Abstract
Summary
The aim of this study was to evaluate changes in activities of daily living and self-reported health status in the first year after fragility fractures of the pelvis. We found out that these fractures lead to a significant, long-lasting deterioration of both parameters, comparable with hip fractures.
Purpose
The aim of this prospective study was to evaluate the development and to identify influencing factors in activities of daily living (ADL) and self-reported health status (HS) in the first year after fragility fractures of the pelvis (FFP).
Methods
A total of 134 patients with FFP ≥ 60 years were included. ADL were measured using the Barthel index (BI) and the IADL scale pre-fracture, at 6 weeks, 6 months, and 12 months. HS was evaluated using the EQ-5D questionnaire at 6 weeks, 6 months, and 12 months. Multiple regression analysis and hierarchical linear models were applied to identify influencing factors in ADL and HS.
Results
The BI was 95 pre-fracture, 75 at 6 weeks (p < 0.001), 80 at 6 months (p = 0.178), and 80 at 12 months (p = 0.149). The IADL was 6 pre-fracture, 3 at 6 weeks (p < 0.001), 4 at 6 months (p = 0.004), and 4 at 12 months (p = 0.711). The EQ-5D index was 0.70 at 6 weeks, 0.788 at 6 months (p = 0.158), and 0.788 at 12 months (p = 0.798). Significant influencing factors in the multiple regression analysis were pre-fracture nursing care level for all scores; pre-fracture mobility for BI; and pre-fracture IADL, ASA score, and age for IADL. Significant influencing factors in the hierarchical linear model were pre-fracture nursing care level for all scores; pre-fracture IADL, ASA score, age, and time for IADL; and pre-fracture mobility, sex, and time for the EQ-5D.
Conclusion
Our results confirm that FFP lead to a significant, long-lasting deterioration in ADL and HS, comparable with hip fractures.
Keywords: Fragility fracture of the pelvis, Outcome, Self-rated health status, Activities of daily living, Osteoporosis, Geriatric fracture
Introduction
Osteoporosis-associated fragility fractures of the pelvic ring (FFP) are among the most frequent fractures in the elderly population [1]. Due to demographic change and increasing life expectancy, their prevalence has been steadily increasing in the last decades [2]. Despite this fact, relatively little has been known about these fractures, especially compared to osteoporotic hip fractures or vertebral fractures. Recently, a growing number of publications concerning pelvic fractures in geriatric patients can be found in the literature. These studies mainly focus on trauma mechanism, fracture morphology, classification systems, and treatment strategies [3–7].
However, little is known about the outcome after FFP. Some investigations have evaluated mortality and functional outcome [8–10]. Besides those objective facts, another important aspect is the patient-based, subjective evaluation of the outcome, particularly with regard to the patients’ abilities concerning activities of daily living (ADL), self-rated health status (HS), and health-related quality of life (HRQOL) [11]. So far, there are only a very limited number of investigations evaluating the abilities in ADL, HS, and HRQOL after FFP, and, to our knowledge, no prospective studies exist [10, 12–14].
The aim of this prospective study therefore was to evaluate the development of ADL and HS and to identify influencing factors in ADL and HS in the first year after FFP. It was expected that the outcome would be comparable with the outcome after hip fractures.
Methods
Study design and patients
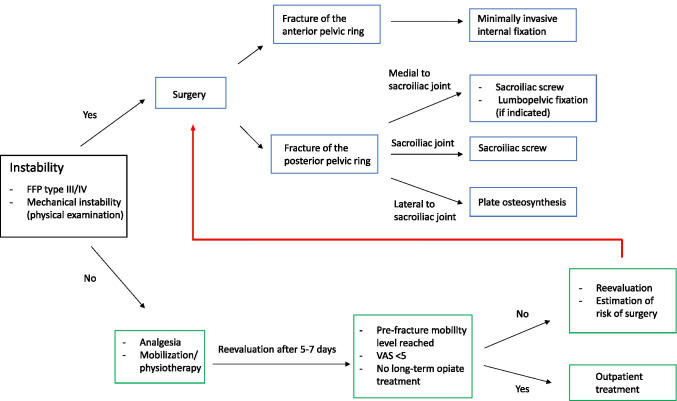
A total of 134 patients aged 60 years or older with FFP who were admitted to our university hospital from June 1, 2012, to December 31, 2016, and treated as inpatients were included in this prospective observational study. All types of FFP, with both conservatively and surgically treated patients, were involved. Exclusion criteria were isolated acetabular fractures, high-energy trauma (ISS ≥ 16) [15], and malignancy-related fractures. Treatment followed the in-house treatment algorithm for FFP in the authors’ institution (see Fig. 1) [16].
