Abstract
Paraneoplastic neurological syndrome (PNS) is associated with malignancies, including small-cell lung cancer. Recently, PNS cases among patients with small-cell lung cancer (SCLC) induced by immune checkpoint inhibitors have increased. We herein report a 66-year-old man with SCLC who developed disorientation, dysphagia, and gait disturbance after three courses of treatment with atezolizumab. Brain magnetic resonance imaging revealed a high-intensity area in the bilateral temporal lobes. Blood test results were positive for anti-Hu and anti-Zic4 antibodies, which led to the diagnosis of limbic encephalitis as PNS. Some symptoms improved with intravenous administration of steroids and immunoglobulins.
1. Introduction
Paraneoplastic neurological syndrome (PNS) is caused by an autoimmune process that develops in patients with any type of malignancy [1, 2]. Immune checkpoint inhibitors (ICIs) are effective treatment options for patients with malignancies, including small-cell lung cancer (SCLC) [3]. However, ICIs cause inflammatory side effects by increasing the activity of the immune system [4]. Therefore, ICIs are presumed to be a risk factor for PNS [5, 6]. In fact, cases of PNS induced by ICIs have recently increased [7–12].
Herein, we report a case of ICI-induced limbic encephalitis developed in a patient with SCLC. The present report suggests that clinicians should consider the possibility of PNS when patients develop neurological symptoms after ICI initiation.
2. Case Report
A 66-year-old man with a history of smoking for 40 years was referred to our hospital for abnormal chest radiograph findings. The patient had a history of bronchial asthma, with no history of autoimmune diseases. Computed tomography (CT) and positron emission tomography with 18F-fluorodeoxyglucose revealed a tumor mass in the right hilum, hilar and mediastinal lymph node swelling, and multiple lung metastases. Brain magnetic resonance imaging (MRI) showed no abnormal finding (Figure 1). Pathological findings of bronchoscopy of the primary tumor revealed SCLC. Therefore, the patient was diagnosed with extensive disease SCLC (ED-SCLC) and was treated with carboplatin and etoposide, and atezolizumab was initiated as first-line chemotherapy. Treatment led to a complete response.
Figure 1.
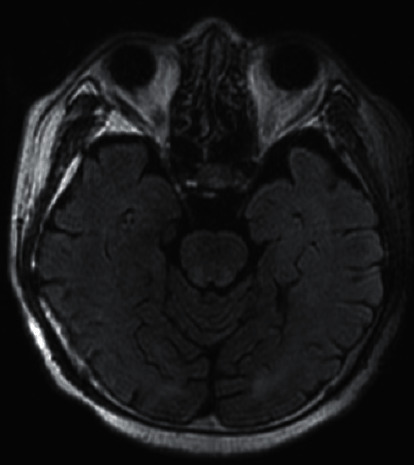
Fluid-attenuated inversion recovery (FLAIR) image of brain magnetic resonance imaging (MRI) before initiation of treatment with immune checkpoint inhibitor reveals no abnormal finding.
The patient developed disorientation after three courses of chemotherapy over 2 months. Although follow-up without any treatment was continued, the disorientation worsened with coma. Dysphagia and gait disturbances due to muscle weakness also developed; however, we could not perform detailed neurological examination owing to the state of his consciousness. Fluid-attenuated inversion recovery (FLAIR) imaging of brain MRI after coma development showed a high-intensity area in the bilateral temporal lobes (Figure 2). Furthermore, anti-Hu and anti-Zic4 antibodies were highly detected in the blood test. The cerebrospinal fluid examination showed no evidence of tumor cells or infection, including herpes simplex virus and varicella-zoster virus (Table 1). Based on these results, anti-Hu and anti-Zic4 antibodies-positive limbic encephalitis as PNS was given as the final diagnosis. As steroid pulse therapy was initiated, the disturbance of consciousness improved. However, dysphagia and gait disturbance showed no improvement. Due to this, intravenous immunoglobulin (IVIG) therapy was also initiated leading to improvement of dysphagia, but not with gait disturbance. Brain MRI findings at 3 months after initiation of steroid treatment also improved slightly (Figure 3), and blood test at that time showed anti-Zic4 antibody negativity with anti-Hu antibody persistence.
Figure 2.
