Abstract
Exercise training is known to reduce CVD risk factors; however, in tactical populations, like veterans and firefighters, the effects of different forms of exercise such as tactical circuit training (CT) or conventional resistance training (RT) is unclear. Thus, the purpose of this study was to compare changes in various CVD risk measures after 4-week tactical CT or RT programs. Thirty-seven firefighters (20 CT, 17 RT), 35% of whom were veterans, participated. Pre- and post-intervention measures included body fat (BF%), carotid artery intima media thickness (IMT), central and brachial BP, and indices of arterial stiffness (augmentation index, Aix@75), myocardial oxygenation (subendocardial viability ratio, SEVR), and endothelial function (flow-mediated dilation, FMD). Estimation of maximum oxygen consumption (VO2peak) for aerobic fitness, balance, muscular endurance, and strength were also compared. For the clinical laboratory values, there were no between group differences and the only within group change was found in triglyceride levels. Tactical CT lowered triglyceride levels by 24.2% (P < 0.05). Only tactical CT exercise lowered BP. Both brachial (4.6% reduction) and central (4.4 % reduction) systolic and diastolic SBP and DBP decreased with CT (all P ≤ 0.01). After training we found improvements in FMD and SEVR with tactical CT only. Percent FMD increased by 28.7% (P < 0.01) while SEVR increased by 4.4% (P < 0.05) in the tactical CT group. Fitness improved in both cohorts (P < 0.05). These data suggest that 4 weeks of a CT program improves several CVD-risk factors and may be more beneficial.
Keywords: Vascular health, blood pressure, intervention, firefighters, occupational fitness
INTRODUCTION
According to the American Heart Association (AHA), over 90% of adults have at least one cardiovascular disease (CVD) risk factor. The AHA defines ideal heart health as the absence of clinically manifested CVD with a focus on reducing modifiable risk factors (40). In certain populations, like veterans and firefighters, increased risk of CVD is especially concerning.
Current military studies have reported that CVD risk is on the rise in younger active and reserve service members while veterans still have worse health profiles than their active-duty counterparts (26, 20). Compared to civilians, the prevalence of increased CVD risk is higher in military populations (37) and in firefighters, (17) but in firefighters 50% of line-of-duty deaths (LODD) are cardiac-related (17). In fact, CVD risk in tactical populations may be a combination of physical and emotional stress due to the nature of the job. Tactical operations and combat training are exposures that influence stress responses in the military and para-military population which have known relation to CVD and acute cardiac incidents (17). Also, many firefighters and military service members have hypertension. Blood pressure (BP) control remains an issue with 75% of hypertensive firefighters not having their BP under control (23). The fire service is a para-military organization, attractive to veterans looking to find a career that shares a similar mission as active-duty service, so understanding firefighter cardiac health and the potential benefits of tactical training may be important for military who are planning to retire.
Civilian-based studies have reported that exercise training reduces CVD risk, leads to improvements in BP and other indices of vascular health, and is associated with lower mortality (8). Military organizations have strict exercise standards and routine testing occurs in active-duty service members, yet the fire service is not the same. The National Fire Protection Agency (NFPA) recognizes the benefits of exercise on overall health yet does not require fire companies to have a fitness program for their crews. In fact, less than 30% of the stations do (10). It has been estimated that the work involved with firefighting requires a VO2max fitness level of 42 ml·kg-1·min-1, but surprisingly only 20% of firefighters meet this threshold (31). Search and rescue work done while wearing PPE places a significant demand on the metabolic and cardiovascular systems, which is a large risk for those with low fitness levels and compromised cardiovascular health. Much like civilians, an inverse relationship exists between fitness and CVD risk or injury in firefighters (11) and in military personnel (4). To date, very few exercise-training studies have been published in firefighters.
Data on firefighter vascular health and exercise is also limited. Recently, we found that short-term circuit training (CT) increased flow-mediated dilation (FMD) and decreased carotid artery intima-media thickness (IMT) levels in firefighters. The firefighters had a larger improvement in health with exercise training compared to civilians (18). In another CT intervention study, Roberts et al. found improvements in body composition and fitness with a 16-week program that included exercises simulating fire-ground activities (32). Specifically, resistance training (RT) studies in firefighters are sparce. Beach et al. found improvements in fitness and strength with a 12-week RT program in career firefighters (2). To date, there has not been a comparison study between tactical CT exercise and traditional RT and there is no clear consensus on which type(s) of exercise (aerobic, resistance, or combination) may be optimal for reducing CVD risk, in any population.
Tactical CT is a type of combination training that incorporates multi-joint exercises with both aerobic and resistance components using occupation-specific tools. The AHA recommends that physicians counsel patients to increase physical activity, yet the type or length of training program required to elicit clinical improvement is not established (39). Thus, the purpose of this study was to compare changes in selected CVD risk and vascular health markers between 4-weeks of tactical CT and 4-weeks of RT in a group of firefighters. We tested the hypotheses that compared to RT, a CT program would result in greater improvements in various indices of vascular health.
