Abstract
Invasive Aspergillosis of the paranasal sinus is an aggressive illness, particularly affecting the immunocompromised and rarely, the immunocompetent. COVID-19 has been shown to cause a derangement of immune parameters both during active infection and the convalescent period. A retrospective study was done from June 10th 2021 to September 10th 2021 on patients who underwent endoscopic debridement of the involved sinuses for post COVID fungal rhinosinusitis. This study included the patients who had Aspergillus infection from the isolated nasal tissue samples. Patient’s information, complaints, history of COVID infection, clinical findings, investigations and treatment details were obtained from the records. 13 patients with post-COVID Invasive Fungal Sinusitis were identified. Symptom onset usually occurred within 1 month of COVID 19 diagnosis in all the patients. Nasal obstruction (84%) and headache (61%) were the most common symptoms. Computerized tomography imaging showed maxillary sinus involvement in all patients followed by ethmoid sinus in 76% of patients. Microbiological diagnosis and histopathological confirmation of Aspergillus species was done. All 13 patients underwent endoscopic debridement of the involved sinuses followed by anti-fungal therapy with Posaconazole. All responded well to the treatment with no recurrence till date. Admist an infinite number of Mucormycosis cases in this era of COVID-19 pandemic, we experienced a surge of Aspergillus infection during this second wave. Presentation at a young age, with no known co-morbidities, with minimal symptoms and history of COVID-19 infection are some of the important aspects to be considered in this series. A better morbidity outcome is expected when early detection and treatment is made in patients with post Covid-19 viral illness with Aspergillosis of nose and paranasal sinus.
Keywords: Aspergillus, COVID 19, Fungal rhinosinusitis, Posaconazole
Introduction
Fungi are ubiquitous organisms. They are widely distributed in air, water, soil and decaying matter. Spores are the reproductive cells of fungi which are airborne, hence gain easy access to enter human airway. As per the literature, the most common fungal species reported in the nose and paranasal sinuses are Mucor and Aspergillus species [1]. Disease presentation by fungi mostly depends on the host immune status rather than the fungus itself [2, 3]. Fungi cause a spectrum of sinonasal disorders ranging from Allergic fungal rhinosinusitis (AFRS) in the atopic patient to “fungal balls'' in the immunocompetent host and finally Invasive fungal rhinosinusitis in the immunocompromised patient. Studies compared the predilection of certain fungi for causing cranial nerve and orbital complications, i.e., Mucor vs Aspergillus, finding greater prevalence with the former [4]. Invasive fungal rhinosinusitis has gained a resurgence during the current COVID-19 pandemic. This may be attributed to immunosuppression resulting from decreased CD4+ and CD8+ T-cells caused by SARS COV 2 virus [5].
Fungal infections were one of the leading causes of death in patients with SARS in earlier studies dated in 2003–2007. Injury to the lung, persistent hypoxemia, hyperglycemia, overuse of corticosteroids leads to secondary infections [6, 7]. A similar presentation seems to be happening in the present pandemic. This SARS COV virus type could be a predisposing factor for Invasive fungal Aspergillosis infection also in parallel to other fungal infections. Hence a high suspicion of fungal infection to be made in patients presenting with minimal complaints for an early detection and intervention to prevent the spread of infection. Recent literature shows an infinite number of Mucormycosis cases in this era of COVID-19 pandemic with a wide range of recovery and deaths [8, 9]. In this case series, we put an effort to emphasize on the surge of Aspergillus infections in the patients recovered from COVID 19 infection during this second wave who presented with mild symptoms.
Materials and Methods
A retrospective study was done from June 10th 2021 to September 10th 2021on patients who underwent endoscopic debridement of the involved sinuses for Post COVID fungal rhinosinusitis. This study included the patients who had Aspergillus infection from the isolated nasal tissue samples. Patient’s demographic details, chief complaints, history of COVID infection, clinical findings, relevant investigations and treatment details were noted from the hospital records after taking institutional ethical clearance. Informed consents from the study population were taken.
A detailed history of COVID infection was collected from these patients—date of definitive diagnosis of COVID 19 by Polymerase Chain Reaction, symptoms during the infection, hospitalization and treatment history. Radioimaging—Computerized Tomography/ Magnetic Resonance Imaging were done according to the patient’s presentation and clinical findings. Details of the nasal swabs and tissue which were subjected to microbiological examination by KOH staining and histopathological examination were obtained. Hemotoxylin and Eosin (H& E), Gomori’s methamine silver staining, Periodic Acid-Schiff stating were used for histopathological diagnosis to differentiate the fungal species. Details of surgical and medical management of these patients were obtained from the hospital records.
