Abstract
As scientific evidence evolves and clinical guidelines change, a certain amount of conflicting health information in the news media is to be expected. However, research is needed to better understand the public’s level of exposure to conflicting health information and the possible consequences of such exposure. This study quantifies levels of public exposure to one paradigmatic case: conflicting information about breast cancer screening for women in their 40s. Using a nationally-representative survey of U.S. adults aged 18–59 in 2016, we implemented four distinct types of measures of exposure to conflicting mammography information: an ecological measure based on keyword counts of local news closed-captioning, an inferred exposure measure based on a series of knowledge questions, a thought-listing exercise where respondents described their perceptions of mammography without prompting, and an explicit measure of self-assessed exposure to conflict. We examined the relationship between these exposure measures and four outcomes: confusion about mammography, backlash toward mammography recommendations, and confusion and backlash about health information more generally. We found moderate amounts of exposure to conflicting information about mammography, more among women than men. Exposure to conflicting information—across multiple measures—was associated with more confusion about mammography, more mammography-related backlash, and general health information backlash, but not general confusion about health information. These observational findings corroborate experimental-based findings that suggest potentially undesirable effects of exposure to conflicting health information. More research is needed to better understand how to mitigate these possible outcomes, in the context of a media landscape that proliferates exposure to multiple scientific perspectives.
Keywords: conflicting information, media exposure, mammography, nationally-representative survey
As scientific evidence evolves, new studies are published, and clinical guidelines change, a certain amount of conflict in the information environment available to the public is inevitable. Yet, when news norms tend to magnify conflict or the appearance of controversy (Gans, 1979)—coupled with an increasing volume of health content available in the broader information environment, with its proliferation of media outlets and round-the-clock news cycles—the likelihood of encountering conflicting health information grows. The importance of conflicting health information has been underscored with the COVID-19 pandemic (Gollust et al., 2020), but conflicting information characterizes many other health issues. Understanding exposure to and potential consequences of conflicting health information is thus an important priority for health communication research.
Past research has documented public awareness of conflicting health information about topics including nutrition (e.g., Lee et al., 2018; Nagler, 2014), medications (e.g., Carpenter et al., 2014), e-cigarettes (e.g., Tan et al., 2015), and, most recently, COVID-19 (e.g., Nagler et al., 2020), and there is nascent evidence that exposure to such information can produce negative cognitive outcomes, including confusion about and backlash toward health recommendations and research (Chang, 2015; Clark et al., 2019; Dixon & Clarke, 2012; Jensen & Hurley, 2012; Lee et al., 2018; Nagler, Yzer, et al., 2019). However, previous studies have assessed exposure either via survey self-report measures or experimental studies where exposure is manipulated. More research on exposure to conflict in naturalistic settings—and using a variety of measurement strategies—is needed to better understand both the extent of media exposure to conflicting health information and its possible consequences. To fill these gaps, the current study examines the prevalence and potential outcomes of public exposure to conflicting information about mammography—a paradigmatic case, given widespread media attention to conflicting recommendations about the age at and frequency with which average-risk women should be screened for breast cancer (Nagler, Fowler, et al., 2019).
