Abstract
In periodontal health, oral streptococci constitute up to 80% of the plaque biofilm. Yet, destructive inflammatory events of the periodontium are rare. This observation suggests that oral streptococci may possess mechanisms to co-exist with the host. However, the mechanisms employed by oral streptococci to modulate the innate immune response have not been well studied. One of the key virulence factors produced by oral streptococci is hydrogen peroxide (H2O2). In mammalian cells, H2O2 triggers the activation of nuclear factor erythroid 2-related factor 2 (Nrf2), a key pathway mediating antioxidant defence. This study aimed to determine (1) if H2O2 producing oral streptococci activated the Nrf2 pathway in macrophages, and (2) if the activation of Nrf2 influenced the innate immune response. We found that oral streptococci downregulated the innate immune response in a H2O2 dependent manner through the activation of the Nrf2. The activation of the Nrf2 signalling pathway led to the inhibition of nuclear factor kappa-light-chain-enhancer of activated B cells (NFĸB), the key transcription factor regulating pro-inflammatory response. This study showed for the first time that oral streptococci are unlikely passive bystanders but could play an active role in the maintenance of periodontal health by preventing overt inflammation.
Subject terms: Microbiology, Diseases, Pathogenesis
Introduction
Periodontal disease is a plaque biofilm-mediated chronic inflammatory disease that affects the supporting structure of the teeth. Periodontitis affects 40% of the adult population and is the most common cause of tooth loss globally1. Patients suffering from periodontitis are also at higher risk for systemic diseases such as diabetes2 and cardiovascular disease3. The oral cavity is heavily colonised by microbial communities, with more than 700 bacterial species identified4,5. Collectively referred to as the oral microbiome, these bacterial species colonise distinct niches of the oral cavity, forming biofilms. Disturbances in the composition of plaque biofilm are the primary aetiological factor for the initiation of periodontal disease6.
Oral streptococci are the pioneer colonisers of the plaque biofilm. In periodontal health, oral streptococci are the dominant species of oral microbiota, which constitute between 60 and 80% of the total cultivable microbial flora7–10. Although the gingiva is exposed to large amounts of oral streptococci, destructive inflammation is rare, suggesting that these bacterial species likely possess mechanisms that modulate the innate immune response, facilitating co-existence with the host. However, mechanisms that enable oral streptococci to achieve symbiosis with the host have not been well studied.
The mitis group streptococci produce hydrogen peroxide (H2O2) as a by-product of aerobic metabolism11. Three enzymatic pathways for the generation of H2O2 in oral streptococci have been described. Pyruvate oxidase, encoded by the spxB gene is highly conserved in oral streptococci. This enzyme catalyses the conversion of inorganic phosphate and pyruvate to acetyl phosphate, carbon dioxide and H2O212. Oral streptococci also produce H2O2 via lactate and L-amino acid oxidases. Lactate oxidase catalyses the formation of H2O2 and pyruvate from lactate and oxygen, while L-amino acid oxidase catalyses the formation of peptone and H2O2 from L-amino acid in the presence of oxygen and water13,14.
The production of H2O2 by oral streptococci is thought to confer a competitive advantage over pathogenic microbes, enhancing their colonisation and survival in the oral cavity. Studies have reported that the production of H2O2 secreted by these organisms inhibited the growth of oral pathogens such as Streptococcus mutans15, and Porphorymonas gingivalis16. Thus, it has been put forth that H2O2 production likely contributes to shaping the biofilm composition towards a microbiome compatible with health. However, it is currently unknown if H2O2 secreted by oral streptococci modulates the innate immune response.
H2O2 belongs to the family of molecules termed reactive oxygen species (ROS). High concentrations of H2O2 elicit cell damage and cell death. At non-cytotoxic concentrations, H2O2 is an important intracellular signalling molecule that controls cellular processes including inflammation17–19. However, there have been conflicting reports concerning the pro- and anti-inflammatory properties of H2O2. For instance, H2O2 was demonstrated to stimulate the production of the pro-inflammatory cytokine tumour necrosis factor- α (TNF-α) in macrophages through the activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NFĸB) signalling pathway20,21. However, H2O2 secreted by Streptococcus pneumoniae was shown to prevent the activation of inflammasome in macrophages, consequently downregulating the innate immune response22.
The key cellular signalling pathway activated by H2O2 in mammalian cells is the nuclear factor E2-related factor 2 (Nrf2) antioxidant pathway. Nrf2 belongs to the Cap ‘n’ Collar (CNC) subfamily of basic region leucine zipper (bZaip) transcription factors. It is a ubiquitous transcription factor that regulates the expression of an array of antioxidant and detoxification genes, controlling the pathophysiological and physiological outcomes during oxidative stress23. Under normal physiological conditions, the expression of Nrf2 is minimal, due to its rapid turnover through constant degradation by the ubiquitin–proteasome system. During oxidative stress, the activation of Nrf2 pathway causes the nuclear translocation of Nrf2, inducing the expression of genes harbouring the antioxidant response element (ARE), a cis-acting DNA enhancer motif located in the promoter region of numerous antioxidant genes and enzymes that metabolise xenobiotics24,25. In addition, the Nrf2 signalling pathway appears to also play critical roles in regulating inflammation. For instance, Nrf2 knockout animals showed exacerbation of inflammation in emphysema and during sepsis, and have a predisposition to develop autoimmune and inflammatory phenotypes in various tissues26–29.
It is currently unknown if oral streptococci regulate the Nrf2 pathway. The objectives of this study were, (1) to determine if H2O2 producing oral streptococci activated the Nrf2 signalling pathway in macrophages, and (2) to determine if the activation of the Nrf2 pathway influenced the innate immune response in macrophages. We hypothesised that H2O2 secreted by oral streptococci upregulates the Nrf2 signalling pathway, dampening the innate immune response, thus enabling the maintenance of host-microbe homeostasis to sustain periodontal health.
