Abstract
Behçet disease (BD) is a form of widespread vasculitis that involves both arteries and veins. Cardiac involvement in BD is exceedingly rare and can present as a form of non-bacterial- thrombotic-endocarditis (NBTE).
A 54-year-old man with Behçet disease was admitted to our hospital after presenting with abdominal pain and fever. He had been recently discharged from a hospital in another country with the diagnosis of infective endocarditis of the mitral valve and mycotic embolization to the superior mesenteric artery. At presentation, oral and genital ulcers were present, raising the suspicion of a flare of BD. Transesophageal echocardiography showed a small vegetation on the anterior leaflet of the mitral valve. Blood cultures results were negative. Computed tomography of the abdomen showed extensive inferior vena cava thrombosis. The aneurysm and thrombotic phenomena were interpreted as related to BD: the vegetation on the mitral valve was diagnosed as NBTE of which BD is a recognized cause. With corticosteroid and anticoagulant therapy, the patient's symptoms steadily improved.
NBTE is a rare manifestation of BD; differential diagnosis with infective endocarditis can be challenging and should be focused on identifying predisposing conditions.
The mainstay of treatment in NBTE is medical therapy with anticoagulation and treatment of the underlying disease.
<Learning objective: Cardiac involvement in the setting of Behçet Disease (BD) is rare and several different manifestations are described (intracardiac thrombus, non-infective endocarditis, myocarditis, pericarditis, endomyocardial fibrosis, coronary arteritis). Non-bacterial thrombotic endocarditis (NBTE) is also a rare finding which can happen in the setting of BD. Its prevalence is unknown and evidence is derived only from scarce case reports.The role of BD as a potential cause of NBTE must be acknowledged to avoid potential misdiagnosis.>
Keywords: Behçet disease, Non-bacterial- thrombotic-endocarditis, Echocardiography, Mitral valve disease, Deep vein thrombosis, Splanchnic artery aneurysm
Introduction
Behçet disease (BD) is an inflammatory disease characterized by widespread vasculitis that involves both arteries and veins. The typical presentation symptoms are recurrent oral and genital ulcers. Cardiovascular involvement in BD is estimated to range from 7 to 46%. It has been reported that venous involvement is 29%, and arterial involvement varies from 8 to 18% [1,2].
Cardiac involvement may occur in the form of intracardiac thrombus, non-infective endocarditis, myocarditis, pericarditis, endomyocardial fibrosis, coronary arteritis, myocardial infarction, and valvular disease [3,4].
Non-infective endocarditis as a manifestation of BD is described in the literature by several case reports [5–7]. Its prevalence amongst patients with BD is unknown [8].
Case report
A 54-year-old man presented to the emergency department with the main complaint of persistent abdominal pain and fever.
He had been recently discharged against medical advice from a hospital in another country, where he presented with the same symptoms, while he was travelling abroad. At that time, computed tomography (CT) of the abdomen revealed the presence of a 2.2 cm aneurysm of the superior mesenteric artery, which was treated with intravascular coil embolization. A subsequent echocardiogram showed images suggestive of a vegetation at the level of the mitral valve.
The patient then decided to return home for further treatment and was discharged with the final diagnosis of infective endocarditis with mycotic embolization to the superior mesenteric artery; three days later he presented to the emergency department of our hospital.
His-past medical history was significant for chronic obstructive pulmonary disorder and BD with cutaneous (typical oral and genital ulcers), ocular, and vascular (deep vein thrombosis) involvement. The disease had been initially treated with steroid therapy, and then switched to infliximab due to the development of severe osteoporosis.
During his stay outside Italy, the patient had skipped scheduled infusions of infliximab. His other medications included edoxaban 30 mg daily (dose reduction due to low body weight) and amoxicillin which was prescribed at discharge from the other hospital as empiric antibiotic therapy.
At physical examination in the emergency department, the patient was febrile with a body temperature of 37.4 °C, the abdomen showed mild tenderness in the lower quadrants, bowel sounds were present. Cardiac auscultation revealed rhythmic heart sounds and no murmurs.
Laboratory examinations were significant for leukocytosis (white blood cell count 12.10×109/L), anemia (hemoglobin 9.7 g/dL), and mildly elevated inflammatory markers (C-reactive peptide 34 mg/L), N-terminal pro-hormone of B-type natriuretic peptide was mildly elevated (489 pg/mL).
Blood culture results from the other hospital were not available: the patient was admitted to the cardiology ward and started on empiric antibiotic therapy with ampicillin, oxacillin, and gentamicin.
