Abstract
Traumatic ventricular septal perforation (VSP) is a rare condition that can occur following chest trauma and can lead to heart failure. Herein, a case of VSP caused by blunt chest trauma successfully closed using the double-patch technique via the right ventricle after medial sternotomy is presented. This case report highlights the necessity of emergency surgery in the acute phase of traumatic VSP if heart failure is difficult to control. This technique was useful for acute surgery.
<Learning objective: Traumatic ventricular septal perforation (VSP) can occur following chest trauma. The timing of surgery depends on the severity of heart failure and the urgency of other traumas. Since the left ventricular pressure is higher than the right ventricular pressure, complete hemostasis of the left ventricle is difficult. Hence, traumatic VSP might be successfully approached and closed via the right ventricle. Here we report a successful closure of traumatic VSP after blunt chest trauma using the right ventricular approach through medial sternotomy.>
Keywords: Traumatic ventricular septal perforation, Right ventricle approach, Blunt trauma, Double-patch
Introduction
Traumatic ventricular septal perforation (VSP) can occur following chest trauma; some patients, however, may not develop symptoms such as heart failure immediately after injury. In other words, time to the onset of heart failure varies among different traumatic VSP patients. Moreover, there is no consensus on the ideal time of surgery once traumatic VSP is diagnosed. The treatment strategy can be further complicated when damage to and fracture of other organs necessitate additional surgical interventions.
Here, we report a case of traumatic VSP caused by blunt chest trauma successfully closed via a right ventricular approach after medial sternotomy. Our report highlights that traumatic VSP should be managed with an optimal surgical strategy according to the patient's hemodynamics.
Case report
A 72-year-old man presented to our hospital with an open right tibial fracture, a rib fracture, a crush injury to the left upper arm, both facial and airway burns, and myocardial contusion following blunt chest trauma. The patient reported sudden explosion of a drum of volatile liquid just 2 m away from him while burning wood. He had no relevant past medical or family history. Physical examination revealed a bruise on the left chest and a Levine III/VI systolic murmur over the cardiac apex.
Laboratory results on admission were as follows: white blood cell, 20,020/μL; red blood cell, 476 × 104/μL; hemoglobin, 15 g/dL; hematocrit, 44.2%; platelet, 14.4 × 104/μL; glucose, 185 mg/dL; gamma-glutamyltransferase, 136 U/L; aspartate aminotransferase, 37 U/L; alkaline phosphatase, 53 U/L; creatinine, 0.55 mg/dL; estimated glomerular filtration rate, 109.3 mL/min/1.73 m2; C-reactive protein, 0.38 mg/dL; creatine kinase (CK), 481 U/L; CK isoenzyme MB (CK-MB), 58 U/L; sodium, 137 mEq/L; potassium, 4.0 mEq/L; and chlorine, 104 mEq/L.
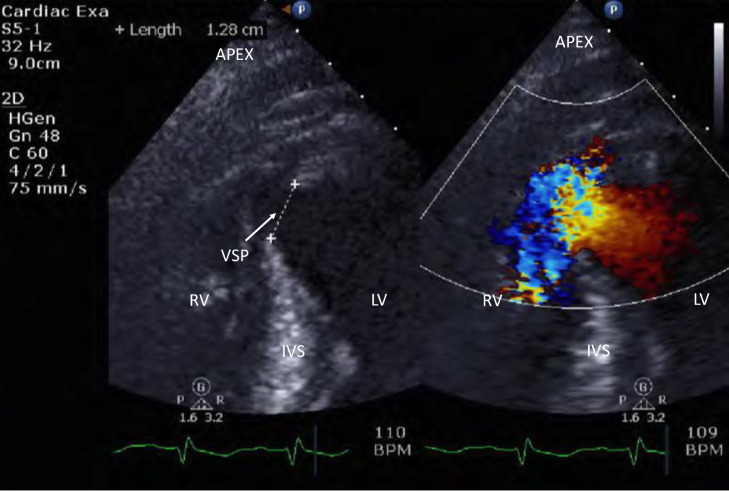
Chest X-ray revealed a cardiothoracic ratio of 53% with bilateral pulmonary congestion. Electrocardiography showed sinus rhythm at a rate of 108 beats/min with ST elevation in leads II, III, aVF, and V2–V6. On transthoracic echocardiography (TTE), a VSP was detected at the cardiac apex with a high-velocity left-to-right shunt (Fig. 1). Contrast-enhanced computed tomography displayed left fifth rib fracture, atelectasis in the dorsal parts of both lower lung lobes, and a VSP with swollen left subpapillary muscles (Fig. 2A).
Fig. 1.
Preoperative transthoracic echocardiography (TTE). Transthoracic echocardiography on admission, revealing blood flow from the left to the right ventricle through a ventricular septal perforation (VSP) with a diameter of approximately 1.3 cm.