Results
H2O2 producing oral streptococci activated the Nrf2-ARE pathway
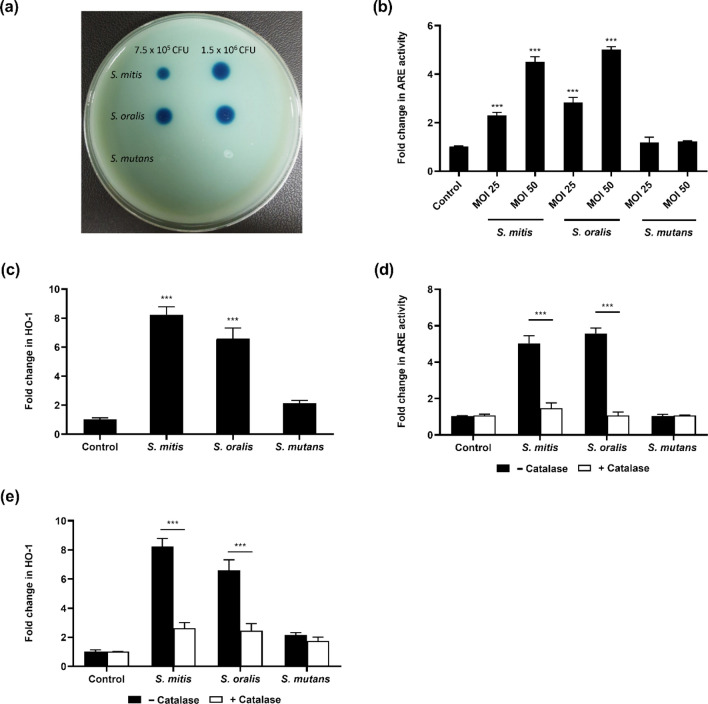
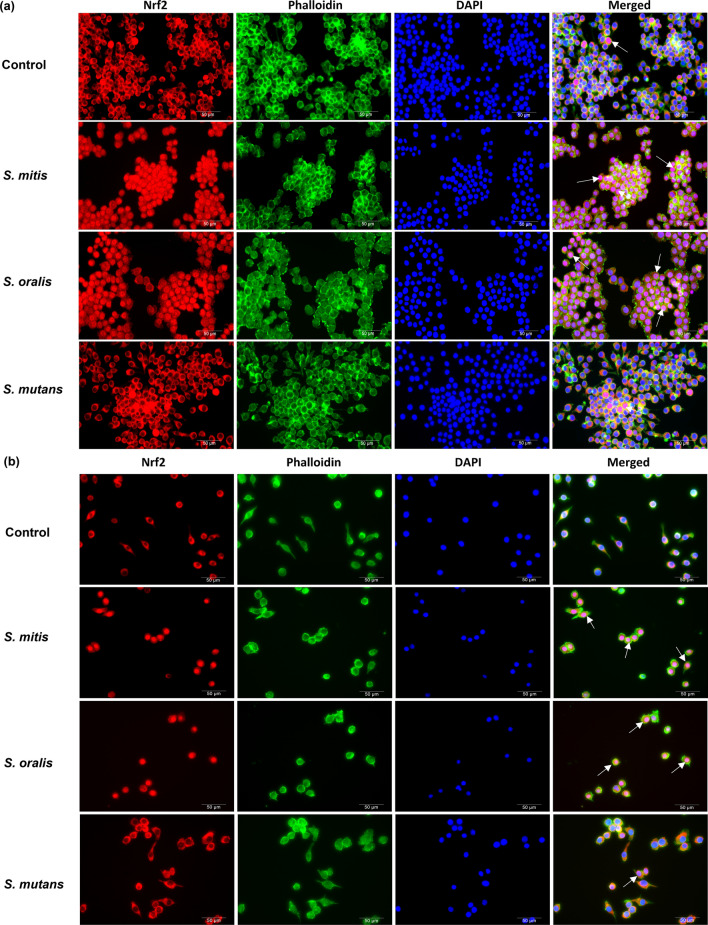
To determine if H2O2 producing oral streptococci modulated the Nrf2 signalling pathway, Raw 264.7 cells stably expressing the ARE-SEAP reporter were infected with H2O2 producing (S. mitis and S. oralis), and H2O2 non-producing oral streptococci species (S. mutans) (Fig. 1a). S. mitis and S. oralis but not S. mutans elicited a dose-dependent increase in Nrf2-ARE activity (Fig. 1b). The expression of the antioxidant genes namely, heme oxygenase-1 (HO-1) (Fig. 1c) and glutathione Peroxidase-3 (GPx-3) (Supplementary Fig. 1a) corroborated with the findings of the Nrf2-ARE reporter assay where S. mitis and S. oralis significantly activated the expression of these genes but not S. mutans. When exogenous catalase was added, S. mitis and S. oralis mediated activation of ARE (Fig. 1d) and upregulation of the antioxidant genes were abrogated (Fig. 1e; Supplementary Fig. 1b). In addition, it was observed that Nrf2 was predominantly sequestered in the cytoplasm in the control untreated cells (Fig. 2). However, treatment of Raw 264.7 macrophages with S. mitis or S. oralis led to the nuclear translocation of Nrf2, which was not observed in S. mutans infected cells (Fig. 2a). Similar results were obtained when bone marrow derived macrophages (BMDMs) were infected with these oral streptococci species (Fig. 2b). Both trypan blue exclusion and LDH assays showed that bacterial infection did not significantly affect the viability of macrophages (Supplementary Fig. 2). Collectively, these results demonstrated that S. mitis and S. oralis elicited the activation of antioxidant defence signalling in macrophages in a H2O2 dependent manner.
Figure 1.
H2O2 producing oral streptococci activated the Nrf2-ARE pathway. (a) The amount of H2O2 produced by oral streptococci was determined by the formation of blue halos on Prussian blue agar plates. (b) Raw 264.7 cells stably expressing the ARE-SEAP reporter were infected with S. mitis, S. oralis or S. mutans at the indicated MOIs. Cellular Nrf2-ARE activity was quantified by SEAP reporter assay. The expression of (c) HO-1 were determined by qRT-PCR. Raw 264.7 cells stably expressing the ARE-SEAP reporter were infected with S. mitis or S. oralis at MOI 50:1 in the presence and absence of 25U/mL of catalase. (d) ARE activity was determined by SEAP reporter assay while the expression of (e) HO-1 were determined by qRT-PCR. ***p < 0.001 compared to the respective control group.
Figure 2.
H2O2 producing oral streptococci induced nuclear translocation of Nrf2. (a) Raw 264.7 cells and (b) BMDMs were infected with the indicated oral streptococci species at MOI 50:1 for 5 h. Cellular localisation of Nrf2 was visualised following staining with anti-Nrf2 antibody (red). Cells were also stained with phalloidin (green), and DAPI (blue) for visualisation of cytoplasm and nuclei respectively. Representative immunofluorescence images are shown at 400× magnification. White arrows indicate nuclear translocated Nrf2. Scale bar: 50 μm.
Bacterial pyruvate oxidase mediated the activation of Nrf2 pathway in macrophages
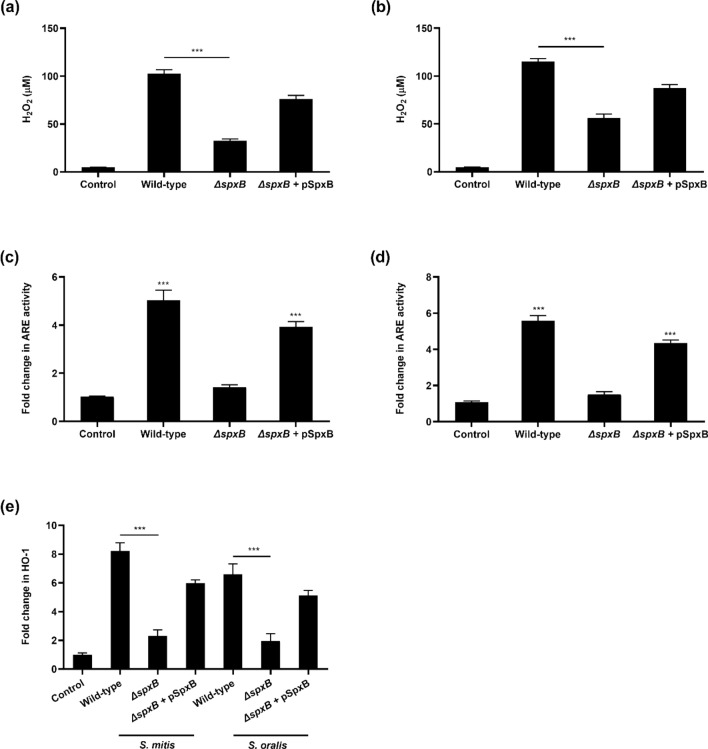
One of the key enzymes involved in the synthesis of H2O2 by oral streptococci is pyruvate oxidase (SpxB)11,12. To determine whether SpxB was the bacterial effector responsible for the activation of Nrf2, ΔspxB mutants of S. mitis and S. oralis were genetically engineered. Compared to the respective wild-type strains, ΔspxB mutants demonstrated 2–3 folds reduction in H2O2 production (Fig. 3a,b), which corresponded with reduced Nrf2-ARE activation (Fig. 3c,d) and the expression of HO-1 and GPx-3, compared to their respective wild-type strains (Fig. 3e and Supplementary Fig. 3). Restoration of SpxB function in S. mitis and S. oralis ΔspxB mutants through complementation restored the mutants’ ability to produce H2O2 which led to the activation of the host Nrf2 antioxidant defence system (Fig. 3 and Supplementary Fig. 3). These results provide evidence that SpxB mediated H2O2 production was responsible for the activation of the Nrf2 pathway, and the induction of synthesis of antioxidant genes in macrophages.