Blood cultures were drawn in the emergency department and the following day when the patient was transferred to the cardiology ward before starting antibiotic therapy: all cultures results were negative.
At further examination oral and genital ulcers were noted, raising the suspicion of a flare of BD.
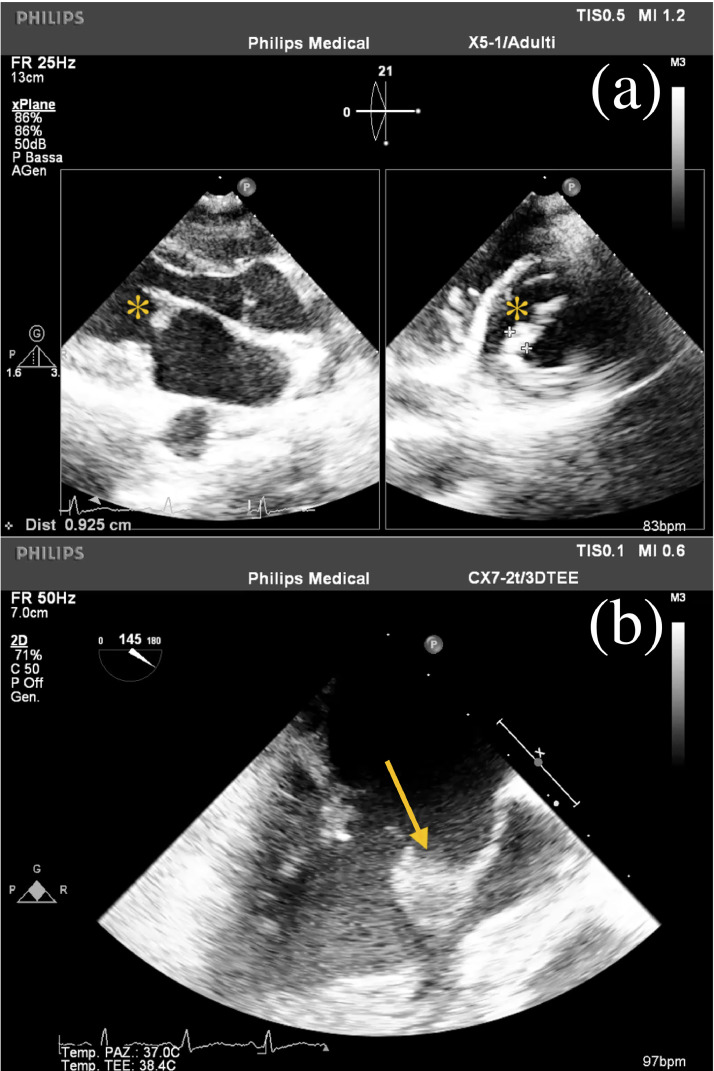
Combined transthoracic and transesophageal echocardiography showed marked thickening of the anterior mitral scallop and leaflet (10 mm), thickening and partial fusion of the respective chordae, and thickening of the P3 scallop with mild mitral regurgitation, findings suggestive of a small vegetation but no definite interpretation (Fig. 1; Online Videos 1,2). The other cardiac valves had no significant abnormalities and systolic function was preserved.
Fig. 1.
(a)Transthoracic echocardiographic images showing the sub-centimetric vegetation at the level of the anterior leaflet of the mitral valve, parasternal view (asterisks); (b) transesophageal echocardiographic view of the vegetation at the level of the mitral valve (arrow).