METHODS
Participants
A power analysis was conducted with G*Power 3.1 (Germany) determined that 28 participants were needed (14 per group) for a power of 0.824, with an effect size of 0.5 and an α = 0.05. Firefighters were recruited from departments located in the suburban Philadelphia area. Overall, 54 firefighters were screened for the study; 46 met the inclusion criteria and were enrolled. Criteria for inclusion were no more than one BP medication and no more than one cholesterol medication; no prior cardiovascular incidents, diagnosed heart disease or diabetes; non-smoker, and no physical limitation that would preclude an exercise program. Greater than 70% adherence to the intervention was required. Each firefighter read and signed the informed consent and completed a general health history form. The protocol was approved by Institutional Review Board, and all procedures were in accordance with the ethical standards of the Helsinki Declaration. This research was carried out fully in accordance with the ethical standards of the International Journal of Exercise Science (29).
Protocol
This was a prospective cohort study. All enrolled firefighters completed pre-testing, a 4-week exercise intervention (CT or RT), and post-testing within 24–48 hours of the last training bout. The pre- and post-testing included two visits each: a fasted and a fitness appointment. Each post-test session was administered in the same manner and at the same time of day as pre-testing. Due to renovations and closure of the campus fitness facility during the initial 6 months of the study, the tactical CT cohort completed the intervention first followed by the RT cohort, who needed the weight-room. The vascular health measures collected at the fasted visit were pulse wave analysis (PWA), FMD, and IMT. The work of military and paramilitary personnel involves exertion, balance, lifting, climbing, dragging, pulling objects, and crawling. Occupational requirements pose demands on all aspects of health and fitness, so a variety of fitness tests were completed at the fitness testing session, including, power, muscular endurance, muscular strength, balance, and a dummy drag.
Fasted Testing: Firefighters were asked to refrain from exercise for 24 hours prior, as well as food, medication, and caffeine for at least 10 hours prior to the fasted test. Height and weight were measured using a stadiometer and digital floor scale (Adam Equipment Inc., Oxford, CT) without shoes. Body mass index (BMI) was calculated and recorded. Body fat percentage (BF%) was estimated by whole-body bioelectrical impedance analysis (BIA) in accordance with the manufacturer’s instructions. (ImpediMed DF50, San Diego, CA). Brachial BP measurements were obtained at each appointment in accordance with clinical guidelines using an aneroid sphygmomanometer (Medline Industries, Mundelein, IL) (41). The measurements were performed in duplicate each visit, with the overall mean brachial systolic and diastolic BP reported. Serum glucose levels and lipid levels, including total cholesterol, LDL-cholesterol (LDL), HDL-cholesterol (HDL), and triglycerides (TG) were measured using the Alere Cholestech LDX® lipid profile system (San Diego, CA). Alere Cholestech lipid profile values correlate with venous plasma measured in clinical diagnostic laboratories (r >0.95).
All vascular measurements were collected after the firefighter had rested supine for 15 minutes. Radial artery PWA waveform images were acquired with applanation tonometry (SphygmoCor, AtCor Medical, Australia). PWA is valid, reliable, and provides multiple biomarker measurements: including central aortic systolic and diastolic BP, augmentation index (Aix@75) adjusted to heart rate (HR) of 75 beats per minute, and subendocardial viability ratio (SEVR). (9) Central BP is argued to be more relevant than peripheral BP for determining CVD risk and thus has gained prognostic significance recently (33). AIx@75 is a measure of arterial stiffness which is an independent marker of premature CVD (30). SEVR is an estimate of myocardial oxygenation related to cardiac workload and is used as an indicator of coronary blood flow (39).
Data from quality pulse waveforms were considered acceptable using software’s internal quality control index (operator index >80%). The average of three measures is reported. We have calculated the intraclass correlation coefficient (ICC) for PWA measurements at >0.97. Next, FMD and IMT measurements were completed as previously described (14). FMD is an index of nitric oxide-mediated endothelial-dependent function, which assesses blood vessel vasodilatory function (8). The ICC for baseline diameter, peak diameter, and FMD are 0.94, 0.94, and 0.73 respectively. Intra-observer reliability for the image analysis using the analysis software has been established at 99.2%. Carotid artery IMT is an index of plaque build-up, atherosclerotic potential, and vascular remodeling (34). We have calculated the ICC for IMT measurements at 0.90, with interobserver variability <0.04 mm and intra-observer variability <0.02 mm. To the best of our knowledge, no study has measured these vascular markers in firefighters in response to exercise training.