Fig. 1.
In-house treatment algorithm for FFP in the authors’ institution
The study was carried out in accordance with the Declaration of Helsinki. Institutional review board approval was obtained from the local ethics committee (AZ 22/12). All patients or their legal representatives provided written informed consent for participation in the study.
Follow-up
The patients were re-examined clinically and radiologically after 6 weeks and by telephone after 6 months and 12 months.
Assessment of ADL
ADL were assessed using the Barthel index (BI) [17] and the Lawton instrumental activities of daily living (IADL) scale [18].
The BI is an instrument for recording basic daily functions. The points achieved in 10 areas of basic ADL are added, resulting in a total score between 0 points (totally dependent) and 100 points (totally independent) [17].
The IADL scale measures more complex ADL skills in eight domains of function. The summary score ranges from 0 points (low function, dependent) to 8 points (high function, independent) [18].
Both scores were assessed at the following times: pre-fracture (retrospectively evaluated at the day of admission to the hospital, regarding the last week before the fracture occurred) and 6 weeks, 6 months, and 12 months after the trauma.
Assessment of self-rated health status
Self-rated health status was evaluated using the EQ-5D-3 L (three-level version) questionnaire. The EQ-5D questionnaire is a standardized measuring instrument of health status developed by the EuroQol Group [19]. It records the patient’s self-rated health with regard to five dimensions—mobility, self-care, usual activities, pain/discomfort and anxiety/depression—with three levels of severity (1 no problems, 2 some or moderate problems, 3 extreme problems) for each of the five dimensions [20]. The responses to the five dimensions are then converted in a single summary index value (EQ-5D index) using a country-specific value set. This country-specific value set provides weights for each health state description according to the preferences of the population of the respective country [21]. The German value set was applied in this study [22]. The EQ-5D index score ranges from a maximum score of 1, indicating perfect health, to less than 0, indicating a health state worse than death [21].
The EQ-5D was assessed at 6 weeks, 6 months, and 12 months after the fracture.
Additional patient data
Apart from socio-demographic patient data (age, sex), fracture type (FFP classification and AO/OTA classification) [3, 23], type of therapy (operative or nonoperative, surgical procedure where appropriate), American Society of Anesthesiologists (ASA) score [24], pre-fracture living situation and nursing care level, pre-fracture Mini-Mental State Examination (MMSE) [25], and the discharge type (geriatric rehabilitation, nursing home, home), inter alia, were recorded during hospital stay.
Data management and analysis
Data were collected in a FileMaker® database (FileMaker Inc., Santa Clara, CA, USA). IBM SPSS Statistics 24 for Mac (Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA) was used for statistical analysis. Means or medians, ranges, and standard deviations were calculated for descriptive analysis. The Kolmogorov–Smirnov test was used for assessment of normal distribution. Dependent variables were compared using the Wilcoxon test. The Mann–Whitney U test was applied for independent variables.
Afterwards, the influence of 11 variables (nonoperatively or operatively treated, fracture type according to the Rommens classification, fracture type according to the OTA classification, pre-fracture BI, pre-fracture IADL, pre-fracture mobility, age, sex, ASA score, pre-fracture MMST, and pre-fracture nursing care level) on the EQ-5D index, on the IADL scale, and on the BI at 6 weeks, 6 months, and 12 months after the fracture was modeled in nine stepwise multiple linear regressions.
Furthermore, three hierarchical models (linear mixed models) were applied to identify predictive variables on the EQ-5D index, the IADL scale, and the BI, respectively, for the three follow-up examinations simultaneously by modeling the time as a predictive variable. For all tests, statistical significance was assumed at p < 0.05.