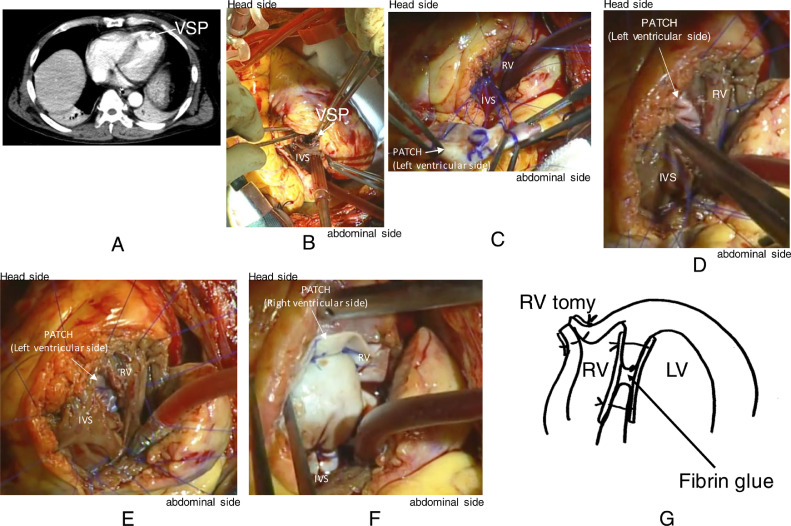
Fig. 2.
Preoperative imaging and intraoperative views. (A) Contrast-enhanced computed tomography illustrates a VSP near the apex. (B) The VSP (1.3 cm in diameter) is exposed during surgery. (C) The patch on the left ventricular side includes 8 mattress sutures. (D) Dutured LV side patch is inserted through the septal perforation into the LV. (E) Intraoperative photograph after LV side patch insertion to LV. (F) Intraoperative photograph after all the mattress sutures were tied. (G) Two circular patches are placed on both sides of the VSP with fibrin glue (BOLHEAL®) used to fill the space between the patches.
On the one hand, the patient's open right tibial fracture required urgent surgery, but on the other hand, it seemed difficult to control heart failure without VSP closure. Thus, given the patient's hemodynamic instability, emergency VSP closure was conducted with intra-aortic balloon pump (IABP) support.
Surgical procedure
Under general anesthesia, a median sternotomy was performed. After cardiopulmonary bypass was established with ascending aortic and bicaval cannulation, the right ventricle was incised longitudinally, exposing the VSP (approximately 1.3 cm in diameter) in the anterior septum near the apex (Fig. 2B). Then, the ascending aorta was cross-clamped, followed by the administration of antegrade cardioplegia. Under cardiac arrest, two circular patches (bovine pericardium) were placed on both sides of the VSP: one attached to the left ventricular side of the septal perforation by applying eight horizontal mattress 4–0 polypropylene sutures—buttressed with Teflon felt pledgets—through the VSP (Fig. 2C). Then the already sutured first patch was inserted through the septal perforation into the left ventricle (Fig. 2D, E) and the other sutured to the right ventricular side. Subsequently, all the mattress sutures were tied (Fig. 2F), and the interspace between the patches was filled with fibrin glue (BOLHEAL®, KM Biologics Co., Ltd., Kumamoto, Japan] (Fig. 2G). Next, the right ventriculotomy was closed using the Teflon felt strips. Following the disappearance of the shunt flow, the patient was uneventfully weaned from cardiopulmonary bypass with IABP support. The total operation time, cardiopulmonary bypass time, and aortic clamp time were 5 h and 28 min, 151 min, and 71 min, respectively.
Postoperative course
The patient was transferred to the intensive care unit and recovered uneventfully. The IABP and respirator were removed on postoperative days (PODs) 2 and 3, respectively. Because of hemodynamic stability after VSP closure, surgery for his right tibial fracture was performed on POD 10. TTE on POD 17 demonstrated a minor and negligible left-to-right shunt, mild mitral regurgitation, and mild tricuspid regurgitation.
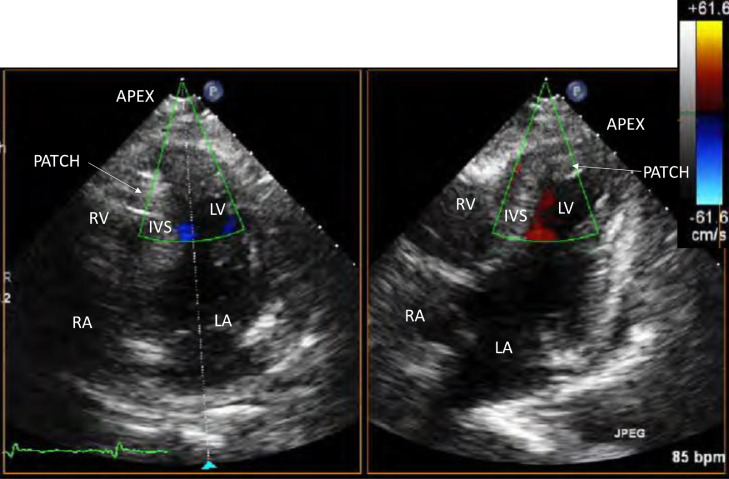
Afterward, the patient was transferred to the rehabilitation department of our hospital and was finally discharged on POD 118. Follow-up TTE at 4 years after VSP closure showed no residual shunt flow (Fig. 3), and the patient is currently living a normal daily life without any symptoms of heart failure.