Fitness Testing: Firefighters reported to the facility on a separate day for fitness testing which included assessment tests listed in the NFPA 1583 Standard on Health-Related Fitness Programs (28). First, after 5 minutes of seated rest, brachial BP was measured. Next, the Bruce maximal treadmill protocol was used to estimate peak oxygen consumption. Heart rate and EKG were continuously monitored (CardioCard, NY, NY), and VO2peak was calculated using termination time, which was measured at the exact timepoint when the test was stopped. (16). Following the treadmill test, the firefighters completed a battery of other fitness tests, each test was followed by a 5-minute rest. First, they completed a stair climb test where they were asked to continuously climb up and down for 2 minutes, and the number of steps was recorded. The stair climb test has been reported as a quality measure of overall fitness in firefighters and is a task performed during the candidate physical ability test (CPAT) (35). The next fitness test completed was a 12-step sprint which was used to indirectly evaluate power. Faster stair sprinting is suggestive of higher speed generation and more explosive power, which are both physical attributes necessary for any military-like occupation (6). Muscular endurance was tested using a prone plank test and a stationary wall sit. The WFI prone static plank test has been used to test firefighter fitness (28, 27). The stationary wall sit test was a timed test with the firefighter squatting down to sitting position, with legs bent at 90°, knees directly over the heels, and back flat against the wall. Finally, balance was assessed. We included a simple single-leg static balance test as part of the pre- and post-fitness testing where time balance was held was recorded for each leg. Even though balance testing is not part of the NFPA fitness standard, part of the CPAT, or part of any military combat testing protocol, it is well established that all combat-related or rescue-type activities require balance. Also, prior research has shown that firefighters with impaired balance have lower fitness levels, and that a relationship between balance, strength and movement ability exists (25). Strength was measured directly by 1RM for the RT cohort and indirectly by a rescue dummy drag test for the CT cohort. Absolute muscular strength was assessed using 1RM bench press (upper body) and 45° incline leg press (lower body). The 1RM values were used for the RT programming. Firefighters completed warm-up sets of 8–10 repetitions. The weight was increased progressively while decreasing the repetitions, with 3–4 minutes of rest between sets, until participants could successfully perform 3–5 repetitions, and from these data the 1RM was extrapolated using the NSCA repetition-maximum table. Since the tactical CT program was an absolute training load where all participants used the same workload for the workouts, 1RM data was not needed for this cohort. For the rescue drag test, the firefighters were instructed to grab and drag a 65.9 kg Rescue Randy Training Manikin (Simulaids, Inc, Saugerties, NY) as far as possible in 30 seconds. Distance was recorded in meters. These mannequins were developed for lifelike simulations involving rescue, extrication, and confined space and have been used by the military, fire, police, and emergency personnel worldwide, and a rescue drag test is one of the specific tasks included in the CPAT (35).
Training Programs: Student trainers worked with firefighters for the first 2 exercise sessions to teach proper technique. After that, the intervention was self-reported weekly by phone or email. The tactical CT program was completed 3 times per week and included 6 stations of occupation-specific exercises which were completed 3 times per workout. The stations included 1) 40-lb extrication tool carry for 100 ft; 2) 3-minute stair climb; 3) 45-second plank pose; 4) 20-lb tool carry with a fast walk for 100 ft; 5) right and left single leg stands for as long as balance was maintained; and 6) 15-lb tool carry up and down 30 stairs. Firefighters were recommended to complete the circuit at the firehouse using hose line, fireground tools, or extrication tools. If they chose to complete the workout at home, they were recommended to select items of the appropriate weight or use dumbbells or weight plates for each station.
The RT program was also completed 3 times per week, where participants alternated between two different workouts. Three sets of 8–12 repetitions per exercise were performed with dumbbells at 70–80% 1RM, with 2–3 minutes of rest. Workout 1 included squat to shrug, bent arm pullovers, side lunge, bent-over rows, dumbbell dead lifts, supine dumbbell extension, incline row, and bicep curl. Workout 2 included dumbbell step-ups, chest press, squat, overhead press, inclined chest press, lateral raise, and reverse fly. Each workout was followed by three sets of abdominal exercises including sit-ups, planks, knee-up crunches, and Russian twists.
Statistical Analysis
Data are presented as mean ± SD. Distribution of all variables was examined using the Shapiro-Wilk test of normality, and homogeneity of variances was determined using Levene’s test. Nonparametric tests were used when appropriate. Paired t-tests were used to assess the mean differences between pre- and post-exercise values. One-way ANOVA and independent t-test were used to evaluate time by group interactions, and within-group Tukey’s post hoc analysis was performed. Alpha level of P < 0.05 was required for statistical significance. All statistical analyses were performed using SPSS version 24.0 (SPSS, Chicago, IL).
RESULTS
Forty-six firefighters who met inclusion criteria were enrolled, with 37 completing the intervention. Seven of the firefighters did not return, one did not complete post-testing, and one did not meet 70% adherence, so they were removed from analysis. Twenty firefighters (17M, 3W) completed the tactical CT program with an overall adherence to exercise of 97.1% (7 sessions missed overall). Seventeen firefighters (15M, 2W) completed the traditional RT intervention with an overall adherence to exercise of 93.9% (10 sessions missed overall). We had 13 veterans (35%) in the study population, which is higher than the U.S. Census Bureau data reporting 6.9% of adults as veterans (data.census.gov). At pre-test, there were no differences between groups in self-report physical activity (2.4 ± 0.4 CT vs 3.3 ± 0.6 hr·wk-1 RT), in family history of CVD (45% CT vs 58.8% RT), or in medication status.
Table 1 presents the health data for measures before and after the training programs. We found no differences between any variable initially suggesting that the groups were similar at pre-test. There were 3 firefighters in the CT group and 2 in the RT group who reported taking BP medication, and we had 1 firefighter in the CT group who reported taking cholesterol medication. There were no significant changes in weight or BF% with training, even though at post-test the firefighters who completed RT were leaner than those completing the CT (32.3 ± 6.9% CT vs 26.7 ± 9.1% RT, P = 0.04, d = 0.70). Both groups were similar in body composition before intervention. For the clinical laboratory values, there were no between group differences. Within group, tactical CT lowered TG levels by 24.2% (95% CI [5.85,41.93], p = 0.012), but no significant changes were found in other laboratory measures.
Table 1.