Results
Descriptive statistics
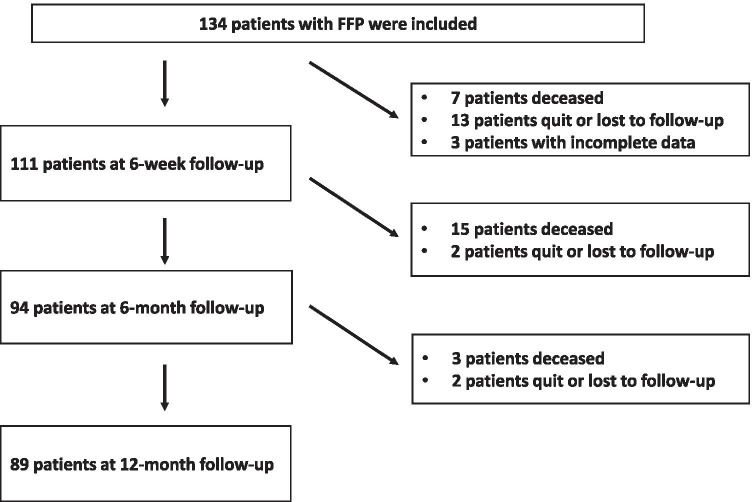
A total of 134 patients were included in the study. After deduction of all patients that were deceased, lost to follow-up, or had incomplete data concerning BI, IADL score, or EQ-5D index, 111 patients could be analyzed at 6 weeks, 94 patients at 6 months, and 89 patients at 12 months after the fracture. Figure 2 shows the flowchart of the study with the number of patients that had to be excluded from the analysis.
Fig. 2.
Flowchart of the study
The mean age of the patients at the time of fracture was 80 years; 83% were female, 64% were treated conservatively, and 36% had surgery. Detailed patients’ characteristics are shown in Table 1.
Table 1.
Baseline data of patients
| Age (mean ± SD) | 80 ± 8 (range: 60–99) |
| Gender | |
| Female | n = 111 (83%) |
| Male | n = 23 (17%) |
| Treatment | |
| Operative | n = 48 (36%) |
| Conservative | n = 86 (64%) |
| Fracture type (Rommes classification) | |
| FFP Ia | n = 39 (29%) |
| FFP Ib | n = 2 (2%) |
| FFP IIa | n = 11 (8%) |
| FFP IIb | n = 53 (40%) |
| FFP IIc | n = 17 (13%) |
| FFP IIIa | n = 5 (4%) |
| FFP IIIb | n = 4 (3%) |
| FFP IIIc | n = 1 (1%) |
| FFP IVa | n = 0 (0%) |
| FFP IVb | n = 2 (2%) |
| ASA score on admission (mean ± SD) | 2.8 ± 0.69 |
| ASA 1 | n = 2 (1%) |
| ASA 2 | n = 41 (31%) |
| ASA 3 | n = 79 (59%) |
| ASA 4 | n = 9 (7%) |
| ASA 5 | n = 3 (2%) |
| ASA 6 | n = 0 (0%) |
| MMSE on admission (mean ± SD) | 23.5 ± 5.47 (range: 6–30) |
| Pre-fracture living situation | |
| Alone | n = 52 (39%) |
| With partner/family | n = 67 (50%) |
| Nursing home | n = 15 (11%) |
The median score in the BI decreased significantly from 95 (min, 20; max, 100; mean, 86.38; standard error, 1.50) before the fracture to 75 (min, 10; max, 100; mean, 70.09; standard error, 2.55) at 6 weeks (p < 0.001), increased slightly, but not statistically significantly to 80 (min, 5; max, 100; mean, 75.53; standard error, 2.41) at 6 months (p = 0.178), and stayed constant at 80 (min, 0; max, 100; mean, 75.51; standard error, 2.54) at 12 months after the fracture (p = 0.149).
The IADL scale also decreased from a median score of 6 (min, 0; max, 8; mean, 4.99; standard error, 0.25) before the fracture to 3 (min, 0; max, 8; mean, 3.38; standard error, 0.25) at 6 weeks (p < 0.001), increased significantly to 4 (min, 0; max, 8; mean, 4.11; standard error, 0.30) at 6 months (p = 0.004), and stayed constant at 4 (min, 0; max, 8; mean, 4.26; standard error, 0.30) at 12 months after the fracture (p = 0.711).
The median of the EQ-5D index was 0.70 (min, − 0.21; max, 1; mean, 0.59; standard error, 0.03) at 6 weeks after the fracture, improved slightly, but not statistically significantly to 0.788 (min, − 0.21; max, 1; mean, 0.66; standard error, 0.03) at 6 months (p = 0.158), and stayed at 0.788 (min, − 0.21; max, 1; mean, 0.68; standard error, 0.03) at 12 months (p = 0.798).