Fig. 3.
Postoperative transthoracic echocardiography (TTE), exhibiting no residual shunt flow.
Discussion
VSP as a result of blunt chest trauma was first reported in 1847 [1]. According to Parmley et al., 5.5% of patients (30/546) undergoing autopsy following death from blunt cardiac injury had VSPs [2]. Various blunt chest traumas, ranging from strong external force experienced in traffic accidents to minor chest bruises from daily activities, have been reported to cause VSP through different mechanisms such as the following: cardiac compression between the sternum and the spine, cardiac contusion, and increased intracardiac pressure induced by the application of external force. The condition may develop even in the absence of presentations such as external scars, bleeding, or spots at initial examination [3]. In some patients, as in the present case, heart murmur is audible immediately after chest trauma; in others, however, it may not be detected until up to 1 month after the trauma. Conducting auscultation and echocardiography in the chronic stage after chest trauma is important, even if VSP is not diagnosed at the first visit. The timing of surgical treatment depends on the severity of heart failure and the urgency of other concomitant injuries. If circulatory dynamics are unstable, surgical treatment of VSP should be prioritized. In contrast, when hemodynamics are medically stabilized, waiting for the damaged myocardial tissue to become fibrotic may be more appropriate. It has been reported that cardiac surgery is advantageous when performed in the chronic stage of VSP as it allows for the formation of trabecular and endocardial fibrous tissue around the defect.
Treatment of congenital ventricular septal defect with a catheter device has become a standard therapeutic option superior to traditional surgery involving median sternotomy or minimally invasive cardiac surgery. Similarly, transcatheter closure with an Amplatzer septal occluder device (ASO; AGA Medical Corporation, Golden Valley, MN, USA) is an option for traumatic VSP treatment, in which case the edges of the perforation are often asymmetric, making it difficult to determine the size of the defect. Nevertheless, hemolysis has been shown to be one of the serious complications after transcatheter closure of traumatic VSP with an ASO [4].
Surgical closure of VSP involves either right or left ventriculotomy. In a study on post-myocardial infarction (MI) VSP, Javid et al. found that the right ventricular approach might be associated with the risks of residual shunt–due to irregular trabeculae in the right ventricle–and decreased right ventricular function. Besides, it has been suggested that post-MI patients with VSP are at risk for left ventricular free wall rupture as well [5]. The left ventricular approach not only prevents free wall rupture but also offers the advantage of feasibility because the trabeculae in the left ventricle are dense. Nonetheless, since the left ventricle is exposed to higher pressure compared to the right ventricle, left ventriculotomy entails the risk of bleeding. Considering the fact that our traumatic VSP patient had no extensive left ventricular infarction, the right ventricular approach was implemented. The advantages of right ventricular approach are easy control of bleeding and geometric preservation of the left ventricle. The disadvantage of right ventricular approach is risk of residual shunt due to irregular trabeculae and we think sandwich technique will prevent residual shunt. As reported by Seguine et al., using a fibrin sealant between patches can reduce the incidence of residual shunt [6]. Hence, the same procedure was followed herein.
Conclusion
The present report demonstrated successful closure of traumatic VSP via the right ventricular approach. Our case emphasizes the necessity of prompt surgery in the acute phase of traumatic VSP if medical treatment fails to stabilize circulatory dynamics.
Declaration of Competing Interest
The authors have no conflict of interest.
References
- 1.Hewett P. Rupture of the heart and large vessels, the result of injuries. Lond Med Gaz. 1847;1:870–872. [Google Scholar]
- 2.Parmley L.F., Manion W.C., Mattingly T.W. Nonpenetrating traumatic injury of the heart. Circulation. 1958;18:371–396. doi: 10.1161/01.cir.18.3.371. [DOI] [PubMed] [Google Scholar]
- 3.Harada T., Fukae K., Ando Y., Masahiro O., Matsunaga S., Yatsunami K., Matsuo O., Nishihara T. Ventricular septal perforation after blunt chest trauma: a case report. Pediatr Cardiol Cardiac Surg. 2016;32:50–53. [Google Scholar]
- 4.Tang L., Tang J.J., Fang Z.F., Hu X.Q., Shen X.Q., Zhou S.H. Severe mechanical hemolysis after transcatheter closure of a traumatic ventricular septal defect using the Amplatzer atrial septal occluder. Int Heart J. 2016;57:519–521. doi: 10.1536/ihj.15-407. [DOI] [PubMed] [Google Scholar]
- 5.Javid H., Hunter J.A., Naiafi H., Dye W.S., Julian O.C. Left ventricular approach for the repair of ventricular septal perforation and infarctectomy. J Thorac Cardiovasc Surg. 1972;63:14–24. [PubMed] [Google Scholar]
- 6.Seguin J.R., Frapier J.M., Colson P., Chaptal P.A. Fibrin sealant for early repair of acquired ventricular sepal defect. J Thorac Cardiovasc Surg. 1992;104:748–751. [PubMed] [Google Scholar]