Participant characteristics and laboratory values at pre- and post-exercise training.
| Variable | Circuit Training (n = 20) | Resistance Training (n = 17) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Pre | Post | % Change | Pre | Post | % Change | |
| Demographic characteristics | ||||||
| Age (yr) | 40.6 (13.1) | - | - | 41.0 (17.3) | - | - |
| Male/Female | 17/3 | - | - | 15/2 | - | - |
| Family History (y/n) | 9/11 | - | - | 10/7 | - | - |
| Weight (kg) | 90.8 (7.8) | 90.5 (8.1) | −0.4 | 90.6 (12.9) | 90.1 (12.6) | −0.5 |
| BMI (kg·m−2) | 31.1 (5.1) | 30.9 (5.2) | −0.9 | 30.7 (6.8) | 30.6 (6.6) | −0.3 |
| Lean Mass (kg) | 59.9 (5.9) | 61.0 (6.1) | 2.5 | 64.5 (8.3) | 66.5 (8.2) | 2 |
| Body Fat (%) | 33.8 (6.5) | 32.3 (6.9) | −4.6 | 28.3 (9.4) | 26.7 (9.1)** | −5.6 |
| Clinical laboratory values | ||||||
| TC (mg/dl) | 160.6 (27.2) | 155.4 (23.6) | −3.3 | 169.4 (33.9) | 170.7 (38.1) | 1 |
| Triglyceride (mg·dl−1) | 122.4 (60.6) | 98.5 (53.2)* | −24.2 | 84.8 (76.3) | 93.5 (89.5) | 10.1 |
| HDL-C (mg·dl−1) | 41.3 (12.5) | 42.1 (12.1) | 1.9 | 46.7 (13.5) | 48.5 (15.2) | 3.8 |
| LDL-C (mg·dl−1) | 98.5 (53.2) | 95.2 (27.6) | −3.4 | 105.4 (27.5) | 105.4 (26.1) | 0 |
| Glucose (mg·dl−1) | 91.3 (10.3) | 90.4 (7.6) | −0.1 | 93.1 (8.8) | 94.1 (12.6) | 1.1 |
| Blood pressure measures | ||||||
| Brachial SBP (mm Hg) | 127.9 (10.1) | 122.2 (11.1)* | −4.6 | 126.4 (9.7) | 123.8 (5.7) | −2.1 |
| Brachial DBP (mm Hg) | 77.6 (5.5) | 74.3 (6.6)* | −4.4 | 80.6 (6.4) | 78.4 (5.0)** | −2.8 |
| Central SBP (mm Hg) | 114.2 (12.7) | 109.3 (11.6)* | −4.4 | 116.9 (14.8) | 114.3 (8.7) | −2.2 |
| Central DBP (mm Hg) | 77.0 (9.1) | 74.4 (6.4)* | −3.6 | 83.5 (13.1) | 80.4 (8.5)** | −3.8 |
| Vascular measures | ||||||
| FMD (%) | 7.3 (3.4) | 9.4 (4.1)* | 28.7 | 7.9 (3.5) | 8.9 (3.1) | 12.6 |
| FMD norm | 0.53 (0.2) | 0.67 (0.3)* | 34 | 0.91 (0.5) | 0.9 (0.5) | −1 |
| IMT (mm) | 0.49 (0.1) | 0.47 (0.1) | −4.2 | 0.53 (0.1) | 0.5 (0.1) | −4 |
| Aix at 75 | 23.5 (17.4) | 20.7 (15.2) | −11.9 | 23.4 (12.7) | 19.6 (15.5) | −16.2 |
| SEVR (%) | 169.1 (23.8) | 176.5 (28.1)* | 4.4 | 178.6 (34.8) | 174.7 (34.3) | −2.2 |
Mean (± SD). BMI, body mass index; TC, total cholesterol; Family history, reports family history of CVD; HDL, high density lipoprotein; LDL low density lipoprotein; SBP, systolic blood pressure; DBP, diastolic blood pressure; FMD, flow mediated dilation; IMT, intima media thickness; AIX at 75, augmentation index adjusted to 75 beats per minute; SEVR, subendocardial viability ratio.
p < 0.05 before and after training,
p < 0.05 between exercise training groups.
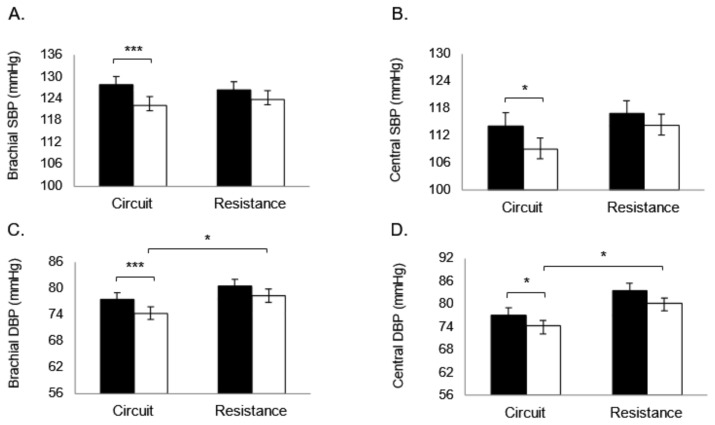
BP data is presented in Figure 1. BP was matched between groups at pre-test, even though both groups had clinically elevated BP. The tactical CT program elicited significant improvements in BP, but the RT program did not. Both brachial (Δ −4.6%, 95% CI [3.49, 7.93], p = 0.001) and central (Δ −4.4%, 95% CI [0.69, 9.10], p = 0.025) SBP decreased with CT. Also, both brachial (Δ −4.4%, 95% CI [1.46, 5.04], p = 0.001) and central (Δ −3.6%, 95% CI [0.01, 5.27], p = 0.041) DBP decreased with CT. Tactical CT intervention seemed to have a better BP effect, as post-intervention DBP levels were higher in firefighters who completed the RT program (74.3 ± 6.6 CT vs 78.4 ± 5 RT brachial, P = 0.041, d = 0.70; 74.4 ± 6.4 CT vs 80.4 ± 8.5 RT central DBP, P = 0.05, d = 0.80).