Results
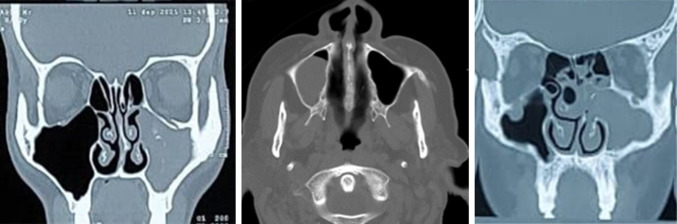
A total of 13 patients met the criteria of this study. Among which 9 were male and 4 were females with a male preponderance of 2.25:1. Patients were in a wide range of age group with youngest age of 27 years to oldest age of 75 years. As per the clinical history, symptom onset occurred within 1 month of COVID 19 diagnosis in all the patients. The most common presenting complaints were nasal obstruction (84%) followed by headache (61%) and facial pain (46%) (Fig. 1). Co-morbidities were found in 8 out of 13 patients (61%). Details as mentioned in Table 1.
Fig. 1.
Showing presenting complaints of the patients
Table 1.
Showing the Co-morbidities and COVID-19 history details of the patients
| S. no | Age | Comorbidities | Date of COVID-19 RTPCR positive | Hospitalization | Received steroids during COVID 19 | Date of symptom onset | Duration between COVID19 infection AND symptom onset (days) |
|---|---|---|---|---|---|---|---|
| 1 | 27 | – | 12/6/2021 | No | No | 30/6/2021 | 18 |
| 2 | 36 | – | 22/6/2021 | No | No | 18/7/2021 | 26 |
| 3 | 56 | DM | 25/6/2021 | Yes | Yes | 17/7/2021 | 23 |
| 4 | 75 | DM, CKD, HTN | 3/7/2021 | Yes | Yes | 25/7/2021 | 22 |
| 5 | 64 | DM, HTN | 10/7/2021 | Yes | Yes | 30/7/2021 | 20 |
| 6 | 32 | – | 20/7/2021 | No | No | 14/8/2021 | 24 |
| 7 | 71 | DM, HTN, ASTHMA | 22/7/2021 | Yes | Yes | 15/8/2021 | 23 |
| 8 | 68 | DM | 26/7/2021 | Yes | Yes | 12/8/2021 | 17 |
| 9 | 35 | DM | 30/7/2021 | Yes | Yes | 18/8/2021 | 19 |
| 10 | 34 | – | 2/8/2021 | No | No | 22/8/2021 | 20 |
| 11 | 50 | DM, HTN | 4/8/2021 | Yes | Yes | 22/8/2021 | 18 |
| 12 | 54 | DM | 16/8/2021 | Yes | Yes | 1/9/2021 | 15 |
| 13 | 29 | – | 20/8/2021 | No | No | 8/9/2021 | 18 |
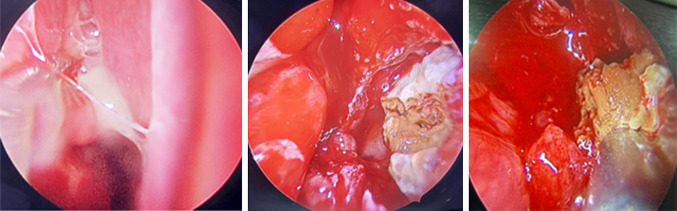
As most of the patient’s chief complaints were limited to the nose and paranasal sinus, initially computerized tomography (CT) of Paranasal sinus (PNS) was done, followed by MRI if required. CT imaging showed opacification of the sinuses along with hyperdense elements in the involved sinuses (Fig. 2). As per CT PNS (Table 2), the most common sinus involved was maxillary sinus in all the patients followed by ethmoid sinus (76%) 0.54% of the patient’s had unilateral presentation while 46% of the patients had bilateral presentation. There was no involvement of brain, orbit, palate in any of our cases.
Fig. 2.
CT scan images showing opacification of sinuses and hyperdense elements
Table 2.