Figure 3.
Bacterial SpxB mediated the activation of Nrf2-ARE. The amount of H2O2 produced by wild-type, ΔspxB mutants and ΔspxB complemented mutant (ΔspxB + pSpxB) of (a) S. mitis and (b) S. oralis were measured. Raw 264.7 cells stably expressing the Nrf2-ARE SEAP reporter were infected with wild-type, ΔspxB mutants or ΔspxB complemented mutants of (c) S. mitis or (d) S. oralis. Cellular ARE activity was quantified by SEAP reporter assay. The expression of (e) HO-1 was determined by qRT-PCR. ***p < 0.001 compared to the control group.
Bacterial secreted H2O2 inhibited NFĸB
To determine whether H2O2 secreted by oral streptococci modulated the innate immune response, Raw 264.7 cells stably expressing the NFĸB-SEAP reporter were infected with wild-type or the ΔspxB mutants of S. mitis and S. oralis. Interestingly, macrophages infected with ΔspxB mutants demonstrated significantly higher levels of NFĸB activation compared to their respective wild-type strains (Fig. 4a,b). Similarly, the expression of the proinflammatory cytokines i.e. TNF-α and IL-1β by macrophages infected with ΔspxB mutants were higher compared to cells infected with wild-type strains at the mRNA (Fig. 4c,d) and protein levels (Fig. 4e,f). Complementation of SpxB function in S. mitis and S. oralis ΔspxB mutants restored the ΔspxB mutants’ ability to produce H2O2, and suppressed NFĸB signalling pathway and synthesis of the proinflammatory cytokines (Fig. 4a–f). Furthermore, H2O2 secreted by S. mitis and S. oralis suppressed Fusobacterium nucleatum or lipopolysaccharide (LPS)-induced NFĸB (Fig. 4g,h). Collectively, these results demonstrated a novel role of SpxB in immune suppression.
Figure 4.
Bacterial pyruvate oxidase mediated suppression of the host NFĸB. Raw 264.7 cells stably transfected with the NFĸB SEAP reporter were infected with wild-type (WT) bacteria, ΔspxB mutants and ΔspxB complemented mutant (ΔspxB + pSpxB) of (a) S. mitis or (b) S. oralis. Cellular NFĸB activity was quantified by SEAP reporter assay. ***p < 0.001 compared to the control group. The expression of (c) TNF-α and (d) IL-1β were determined by qRT-PCR. Amount of (e) TNF-α and (f) IL-1β protein was determined by ELISA. Macrophages were incubated with WT, ΔspxB mutants or ΔspxB complemented mutant of (g) S. mitis or (h) S. oralis, in the presence or absence of F. nucleatum (FN) and LPS. ***p < 0.001.
Activation of Nrf2-ARE by oral streptococci H2O2 inhibited the NFĸB signalling pathway
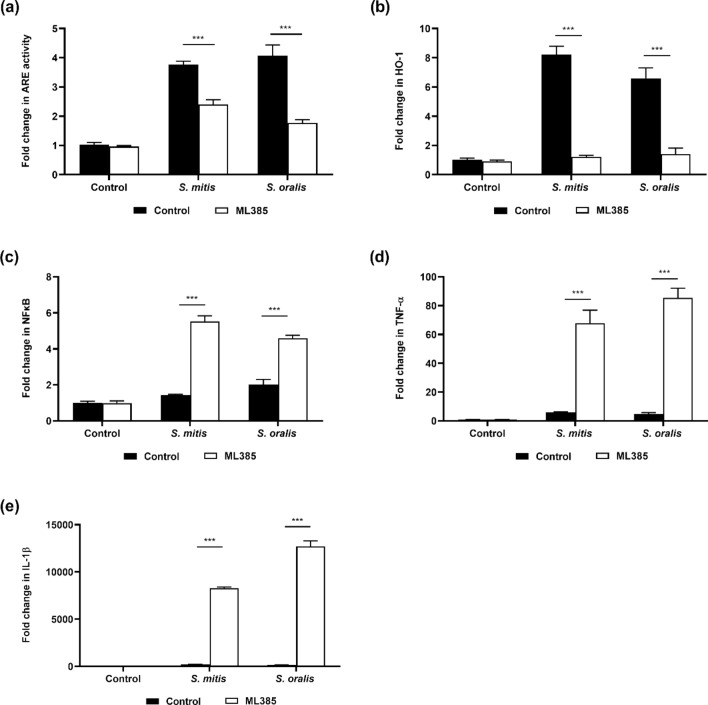
To determine if the activation of the host antioxidant pathway could potentially inhibit the innate immune response of macrophages, Raw 264.7 cells were treated with ML385, a Nrf2 inhibitor. It was observed that treatment of macrophages with ML385 led to the inhibition of S. mitis or S. oralis mediated Nrf2-ARE activation (Fig. 5a), and downregulation of the expression of HO-1 and GPx-3 (Fig. 5b, Supplementary Fig. 4). However, the inhibition of Nrf2 pathway led to enhanced NFĸB activation and potentiation of TNF-α and IL-1β production (Fig. 5c–e). ML385 did not affect the viability of the macrophages and bacteria (Supplementary Fig. 5).
Figure 5.
Activation of Nrf2 by oral streptococci inhibited the NFĸB signalling pathway. Raw 264.7 cells were pre-treated with 10 µM ML385 for 24 h prior to infection with oral streptococci. (a) Raw 264.7 cells stably transfected with the ARE SEAP reporter were infected with S. mitis or S. oralis. The expression of (b) HO-1 was determined by qRT-PCR. (c) Raw 264.7 cells stably transfected with the NFĸB SEAP were infected with bacteria. The expression of (d) TNF-α and (e) IL-1β were determined by qRT-PCR. ***p < 0.001.