Conceptualizing Conflicting Health Information
Scholars have conceptualized conflicting or contradictory health information in several ways (see Nagler & LoRusso, 2018 for a review). At its most basic level, conflicting health information presents two, usually opposing, sides of a particular topic. So-called “two-sided messages” (or “two-sided” or “competitive” frames) are a common convention in health and political journalism, and the effects of such messages on the public are well-documented (Chong, 2019). For example, this might occur when news coverage reports a “pro-policy” stance (e.g.., pro-soda tax) and an “anti-policy” stance (e.g., anti-soda tax). Such coverage can appear simultaneously in a single news story or over time (e.g., a pro-tax article followed at some later time by an anti-tax article) (Niederdeppe et al., 2014). Both of these contexts—simultaneous exposure or over-time exposure to conflicting perspectives—can be considered conflict in the public information environment
More relevant to the present context are two narrower conceptualizations of conflicting health information, which reflect nuances not captured when defining conflict solely in terms of sidedness (Nagler & LoRusso, 2018). The first defines conflicting messages as those that offer information about the same health behavior producing two distinct outcomes (Nagler, 2014). Using an exemplar from the nutrition context, a single health behavior (such as consumption of coffee) is reported to be linked to two different outcomes, one that is positive or a potential benefit (e.g., improved cognitive function) and one that is negative or a potential risk (e.g., increased risk of heart disease). When exposed to such information, decisional conflict could arise: Although the information itself might not conflict (i.e., coffee consumption could legitimately be linked to both outcomes), a person might nonetheless perceive conflict and thus question if they should consume coffee and, if so, how much. In contrast, a second conceptualization defines conflicting messages as those that provide competing claims about a particular behavior resulting in a particular health outcome (Nagler & LoRusso, 2018)—or, put another way, “two or more health-related propositions [statements or assertions about a health-related issue] that are logically inconsistent with one another” (Carpenter et al., 2016, p. 1175). For example, drawing from the mammography screening context, an individual woman cannot simultaneously initiate screening at age 40 (as recommended by some professional societies) and at age 50 (as recommended by others), as this information is logically inconsistent. This conceptualization therefore reflects informational conflict, whereby “people are confronted by two or more distinct propositions that they cannot simultaneously engage in or believe” (Nagler & LoRusso, 2018, p. 356). While the empirical literature remains limited, emerging evidence suggests that exposure to conflicting information (regardless of whether it reflects decisional or informational conflict) can have consequences for public understanding and health behavior (see Nagler & LoRusso, 2018 and Carpenter et al., 2016 for a review).
Possible Effects of Conflicting Health Information: The Case of Mammography
The context of mammography recommendations offers an exemplar of conflict in the public information environment. Breast cancer is the second most common cancer in women, and represents 15% of all new cancer cases in 2020 and 7% of all deaths (National Cancer Institute, n.d.). Screening through mammograms is considered the best way to detect breast cancer (Centers for Disease Control and Prevention, 2020), but for decades there has been expert disagreement over the age at and frequency with which women should get screened for breast cancer (Jacobson & Kadiyala, 2017). These debates gained broader public attention in 2009, when the United States Preventive Services Task Force (USPSTF) recommended against routine annual screening for women aged 40–49 at average risk for breast cancer, presenting conflict not only with its previous recommendation from 2002 but also with contemporaneous recommendations from other professional societies that recommended regular screening begin at 40 (including the American Cancer Society (ACS), the American College of Radiology, and the American College of Obstetrics and Gynecology). The publication of the USPSTF recommendation in November 2009—during the midst of Congressional deliberation over the Affordable Care Act—accompanied by broad public and policymaker concern about government intrusion into women’s health, contributed to a media firestorm (DeAngelis & Fontanarosa, 2010; Nagler, Fowler, et al., 2019).
The presence of conflict has persisted since 2009, as scientific evidence on the risks and benefits of mammography continues to grow. In October 2015, ACS updated their long-standing recommendations that average-risk women begin screening at age 40, recommending instead that annual screening for average-risk women begin at age 45 until age 55, at which point ACS recommends biennial mammography. In 2016, the USPSTF retained its recommendation of beginning routine biennial mammography at age 50. Thus, these two professional recommendations still conflict in terms of both age and frequency of screening. And news media continue to present this conflict to the public: one study reported that conflict and/or controversy were salient themes in more than half of all news coverage of the USPSTF draft recommendation (released in April 2015), the ACS 2015 recommendation, and the 2016 USPSTF final recommendation (Nagler, Fowler, et al., 2019). Past research suggests that such dissemination of conflicting information may generate two types of cognitive responses: confusion and backlash, about mammography in particular and health information more generally.
Confusion about and Backlash toward Breast Cancer Screening
One possible outcome of exposure to conflicting health information is confusion, or perceived ambiguity or uncertainty about the health topic in question (here, breast cancer screening). Both observational survey (Lee et al., 2018; Nagler, 2014; Shi et al., 2021) and experimental (Clark et al., 2019; Dixon & Clarke, 2012; Jensen & Hurley, 2012; Nagler, Yzer, et al., 2019) studies have linked exposure to conflicting health information with confusion, with several studies drawing on decision theory’s concept of ambiguity to inform this hypothesis. Decision theorist Daniel Ellsberg (1961, p. 659) originally proposed that one important condition under which ambiguity may be high is “where there is conflicting opinion and evidence [emphasis in original].” Thus, exposure to conflicting information could contribute to confusion along with a feeling of “ambiguity aversion,” which can take shape in negative beliefs, sometimes called backlash, toward the subject of ambiguity (Han, Kobrin, et al., 2007; Han, Moser, et al., 2007). Previous research on nutrition and cancer prevention (including on mammography in particular, see e.g., Nagler, Yzer et al. 2019) suggest that both confusion and these backlash cognitions might result from exposure to conflicting information (Clark et al., 2019; Han, Kobrin, et al., 2007; Han, Moser, et al., 2007; Lee et al., 2018; Nagler, 2014; Patterson et al., 2001).
