institutions, eight disciplines, and hundreds of participants; however, west coast and community programs and racial minorities were under-represented. Time zone differences impaired coordinating live meetings with west coast programs. Several participating programs initially classified as community requested reclassification as hybrid, acknowledging an academic affiliation. Finally, to the extent that ASCO networks were the primary mechanism for outreach, ensuring that these networks promote inclusion among racial minorities and community programs is critical.
During a pandemic, trainees successfully led an educational initiative and collaborated on scholastic presentations and manuscripts.16,31,33,34 Trainee self-confidence improved in leading a multi-institutional initiative but not in other leadership or educational skills. Trainees increasingly desired more training in teaching methods and theories, which remained unfulfilled at the conclusion of this pilot. This desire exposes a potential need for formalized scholastic education pathways for trainees.
The constantly evolving nature of COVID-19 knowledge and feelings made it challenging to find appropriate evaluation tools for these goals. For example, although the initiative might have disseminated knowledge on learning objectives, many learning objectives quickly became obsolete as new information emerged, raising questions about the value of this measure. Evaluating whether learners can identify key strengths or limitations from available evidence may be a more meaningful measure of self-efficacy. Q&A segments received consistently positive feedback in debriefs, particularly with respect to building consensus around experiences and practice patterns.
Finally, although the initiative addressed ethical dilemmas and burnout, attendance was lower in these sessions. Reasons for declining attendance were discussed among trainees and included later topics no longer meeting perceived needs, redundancy with other COVID-19 learning, or a desire to transition back to standard hematology-oncology learning.
A process-oriented learning model, the H/O CO-VID Learning Initiative, was not designed to prove dissemination of knowledge, nor make comparisons with other medical education models. Session response rates of 20%-30% prevented assessments of whether observations were attributable to all attendees or only subgroups and created potential for nonresponse bias. Reasons for low response rates included late-arriving attendees with competing duties, voluntary participation, technologic difficulties, and unfamiliarity in navigating a novel learning environment. The largest subgroup was hematology-oncology clinical fellows from academic programs. No significant post-test dropout was observed among attendees. To negate or reverse the observed associations, nonresponders would have needed to disproportionately unlearn concepts or become less comfortable.
A subset of authors contributed to research data, creating potential for author conflicts of interest. Consideration of manuscripts and authorship occurred after all data collection, the deidentified nature of survey data precluded author selection on the basis of data participation, and the purpose of this manuscript was to describe the process of creating the initiative, rather than demonstrating statistically significant outcomes.
Given the role of virtual learning environments during disasters, developing permanent structures that can provide prompt, consistent support during the next disaster is critical. This could relieve educators from creating infrastructure, prevent redundancy, reduce technical difficulties, and improve response rates. Efforts to create and validate disaster learning evaluation tools are needed. To improve formalized educational training, future initiatives could invite graduates of the American Society of Hematology Medical Educators Institute and ASCO Education Scholars Programs to serve as faculty mentors.
In conclusion, this manuscript presents a framework for how GME initiatives can rapidly leverage virtual learning to develop multi-institutional collaborations, provide trainees with educational leadership experiences and access to multi-disciplinary experts, and incorporate trainee leadership in all aspects of initiative development. Future endeavors would benefit from establishing a more permanent technology platform, ensuring greater minority and community program representation, and incorporating more formalized educational leadership and mentoring development for trainees.