Figure 1.
Blood Pressure changes (mean ± SD) with exercise training comparisons between 4 weeks of tactical circuit training and 4 weeks of resistance training. Bars show pre-test (solid bars) compared to post-test measures (open bars) in A. Brachial SBP. B. Central SBP. C. Brachial DBP. D. Central DBP. *P<0.05, **P<0.01, ***P<0.001.
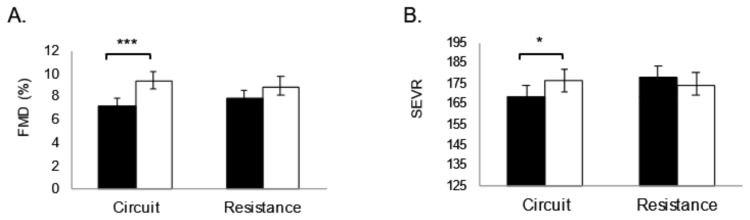
Vascular health data is presented in Figure 2. Vascular health levels were similar at pre- and post-intervention. We found improvements in FMD and SEVR with tactical CT but not with RT. Percent FMD increased by 28.7% (95% CI [1.06, 3.18], p = 0.012) with tactical CT compared to 12.6% with RT (P = 0.07). SEVR increased by 4.4% (95% CI [1.47, 4.22], p = 0.041) with CT but decreased with RT by 2.2% (P = 0.09). We found no changes in IMT or Aix@75 in either group.
Figure 2.
Vascular health changes (mean ± SD) with exercise training comparisons between 4 weeks of tactical circuit training and 4 weeks of resistance training. Bars show pre-test (solid bars) compared to post-test measures (open bars) in A. FMD, flow mediated dilation percentage. B. SEVR, subendocardial viability ratio. *P<0.05, **P<0.01, ***P<0.001.
Fitness test data are presented in Table 2. We found improvements in fitness, and adherence was above 93% for both cohorts. At pre- and post-testing, the firefighters in the tactical CT cohort performed better on plank pose and wall sit endurance tests. Overall, both cohorts improved in number of steps climbed (CT Δ 14.1%: 95% CI [29.16, 56.53], p = 0.001; RT Δ 7.9%: 95% CI [7.52, 37.30], p = 0.01). Tactical CT led to improvement (Δ 90.7%, 95% CI [15.09, 124.69], p = 0.012) in balance and aerobic capacity (Δ 4.6%: 95% CI [0.83, 2.31], p = 0.000). Both interventions improved strength in firefighters. Tactical CT led to a 17.4% improvement in functional strength (95% CI [199.61, 555.69], p = 0.000) and RT led to a 10.3% improvement in upper body strength (95% CI [27.49, 66.86], p = 0.000) and a 11.6% improvement in lower body strength (95% CI [5.51, 14.42], p = 0.000).
Table 2.
Fitness measurements at pre- and post-exercise training.
| Variable | Circuit Training (n = 20) | Resistance Training (n = 17) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Pre | Post | % Change | Pre | Post | % Change | |
| Adherence to program (%) | 97.1 (1.2) | - | - | 93.9 (1.9) | - | - |
| VO2peak (mg·kg−1·min−1) | 34.6 (4.1) | 36.2 (4.6)* | 4.6 | 35.3 (9.8) | 37.3 (8.1) | 5.6 |
| Balance (s) | 155.6 (26.6) | 296.6 (32.4)* | 90.7 | 108.1 (28.9) | 134.4 (26.9)** | 23.8 |
| Plank pose (s) | 110.8 (46.8) | 149.5 (59.9) | 35.3 | 70.1 (33.9)** | 96.1 (40.7)*,** | 37.9 |
| Wall sit (s) | 99.6 (66.8) | 125.4 (55.5) | 25.9 | 55.7 (32.2)** | 71.2 (41.2)*,** | 29.3 |
| Stair Climb (#) | 304.9 (40.7) | 347.8 (41.1)* | 14.1 | 281.4 (59.1) | 303.8 (62.3)*,** | 7.9 |
| 12-step sprint (s) | 2.8 (0.4) | 2.7 (0.3) | −3.7 | 2.9 (0.5) | 2.6 (0.4)* | −11.5 |
| Dummy drag (m) | 54.8 (4.8) | 64.5 (4.6)* | 17.4 | - | - | - |
| 1RM Bench Press (kg) | - | - | - | 69.9 (13.3) | 78.9 (13.9) | 12.8 |
| RM/BM Bench Press | - | - | - | 0.77 (0.1) | 0.88 (0.1)* | 14.2 |
| 1RM Leg Press (kg) | - | - | - | 195.1 (61.1) | 216.5 (63.1) | 10.9 |
| RM/BM Leg Press | - | - | - | 2.15 (0.2) | 2.4 (0.2)* | 11.6 |
Mean (± SD). VO2peak, maximal volume of oxygen consumption; Balance, sum of right and left leg balance; 1RM, 1 repetition maximum; RM/BM, 1RM/body mass.
p < 0.05 before and after training,
p < 0.05 between exercise training groups.