Potential Carryover Effects of Conflicting Health Information
An additional concern is whether cognitive responses to conflicting information might extend beyond the health topic in question, by carrying over to other health topics or to health information in general. There is a growing body of research documenting these potential downstream carryover effects, defined here as a negative cognitive response about a topic other than or broader than the one for which there is conflict (Chang, 2015; Lee et al., 2018; Nagler, 2014; Nagler, Yzer, et al., 2019; Yang et al., 2020). For example, Nagler and colleagues (2019) found that women exposed to conflicting information about mammography not only reported greater ambivalence about mammography screening but also about other types of cancer screening, suggesting that the influence of conflicting information can carry over from one health domain (e.g., mammography) to other health domains (e.g., other types of cancer screening). Similarly, Chang (2015) found that participants exposed to news reports of conflicting research findings about milk consumption and jogging reported less favorable attitudes toward health research in general. This suggests that influence can carry over not only between health domains, but from specific health domains to a broader health context. If people are routinely exposed to conflicting information about mammograms and experience negative cognitions (i.e., mammography related confusion and backlash) as a result, these negative outcomes could contribute to reduced understanding of and trust in health information more generally.
Measuring Exposure to Conflicting Health Information
In order to ascertain potential consequences of conflicting information about mammography, it is first important to establish prevalence estimates of exposure to conflict. Although there has been high attention to conflicting recommendations among public health commentators and policymakers, considerable coverage of such recommendations in the news media (Nagler, Fowler, et al., 2019), and some indication of public awareness of key media events (like the 2009 USPSTF recommendation announcement) (Kiviniemi & Hay, 2012; Squiers et al., 2011), no nationally representative estimates of public exposure to mammography-related conflict are available. Yet if people are not exposed to conflicting information, there is no reason to be concerned about effects, whether positive or negative. As recent reviews make clear (Nagler, 2017; Niederdeppe, 2014), measuring public exposure to information is challenging, and different approaches have strengths and limitations. The main classes of media exposure measures are self-report survey measures, ecological measures capturing the volume or content of media in an individual’s environment, and measures that combine self-reports with ecological measures to create an individually-variant measure that assesses an individual’s likelihood of exposure to content (Nagler, 2017).
Self-reports have limitations related to respondents’ inaccurate recall as well as bias, if their motivations to recall a particular message about a particular topic correlate with their attitudes about the topic. Such biases can be overcome by using non-domain-specific measures (i.e., asking about news use in general, rather than recall of specific messages about mammography) or by asking respondents to report awareness of specific messages that are logically inconsistent (i.e., asking them about at what ages they have heard recommendations to initiate breast cancer), instead of asking them explicitly to recall conflicting information. Self-reported measures can thus vary based on two dimensions: whether the measures mention specific topics (content specificity); and whether the measures specifically refer to “contradictory or conflicting information” in the question scripting (obtrusiveness) (Nagler & Hornik, 2012). Ecological measures, on the other hand, avoid the concerns surrounding reporting bias since the content domain is measured in the individual’s environment, rather than as a function of an individual’s recall of exposure. However, such measures are always just a proxy for plausible exposure since individuals are never exposed to all available content in the media environment. Finally, hybrid measures attempt to marry measures of the information environment (such as news volumes) with an individual’s propensity to consume media in that environment.