Shonali Midha
Stock and Other Ownership Interests: AbbVie, Moderna Therapeutics
Jori May
Stock and Other Ownership Interests: Roche, Novartis, Thermo Fisher Scientific
Emily Collier
Research Funding: Mirati Therapeutics
Nikesh Shah
Honoraria: MJH Life Sciences
Samuel Rubinstein
Honoraria: Sanofi
Consulting or Advisory Role: Roche
Jill Gilbert
Leadership: Tennessee Oncology
Honoraria: UpToDate, Bayer, Loxo/Bayer, Exelixis, HRA Pharma
Consulting or Advisory Role: Bayer, HRA Pharma, Exelixis
Research Funding: Pfizer, Exelixis
Christine M. Lovly
Honoraria: Novartis, Takeda, Pfizer, Cepheid, Foundation Medicine, AstraZeneca, Blueprint Medicines, Achilles Therapeutics, Lilly, Genentech, Syros Pharmaceuticals, Amgen, Roche, EMD Serono
Consulting or Advisory Role: Novartis, Foundation Medicine, Pfizer, Takeda, Cepheid, AstraZeneca, Blueprint Medicines, Achilles Therapeutics, Syros Pharmaceuticals, Genentech, Lilly, Amgen, EMD Serono
Research Funding: Novartis, Xcovery, AstraZeneca
Travel, Accommodations, Expenses: Pfizer, Takeda, Foundation Medicine, Novartis, Cepheid, Genentech
Nagashree Seetharamu
Consulting or Advisory Role: AstraZeneca, Genentech, Takeda, Amgen, Boehringer Ingelheim
Deepa Rangachari
Honoraria: AstraZeneca
Consulting or Advisory Role: Advance Medical, DynaMed
Research Funding: Bristol Myers Squibb, Novocure, AbbVie/Stemcentrx
Open Payments Link: https://openpaymentsdata.cms.gov/physician/941245
Martina Murphy
Consulting or Advisory Role: Pfizer
Elizabeth Henry
Consulting or Advisory Role: Seattle Genetics/Astellas
Research Funding: Seattle Genetics/Astellas, Bristol Myers Squibb, Nektar
Frances Collichio
Research Funding: Amgen, Novartis, Merck, Replimune, Nektar
Other Relationship: ACGME
Jennifer R. Green
Honoraria: Scripps Hospital
Travel, Accommodations, Expenses: Scripps Hospital
No other potential conflicts of interest were reported.
AUTHOR CONTRIBUTIONS
Conception and design: Richard L. Martin III, Michael J. Grant, Stephen Kimani, Jori May, Rushad Patell, Emily Collier, David Furfaro, Charles Bodine, Nikesh Shah, Jess DeLaune, Samuel Brusca, Samuel Rubinstein, Nausheen Hakim, Sabrina L. Browning, Laura Sena, Jill Gilbert, Christine M. Lovly, Nagashree Seetharamu, Deepa Rangachari, Martina Murphy, Elizabeth Henry, Frances Collichio, Jennifer R. Green
Provision of study materials or patients: Shonali Midha, Deepa Rangachari
Collection and assembly of data: Richard L. Martin III, Michael J. Grant, Stephen Kimani, Rushad Patell, Emily Collier, Leo Reap, Jess DeLaune, Samuel Brusca, Coral Olazagasti, Shreya Goyal, Samuel Rubinstein, Shuai Qin, Martina Murphy, Monica Chatwal, Frances Collichio, Jennifer R. Green
Data analysis and interpretation: Richard L. Martin III, Michael J. Grant, Shonali Midha, Rushad Patell, Emily Collier, Jill Gilbert, Mario Davidson, Martina Murphy, Monica Chatwal, Rita Paschal, Elizabeth Henry, Frances Collichio, Jennifer R. Green
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Forming the Hematology-Oncology Collaborative Videoconferencing (CO-VID) Learning Initiative: Experiential Lessons Learned From a Novel Trainee-Led Multidisciplinary Virtual Learning Platform
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Shonali Midha
Stock and Other Ownership Interests: AbbVie, Moderna Therapeutics
Jori May
Stock and Other Ownership Interests: Roche, Novartis, Thermo Fisher Scientific
Emily Collier
Research Funding: Mirati Therapeutics
Nikesh Shah
Honoraria: MJH Life Sciences
Samuel Rubinstein
Honoraria: Sanofi
Consulting or Advisory Role: Roche
Jill Gilbert
Leadership: Tennessee Oncology
Honoraria: UpToDate, Bayer, Loxo/Bayer, Exelixis, HRA Pharma
Consulting or Advisory Role: Bayer, HRA Pharma, Exelixis
Research Funding: Pfizer, Exelixis
Christine M. Lovly
Honoraria: Novartis, Takeda, Pfizer, Cepheid, Foundation Medicine, AstraZeneca, Blueprint Medicines, Achilles Therapeutics, Lilly, Genentech, Syros Pharmaceuticals, Amgen, Roche, EMD Serono