Structures involved on CT imaging
| Sites involved | No. of patients |
|---|---|
| Maxillary sinus | 13 (100%) |
| Ethmoid sinus | 10 (76%) |
| Sphenoid sinus | 3 (23%) |
| Frontal sinus | 1 (7%) |
| Septum | 0 |
| Skull base | 0 |
| Unilateral presentation | 7 (54%) |
| Bilateral presentation | 6 (46%) |
| Orbital involvement | 0 |
| Cranial involvement | 0 |
| Palatal involvement | 0 |
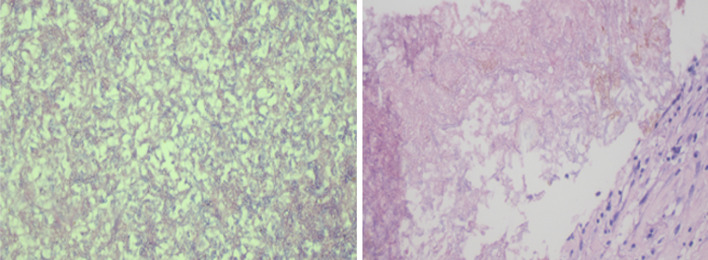
All these patients underwent endoscopic debridement of the involved sinuses—endoscopic middle meatal antrostomy, anterior and posterior ethmoidectomy, sphenoidotomy as per the involved sinuses as the initial management. Pus and the tissue from the sinuses involved were sent for KOH staining and histopathological examination. However, the extent of involvement was minimal limiting to one or two sinuses in most of the cases. There was no involvement of orbit, palate or brain in our reported cases. The entire diseased tissue and unhealthy mucosa was debrided (Fig. 3) None of the patients had any complications during the surgery.
Fig. 3.
Intra-operative images showing thick, yellowish inspissated material within the sinus
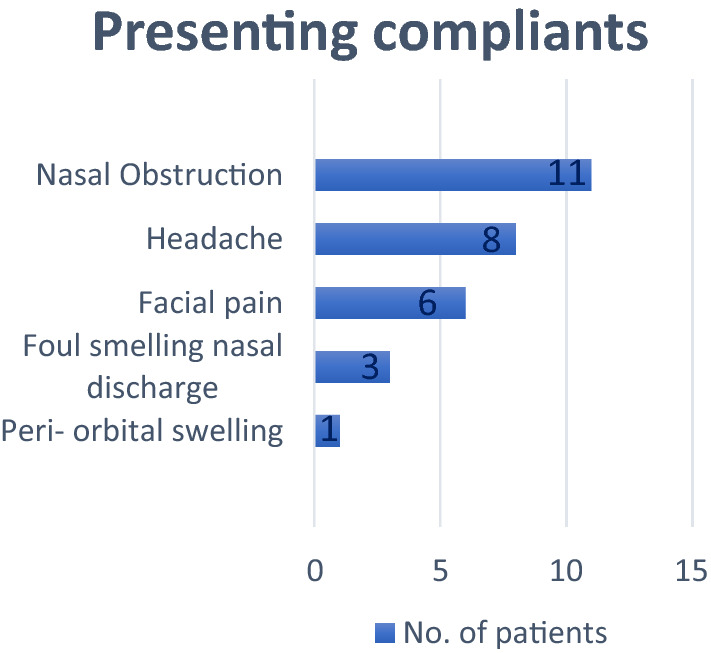
KOH staining from the nasal discharge demonstrated fungal elements in 4 out of 13 patients, whereas KOH staining of the tissue from the involved sinuses demonstrated septate hyphae with dichotomous branching in all the 13 patients. This diagnosis was further confirmed by histopathological examination of the tissue which showed fungal elements with acute branching narrow septate hyphae resembling Aspergillus flavus which indicates invasive fungal infection (Fig. 4).
Fig. 4.
Histopathological examination showing Aspergillus flavus organism
Post-surgery, all the patients received tablet Posaconazole a loading dose of 600 mg and a maintenance dose of 300 mg for a period of one month along with saline nasal douching. Regular follow-up was done once every week during which diagnostic nasal endoscopy was done to look for any new changes in the mucosa and to ensure eradication of the disease. Liver function tests were monitored during the entire course of Posaconazole treatment. All the patients recovered well without any recurrence or complications till date.