The consequences of exposure to conflict can also vary based on audience factors that are important to measure: how the conflict is perceived by the audience (i.e., do they actually perceive conflicting information as having a negative valence) and how personally salient the conflicting information is (i.e., how relevant). As Carpenter and colleagues (2016, p. 1178) noted, “we recognize that perceptions of conflicting information, rather than the objective existence of conflicting information, are important determinants of people’s behavioral responses.” Thus, if individuals proactively recognize conflict in the environment and perceive that conflict to be negative or otherwise problematic, it is more likely that there will be deleterious consequences than if individuals do not assign any negativity to that exposure. As Carpenter and colleagues further propose, the personal salience of a topic around which there is conflict may influence “the degree to which individuals perceive informational conflict” (Carpenter et al., 2016, p. 1178). Thus, gender is likely an important factor shaping likelihood of perceived exposure to conflict about mammography, with women possibly perceiving conflict more than men given the salience of breast cancer for women.
The Current Study
Our study advances the literature on exposure to and potential consequences of conflicting health information by incorporating multiple and varied measurements of exposure, including ecological measures, direct self-report, and a range of obtrusive and less obtrusive measures that vary in whether they explicitly identify media as the source of conflicting information. This innovative multidimensional measurement approach responds to recent calls to “develop measures that accurately capture conflicting health information in its many potential manifestations” (Carpenter et al., 2016, p. 1180), as well as to further the use of ecological research in health communication studies (Moran et al., 2016). We include multiple measures of exposure to establish whether there is consistency in prevalence estimates and in the relationships between exposure to conflict and our cognitive outcomes of interest.
Specifically, the objectives of this study are twofold: (1) to assess the prevalence of population-level exposure to conflicting information about mammography, measured in multiple ways, and to examine whether prevalence differs by gender of respondent; and (2) to assess whether such exposure to conflicting information is associated with confusion about breast cancer screening recommendations and research, backlash toward these recommendations and research, and confusion about and backlash toward health information in general (as markers of potential carryover effects).
Method
Sample
The data for this study come from a nationally-representative survey fielded by the survey firm GfK between May 24 and June 6, 2016. GfK recruits a panel of research participants to their KnowledgePanel using probability sampling of addresses. For this study, GfK invited 2991 U.S. adult panel members aged 18–59 to participate in the survey. Of these, 1,519 agreed to participate for a completion rate of 51%. Participants were randomly assigned to one of two modules in the survey; data for this study come from the 1,113 participants who were assigned to a survey module that encompassed the measures of media exposure and perceptions of breast cancer screening and other health information detailed below. Characteristics of the sample are shown in Appendix Table 1. The study was reviewed and approved by the University of Minnesota Institutional Review Board. Respondents read a short study introduction before agreeing to participate; documentation of consent was waived because of the anonymous online study design. The survey items used in this study were displayed to respondents in the following order: health news consumption, thought-listing about mammograms, mammogram status (for women), awareness of mammograms (sequence described as “inferred” measures below), self-assessed exposure to conflict, confusion and backlash about breast cancer screening, general health information confusion and backlash, and confidence in institutions.
Appendix.
Descriptive Characteristics of the Sample (N = 1,113)
| Characteristic | Weighted % |
|---|---|
|
| |
| Female | 50.9 |
| Age | |
| 18–29 | 22.2 |
| 30–39 | 23.1 |
| 40–49 | 22.9 |
| 50–59 | 24.8 |
| Household Income | |
| Less than $15,000 | 9.2 |
| $15,000 to $34,999 | 13.6 |
| $35,000 to $49,999 | 11.6 |
| $50,000 to $74,999 | 18.1 |
| $75,000 to $99,999 | 15.4 |
| $100,000 or more | 32.0 |
| Education | |
| Less than high school | 11.7 |
| High school | 28.2 |
| Some college | 29.7 |
| Bachelor’s or higher | 30.4 |
| Race / ethnicity | |
| White, Non-Hispanic | 60.7 |
| Black, Non-Hispanic | 12.3 |
| Other, Non-Hispanic | 8.7 |
| Hispanic | 18.1 |
| Married | 48.5 |
| Mammogram status (ever had)a | |
| Yes | 64.9 |
| No | 35.1 |
Asked of women aged 30–59 (n = 554).