Consulting or Advisory Role: Novartis, Foundation Medicine, Pfizer, Takeda, Cepheid, AstraZeneca, Blueprint Medicines, Achilles Therapeutics, Syros Pharmaceuticals, Genentech, Lilly, Amgen, EMD Serono
Research Funding: Novartis, Xcovery, AstraZeneca
Travel, Accommodations, Expenses: Pfizer, Takeda, Foundation Medicine, Novartis, Cepheid, Genentech
Nagashree Seetharamu
Consulting or Advisory Role: AstraZeneca, Genentech, Takeda, Amgen, Boehringer Ingelheim
Deepa Rangachari
Honoraria: AstraZeneca
Consulting or Advisory Role: Advance Medical, DynaMed
Research Funding: Bristol Myers Squibb, Novocure, AbbVie/Stemcentrx
Open Payments Link: https://openpaymentsdata.cms.gov/physician/941245
Martina Murphy
Consulting or Advisory Role: Pfizer
Elizabeth Henry
Consulting or Advisory Role: Seattle Genetics/Astellas
Research Funding: Seattle Genetics/Astellas, Bristol Myers Squibb, Nektar
Frances Collichio
Research Funding: Amgen, Novartis, Merck, Replimune, Nektar
Other Relationship: ACGME
Jennifer R. Green
Honoraria: Scripps Hospital
Travel, Accommodations, Expenses: Scripps Hospital
No other potential conflicts of interest were reported.
REFERENCES
- 1.Garzaro G, Clari M, Ciocan C, et al. : COVID-19 infection and diffusion among the healthcare workforce in a large university-hospital in northwest Italy. Med Lav 111:184-194, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 Module Data Dashboard—Hospital Capacity Snapshot. National Healthcare Safety Network (NHSN). Atlanta, GA, Centers for Disease Control and Prevention [Google Scholar]
- 3.Sanger-Katz M, Kliff S, Parlapiano A. These places could run out of hospital beds as coronavirus spreads. New York Times, March 17, 2020 [Google Scholar]
- 4.Ranney ML, Griffeth V, Jha AK: Critical supply shortages—The need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med 382:e41, 2020 [DOI] [PubMed] [Google Scholar]
- 5.Strategies for Optimizing the Supply of N95 Respirators. Atlanta, GA: Centers for Disease Control and Prevention, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html [Google Scholar]
- 6.Strategies to Mitigate Healthcare Personnel Staffing Shortages : Healthcare Workers Coronavirus Disease 2019. Atlanta, GA, Centers for Disease Control and Prevention [Google Scholar]
- 7.American Society of Hematology : Trainees on the Front Lines of COVID-19: An Interview with Dr. Nicole Cruz of New York Presbyterian Hospital, 2020. https://www.hematology.org/education/trainees/fellows/trainee-news/2020/trainees-on-the-front-lines-of-covid-19 [Google Scholar]
- 8.ACGME Response to Pandemic Crisis. https://acgme.org/covid-19 [Google Scholar]
- 9.Knowles MS, Holton EF, Swanson RA: The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development (ed 6). Amsterdam, the Netherlands, Elsevier, 2005 [Google Scholar]
- 10.Hilburg R, Patel N, Ambruso S, et al. : Medical education during the coronavirus disease-2019 pandemic: Learning from a distance. Adv Chronic Kidney Dis 27:412-417, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Considerations for Institutes of Higher Education : Community, Work & School Coronavirus Disease 2019. Atlanta, GA, Centers for Disease Control and Prevention [Google Scholar]
- 12.Rose S: Medical student education in the time of COVID-19. JAMA 323:2131-2132, 2020 [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb M, Landry A, Egan DJ, et al. : Rethinking residency conferences in the era of COVID-19. AEM Educ Train 4:313-317, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balanchivadze N, Donthireddy V: Hematology/oncology fellowship emergency restructuring in response to the COVID-19 pandemic—Henry Ford Hospital, Michigan. JCO Oncol Pract 16:e943-947, 2020 [DOI] [PubMed] [Google Scholar]