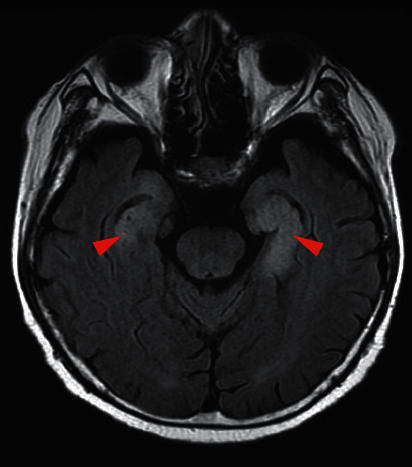
FLAIR image of brain MRI after development of neurological symptoms reveals high-intensity area in bilateral temporal lobes (red arrowheads).
Table 1.
Laboratory findings at the onset of PNS.
| Anti-neuronal antibodies | Cerebrospinal fluid | |||
|---|---|---|---|---|
| Amphiphysin | Negative | Appearance | Clear | |
| CV2 | Negative | Cell count | 5 | /μl |
| PNMA2 | Negative | Poly | 0 | % |
| Ri | Negative | Mono | 100 | % |
| Yo | Negative | Protein | 94 | mg/dl |
| Hu | 3+ | Glucose | 72 | mg/dl |
| Recoverin | Negative | ADA | ≦1 | U/l |
| SOX1 | Negative | HSV-PCR | Negative | |
| Titin | Negative | VZV-PCR | Negative | |
| Zic4 | 3+ | |||
| GAD65 | Negative | Cytology | Class I | |
| Tr | Negative | Culture | Negative |
ADA, adenosine deaminase; HSV, herpes simplex virus; VZV, varicella-zoster virus.
Figure 3.
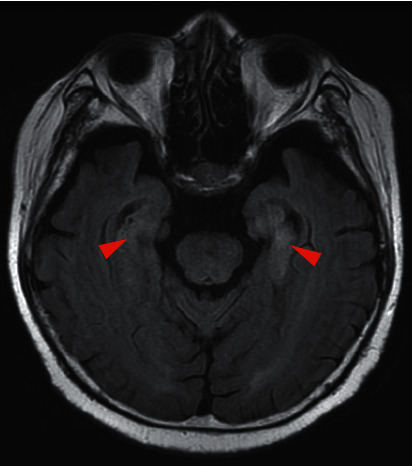
FLAIR image of brain MRI after development of neurological symptoms reveals slight improvement of high-intensity area in bilateral temporal lobes (red arrowheads).
At the time of writing, 6 months have passed since the development of limbic encephalitis, and the neurological symptoms did not worsen. Furthermore, a complete response was observed.
3. Discussion
In the present case, limbic encephalitis as PNS was diagnosed due to the following reasons. (1) Anti-Hu and anti-Zic4 antibodies were detected in the serum at the onset of neurological symptoms. (2) SCLC was presented at the onset of neurological symptoms. (3) SCLC is one of the most strongly associated tumors with PNS [7–12]. (4) MRI revealed a high-intensity area in the bilateral temporal lobes, which was consistent with limbic encephalitis. (5) No other possible cause was found for disorientation, such as central nervous system metastasis, stroke, or metabolic disorders in blood tests and brain MRI. (6) No evidence of meningeal carcinomatosis or infection in the cerebrospinal fluid was found.
Anti-Hu antibody is an auto-antibody associated with limbic encephalitis and sensory neuropathy [13]. Anti-Zic4 antibody is also associated with limbic encephalitis, cerebellar dysfunction, and sensory neuropathy [14]. The MRI findings of the patient were consistent with those of limbic encephalitis. Therefore, the neurological symptoms, disturbance of consciousness, dysphagia, and gait disturbance were considered to be caused by anti-Hu and anti-Zic4 antibodies-positive limbic encephalitis as PNS in the present case. Previous reports also showed several types of neurological symptoms of PNS in SCLC patients treated with ICIs (Table 2). However, a limitation of the present case is the non-examination of the neuronal cell surface antibodies. Neuronal cell surface antibody-mediated autoimmune encephalitis should be considered as a differential diagnosis [15]. A diagnosis of anti-Hu and anti-Zic4 antibodies-positive limbic encephalitis may be more likely, if neuronal cell surface antibodies, such as anti-n-methyl-D-aspartate (NMDA) receptor antibody, are fount to be negative.
Table 2.