Multiple regression analysis
Barthel index
Multiple regression analysis showed that the pre-fracture IADL scale was the only independent positive influencing factor and the pre-fracture nursing care level was the only independent negative influencing factor for the BI at 6 weeks after the fracture. Bad pre-fracture mobility and pre-fracture nursing care level both were independent negative influencing factors for the BI at 6 months, and bad pre-fracture mobility, pre-fracture nursing care level, and age were independent negative influencing factors for the BI at 12 months (see Table 2).
Table 2.
Significant independent influencing factors for Barthel index, IADL scale, and EQ-5D index 6 weeks, 6 months, and 12 months after surgery (multiple regression analysis)
| Ba | βb | p-value | ||
|---|---|---|---|---|
| Barthel index | ||||
| 6 weeks | Pre-fracture IADL | 3.333 | 0.365 | 0.001 |
| Pre-fracture nursing care level | − 7.673 | − 0.357 | 0.001 | |
| 6 months | Pre-fracture nursing care level | − 9.994 | − 0.510 | 0.000 |
| Pre-fracture mobility | − 13.342 | − 0.281 | 0.001 | |
| 12 months | Pre-fracture nursing care level | − 7.349 | − 0.357 | 0.001 |
| Pre-fracture mobility | − 12.000 | − 0.231 | 0.014 | |
| Age | − 0.669 | − 0.215 | 0.030 | |
| IADL scale | ||||
| 6 weeks | Pre-fracture IADL | 0.437 | 0.495 | 0.000 |
| Surgery | − 0.769 | − 0.144 | 0.020 | |
| ASA score | − 0.745 | − 0.188 | 0.005 | |
| Pre-fracture nursing care level | − 0.547 | − 0.262 | 0.003 | |
| 6 months | Pre-fracture IADL | 0.392 | 0.381 | 0.000 |
| Age | − 0.130 | − 0.340 | 0.000 | |
| Pre-fracture nursing care level | − 0.744 | − 0.294 | 0.001 | |
| 12 months | Pre-fracture IADL | 0.443 | 0.437 | 0.000 |
| Age | − 0.098 | − 0.261 | 0.001 | |
| Pre-fracture nursing care level | − 0.550 | − 0.222 | 0.032 | |
| EQ-5D index | ||||
| 6 weeks | Pre-fracture BI | 0.006 | 0.349 | 0.002 |
| Pre-fracture nursing care level | − 0.062 | − 0.241 | 0.031 | |
| 6 months | Pre-fracture nursing care level | − 0.105 | − 0.428 | 0.000 |
| ASA score | − 0.092 | − 0.194 | 0.046 | |
| 12 months | Pre-fracture nursing care level | − 0.120 | − 0.468 | 0.000 |
aNon-standardized regression coefficient
bStandardized regression coefficient
IADL scale
At 6 weeks after the fracture, the pre-fracture IADL scale was the only independent positive influencing factor; surgery, the ASA score, and pre-fracture nursing care level were independent negative influencing factors for the IADL scale. At six and at 12 months, the pre-fracture IADL scale was the only independent positive influencing factor; age and pre-fracture nursing care level were independent negative influencing factors (see Table 2).
EQ-5D index
Pre-fracture BI was the only independent positive influencing factor and pre-fracture nursing care level was the only independent negative influencing factor for the EQ-5D index at 6 weeks; ASA score and pre-fracture nursing care level both were independent negative influencing factors for the EQ-5D index at 6 months, and pre-fracture nursing care level was an independent negative influencing factor for the EQ-5D index at 12 months after the fracture (see Table 2).
Hierarchical linear model
The hierarchical linear model showed that the BI was only significantly influenced by the pre-fracture nursing care level as a negative influencing factor.
The IADL scale was significantly influenced by time (meaning that the IADL scale got significantly better over time) and pre-fracture IADL scale as positive influencing factors, and by age, pre-fracture nursing care level, and ASA score as negative influencing factors.
The EQ-5D index was significantly influenced by time and sex as positive influencing factors (meaning that the EQ-5D index got significantly better over time and that men had a higher EQ-5D index then women), and by pre-fracture nursing care level and bad pre-fracture mobility as negative influencing factors (see Table 3).
Table 3.