Measures
Independent Variables: Exposure to Conflicting Information about Mammography
We constructed four sets of measures of exposure to mammography conflict, adapting from and building on work by Nagler and Hornik (2012) in the nutrition context. The measures varied in their obtrusiveness to the study participant, how specific they are to the context of mammography conflict, whether they referred to media or not, and whether they incorporated participants’ own perceptions. These included 1) an ecological measure, 2) inferred exposure measures, 3) “top of head” thought-listing exposure measures, and 4) an overt self-assessed measure.
Ecological Exposure Measure.
The first (and least obtrusive) measure, ecological exposure, takes into account information on the volume of breast cancer screening-related news aired on local television in a respondent’s area of residence. Specifically, we conducted mammography-related keyword searches from the closed captioning of local television news aired from January 10, 2016 to the date that respondents answered the survey (between May 24 and June 6, depending on the participant). The keywords were derived from a set of pilot tests to ascertain that they reliably picked up news coverage of mammography and included the following: (cancer and screen*) OR mammog* OR (“services task force” and cancer). January 10, 2016 was the date that the USPSTF published updated recommendations for mammography screening. Content analyses suggested that about 55% of content in TV news coverage of these recommendations described conflict or controversy surrounding the recommendations; in 45% of the stories, the reporter or anchor mentioned conflict or controversy explicitly, and 36% referenced conflict across professional organizations’ recommendations (Nagler, Fowler, et al., 2019). To assign survey respondents to the volume of conflict in media coverage in their area, we linked the volume of keywords hits based on each participant’s Designated Market Area (DMA) of residence (available from GfK’s panelist data). To account for the fact that respondents vary in how much they would actually be exposed to this content based on their TV viewership habits, we multiplied the volume of content in a respondent’s DMA by a measure of a respondent’s local TV news consumption: “In the past seven days, on how many days did you watch the local news on television?” (responses ranged from 0 to 7 days and were rescaled to run between 0 and 1 before multiplication; 10 respondents who did not complete this item are missing from this measure, so n = 1,103). The resulting measure ranged from 0 (for the 28% of the sample that reported no local TV viewing, and thus were assigned none of the keywords in their DMA) to 414 (the highest bound, for a respondent who consumed local TV news every day of the week and lived in a DMA with 414 mammography-related keyword hits appearing on local TV between January 10, 2016 and the date of their survey).
Inferred Exposure Measures.
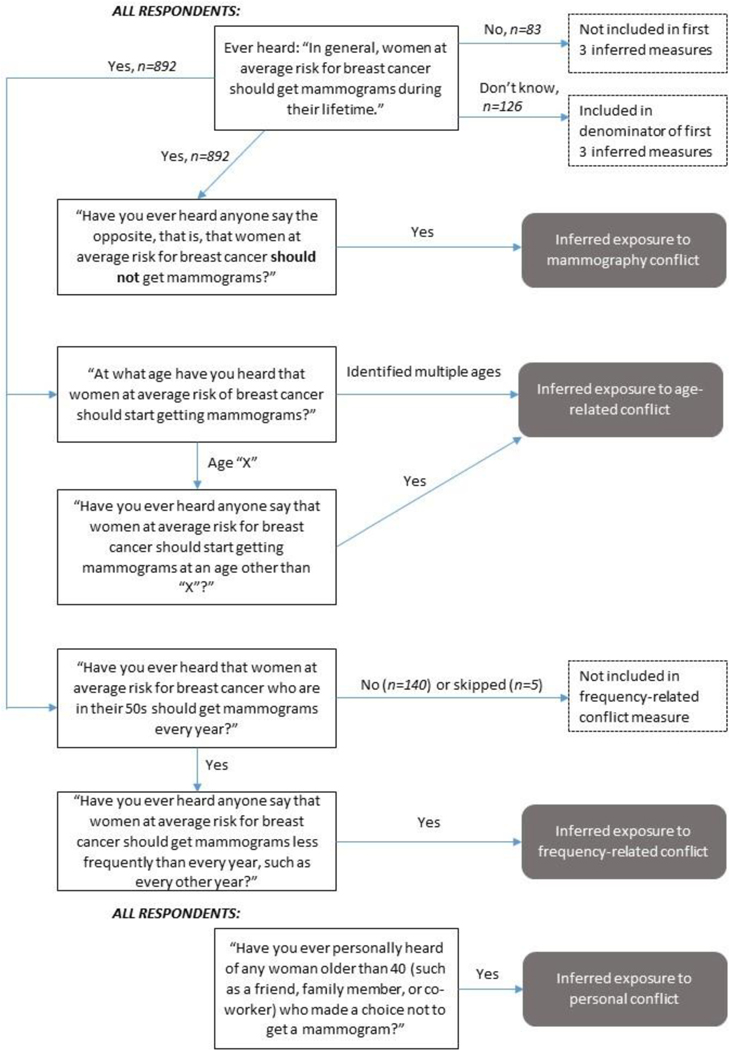
The second (and next-least-obtrusive) set of exposure measures were derived from a series of seven survey items asking respondents about what they had heard about mammograms (see Figure 1 for a flow chart), tapping into concepts of decisional conflict (to get a mammogram or not) and informational conflict (differences in age of initiation and frequency in recommendations). First, respondents were asked whether they had ever heard the statement: “In general, women at average risk for breast cancer should get mammograms during their lifetime.” Participants who answered “yes” (n = 892) were then asked “Have you ever heard anyone say the opposite, that is, that women at average risk for breast cancer should not get mammograms?” Respondents who answered “yes” to the first item and yes to this second item were classified as 1 in a dichotomous inferred exposure to mammography conflict