Details of cases of PNS induced by ICI in SCLC patients.
| No. | Age | Sex | Country | ICI | Antibody | PNS | PNS symptoms | Time to onset | Treatment for PNS | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 76 | M | Japan | Atezolizumab | CRMP5 | Striatal encephalitis | Forgetfulnes, irritability | 5 months | Methylprednisolone | Improved | [7] |
|
| |||||||||||
| 2 | 70 | M | Japan | Atezolizumab | Hu, SOX1 | Sensory polyneuropathy | Tactile and pain disturbances | 1 month | IVIG | Not improved | [8] |
|
| |||||||||||
| 3 | 66 | F | China | Sintilimab | Hu | Encephalitis | Focal seizures | 1.5 months | Methylprednisolone | Improved | [9] |
|
| |||||||||||
| 4 | 62 | F | USA | Nivolumab | Hu | Sensory polyneuropathy | Numbness in hands and feet, tremor, loss of dexterity, gait ataxia | a few days | Methylprednisolone, IVIG | Not improved | [10] |
|
| |||||||||||
| 5 | 71 | F | Switzerland | Nivolumab + ipilimumab | Hu | Limbic encephalitis | Short-term memory deficits | 4 days | Methylprednisolone, natalizumab | Improved (not completely) | [11] |
|
| |||||||||||
| 6 | 46 | M | France | Pembrolizumab | Hu | Sensory neuropathy | Painful paresthesia, gait disturbance | 3 months | Methylprednisolone, IVIG | Improved (temporary) | [12] |
|
| |||||||||||
| 7 | 71 | M | France | Atezolizumab | Hu | Encephalitis | Dizziness, vomiting, diplopia, gait disturbance | 2 months | IVIG | Improved (not completely) | [12] |
|
| |||||||||||
| Present case | 66 | M | Japan | Atezolizumab | Hu, Zic4 | Limbic encephalitis | Disorientation, dysphagia, gait disturbance | 2 months | Methylprednisolone, IVIG | Improved (not completely) | |
PNS, paraneoplastic neurological syndrome; ICI, immune checkpoint inhibitor; SCLC, small-cell lung cancer.
ICI might have induced the neurological symptoms in the present case, since one of the mechanisms of immune-related adverse events is an increase in pre-existing autoantibodies [2, 12]. The neurological symptoms occurred 2 months after the first initiation of ICI, similar to previous reports (Table 2). Moreover, ICI-activated autoantibodies might be a reason why neurological symptoms were not improved completely. The persistence of neurological symptoms was also similar to previous reports (Table 2). ICI-induced PNS cases may be relatively rare in non-small-cell lung cancer patients, with only a few cases reported previously [16, 17]. Clinicians should consider the possibility of PNS especially when patients with SCLC complain of neurological symptoms after initiation of ICIs, especially after several months.
There is no established treatment for most cases of PNS. However, corticosteroids and other immunosuppressive drugs, such as cyclophosphamide or tacrolimus, IVIG, and plasma exchange, are often used in clinical practice [1]. In the present case, methylprednisolone and IVIG were used to treat PNS, and the disturbance of consciousness and dysphagia improved. However, gait disturbance did not improve. In previous cases, methylprednisolone and IVIG were the most frequently used treatments for PNS, but only a few patients had improved neurological symptoms completely (Table 2). Information about the appropriate treatments for PNS is needed in the future.
There are some limitations of present case. First, the examination of the neuronal cell surface antibodies was not performed. Second, other causes of limbic encephalitis, such as primary autoimmune encephalitis or iatrogenic encephalopathy, could not be ruled out completely.
In conclusion, we described a case of ICI-induced limbic encephalitis as PNS and reviewed the literature on cases of PNS induced by ICI in SCLC patients. Clinicians should consider the possibility of PNS when patients with SCLC develop neurological symptoms after ICI initiation.
Acknowledgments
We would like to thank Editage (https://www.editage.com) for providing English language editing assistance.
Conflicts of Interest
The authors have no conflicts of interest directly relevant to the content of this article to declare.