Significant influencing factors for Barthel index, IADL scale, and EQ-5D index in the hierarchical linear model
| Regression coefficient | p-value | ||
|---|---|---|---|
| Barthel index | Pre-fracture nursing care level | − 7.477 | 0.000 |
| IADL scale | Time | 0.255 | 0.008 |
| Pre-fracture IADL | 0.353 | 0.000 | |
| Age | − 0.064 | 0.003 | |
| Pre-fracture nursing care level | − 0.555 | 0.001 | |
| ASA score | − 0.738 | 0.002 | |
| EQ-5D index | Time | 0.038 | 0.021 |
| Sex | 0.111 | 0.041 | |
| Pre-fracture nursing care level | − 0.089 | 0.000 | |
| Pre-fracture mobility | − 0.118 | 0.005 |
Discussion
The aim of this study was to evaluate the development of ADL and HS and to identify influencing factors in ADL and HS in the first year after FFP.
Both scores measuring ADL—the IADL scale and Barthel index—showed a significant decrease 6 weeks after the fracture; they increased slightly until 6 months after the fracture and remained steady until 12 months after the fracture. The EQ-5D index at 6 weeks after the fracture was, at 0.70, considerably lower than the average EQ-5D index of 0.84 in the German population aged 75 years and older; improved slightly to 0.78 at 6 months after the fracture; and remained at 0.78 at the 12-month follow-up [26].
Significant influencing factors in the multiple regression analysis were, inter alia, pre-fracture nursing care level and pre-fracture mobility for the BI; pre-fracture nursing care level, pre-fracture IADL scale, ASA score and age for the IADL scale; and pre-fracture nursing care level for the EQ-5D index (for all significant influencing factors at the different follow-up investigations, see Table 2). Significant influencing factors in the hierarchical linear model were pre-fracture nursing care level for the BI; pre-fracture nursing care level, pre-fracture IADL scale, ASA score, age, and time for the IADL scale; and pre-fracture nursing care level, pre-fracture mobility, sex, and time for the EQ-5D index (see Table 3).
To our knowledge, this is the first prospective study measuring the BI, IADL, and EQ-5D index after fragility fractures of the pelvis. However, there are a limited number of retrospective investigations evaluating the abilities in ADL, HS, and HRQOL after FFP, using diverse measuring instruments.
Corresponding with our results, Schmitz et al., Höch et al., and Noser et al. all describe a lower patient-related quality of life after fragility fractures of the pelvis using the SF-36 questionnaire, the SF-12 questionnaire, the Majeed score, the visual analog scale, and the EQ-5D visual analog scale [12, 13, 29].
Banierink et al. recorded the physical functioning and health status of 53 elderly patients on average 3.4 years after pelvic ring injury and report significantly lower scores on the Dutch version of the Short Musculoskeletal Functioning Assessment and the EQ-5D index compared to the age-matched general Dutch population. The average EQ-5D index of 0.72 after 3.4 years was slightly lower than the EQ-5D index of 0.78 that we found in our study population 12 months after the fracture [27].
Breuil et al., Eckardt et al., Leung et al., Taillandier et al., and Yoshida et al. report a deterioration in activities of daily living, independence, and ambulatory status, which is also corresponding with the results of our study [8–10, 14, 28].
The results of these studies are only comparable to a limited extent because of the different study designs and the different scores that were assessed. They nevertheless do show, according to the findings of our study, that FFP cause a relevant and long-lasting deterioration in activities of daily living and health status. In contrast to our study, all of the abovementioned studies have a retrospective design and—except for the studies by Schmitz et al. and Yoshida et al.—a smaller number of patients was included [12, 28].
To date, only very few studies have evaluated influencing factors in ADL and HS after FFP.
In their abovementioned study, Leung et al. report no significant association between ambulatory status and sex, age, complications, or number of associated injuries in patients with FFP. However, they found a significant correlation between the change in ambulatory status and the presence of two or more comorbidities [9].
In contrast to the findings by Leung et al. and corresponding with our results, Taillandier et al. describe in their abovementioned study that age was associated with a loss of self-sufficiency one year after FFP [10]. These results are consistent with our findings that age was a significant negative influencing factor for the BI at 12 months and for the IADL scale at 6 months and 12 months after the fracture.
Looking at the significant influencing factors in ADL and HS that we identified in our study population, most of them are not unexpected: high pre-fracture nursing care level is a negative influencing factor for the BI, IADL scale, and EQ-5D index; limited pre-fracture mobility is a negative influencing factor for the BI and EQ-5D index; high pre-fracture IADL scale is a positive influencing factor for the IADL scale after the fracture; and a bad pre-fracture physical status, measured by the ASA score, is associated with lower scores on the IADL scale at 6 weeks after the fracture. All these influencing factors illustrate that low physical functioning before the fracture is associated with a poorer health status after FFP.