DISCUSSION
We compared changes in selected CVD risk and vascular health markers between 4-weeks of tactical CT and RT in firefighters. The data we report are comparable to studies 3–6 times longer (24, 31, 2). The main findings are that 4-weeks of tactical CT elicited improvements in some vascular health markers, which supported our hypothesis.
It is well known that exercise training reduces BP, but data is lacking in firefighters, in fact BP does not seem to be a main outcome in firefighter-focused studies. Clinical guidelines suggest BP levels of <120 mm Hg systolic and <80 mm Hg diastolic as a therapeutic goal (41). In 4-weeks we found reductions in all BP measures with tactical CT, but no improvements with RT. This is consistent with prior studies (7). Emergency service providers and military-like occupations have emotionally and physically demanding jobs placing them at risk of developing hypertension, so BP research is critical (22). In civilians, four months of functional CT improves BP and lipid levels in hypertensive men, (36) while two months of RT has no effect on BP (38). Exercise interventions have variations in the type of exercise, number of repetitions, and intensity of the effort. These variations may contribute to the inconsistencies observed in the BP changes seen in the exercise training literature base. Yet, hypertension in firefighters and in military populations remains an issue, is many times undocumented or undiagnosed. This study helps to show the beneficial effects that CT exercise, which mimics fireground work, can have on BP levels. We show here that tactical CT may have larger effect on BP.
Central BP has recently gained attention and been suggested to be a better predictor of CVD-related outcomes compared with brachial BP (33). We report that central BP decreased more with tactical CT than with RT. This is similar to other studies that report short-term exercise lowers central BP in adults (19). It can be hypothesized that the decrease in central BP with tactical training is due to enhanced vascular function, as evidenced by improvements we saw in endothelial function (FMD) and myocardial oxygenation (SEVR).
It is established that changes in vascular function or arterial stiffness may be due to type of training program, but results in the literature differ based on type and dose of exercise. Comparison between CT and RT has not been done in firefighters, so these findings are novel. Vascular health has been found to improve with different types of exercise training. We previously reported that 24 weeks of aerobic exercise training improved vascular health in hypertensive civilians (15). Beck et al. reported improved FMD and BP in hypertensive adults with a 2-month intervention (3). Yet there is no study that reports exercise-induced changes in vascular health in a group of firefighters. The FATE (Firefighters and Their Endothelium) study measured vascular function by FMD and IMT and found a direct relationship between BP and CV events but did not examine physical activity (1). Fahs et al. examined the effects of body weight on vascular function and BP. They found that obesity was related to greater vascular stiffness and higher BP, but they did not examine exercise-related changes (12). Separately, Fahs et al. found that 3-hours of live-fire training led to an acute response in vascular stiffness and BP, but it was not an exercise intervention (18). Finally, the data reporting SEVR levels in firefighters is also limited. SEVR reflects the balance between arterial load and coronary perfusion, and it provides a measure of the supply and demand. A drop in SEVR suggests lower energy reserve from reduced myocardial oxygenation levels, but a direct causation has yet to be established. In 2011, Horn et al. examined vascular responses to acute firefighting and found a significant time and condition interaction for SEVR. They reported a drop in SEVR immediately following acute firefighting which recovered over time (21). The strenuous activity of firefighting, combined with lower fitness tolerance in firefighters, contributes to an increased cardiac risk. Therefore, understanding what types of interventions or what types of occupational work can improve SEVR levels could reduce the potential for cardiac events. We found increased SEVR levels after the tactical CT program with no changes in SEVR after RT. More studies are needed that examine SEVR in the firefighting and military populations. Generally, we are the first to report significant improvements in firefighters in BP and indices of vascular health with an exercise intervention.
This study has several limitations. First, the exercise program is self-report. The NFPA has a set of published standards and codes that are designed to provide guidance, and NFPA 1583 outlines a need for fitness and wellness programming in the firehouse, which would inherently be self-report (28). Therefore, this study could provide valuable evidence for a type of exercise program that firehouses could prescribe to their firefighters. Also, the study is small for an intervention study, so the data is not representative of the entire tactical population. Finally, our study included firefighters from the Philadelphia suburban region, which may not be generalizable to firefighters in rural or urban areas or in other parts of the world.
In conclusion. The exercise-training literature base in firefighters is small. Understanding which type of exercise training reduces CVD risk in firefighters could be a tangible way to reduce the number of CVD-related LODD. Here we report improvements in vascular health in firefighters with both CT and RT, yet we show that CT has larger benefit on BP levels. Furthermore, tactical training may be more appealing to certain populations, and could be a low-cost alternative to an actual on-site gym in rural firehouses.
ACKNOWLEDGEMENTS
The authors thank the firefighters from the Collegeville PA, East Brandywine PA, Limerick PA, Trappe PA, Downingtown PA, and Glenmoore PA Fire Departments for their participation in the study. The authors also thank all the HEART lab research students who helped with data collection. We have no disclosures to report.