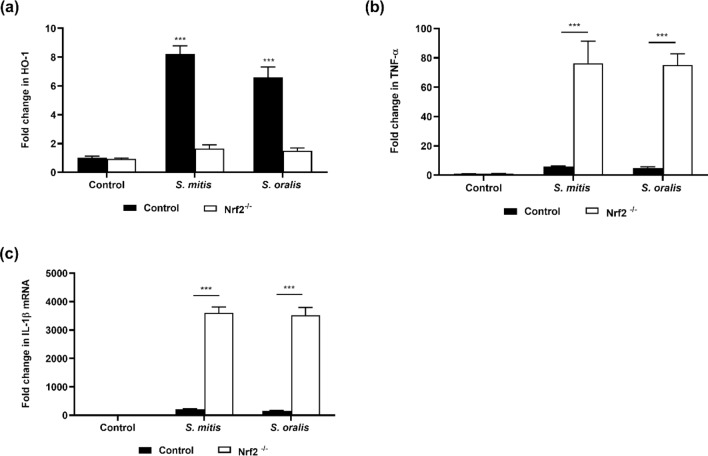
To confirm these results, Nrf2-/- Raw 264.7 cells were engineered (Supplementary Fig. 6). While the expression of HO-1 and GPx-3 increased significantly in the control macrophages following infection with S. mitis or S. oralis (Fig. 6a, Supplementary Fig. 7), this change was not observed in Nrf2-/- macrophages, providing evidence that these antioxidant genes were under the regulation of Nrf2. In Nrf2-/- macrophages, treatment with S. mitis or S. oralis led to enhanced TNF-α and IL-1β levels compared to wild-type macrophages, demonstrating that activation of Nrf2 suppressed the innate immune response (Fig. 6b,c).
Figure 6.
Activation of Nrf2 inhibits the innate immune response. Wild-type (control) or Nrf2-/- Raw 264.7 cells were infected with oral streptococci for 8 h and the expression of (a) HO-1, (b) TNF-α and (c) IL-1β were determined by qRT-PCR. ***p < 0.001.
Discussion
As periodontal health transitions to disease, a shift occurs in the oral microbiota. In disease, the amount of oral streptococci is diminished and the microbiota is dominated by gram-negative anaerobes10,30–32. A key metabolite secreted by oral streptococci species is H2O2. Previous studies have reported that H2O2 of oral streptococci led to the loss of viability of macrophages and oral epithelial cells33–35. However, those studies employed high bacterial loads and infection time. In this study, using bacterial loads which did not affect the viability of macrophages, we discovered that the production of H2O2 by oral streptococci inhibited the activation of NFĸB through the upregulation of the Nrf2-ARE antioxidant defence system pathway. Moreover, we showed that the SpxB was the bacterial effector involved in this process.
The ability to colonise and evade host defences would provide bacterial pathogens an advantage to survive. Since the NFĸB regulates immune surveillance, it is not surprising that successful pathogens have developed diverse strategies to evade host defences by exploiting or manipulating the NFĸB signalling pathway. For instance, the SseL of Salmonella enterica subsp. enterica serovar Typhimurium inhibits the ubiquitination of the inhibitory κB (IĸB) protein, preventing IĸB protein from degradation by the proteasome system36,37. Consequently, NFĸB remains sequestered in the cytoplasm, causing immune suppression. On the other hand, S. pneumoniae secreted H2O2 which inhibits the activation of inflammasomes through oxidative inactivation of the adaptor protein ASC and caspases22.
In this study, we discovered that S. mitis and S. oralis inhibited NFĸB in a H2O2 dependent manner. We further discovered that H2O2 secreted by S. mitis and S. oralis significantly downregulated LPS and F. nucleatum-mediated NFĸB activation. F. nucleatum is one of the early gram-negative bacterial species colonising the plaque biofilm. Compared to other gram-negative oral bacteria, we and others have demonstrated that F. nucleatum triggers strong pro-inflammatory responses38–40. Due to its ability to coaggregate with a wide variety of microorganisms, F. nucleatum plays an important role in plaque biofilm development serving as a key bridging organism between the early and late colonisers. The late colonisers, such as P. gingivalis, Treponema denticola and Tannerella forsythia are organisms associated with periodontal destruction41. Interestingly, in the absence of F. nucleatum, the amounts of periodontal disease associated bacteria reduced significantly42,43. Thus, through dampening of the immune response against F. nucleatum and LPS, it can be hypothesised that the SpxB of oral streptococci could potentially enhance the colonisation and survival of F. nucleatum and other gram-negative organisms in the plaque biofilm.
We found that in the presence of bacterial H2O2, the Nrf2 pathway was activated, resulting in an elevation in HO-1 and GPx3. HO-1 is an antioxidant that protects multiple organs against oxidative stress and regulates a variety of cellular activities, including cell oxidation and apoptosis44. HO-1 is a rate-limiting enzyme in heme catabolism and is responsible for the degradation of pro-inflammatory free heme into anti-inflammatory compounds such as carbon monoxide, free iron and bilirubin, which play major roles in maintaining the protective effects of HO-145. The critical role of Nrf2 mediated HO-1 expression for the anti-inflammatory activity was substantiated in a series of in vitro and in vivo experiments45. For instance, the elevation of Nrf2 mediated HO-1 expression leads to the inhibition of NFĸB signalling by preventing nuclear translocation of NFĸB, leading to a reduction in intestinal mucosal injury46. GPx3 is a selenium-containing antioxidant enzyme that reduces H2O2 and peroxide radicals with reduced glutathione (GSH), which is concomitantly oxidised to form oxidised glutathione (GSSG)47,48. As the major small molecule thiol in most organisms, GSH functions as a co-factor for GPx enzymes that quench H2O2 and other ROS49,50. Acute and chronic inflammation in the mice model has been shown to be caused by low GPx enzymatic activity in the mucosal epithelial49,51,52. In addition, increased GPx activity is associated with increased microbicidal activity in neutrophils, suggesting that GPx has potential anti-inflammatory properties53,54.
Studies have shown that H2O2 elicits activation of Nrf2 during oxidative stress55,56. Yet, it has been reported that the protein expression level of Nrf2 does not differ between periodontitis and periodontally healthy tissues57. The physiologically and clinical implications of Nrf2 activation by H2O2 producing oral streptococci are likely important during the early stages of colonisation of plaque biofilm formation. The ability to subvert the host's innate immune response will likely enable the bacteria with a colonisation advantage. However, as the plaque biofilm matures, the amount of oxygen available will decrease since bacteria within the biofilm matrix consume oxygen as they metabolise dietary sugars58,59. It has been shown that after 2 days of in vitro culture of plaque biofilm, the amount of dissolved oxygen content at the base of the biofilm reduced from 6 to 0.1 mg/l59. Additionally, a study also reported that the average oxygen profile measured in situ on dental biofilms decreased from 40 to 0% as the thickness of the biofilm increased60. Since the production of H2O2 by pyruvate oxidase is an oxygen-dependent process it can be anticipated that the H2O2 production by oral streptococci will decrease as plaque biofilm matures. This may explain why it was immunohistochemically demonstrated that the protein expression level of Nrf2 does not differ between periodontitis and periodontally healthy tissues, since the production of H2O2 by oral streptococci is expected to be low in these mature plaque biofilm57.