On the other hand, some findings are surprising. First, the male sex was associated with a higher score on the EQ-5D index. However, similar findings exist for hip fractures. In their literature review on quality of life after hip fracture, Peeters et al. describe strong evidence for the female sex being negatively associated with HS [30].
Another unexpected finding was that, in our study population, time was only associated with improving scores for the IADL scale and EQ-5D index in the hierarchical linear model, but not for BI. This might be explained by the fact that the BI measures basic daily functions that can be regained more easily and faster than the more complex skills that are measured on the IADL scale and in the EQ-5D index.
We expected the outcome after FFP to be comparable with the outcome after hip fractures. The EQ-5D index of 0.70 6 weeks after the fracture was marginally higher than the EQ-5D index of 0.54–0.57 that is reported in the literature four months after hip fracture [31, 32]. The EQ-5D index of 0.78 at 6 months and at 12 months after the fracture in our study population was also slightly higher than the scores between 0.6 and 0.64 that are found in the literature for six to 12 months after hip fracture [31–33].
Corresponding with the findings after hip fracture, our results show that the majority of the recovery after FFP takes place in the first two to 6 months [30].
Limitations
Our study has some limitations. First, the pre-fracture BI and IADL scale had to be evaluated retrospectively at the day of admission to the hospital, regarding the last week before the fracture occurred. Second, in contrast to the BI and IADL scale, the pre-fracture EQ-5D index was not recorded, and consequently, the scores at 6 weeks, 6 months, and 12 months after the fracture had to be compared to the average EQ-5D index in the age-matched German population. Another limitation of our study is the possible bias of the results due to the fact that some patients died or withdrew from the study during the study period and that, in addition, a few patients had to be excluded from the data analysis because of missing data. Since it is likely that the deceased patients had poorer quality of life and poorer abilities in activities of daily living and the surviving patients were the best functioning individuals, this may bias the results with possibly falsely high values. Last, the patient collective is inhomogeneous with regard to fracture type and therapy, because nonoperative and operative therapy as well as different operative procedures have been included. However, this might even be seen as a strength because it reflects the reality in clinical practice and a high number of patients could be included.
Conclusion
In conclusion, the results of this prospective study confirm that FFP lead to a significant and long-lasting deterioration in ADL and HS, comparable with hip fractures. Thus, awareness of this vulnerable patient group has to be raised, and establishing special therapy algorithms, similar to those that exist for hip fracture patients, seems to be essential.
Author contribution
All authors have made substantial contributions to the conception and design of the study.
Conception and design: LO, JH, SR, BB. Acquisition of data: LO, LS, JL, TK. Analysis and interpretation of data: LO, JH, SR, BB. Drafting of the manuscript: JH, LO. Revision of the manuscript: BB, LS, JL, TK, SR. All authors have read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
11/15/2021
The original version was revised due to an update in the funding note.
References
- 1.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Min Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 2.Kannus P, Palvanen M, Niemi S, et al. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970–1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11:443–448. doi: 10.1007/s001980070112. [DOI] [PubMed] [Google Scholar]
- 3.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44:1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Rommens PM, Wagner D, Hofmann A (2017) Fragility fractures of the pelvis. JBJS Rev 5: 10.2106/JBJS.RVW.16.00057 [DOI] [PubMed]
- 5.Wagner D, Ossendorf C, Gruszka D, et al. Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg. 2015;41:349–362. doi: 10.1007/s00068-015-0530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagner D, Kamer L, Sawaguchi T, et al. Sacral bone mass distribution assessed by averaged three-dimensional CT models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Jt Surg Am. 2016;98:584–590. doi: 10.2106/JBJS.15.00726. [DOI] [PubMed] [Google Scholar]