- 15.Porfidia A, Pola R: Venous thromboembolism and heparin use in COVID-19 patients: Juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines. J Thromb Thrombolysis 50:68-71, 2020. [Erratum: J Thromb Thrombolysis 50:477, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patell R, Midha S, Kimani S, et al. : Variability in institutional guidance for COVID-19-associated coagulopathy in the United States. Thromb Haemost 120:1725-1732, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritschl PV, Nevermann N, Wiering L, et al. : Solid organ transplantation programs facing lack of empiric evidence in the COVID-19 pandemic: A by-proxy society recommendation consensus approach. Am J Transpl 20:1826-1836, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cornwall W, Kaiser J, Kupferschmidt K, et al. : The United States leads in coronavirus cases, but not pandemic response. Science, April 1, 2020 [Google Scholar]
- 19.Davis D, Ryan D, Sibbald G, et al. : Severe acute respiratory syndrome and the delivery of continuing medical education: Case study from Toronto. J Contin Educ Health Prof 24:76-81, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Lim ECH, Oh VMS, Koh DR, et al. : The challenges of “continuing medical education” in a pandemic era. Ann Acad Med Singap 38:724-726, 2009 [PubMed] [Google Scholar]
- 21.Mo Y, Archuleta S, Salmon S, et al. : Residency training at the front of the West African Ebola outbreak: Adapting for a rare opportunity. PLoS Curr 8:ecurrents.outbreaks.2ccbcab30e96d3fe28d3896d258b818e, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lopez NY, Hernandez-Suarez DF, Marrero-Ortiz W, et al. : Challenges and opportunities after hurricane Maria: University of Puerto Rico medical students' perspectives. J Grad Med Educ 10:382-384, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnett-Vanes A, Hassounah S, Shawki M, et al. : Impact of conflict on medical education: A cross-sectional survey of students and institutions in Iraq. BMJ open 6:e010460, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redinger JW, Cornia PB, Albert TJ: Teaching during a pandemic. J Grad Med Educ 12:403-405, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon M, Patricio M, Horne L, et al. : Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Med Teach 42:1202-1215, 2020 [DOI] [PubMed] [Google Scholar]
- 26.Goldie JGS: Connectivism: A knowledge learning theory for the digital age? Med Teach 38:1064-1069, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Taylor DCM, Hamdy H: Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach 35:e1561-e1572, 2013 [DOI] [PubMed] [Google Scholar]
- 28.Gil Rivas V, Kilmer RP: Building community capacity and fostering disaster resilience. J Clin Psychol 72:1318-1332, 2016 [DOI] [PubMed] [Google Scholar]
- 29.Thakur A, Soklaridis S, Crawford A, et al. : Using rapid design thinking to overcome COVID-19 challenges in medical education. Acad Med 96:56-61, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas PA, Kern DE, Hughes MT, et al. : Curriculum Development for Medical Education: A Six-Step Approach (ed 4). Baltimore, MD, Johns Hopkins University Press, 2016 [Google Scholar]
- 31.Martin R, Kimani S, May J: Mentoring Oncologists in the Era of Social Distancing, Volume 1. Oncology Fellows, 2020. https://www.onclive.com/view/mentoring-in-the-era-of-social-distancing [Google Scholar]
- 32.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377-381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin RL, Green J, Henry E, et al. : The Heme/Onc COVID Learning Initiative: Trainees Step Up to Build a Novel Virtual Shared Learning Platform. ASCO Connection, 2020. https://connection.asco.org/tec/career/hemeonc-covid-learning-initiative-trainees-step-build-novel-virtual-shared-learning [Google Scholar]
- 34.Grant MJ, Martin RL, Olazagasti C, et al. : Hematology Oncology Collaborative Videoconferencing Learning Initiative: Unleashing the Potential of Trainees as Leaders in Medical Education. Harvard Macy Institute Education Blog, 2020. https://harvardmacy.org/index.php/hmi/hematology-oncology-collaborative [Google Scholar]
- 35.WHO : WHO COVID-19 Dashboard. Geneva, Switzerland: World Health Organization, 2020. https://covid19.who.int/ [Google Scholar]