In summary, our results suggest that oral streptococci are likely not passive bystanders but could play an essential role in the maintenance of periodontal health through the prevention of overt inflammation. Future work will be required to understand the regulatory mechanisms involved in H2O2 production by oral streptococci, which might enhance our understanding of periodontal disease development. Since oral commensals naturally employ the Nrf2 pathway to downregulate inflammatory responses, another interesting area of further research will be to explore and identify suitable Nrf2 pathway modulators in the design of the next generation oral health care products for the prevention and treatment of oral inflammatory diseases.
Methods
Bacterial strains and culture
Streptococcus mitis ATCC 49456, Streptococcus oralis ATCC 35037, and Streptococcus mutans UA159 were obtained from the American Type Culture Collection (Manassas, VA, USA). Bacteria were cultured in brain heart infusion (BHI) broth (Acumedia, Lansing, MI, USA), and incubated at 37 °C with 5% CO2 supplementation.
Prussian blue agar assay
The Prussian Blue Agar was employed to detect H2O2 producing oral streptococci. This agar comprised 52 g/L of BHI agar (Acumedia), 1 g/L of iron (III) chloride (Sigma-Aldrich, St. Louis, MO, USA) and 1 g/L of potassium hexacyanoferrate (Sigma). Overnight cultures of oral streptococci were spotted on Prussian Blue agar, and incubated at 37 °C for 4 h before visualization.
spxB mutant generation and complementation
The spxB deletion (ΔspxB) mutants of S. mitis and S. oralis were generated as described previously with modifications33. Genomic DNA of S. mitis and S. oralis were extracted from overnight culture using QIAamp Mini kit (Qiagen, CA, USA). The upstream and downstream regions of the spxB gene were amplified using the primers spxKO-F1-BamHI and spxKO-R1. The PCR reactions consisted of 100 ng genomic DNA, 12.5 µl GoTaq PCR Master Mix (Promega, Madison, WI, USA), 0.2 µM of forward and reverse primers in a final reaction volume of 25 µl. The sequences of the primers used in the mutagenesis process are listed in Table 1. An aliquot of the purified upstream and downstream PCR products was used as a template in subsequent PCR reactions with the primer pair spxKO-F1-BamHI and spxKO-R2-SacI to yield an overlapping PCR fragment. The PCR products were purified and digested with BamHI and SacI, and ligated to BamHI and SacI digested pSET4s plasmid (Life Science Market, Scientific Hub Services, Singapore). Competent S. mitis and S. oralis were prepared by inoculating overnight bacterial culture into BHI media until OD600 of 0.05 was achieved. These bacterial cultures were incubated at 37 °C and 5% CO2 and growth were monitored every hour until OD600 reached 0.5. The bacterial cells were centrifuged at 3200 × g at 4 °C for 30 min, and the resulting supernatant was discarded. Bacterial cells were washed thrice with 10% ice-cold glycerol and resuspended in electroporation buffer (5 mM potassium phosphate [pH 4.5], 0.4 M sorbitol, 10% glycerol), and stored at − 70 °C.
Table 1.
Sequences of oligonucleotides used in mutagenesis.
| Primer | Sequence (5′ to 3′) | References |
|---|---|---|
| SpxKO-F1-BamHI | ATGGATCCCATCTTTATTATAAGCACCCTCAC | 33 |
| SpxKO-R1 | GAGAGTTATCATTATGACTCAGGATTGCAATC ACGCGCAATC | 33 |
| SpxKO-F2 | TTGCGCGTGATTGCAATCCTGAGTCATAATGA TAACTCTCCTTC | 33 |
| SpxKO-R2-SacI | GCGAGCTCATTGGTATCGAAGAGGTCATTGC | This study |
| Spx-inside-F | ACCATGGAGTAGACTCAACTGG | 33 |
| Spx-inside-R | ATGGATAACACTCCATTCCTTG | 33 |
| SpxB-EcoRI-F | ATGAATCCGGATTGCTCCGATCTTTTCA | This study |
| SpxB-BamHI-R | CTGGATCCCGAGCTTGCTCGCTTTTTAT | This study |
The recombinant plasmids were electroporated into competent S. mitis and S. oralis using a Bio-Rad MicroPulser™ electroporator (Bio-Rad Laboratories) at 3.0 kV using 0.2 cm electroporation cuvette (Bio-Rad Laboratories, Hercules, CA, US). Transformants were grown at 28 °C and selected on BHI agar plates containing spectinomycin (100 µg/ml). Single-crossover mutants were selected by culturing the bacteria on agar plates containing spectinomycin at 37 °C. Double-crossover mutants were obtained by repeated passaging on agar plates with no antibiotics at 28 °C, and determined by PCR using the primers targeting an internal region of the spxB gene (i.e. spx-inside-F and spx-inside-R); and subsequently confirmed by DNA sequencing.
S. mitis and S. oralis spxB mutants with spxB gene complementation were engineered using the method described previously61. The full length spxB gene was obtained by PCR using the primers SpxB-EcoRI-F and SpxB-BamHI-R (Table 1), was cloned into the Streptococcus-E. coli shuttle plasmid pDL278 via the EcoRI and BamHI restriction sites. The recombinant plasmid was introduced into the spxB mutants by electroporation and selected on agar plates containing spectinomycin as described above.
H2O2 assay
The amount of H2O2 produced by wild-type and ΔspxB S. mitis and S. oralis were determined using the ROS-Glo™ H2O2 Assay Kit (Promega) according to the manufacturer’s instruction.
Cell culture
The Raw 264.7 macrophage cell line was obtained from the ATCC. Cells were cultured in DMEM (Hyclone) supplemented with 10% FBS (Hyclone). The Raw 264.7 macrophage stably expressing the NFĸB-SEAP reporter62 was cultured in DMEM + 10% FBS supplemented with 500 μg/ml geneticin (Sigma-Aldrich). Bone marrow derived macrophages (BMDMs) were obtained from Cell Biologics (Cell Biologics, Chicago, USA) and cultured as described previously63. All cells were incubated at 37 °C in a humidified incubator supplemented with 5% CO2.
Generation of macrophage stable cell line stably expressing the ARE-SEAP reporter
An antioxidant response element (ARE)-SEAP reporter vector was generated by annealing two phosphorylated oligonucleotides with the ARE motif (ARE-F and ARE-R, Table 2). The resulting double-stranded fragment was subsequently ligated into KpnI and BglII digested pNFĸB-SEAP reporter plasmid expressing the neomycin gene resistance cassette, which encodes resistance to geneticin62. The sequence of the recombinant vector engineered was confirmed by DNA sequencing. Raw 264.7 macrophages were transfected with the ARE-SEAP reporter plasmid using Lipofectamine 3000 (Thermo Fisher Scientific, Waltham, MA, US) according to the manufacturer’s protocol. SEAP activity in the culture supernatant was measured using a Phospha-Light assay kit (Life Technologies, Rockville, MD, USA), according to the manufacturer’s protocol.
Table 2.