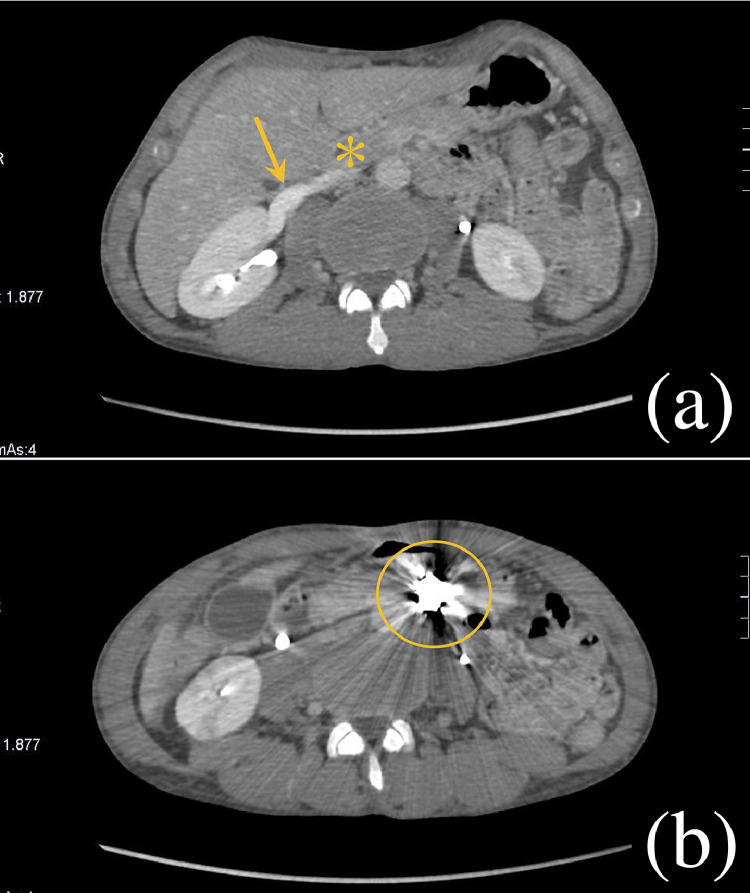
Due to persistent abdominal pain, a contrast CT of the abdomen was performed which confirmed the presence of an endovascular coil at the level of the superior mesenteric artery and revealed extensive inferior vena cava thrombosis up to the renal veins (Fig. 2) with the development of collateral venous circulation.
Fig. 2.
Abdominal contrast computed tomography slices showing: (a) patency of the right renal vein (arrow) and subsequent inferior vena cava thrombosis (asterisk); (b) the intravascular coil placed at the level of the superior mesenteric artery aneurysm during the previous hospital admission (circle).
Considering the manifest flare of BD, we ascribed the aneurysm of the superior mesenteric artery and the thrombotic phenomena to BD. We also attributed the findings at the level of the mitral valve to a form of non-infective endocarditis - of which BD is a recognized cause - since the Duke criteria for the diagnosis of infective endocarditis were not satisfied and blood cultures were persistently negative.
Empiric antibiotic therapy was stopped and, with high-dose intravenous methylprednisolone, the patient's symptoms steadily improved and the fever receded. Blood cultures drawn two days after the interruption of antibiotic therapy were persistently negative. We also screened the patient for Chlamydia, Coxiella, Legionella, and Bartonella, pathogens related to culture-negative infective endocarditis, and these were negative as well.
White cell count and inflammatory markers came back to normal values. Due to the evidence of thrombotic manifestations despite therapy with edoxaban, the patient was started on warfarin.
A pulmonary CT-angiogram ruled out the presence of pulmonary artery aneurysms, one of the most threatening complications of arterial involvement in BD.
The patient was discharged and referred to the immunology department for resuming therapy with infliximab.
A month after discharge he underwent an 18-fluorodeoxyglucose positron emission tomography-CT examination which excluded the presence of hypermetabolism at the level of the heart. Three months after discharge, at the time of the first infusion of infliximab, he was feeling well and was apyretic. We had scheduled follow-up echocardiography but the patient missed the appointment and was then lost to follow-up.
Discussion
Non-bacterial thrombotic endocarditis (NBTE) is a rare disease characterized by the formation of sterile vegetations and is associated with inflammatory or autoimmune disorders, cancer, and hypercoagulable states [8,9].
BD is recognized as a possible cause of non-bacterial endocarditis, although this evidence is derived exclusively from scarce case reports [5], [6], [7].
Deposition of sterile fibrin and platelets on the surface of the valve leaflets is the pathological mechanism resulting in NBTE [8–10].
Diagnosis and exclusion of an infective cause can be challenging. Definite diagnosis should rely on the integration of imaging, laboratory, and microbiologic findings as well as the research of predisposing conditions (cancer, hypercoagulable states, autoimmune disorders).
Echocardiography is the first imaging approach but is not able to differentiate sterile from infective vegetations. Sterile vegetations, though, tend to be smaller than those caused by bacterial endocarditis (typically less than 1 cm), and show a general predilection for the left-sided heart valves.
Patients with NBTE are often asymptomatic: the most common presenting symptom is systemic embolization. Valve destruction, and consequently valve insufficiency or heart failure, is infrequent [8–10].
Negative blood cultures can be misleading as up to 30% of patients with infective endocarditis presents with negative blood cultures (blood-culture negative infective endocarditis).
Anticoagulation, combined with adequate treatment of the underlying disease, is the mainstay of treatment of these forms. Surgery is rarely required as vegetations are usually small and do not cause significant valve damage.
Echocardiographic follow up, to ensure adequate anticoagulation and regression of the sterile vegetations with treatment, is advised [8,9].