- 7.Linstrom NJ, Heiserman JE, Kortman KE, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976) 2009;34:309–315. doi: 10.1097/BRS.0b013e318191ea01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eckardt H, Egger A, Hasler RM, et al. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury. 2017;48:2717–2723. doi: 10.1016/j.injury.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Leung WY, Ban CM, Lam JJ, et al. Prognosis of acute pelvic fractures in elderly patients: retrospective study. Hong Kong Med J. 2001;7:139–145. [PubMed] [Google Scholar]
- 10.Taillandier J, Langue F, Alemanni M, Taillandier-Heriche E. Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Jt Bone Spine. 2003;70:287–289. doi: 10.1016/S1297-319X(03)00015-0. [DOI] [PubMed] [Google Scholar]
- 11.Ayers DC, Bozic KJ. The importance of outcome measurement in orthopaedics. Clin Orthop Relat Res. 2013;471:3409–3411. doi: 10.1007/s11999-013-3224-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitz P, Lüdeck S, Baumann F, et al. Patient-related quality of life after pelvic ring fractures in elderly. Int Orthop. 2018 doi: 10.1007/s00264-018-4030-8. [DOI] [PubMed] [Google Scholar]
- 13.Höch A, Özkurtul O, Pieroh P, et al. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr Orthop Surg Rehabil. 2017;8:3–9. doi: 10.1177/2151458516681142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breuil V, Roux CH, Testa J, et al. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Jt Bone Spine. 2008;75:585–588. doi: 10.1016/j.jbspin.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 15.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Oberkircher L, Ruchholtz S, Rommens PM, et al. Osteoporotic pelvic fractures. Dtsch Arztebl Int. 2018;115:70–80. doi: 10.3238/arztebl.2018.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 18.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 19.Group E EuroQol–a new facility for the measurement of health-related quality of life. Health Policy (New York) 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 20.Gusi N, Olivares P, Rajendram R (2010) The EQ-5D Health-Related Quality of Life Questionnaire. In: Preedy V, RR W (eds) Handbook of Disease Burdens and Quality of Life Measures. Springer, New York, pp 87–99
- 21.(2015) EQ-5D-3L user guide.
- 22.Greiner W, Claes C, Busschbach JJ, von der Schulenburg JM. Validating the EQ-5D with time trade off for the German population. Eur J Heal Econ. 2005;6:124–130. doi: 10.1007/s10198-004-0264-z. [DOI] [PubMed] [Google Scholar]
- 23.Isler B, Ganz R (1996) Classification of pelvic ring injuries. Injury 27 Suppl 1:S-A3–12 [DOI] [PubMed]
- 24.Saklad M. Grading of patients for surgical procedures.N. Anesthesiology. 1941;2:281–284. doi: 10.1097/00000542-194105000-00004. [DOI] [Google Scholar]
- 25.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 26.Janssen B, Szende A. Population norms for the EQ-5D. In: Szende A, Janssen B, Cabases J, editors. Self-Reported Population Health: An International Perspective based on EQ-5D. New York: Springer; 2014. pp. 19–30. [PubMed] [Google Scholar]
- 27.Banierink H, ten Duis K, de Vries R, et al. Pelvic ring injury in the elderly: fragile patients with substantial mortality rates and long-term physical impairment. PLoS ONE. 2019;14:e0216809. doi: 10.1371/journal.pone.0216809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoshida M, Tajima K, Saito Y, et al. Mobility and mortality of 340 patients with fragility fracture of the pelvis. Eur J Trauma Emerg Surg. 2020 doi: 10.1007/s00068-020-01481-3. [DOI] [PubMed] [Google Scholar]
- 29.Noser J, Dietrich M, Tiziani S, et al. Mid-term follow-up after surgical treatment of fragility fractures of the pelvis. Injury. 2018;49:2032–2035. doi: 10.1016/j.injury.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 30.Peeters CM, Visser E, Van de Ree CL, et al. Quality of life after hip fracture in the elderly: a systematic literature review. Injury. 2016;47:1369–1382. doi: 10.1016/j.injury.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 31.Svedbom A, Borgström F, Hernlund E, et al. Quality of life after hip, vertebral, and distal forearm fragility fractures measured using the EQ-5D-3L, EQ-VAS, and time-trade-off: results from the ICUROS. Qual Life Res. 2018;27:707–716. doi: 10.1007/s11136-017-1748-5. [DOI] [PubMed] [Google Scholar]
- 32.Peasgood T, Herrmann K, Kanis JA, Brazier JE. An updated systematic review of Health State Utility Values for osteoporosis related conditions. Osteoporos Int. 2009;20:853–868. doi: 10.1007/s00198-009-0844-y. [DOI] [PubMed] [Google Scholar]
- 33.Hack J, Buecking B, Aigner R, et al. What are the influencing factors in self-rated health status after hip fracture? A prospective study on 402 patients. Arch Osteoporos. 2019;14:92. doi: 10.1007/s11657-019-0642-x. [DOI] [PubMed] [Google Scholar]