ARE oligonucleotide sequences used in this study.
| Oligonucleotide | Sequence (5′ to 3′) | References |
|---|---|---|
| ARE-F | CTAGCTTGGAAATGACATTGCTAATGGTGACAAAGCAACTTTTAGCTTGGAAATGACATTGCTAATGGTGACAAAGCAACTTTA | This study |
| ARE-R | GATCTAAAGTTGCTTTGTCACCATTAGCAATGTCATTTCCAAGCTAAAAGTTGCTTTGTCACCATTAGCAATGTCATTTCCAAGCTAGGTAC | This study |
Cell infection
Cells were infected with oral streptococci at the required multiplicity of infection (MOI), in the presence or absence of 25U/ml of catalase (Sigma-Aldrich) and incubated at 37 °C in a humidified incubator supplemented with 5% CO2 for 8 h. Cellular ARE and NFĸB activities were quantified using the SEAP reporter assay as described above.
Cell viability assays
The viability of macrophages after bacterial infection were determined by trypan blue exclusion and Lactate Dehydrogenase (LDH) assays. For trypan blue assay, equal volume of 0.4% of trypan blue (Sigma-Aldrich) was added to cell suspension and the number of viable cells enumerated. The LDH assay was carried out using the CytoTox 96 Non-Radioactive Cytotoxicity Assay Kit (Promega) according to the manufacturer’s protocol.
Immunofluorescence
Raw 264.7 cells were seeded at a density of 3 × 104 cells/well in a 96-well plate. BMDMs were seeded at a density of 1 × 104 cell/well. These cells were infected with oral streptococci as described above. Cells were fixed with 4% paraformaldehyde, followed by permeabilization with 0.2% Triton-X in PBS for 15 min and blocked for 1 h at room temperature with PBS containing 5% bovine serum albumin (Sigma-Aldrich). Cells were stained with primary antibody against Nrf2 (ab31163; Abcam, MA, USA) overnight at 4 °C. Subsequently, cells were incubated with goat anti-rabbit IgG (Alexa Fluor® 488, ab150077; Abcam) in the dark for 1 h at room temperature. Nuclei and cytoskeleton were sequentially counterstained with 4′6-diamidino-2-phenylindole, DAPI (Abcam) and Phalloidin-iFluor 594 reagent (Abcam) respectively. Representative fluorescence images were captured using a DMi8 fluorescence microscope (Leica Microsystems, Wetzlar, Germany).
ML385 treatment
Raw 264.7 macrophages were seeded at a density of 3 × 104/well in 96-well tissue culture plates (Nunc) and allowed to adhere overnight. The Nrf2 inhibitor ML385 (Sigma) was added into the cell culture media at 10 µM and incubated for 24 h. The next day, cells were infected with oral streptococci for 8 h. Culture supernatant was harvested and the amount of cellular ARE or NFĸB activity was quantified by measuring SEAP reporter activity as described above. The expression of target genes was determined by qPCR.
Nrf2 gene knockout
Raw 264.7 cells with Nrf2 gene knockout were engineered via the CRISPR/Cas9 genome editing method. pLentiCRISPRv2 plasmids harbouring the Nrf2 CRISPR gRNA target sequences 5′-TAGTTGTAACTGAGCGAAAA (NFE2L2 CRISPR Guide RNA 1) and 5′-GCATACCGTCTAAAT CAAC (NFE2L2 CRISPR Guide RNA 2) were obtained from GenScript (NJ, USA). The pLentiCRISPRv2 plasmids were transfected into Raw 264.7 cells using Lipofectamine 3000 (ThermoFisher Scientific). The efficiency of Nrf2 knockdown was determined via immunofluorescence staining with primary antibodies against Nrf2 as described above.
RNA extraction and qPCR analysis
Total RNA from treatment and non-treatment groups of Raw 264.7 cells were extracted using the RNeasy Mini Kit (Qiagen, Valencia, CA, USA) with on-column DNaseI treatment according to the manufacturer’s protocol. Reverse transcription (RT) of RNA to cDNA was performed using the iScript Reverse Transcription SuperMix (BioRad, Hercules, CA, USA). qPCR was performed using a CFX Connect Real-Time Detection System (BioRad). The reaction mixture consisted of 1 μl of cDNA, 10 μl of iTaq Universal SYBR Green Supermix (BioRad), 1 μl each of 10 µM of respective forward and reverse primers and nuclease-free water in a final volume of 20 μl. The expression of the respective target gene was normalized to the relative abundance of a housekeeping gene, beta actin. Fold changes in gene expression were calculated using the ΔΔCT method. The sequences of primers used are listed in Table 3.
Table 3.
Primer sequences used for qPCR analysis.
| Primer | Sequence (5′ to 3′) | References |
|---|---|---|
| GPx-3-F | ACAATTGTCCCAGTGTGTGCAT | This study |
| GPx-3-R | TGGACCATCCCTGGGTTTC | This study |
| HO-1-F | AAGCCGAGAATGCTGAGTTCA | This study |
| HO-1-R | GCCGTGTAGATATGGTACAAGGA | This study |
| TNF-α-F | CATCTTCTCAAAATTCGAGTGACCA | This study |
| TNF-α-R | TGGGAGTAGACAAGGTACAACCC | This study |
| IL-1β-F | CAACCAACAAGTGATATTCTCCATG | This study |
| IL-1β-R | GATCCACACTGTCCAGCTGCA | This study |
| Beta actin-F | GGCTGTATTCCCCTCCATCG | This study |
| Beta actin-R | CCAGTTGGTAACAATGCCATGT | This study |
Enzyme-linked immunosorbent assay (ELISA)
The amount of TNF-α and IL-1β protein in the culture supernatant were quantified by ELISA using the ELISA kits from Biolegend (San Diego, CA, USA). ELISA was performed according to the manufacturer’s instruction.
Statistical analysis
All experiments were performed in triplicate and repeated 3 independent times. The values were expressed as the mean ± standard deviation. Statistical analyses were performed using GraphPad Prism 8 software (GraphPad Software, Inc., USA). Differences between groups were assessed using one-way analysis of variance followed by Tukey's post hoc multiple comparison test. p < 0.05 was considered to indicate a statistically significant difference.
Supplementary Information
Author contributions
Conceptualization: K.S.T.; Study design: Y.L.T., T.S.S. & K.S.T. Data acquisition: Y.L.T.; Data analysis and interpretation: Y.L.T., T.S.S. & K.S.T; Manuscript preparation: Y.L.T., T.S.S. & K.S.T; Manuscript editing: Y.L.T., T.S.S. & K.S.T. All authors have read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-04562-4.