Our patient presented with symptoms not related to his cardiac condition but to widespread venous involvement which is extremely common in BD. Arterial involvement, mainly manifesting with aneurysm formation, is less frequent: pulmonary artery aneurysms are the most threatening complication associated with BD and its presence was promptly excluded in our patient. Vascular manifestations tent to be more frequent in males.
The small, localized thickening at the level of the mitral valve was found incidentally and was suggestive of a small vegetation. Negative blood cultures and the lack of other Duke criteria necessary for the definite diagnosis of infective endocarditis, in association with the underlying disease and the presence of thrombotic manifestations in other districts, led to the final diagnosis of non-bacterial endocarditis related to a flare of BD.
Anticoagulation and immunosuppressant therapy were resumed and optimized: echocardiographic follow up was unfortunately not possible due to patient loss at follow up.
Conclusions
NBTE is a rare disease that can be one of the multiple manifestations of BD, a form of widespread vasculitis involving both arteries and veins.
Definite diagnosis of NBTE requires careful exclusion of an infective form taking into consideration laboratory and microbiological examinations, imaging findings, and presence of a predisposing pathology.
Anticoagulation and treatment of the underlying disease are fundamental to ensure regression of the lesions and to avoid the risk of systemic embolization which is the most frequent presenting symptom of NBTE.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2021.03.003.
Appendix. Supplementary materials
Transesophageal (1) and parasternal long-axis view (2) echocardiographic clips showing images suggestive of a small vegetation on the anterior leaflet of the mitral valve.
References
- 1.Sezen Y., Buyukhatipoglu H., Kucukdurmaz Z., Geyik R. Cardiovascular involvement in Behçet's disease. Clin Rheumatol. 2010;29:7–12. doi: 10.1007/s10067-009-1302-0. [DOI] [PubMed] [Google Scholar]
- 2.Demirelli S., Degirmenci H., Inci S., Arisoy A. Cardiac manifestations in Behcet's disease. Intractable Rare Dis Res. 2015;4:70–75. doi: 10.5582/irdr.2015.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owlia M.B., Mehrpoor G. Behcet's disease: new concepts in cardiovascular involvements and future direction for treatment. ISRN Pharmacol. 2012;2012 doi: 10.5402/2012/760484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Román Rego A., García Acuña J.M., Álvarez Rodríguez L., Rigueiro Veloso P., López Otero D., González Juanatey J.R. Cardiac involvement in a patient with Behçet disease. Diagnostic and therapeutic approach. Rev Esp Cardiol (Engl Ed) 2018;71:1075–1077. doi: 10.1016/j.rec.2017.09.017. [DOI] [PubMed] [Google Scholar]
- 5.Kang H.M., Kim G.B., Jang W.S., Kwon B.S., Bae E.J., Noh C.I., Choi J.Y., Kim Y.J. An adolescent with aortic regurgitation caused by Behçet's disease mimicking endocarditis. Ann Thorac Surg. 2013;95:e147–e149. doi: 10.1016/j.athoracsur.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 6.Lee H.S., Choi W.S., Kim K.H., Kang J.K., Kim N.Y., Park S.H., Park Y., Nam E.J., Yang D.H., Park H.S., Cho Y., Lee J.M., SC Chae. Aseptic endocarditis in Behçet's disease presenting as tricuspid valve stenosis. Korean Circ J. 2011;41:399–401. doi: 10.4070/kcj.2011.41.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nassenstein K., Deluigi C., Afube T., Schaaf B., Lorenzen J., Bruder O. Nonbacterial endocarditis presenting as a right ventricular tumor in assumed Behçet's disease. Herz. 2015;40:225–227. doi: 10.1007/s00059-013-4017-6. [DOI] [PubMed] [Google Scholar]
- 8.Hurrell H., Roberts-Thomson R., Prendergast B.D. Non-infective endocarditis. Heart. 2020;106:1023–1029. doi: 10.1136/heartjnl-2019-315204. [DOI] [PubMed] [Google Scholar]
- 9.Liu J., Frishman W.H. Nonbacterial thrombotic endocarditis: pathogenesis, diagnosis, and management. Cardiol Rev. 2016;24:244–247. doi: 10.1097/CRD.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 10.Bussani R., DE-Giorgio F., Pesel G., Zandonà L., Sinagra G., Grassi S., Baldi A., Abbate A., Silvestri F. Overview and comparison of infectious endocarditis and non-infectious endocarditis: a review of 814 autoptic cases. In Vivo. 2019;33:1565–1572. doi: 10.21873/invivo.11638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transesophageal (1) and parasternal long-axis view (2) echocardiographic clips showing images suggestive of a small vegetation on the anterior leaflet of the mitral valve.