REFERENCES
- 1.Anderson TJ, Charbonneau F, Title LM, Buithieu J, Rose MS, Conradson H, Hildebrand K, Fung M, Verman S, Lonn EM. Microvascular function predicts cardiovascular events in primary prevention: long-term results from the Firefighters and Their Endothelium (FATE) study. Circulation. 2011;123(2):163–169. doi: 10.1161/CIRCULATIONAHA.110.953653. [DOI] [PubMed] [Google Scholar]
- 2.Beach TA, Frost DM, McGill SM, Callaghan JP. Physical fitness improvements and occupational low-back loading - an exercise intervention study with firefighters. Ergonomics. 2014;57(5):744–763. doi: 10.1080/00140139.2014.897374. [DOI] [PubMed] [Google Scholar]
- 3.Beck DT, Casey DP, Martin JS, Emerson BD, Braith RW. Exercise training improves endothelial function in young prehypertensives. Exp Biol Med (Maywood) 2013;238:433–441. doi: 10.1177/1535370213477600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boos CJ, DeVilliers N, Dyball D, McConnell A, Bennett AN. The relationship between military combat and cardiovascular risk: a systematc review and meta-analysis. Int J Vasc Med. 2019;14:2019. doi: 10.1155/2019/9849465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bustamante-Sanchez A, Tornero-Aguilera JF, Fernandez-Elias VE, Hormeno-Holgado AJ, Dalamitros AA, Clemente-Suarez VJ. Effect of stress on automonic and cardiovascular systems in military population: as systematic review. Card Res Prac. 2020;9:2020. doi: 10.1155/2020/7986249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clemons J, Harrison ML. Validity and reliability of a new stair sprinting test of explosive power. J Strength Cond Res. 2008;22:1578–1583. doi: 10.1519/JSC.0b013e31817ae91d. [DOI] [PubMed] [Google Scholar]
- 7.Collier SR, Kanaley JA, Carhart R, Frechette V, Tobin MM, Hall AK, Luckenbaugh AN, Fernhall B. Effect of 4 weeks of aerobic or resistance exercise training on arterial stiffness, blood flow and blood pressure in pre- and stage-1 hypertensives. J Hum Hypertens. 2008;22:678–686. doi: 10.1038/jhh.2008.36. [DOI] [PubMed] [Google Scholar]
- 8.Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R International Brachial Artery Reactivity Task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–265. doi: 10.1016/s0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- 9.Crilly M, Coch C, Bruce M, Clark H, Williams D. Indices of cardiovascular function derived from peripheral pulse wave analysis using radial applanation tonometry: a measurement repeatability study. Vasc Med. 2007;12:189–197. doi: 10.1177/1358863X07081134. [DOI] [PubMed] [Google Scholar]
- 10.Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel RG. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 11.Durand G, Tsismenakis AJ, Jahnke SA, Baur DM, Christophi CA, Kales SN. Firefighters’ physical activity: relation to fitness and cardiovascular disease risk. Med Sci Sports Exerc. 2011;43:1752–1759. doi: 10.1249/MSS.0b013e318215cf25. [DOI] [PubMed] [Google Scholar]
- 12.Fahs CA, Smith DL, Horn GP, Agiovlasitis S, Rossow LM, Echols G, Heffernan KS, Fernhall B. Impact of excess body weight on arterial structure, function, and blood pressure in firefighters. Am J Cardiol. 2009;104:1441–1445. doi: 10.1016/j.amjcard.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Fahs CA, Yan H, Ranadive S, Rossow LM, Agiovlasitis S, Echols G, Smith D, Horn GP, Rowland T, Lane A, Fernhall B. Acute effects of firefighting on arterial stiffness and blood flow. Vasc Med. 2011;16:113–118. doi: 10.1177/1358863X11404940. [DOI] [PubMed] [Google Scholar]
- 14.Feairheller DL, Aichele KR, Oakman JE, Neal MP, Cromwell CM, Lenzo JM, Perez AN, Bye NL, Santaniello EL, Hill JA, Evans RC, Thiele KA, Chavis LN, Getty AK, Wisdo TR, McClelland JM, Sturgeon K, Chlad P. Vascular health in American football players: cardiovascular risk increased in Division III players. Int J Vasc Med. 2016;2016 doi: 10.1155/2016/6851256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feairheller DL, Diaz KM, Kashem MA, Thakkar SR, Veerabhadrappa P, Sturgeon KM, Ling C, Williamson ST, Kretzschmar J, Lee H, Grimm H, Babbitt DM, Vin C, Fan X, Crabbe DL, Brown MD. Effects of moderate aerobic exercise training on vascular health and blood pressure in African Americans. J Clin Hypertens (Greenwich) 2014;16:504–510. doi: 10.1111/jch.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foster C, Jackson AS, Pollock ML, Taylor MM, Hare J, Sennett SM, Rod JL, Sarwar M, Schmidt DH. Generalized equations for predicting functional capacity from treadmill performance. Am Heart J. 1984;107:1229–1234. doi: 10.1016/0002-8703(84)90282-5. [DOI] [PubMed] [Google Scholar]