References
- 1.Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J. Dent. Res. 2012;91:914–920. doi: 10.1177/0022034512457373. [DOI] [PubMed] [Google Scholar]
- 2.Kocher T, König J, Borgnakke WS, Pink C, Meisel P. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol. 2018;2000(78):59–97. doi: 10.1111/prd.12235. [DOI] [PubMed] [Google Scholar]
- 3.Larvin H, Kang J, Aggarwal VR, Pavitt S, Wu J. Risk of incident cardiovascular disease in people with periodontal disease: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2021;7:109–122. doi: 10.1002/cre2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 2005;43:5721–5732. doi: 10.1128/JCM.43.11.5721-5732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dewhirst FE, et al. The human oral microbiome. J. Bacteriol. 2010;192:5002–5017. doi: 10.1128/JB.00542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat. Rev. Dis. Primers. 2017;3:1–14. doi: 10.1038/nrdp.2017.38. [DOI] [PubMed] [Google Scholar]
- 7.Nyvad B, Kilian M. Comparison of the initial streptococcal microflora on dental enamel in caries-active and in caries-inactive individuals. Caries Res. 1990;24:267–272. doi: 10.1159/000261281. [DOI] [PubMed] [Google Scholar]
- 8.Marsh PD, Lewis MA, Williams D, Martin MV. Oral Microbiology E-Book. Elsevier; 2009. [Google Scholar]
- 9.Aruni AW, et al. Filifactor alocis–a new emerging periodontal pathogen. Microbes Infect. 2015;17:517–530. doi: 10.1016/j.micinf.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Listgarten MA, Hellden L. Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J. Clin. Periodontol. 1978;5:115–132. doi: 10.1111/j.1600-051x.1978.tb01913.x. [DOI] [PubMed] [Google Scholar]
- 11.Zhu L, Kreth J. The role of hydrogen peroxide in environmental adaptation of oral microbial communities. Oxid. Med. Cell. Longev. 2012;2012:717843. doi: 10.1155/2012/717843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen L, et al. Identification of hydrogen peroxide production-related genes in Streptococcus sanguinis and their functional relationship with pyruvate oxidase. Microbiology. 2011;157:13. doi: 10.1099/mic.0.039669-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tong H, Chen W, Merritt J, Qi F, Shi W, Dong X. Streptococcus oligofermentans inhibits Streptococcus mutans through conversion of lactic acid into inhibitory H2O2: A possible counteroffensive strategy for interspecies competition. Mol. Microbiol. 2007;63:872–880. doi: 10.1111/j.1365-2958.2006.05546.x. [DOI] [PubMed] [Google Scholar]
- 14.Liu L, Tong H, Dong X. Function of the pyruvate oxidase-lactate oxidase cascade in interspecies competition between Streptococcus oligofermentans and Streptococcus mutans. Appl. Environ. Microbiol. 2012;78:2120–2127. doi: 10.1128/AEM.07539-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kreth J, Zhang Y, Herzberg MC. Streptococcal antagonism in oral biofilms: Streptococcus sanguinis and Streptococcus gordonii interference with Streptococcus mutans. J. Bacteriol. 2008;190:4632–4640. doi: 10.1128/JB.00276-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herrero ER, et al. Antimicrobial effects of commensal oral species are regulated by environmental factors. J. Dent. 2016;47:23–33. doi: 10.1016/j.jdent.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Veal EA, Day AM, Morgan BA. Hydrogen peroxide sensing and signaling. Mol. Cell. 2007;26:1–14. doi: 10.1016/j.molcel.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Marinho HS, Real C, Cyrne L, Soares H, Antunes F. Hydrogen peroxide sensing, signaling and regulation of transcription factors. Redox Biol. 2014;2:535–562. doi: 10.1016/j.redox.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sies H. Role of metabolic H2O2 generation: Redox signaling and oxidative stress. J. Biol. Chem. 2014;289:8735–8741. doi: 10.1074/jbc.R113.544635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takada Y, et al. Hydrogen peroxide activates NF-kappa B through tyrosine phosphorylation of I kappa B alpha and serine phosphorylation of p65: Evidence for the involvement of i kappa b alpha kinase and syk protein-tyrosine kinase. J. Biol. Chem. 2003;278:24233–24241. doi: 10.1074/jbc.M212389200. [DOI] [PubMed] [Google Scholar]
- 21.Nakao N, et al. Hydrogen peroxide induces the production of tumor necrosis factor-α in RAW 264.7 macrophage cells via activation of p38 and stress-activated protein kinase. Innate Immun. 2008;14:190–196. doi: 10.1177/1753425908093932. [DOI] [PubMed] [Google Scholar]
- 22.Erttmann SF, Gekara NO. Hydrogen peroxide release by bacteria suppresses inflammasome-dependent innate immunity. Nat. Commun. 2019;10:1–13. doi: 10.1038/s41467-019-11169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kensler TW, Wakabayashi N, Biswal S. Cell survival responses to environmental stresses via the keap1-Nrf2-ARE pathway. Annu. Rev. Pharmacol. Toxicol. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 24.Jaiswal AK. Nrf2 signaling in coordinated activation of antioxidant gene expression. Free Radic. Biol. Med. 2004;36(1199–1207):2004. doi: 10.1016/j.freeradbiomed.2004.02.074. [DOI] [PubMed] [Google Scholar]
- 25.Malhotra D, et al. Global mapping of binding sites for Nrf2 identifies novel targets in cell survival response through ChIP-Seq profiling and network analysis. Nucleic Acids Res. 2010;38:5718. doi: 10.1093/nar/gkq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishii Y, et al. Transcription factor Nrf2 plays a pivotal role in protection against elastase-induced pulmonary inflammation and emphysema. J. Immunol. 2005;175:6968–6975. doi: 10.4049/jimmunol.175.10.6968. [DOI] [PubMed] [Google Scholar]
- 27.Thimmulappa RK, et al. Nrf2 is a critical regulator of the innate immune response and survival during experimental sepsis. J. Clin. Invest. 2006;116:984–995. doi: 10.1172/JCI25790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoh K, et al. Nrf2-deficient female mice develop lupus-like autoimmune nephritis. Kidney Int. 2001;60:1343–1353. doi: 10.1046/j.1523-1755.2001.00939.x. [DOI] [PubMed] [Google Scholar]
- 29.Ma Q, Battelli L, Hubbs AF. Multiorgan autoimmune inflammation, enhanced lymphoproliferation, and impaired homeostasis of reactive oxygen species in mice lacking the antioxidant-activated transcription factor Nrf2. Am. J Pathol. 2006;168:1960. doi: 10.2353/ajpath.2006.051113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nyvad B, Kilian M. Microbiology of the early colonization of human enamel and root surfaces in vivo. Scand. J. Dent. Res. 1987;95:369–380. doi: 10.1111/j.1600-0722.1987.tb01627.x. [DOI] [PubMed] [Google Scholar]
- 31.Marsh PD. Microbial ecology of dental plaque and its significance in health and disease. Adv. Dent. Res. 1994;8:263–271. doi: 10.1177/08959374940080022001. [DOI] [PubMed] [Google Scholar]
- 32.Cassels FJ, Hughes CV, Nauss JL. Adhesin receptors of human oral bacteria and modeling of putative adhesin-binding domains. J. Ind. Microbiol. 1995;15:176–185. doi: 10.1007/BF01569823. [DOI] [PubMed] [Google Scholar]