Discussion
Patients with an immunocompromised state which can be related to uncontrolled Diabetes mellitus, hematological malignancies, post renal or bone marrow transplant patients, acquired immunodeficiency syndrome, immunosuppressant or receiving chemotherapy for underlying malignancies, may it be any above mentioned state are the most susceptible individuals for secondary bacterial or fungal infections [4, 8–11]. COVID-19 infection is now added to this list in causing severe immune suppression which can be attributed to reduced CD8+ T cells and CD4+ T cells [9–11]. COVID-19 infection in an individual with underlying co-morbidities paved a path for development of fungal infection. Of late, post COVID patients without any underlying comorbidities have also become prey for fungal infections. This was one of the findings to be highlighted in our study as 46% of the patients were young and did not have any associated comorbidities, yet diagnosed to have invasive fungal infection.
Mucor and Aspergillus are the most commonly reported fungal infections in immunocompromised patients. Till date, many case series and case reports are published on rhino-orbito-cerebral mucormycosis and few isolated case reports on aspergillus [1, 4, 8–11]. A number of case reports are published on covid-19 associated pulmonary aspergillus [12, 13]. In a study by Koehler P et al., which shows invasive pulmonary Aspergillosis in 5 out of 19 COVID 19 associated patients highlights the importance of subjecting respiratory samples to detect fungal infections [12]. Another study by Van Arkel et al., also proved presence of aspergillus infection in COVID-19 affected ICU patients [13]. This case series focusses on reporting aspergillus infection in nose and paranasal sinuses in post COVID-19 individuals.
In our series, most of the patients presented with mild symptoms of nasal obstruction, headache, facial pain and the symptom onset was within 1 month of post COVID illness. These coincides with the study done by Sebastian et al., in which patients developed symptoms and signs of fungal rhinosinusitis 10–15 days after the onset of COVID-19 infection [11]. This period would mostly represent the phase of sepsis induced immunosuppression.
As per the study on Invasive Fungal Sinusitis in Post COVID-19, patients by Noha Ahmed et al., all the 36 patients had sino-nasal involvement, 80.6% had orbital, 27.8% had cerebral and 33.3% of the patients had palatine involvement. Among 32 patients 77.8% were diagnosed to have Mucor species and 30.6% of the patients had Aspergillus species [10]. In our series on aspergillus infection, all the 13 patients had sino-nasal involvement, but none of our patients had orbital, cerebral or palatine involvement.
Tissue from the sinuses during the surgery showed presence of aspergillus species. Hence, this highlights the importance of suspicion of fungal infections in patients with history of COVID-19 infection. Among the various sub-types of fungal sinusitis, Acute invasive fungal rhino-sinusitis (AIFR) is the most belligerent subtype [1, 11]. An early detection definitely helps in preventing the spread of infection to the vital structures. Hence, early detection with an active intervention helps in improving mortality and morbidity of the patient.
Surgical intervention along with administration of antifungal agents remains as the main stay of treatment in these patients [9–11]. As per the literature till date all the patients detected with fungal rhinosinusitis initially underwent minimal to extensive endoscopic sinus surgery as per the presentation, clinical and radiological findings [1, 9–11]. Surgery aims in clearance of the disease and thus helps in providing better access for the penetration of anti-fungal medications. Control of underlying medical condition plays an important role in better recovery of the patient. Choice of antifungal medications is tailor made to every patient. Most commonly administered anti-fungal agents includes Amphotericin, Voriconazole, Posaconazole [1, 9–11]. In this case series, patients received Posaconazole which is a triazole antifungal medication. It acts by disrupting the close packing of acyl chains of phospholipids further impairing the function of certain enzymes which ultimately lead to inhibition of growth of fungi. It is available in injectable, delayed release tablet and oral suspension forms. Tablet form is known to have threefold increased efficacy compared to oral suspension [14]. All our patients received Tablet Posaconazole 600 mg as a loading dose on Day 1 followed by 300 mg once a day for a period of 30 days. Patients were on regular follow ups with diagnostic nasal endoscopy and monitored liver function tests. All the patients responded well to treatment with no recurrence till date. Survival rates of post COVID-19 fungal rhinosinusitis can be improved by early diagnosis when patient is in the recovery phase of COVID-19 infection.