- 17.Geibe JR, Holder J, Peeples L, Kinney AM, Burress JW, Kales SN. Predictors of on-duty coronary events in male firefighters in the United States. Am J Cardiol. 2008;101:585–589. doi: 10.1016/j.amjcard.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 18.Getty AK, Wisdo TR, Chavis LN, Derella CC, McLaughlin KC, Perez AN, DiCiurcio WT, Corbin M, Feairheller DL. Effects of circuit exercise training on vascular health and blood pressure. Prev Med Rep. 2018;10:106–112. doi: 10.1016/j.pmedr.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heffernan KS, Fahs CA, Iwamoto GA, Jae SY, Wilund KR, Woods JA, Fernhall B. Resistance exercise training reduces central blood pressure and improves microvascular function in African American and white men. Atherosclerosis. 2009;207:220–226. doi: 10.1016/j.atherosclerosis.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 20.Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences US military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Horn GP, Gutzmer S, Fahs CA, Petruzzello SJ, Goldstein E, Fahey GC, Fernhall B, Smith DL. Physiological recovery from firefighting activities in rehabilitation and beyond. Prehospital Emergency Care. 2011;15:214–225. doi: 10.3109/10903127.2010.545474. [DOI] [PubMed] [Google Scholar]
- 22.Kaikkonen P, Lindholm H, Lusa S. Physiological Load and Psychological Stress During a 24-hour Work Shift Among Finnish Firefighters. J Occup Environ Med. 2017;59:41–46. doi: 10.1097/JOM.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 23.Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens. 2009;22:11–20. doi: 10.1038/ajh.2008.296. [DOI] [PubMed] [Google Scholar]
- 24.Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 25.Marciniak RA, Ebersole KT, Cornell DJ. Relationships between balance and physical fitness variables in firefighter recruits. Work. :2021. doi: 10.3233/WOR-203401. [DOI] [PubMed] [Google Scholar]
- 26.McGraw LK, Turner BS, Stotts NA, Dracup KA. A review of cardiovascular risk factors in US military personnel. J Cardiov Nurs. 2008;23(4):338–344. doi: 10.1097/01.JCN.0000317437.75081.e7. [DOI] [PubMed] [Google Scholar]
- 27.Morris CE, Arnett SW, Winchester LJ. Comparing Physical Fitness in Career vs. Volunteer Firefighters. J Strength Cond Res. :2020. doi: 10.1519/JSC.0000000000003650. [DOI] [PubMed] [Google Scholar]
- 28.National Fire Protection Association. NFPA 1583 Standard on Health-Related Fitness Programs for Firefighters. Quincy, MA: 2008. [Google Scholar]
- 29.Navalta JW, Stone WJ, Lyons TS. Ethical Issues Relating to Scientific Discovery in Exercise Science. Int J Exerc Sci. 2019;12(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 30.Nurnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schäfers RF. Augmentation index is associated with cardiovascular risk. J Hypertens. 2002;20:2407–2414. doi: 10.1097/00004872-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 31.Poston WS, Haddock CK, Jahnke SA, Jitnarin N, Tuley BC, Kales SN. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med. 2011;53:266–273. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts MA, O’Dea J, Boyce A, Mannix ET. Fitness levels of firefighter recruits before and after a supervised exercise training program. J Strength Cond Res. 2002;16:271–277. [PubMed] [Google Scholar]
- 33.Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension. 2007;50:197–203. doi: 10.1161/HYPERTENSIONAHA.107.089078. [DOI] [PubMed] [Google Scholar]
- 34.Roman MJ, Naqvi TZ, Gardin JM, Gerhard-Herman M, Jaff M, Mohler E American Society of Echocardiography, Society for Vascular Medicine and Biology. Clinical application of noninvasive vascular ultrasound in cardiovascular risk stratification: a report from the American Society of Echocardiography and the Society of Vascular Medicine and Biology. J Am Soc Echocardiogr. 2006;19:943–954. doi: 10.1016/j.echo.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 35.Sheaff AK, Bennett A, Hanson ED, Kim YS, Hsu J, Shim JK, Edwards ST, Hurley BF. Physiological determinants of the candidate physical ability test in firefighters. J Strength Cond Res. 2010;24:3112–3122. doi: 10.1519/JSC.0b013e3181f0a8d5. [DOI] [PubMed] [Google Scholar]
- 36.Shim KS, Kim JW. The effect of resistance exercise on fitness, blood pressure, and blood lipid of hypertensive middle-aged men. J Exerc Rehabil. 2017;13:95–100. doi: 10.12965/jer.1734894.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shrestha A, Ho TE, Vie LL, Labarthe DR, Scheier LM, Lester PB, Seligman M. Comparison of cardiovascular health between US Army and Civilians. J Am Heart Assoc. 2019;8(12):e009056. doi: 10.1161/JAHA.118.009056. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.South MA, Layne AS, Stuart CACA, Triplett NT, Ramsey M, Howell ME, Sands WA, Mizuguchi S, Hornsby WG, Kavanaugh AA, Stone MH. Effects of Short-Term Free-Weight and Semiblock Periodization Resistance Training on Metabolic Syndrome. J Strength Cond Res. 2016;30:2682–2696. doi: 10.1519/JSC.0000000000001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsiachris D, Tsioufis C, Syrseloudis D, Roussos D, Tatsis I, Dimitriadis K, Toutouzas K, Tsiamis E, Stefanadis C. Subendocardial viability ratio as an index of impaired coronary flow reserve in hypertensives without significant coronary artery stenoses. J Hum Hypertens. 2012;26:64–70. doi: 10.1038/jhh.2010.127. [DOI] [PubMed] [Google Scholar]
- 40.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang N-Y, Tsao CW On behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 41.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017 ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]