- 33.Okahashi N, Nakata M, Sumitomo T, Terao Y, Kawabata S. Hydrogen peroxide produced by oral streptococci induces macrophage cell death. PLoS ONE. 2013;8:e62563. doi: 10.1371/journal.pone.0062563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okahashi N, et al. Hydrogen peroxide contributes to the epithelial cell death induced by the oral mitis group of streptococci. PLoS ONE. 2014;9:e88136. doi: 10.1371/journal.pone.0088136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okahashi N, Nakata M, Kuwata H, Kawabata S. Streptococcus oralis induces lysosomal impairment of macrophages via bacterial hydrogen peroxide. Infect. Imm. 2016;84:2042–2050. doi: 10.1128/IAI.00134-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Le Negrate G, et al. Salmonella secreted factor L deubiquitinase of Salmonella typhimurium inhibits NF-κB, suppresses IκBα ubiquitination and modulates innate immune responses. J. Immunol. 2008;180:5045–5056. doi: 10.4049/jimmunol.180.7.5045. [DOI] [PubMed] [Google Scholar]
- 37.Rahman MM, McFadden G. Modulation of NF-κB signalling by microbial pathogens. Nat. Rev. Microbiol. 2011;9:291–306. doi: 10.1038/nrmicro2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peyret-Lacombe A, Brunel G, Watts M, Charveron M, Duplan H. TLR2 sensing of F. nucleatum and S. sanguinis distinctly triggered gingival innate response. Cytokine. 2009;46:201–210. doi: 10.1016/j.cyto.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 39.Quah SY, Bergenholtz G, Tan KS. Fusobacterium nucleatum induces cytokine production through T oll-like-receptor-independent mechanism. Int. Endod. J. 2014;47:550–559. doi: 10.1111/iej.12185. [DOI] [PubMed] [Google Scholar]
- 40.Bashir A, Miskeen AY, Hazari YM, Asrafuzzaman S, Fazili KM. Fusobacterium nucleatum, inflammation, and immunity: The fire within human gut. Tumor Biol. 2016;37:2805–2810. doi: 10.1007/s13277-015-4724-0. [DOI] [PubMed] [Google Scholar]
- 41.Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL., Jr Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998;25(134–144):1998. doi: 10.1111/j.1600-051x.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 42.Bradshaw DJ, Marsh PD, Watson GK, Allison C. Role of Fusobacterium nucleatum and coaggregation in anaerobe survival in planktonic and biofilm oral microbial communities during aeration. Infect. Immun. 1998;66:4729–4732. doi: 10.1128/IAI.66.10.4729-4732.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diaz PI, Zilm PS, Rogers AH. Fusobacterium nucleatum supports the growth of Porphyromonas gingivalis in oxygenated and carbon-dioxide-depleted environments. Microbiol. 2002;148:467–472. doi: 10.1099/00221287-148-2-467. [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, et al. New insights into the Nrf-2/HO-1 signaling axis and its application in pediatric respiratory diseases. Oxid. Med. Cell. Longev. 2019 doi: 10.1155/2019/3214196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmed SMU, Luo L, Namani A, Wang XJ, Tang X. Nrf2 signaling pathway: Pivotal roles in inflammation. Biochim. Biophys. Acta. Mol. Basis Dis. 2017;1863:585–597. doi: 10.1016/j.bbadis.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 46.Chi X, Yao W, Xia H, Jin Y, Li X, Cai J, Hei Z. Elevation of HO-1 expression mitigates intestinal ischemia-reperfusion injury and restores tight junction function in a rat liver transplantation model. Oxid. Med. Cell. Longev. 2015 doi: 10.1155/2015/986075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brigelius-Flohé R. Glutathione peroxidases and redox-regulated transcription factors. Biol. Chem. 2006;387:1329–1335. doi: 10.1515/BC.2006.166. [DOI] [PubMed] [Google Scholar]
- 48.Chang C, Worley BL, Phaëton R, Hempel N. Extracellular glutathione peroxidase GPx3 and its role in cancer. Cancers. 2020;12:2197. doi: 10.3390/cancers12082197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chu FF, Esworthy RS, Doroshow JH. Role of Se-dependent glutathione peroxidases in gastrointestinal inflammation and cancer. Free Radic. Biol. Med. 2004;36:1481–1495. doi: 10.1016/j.freeradbiomed.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 50.Kurutas EB. The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: Current state. Nutr. J. 2015;15:1–22. doi: 10.1186/s12937-016-0186-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Esworthy RS, et al. Mice with combined disruption of Gpx1 and Gpx2 genes have colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2001;281:G848–G855. doi: 10.1152/ajpgi.2001.281.3.G848. [DOI] [PubMed] [Google Scholar]
- 52.Esworthy RS, Binder SW, Doroshow JH, Chu FF. Microflora trigger colitis in mice deficient in selenium-dependent glutathione peroxidase and induce Gpx2 gene expression. Biol. Chem. 2003;384:597–607. doi: 10.1515/BC.2003.067. [DOI] [PubMed] [Google Scholar]
- 53.Serfass RE, Ganther HE. Defective microbicidal activity in glutathione peroxidase-deficient neutrophils of selenium-deficient rats. Nature. 1975;255:640–641. doi: 10.1038/255640a0. [DOI] [PubMed] [Google Scholar]
- 54.Arthur JR, McKenzie RC, Beckett GJ. Selenium in the immune system. J. Nutr. 2003;133(5):1457S–1459S. doi: 10.1093/jn/133.5.1457S. [DOI] [PubMed] [Google Scholar]
- 55.Mercado N, et al. Decreased histone deacetylase 2 impairs Nrf2 activation by oxidative stress. Biochem. Biophys. Res. Commun. 2011;406:292–298. doi: 10.1016/j.bbrc.2011.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yin J, Duan J, Cui Z, Ren W, Li T, Yin Y. Hydrogen peroxide-induced oxidative stress activates NF-κB and Nrf2/Keap1 signals and triggers autophagy in piglets. RSC Adv. 2015;5:15479–15486. doi: 10.1039/C4RA13557A. [DOI] [Google Scholar]
- 57.Kasnak G, Firatli E, Könönen E, Olgac V, Zeidán-Chuliá F, Gursoy UK. Elevated levels of 8-OHdG and PARK7/DJ-1 in peri-implantitis mucosa. Clin. Implant Dent. Relat. Res. 2018;20:574–582. doi: 10.1111/cid.12619. [DOI] [PubMed] [Google Scholar]
- 58.Stewart PS, et al. Reaction–diffusion theory explains hypoxia and heterogeneous growth within microbial biofilms associated with chronic infections. NPJ Biofilms Microbiomes. 2016;2:1–8. doi: 10.1038/npjbiofilms.2016.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khosravi Y, et al. Use of an oxygen planar optode to assess the effect of high velocity microsprays on oxygen penetration in a human dental biofilms in-vitro. BMC Oral Health. 2020;20:1–14. doi: 10.1186/s12903-020-01217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.von Ohle C, et al. Real-time microsensor measurement of local metabolic activities in ex vivo dental biofilms exposed to sucrose and treated with chlorhexidine. Appl. Environ. Microbiol. 2010;76:2326–2334. doi: 10.1128/AEM.02090-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dunny GM, Lee LN, LeBlanc DJ. Improved electroporation and cloning vector system for gram-positive bacteria. Appl. Environ. Microbiol. 1991;57:1194–1201. doi: 10.1128/aem.57.4.1194-1201.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tan KS, et al. Suppression of host innate immune response by Burkholderia pseudomallei through the virulence factor TssM. J. Immunol. 2010;184:5160–5171. doi: 10.4049/jimmunol.0902663. [DOI] [PubMed] [Google Scholar]
- 63.Moore EM, Ying G, West JL. Macrophages influence vessel formation in 3D bioactive hydrogels. Adv. Biosyst. 2017;1:1600021. doi: 10.1002/adbi.201600021. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.