Conclusion
Admist an infinite number of Mucormycosis cases in this era of COVID-19 pandemic, we experienced a surge of Aspergillus infection during this second wave. Presentation at a young age, with no known co-morbidities, with minimal symptoms and history of COVID-19 infection are some of the important aspects to be considered in this series. This emphasizes on the need for careful evaluation of the patients recovering from COVID-19 and presenting with signs and symptoms of sinusitis to the OPD. A better morbidity outcome is expected with accurate clinical suspicion and early diagnosis of fungal rhinosinusitis. Survival rate can be improved by an immediate surgical intervention and appropriate anti-fungal medications with a contemplate follow-up.
Funding
No external funding has been received.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Appropriate ethical clearance has been obtained from the institute.
Research Involving Human Participants and/or Animals
It was an observational study done on the human participants after obtaining the informed consent from all the individuals.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Monroe M, Sautter N, Smith T, Andersen P, Wax M, Gross N. Acute Invasive fungal rhinosinusitis: a 15-year experience with 29 patients. Laryngoscope. 2011;121(S5):S364–S364. doi: 10.1002/lary.22320. [DOI] [PubMed] [Google Scholar]
- 2.Ziaee A, Zia M, Goli M. Identification of saprophytic and allergenic fungi in indoor and outdoor environments. Environ Monit Assess. 2018;190(10):66. doi: 10.1007/s10661-018-6952-4. [DOI] [PubMed] [Google Scholar]
- 3.Lop-Gros J, Gras-Cabrerizo J, Bothe-González C, Montserrat-Gili J, Sumarroca-Trouboul A, Massegur-Solench H. Fungus ball of the paranasal sinuses: analysis of our series of patients. Acta Otorrinolaringologica. 2016;67(4):220–225. doi: 10.1016/j.otorri.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Ingley A, Parikh S, DelGaudio J. Orbital and cranial nerve presentations and sequelae are hallmarks of invasive fungal sinusitis caused by mucor in contrast to aspergillus. Am J Rhinol. 2008;22(2):155–158. doi: 10.2500/ajr.2008.22.3141. [DOI] [PubMed] [Google Scholar]
- 5.Wang W, Su B, Pang L, Qiao L, Feng Y, Ouyang Y, et al. High-dimensional immune profiling by mass cytometry revealed immunosuppression and dysfunction of immunity in COVID-19 patients. Cell Mol Immunol. 2020;17(6):650–652. doi: 10.1038/s41423-020-0447-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y, Li WX, Huang KW, Cao ZX, Hao JY. Hospital acquired pneumonia occurring after acute stage of the serious SARS and its treating strategies. Chin J Nosocomiol. 2003;11(13):1081–1087. [Google Scholar]
- 7.Li CS, Pan SF. Analysis and causation discussion of 185 severe acute respiratory syndrome dead cases. Zhongguo wei zhong bing ji jiu yi xue Chin Crit Care Med Zhongguo weizhongbing jijiuyixue. 2003;15(10):582–4. [PubMed] [Google Scholar]
- 8.Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabet Metabc Synd Clin Res Rev. 2021;6:66. doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–447. doi: 10.1017/S0022215121000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Kholy NA, Abd El-Fattah AM, Khafagy YW. Invasive fungal sinusitis in post COVID-19 patients: a new clinical entity. The Laryngoscope. 2021;6:66. doi: 10.1002/lary.29632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sebastian SK, Kumar VB, Gupta M, Sharma Y. Covid assossiated invasive fungal sinusitis. Indian J Otolaryngol Head Neck Surg. 2021;25:1–4. doi: 10.1007/s12070-021-02471-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koehler P, Cornely O, Böttiger B, Dusse F, Eichenauer D, Fuchs F, et al. COVID-19 associated pulmonary Aspergillosis. Mycoses. 2020;63(6):528–534. doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Arkel A, Rijpstra T, Belderbos H, van Wijngaarden P, Verweij P, Bentvelsen R. COVID-19–associated pulmonary Aspergillosis. Am J Respir Crit Care Med. 2020;202(1):132–135. doi: 10.1164/rccm.202004-1038LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schauwvlieghe A, Buil J, Verweij P, Hoek R, Cornelissen J, Blijlevens N, et al. High-dose posaconazole for azole-resistant Aspergillosis and other difficult-to-treat mould infections. Mycoses. 2019;63(2):122–130. doi: 10.1111/myc.13028. [DOI] [PMC free article] [PubMed] [Google Scholar]