References
- 1.Darnell R. B., Posner J. B. Paraneoplastic syndromes involving the nervous system. New England Journal of Medicine . 2003;349(16):1543–1554. doi: 10.1056/nejmra023009. [DOI] [PubMed] [Google Scholar]
- 2.Dalmau J., Rosenfeld M. R. Paraneoplastic syndromes of the CNS. The Lancet Neurology . 2008;7(4):327–340. doi: 10.1016/s1474-4422(08)70060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horn L., Mansfield A. S., Szczęsna A., et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. New England Journal of Medicine . 2018;379(23):2220–2229. doi: 10.1056/nejmoa1809064. [DOI] [PubMed] [Google Scholar]
- 4.Postow M. A., Sidlow R., Hellmann M. D. Immune-related adverse events associated with immune checkpoint blockade. New England Journal of Medicine . 2018;378(2):158–168. doi: 10.1056/nejmra1703481. [DOI] [PubMed] [Google Scholar]
- 5.Graus F., Dalmau J. Paraneoplastic neurological syndromes in the era of immune-checkpoint inhibitors. Nature Reviews Clinical Oncology . 2019;16(9):535–548. doi: 10.1038/s41571-019-0194-4. [DOI] [PubMed] [Google Scholar]
- 6.Zekeridou A., Lennon V. A. Neurologic autoimmunity in the era of checkpoint inhibitor cancer immunotherapy. Mayo Clinic Proceedings . 2019;94(9):1865–1878. doi: 10.1016/j.mayocp.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Tatsumi S., Uryu K., Iwasaki S., Harada H. A case of anti-CRMP5 paraneoplastic neurological syndrome induced by atezolizumab for small cell lung cancer. Internal Medicine . 2020 doi: 10.2169/internalmedicine.4889-20. (article in press) [DOI] [PubMed] [Google Scholar]
- 8.Morimoto T., Orihashi T., Yamasaki K., Tahara M., Kato K., Yatera K. Paraneoplastic sensory polyneuropathy related to anti-PD-L1-including anticancer treatment in a patient with lung cancer. Internal Medicine . 2021;60(10):1577–1581. doi: 10.2169/internalmedicine.5629-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang K., Zheng K., Zhang Y. Paraneoplastic encephalitis and enteric neuropathy associated with anti-hu antibody in a patient following immune-checkpoint inhibitor therapy. Journal of Immunotherapy (Hagerstown, Md: 1997) . 2020;43(5):165–168. doi: 10.1097/CJI.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 10.Raibagkar P., Ho D., Gunturu K. S., Srinivasan J. Worsening of anti-Hu paraneoplastic neurological syndrome related to anti-PD-1 treatment: case report and review of literature. Journal of Neuroimmunology . 2020;341 doi: 10.1016/j.jneuroim.2020.577184.577184 [DOI] [PubMed] [Google Scholar]
- 11.Hottinger A. F., De Micheli R., Guido V., Karampera A., Hagmann P., Du Pasquier R. Natalizumab may control immune checkpoint inhibitor-induced limbic encephalitis. Neurology-Neuroimmunology Neuroinflammation . 2018;5(2):p. e439. doi: 10.1212/nxi.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mongay-Ochoa N., Vogrig A., Muñiz-Castrillo S., Honnorat J. Anti-Hu-associated paraneoplastic syndromes triggered by immune-checkpoint inhibitor treatment. Journal of Neurology . 2020;267(7):2154–2156. doi: 10.1007/s00415-020-09940-y. [DOI] [PubMed] [Google Scholar]
- 13.Graus F., Keime-Guibert F., Reñe R., et al. Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain . 2001;124(6):1138–1148. doi: 10.1093/brain/124.6.1138. [DOI] [PubMed] [Google Scholar]
- 14.Bataller L., Wade D. F., Graus F., Stacey H. D., Rosenfeld M. R., Dalmau J. Antibodies to Zic4 in paraneoplastic neurologic disorders and small-cell lung cancer. Neurology . 2004;62(5):778–782. doi: 10.1212/01.wnl.0000113749.77217.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayden Z., Bóné B., Orsi G., et al. Clinical characteristics and outcome of neuronal surface antibody-mediated autoimmune encephalitis patients in a national cohort. Frontiers in Neurology . 202;12 doi: 10.3389/fneur.2021.611597.611597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakatani Y., Tanaka N., Enami T., Minami S., Okazaki T., Komuta K. Lambert-eaton myasthenic syndrome caused by nivolumab in a patient with squamous cell lung cancer. Case Reports in Neurology . 2018;10(3):346–352. doi: 10.1159/000494078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakashima K., Fujii Y., Sato M., Igarashi K., Kobayashi M., Ishizuka T. A case of non-small cell lung cancer presenting anti-amphiphysin antibody-positive paraneoplastic neurological syndrome. Respiratory Medicine Case Reports . 2021;34 doi: 10.1016/j.rmcr.2021.101525.101525 [DOI] [PMC free article] [PubMed] [Google Scholar]