measure. Then, also among only those who had heard of getting mammograms (n=892), we asked: “At what age have you heard that women at average risk for breast cancer should start getting mammograms?” The responses were check all that apply, and included “age 35”, “age 40”, “age 45”, “age 50”, “some other age” (that they could write in)”, or “not sure”. Any respondent who indicated more than one age was classified affirmatively in a dichotomous inferred exposure to age-related conflict measure, in that they noted two logically-conflicting ages at which women should start screening. Next, respondents who selected a single age were asked, “Have you ever heard anyone say that women at average risk for breast cancer should start getting mammograms at an age other than [the age they noted in the previous item]?” Any respondent who answered “yes” to this item was also classified as a yes (or 1) in our inferred exposure to age-related conflict measure (where 0=reporting only one age or reporting “don’t know” on either item). Last, those who indicated they had heard about mammograms (n=892) were asked, “Have you ever heard that women at average risk for breast cancer who are in their 50s should get mammograms every year?” Response options included “yes”, “no”, or “don’t know.” Any respondent who indicated “yes” was then asked, “Have you ever heard anyone say that women at average risk for breast cancer should get mammograms less frequently than every year, such as every other year?” Respondents who answered “yes” to this latter item were classified as affirmative (or 1) in a dichotomous inferred exposure to frequency-related conflict measure (where 0=reporting yes on the first item and no on the second or “don’t know” on either).
Figure 1. Flow Chart of Constructing Inferred Exposure to Mammogram Conflict Measures.
Note. Figure shows the construction of the four inferred conflict measures (in gray boxes with rounded corners) from the seven survey items (in black boxes). Respondents who answered “I don’t know” for either of the age items were included in the denominator of the “inferred exposure to age-related conflict” measure. Respondents who answered “I don’t know” to either of the frequency items were included in the denominator of the “inferred exposure to frequency-related conflict” measure. Respondents who answered “I don’t know” to the personal item were included in the denominator of the “inferred exposure to personal conflict” measure.
For a final inferred measure, all respondents were asked, “Have you ever personally heard of any woman older than 40 (such as a friend, family member or co-worker) who made a choice not to get a mammogram?” Any respondent who answered “yes” to this item (as opposed to “no” or “I don’t know”) was classified affirmatively on a dichotomous inferred exposure to personal conflict measure to capture the respondent’s familiarity with women’s decision making against screening by the age at which women have been historically encouraged to have routine mammograms. This personal dimension is important because the processing of conflicting information may differ when the source of the conflict is personal versus, for instance, scientific evidence (Carpenter et al., 2016). While we classify these inferred measures as less obtrusive measures of reported conflict, it is not necessarily the case that women attribute a negative valence to this information.
Thought-Listing Exposure Measures.
The third set of measures require respondents’ more active recognition and perception of conflicting information. Prior to asking respondents any mammography-specific measure, respondents were told: “Now we would like to ask you some questions about mammograms. A mammogram is an X-ray of each breast to check for breast cancer. What, if anything, have you heard recently about mammograms? Please write down the first things that come to mind.” Communication and psychology researchers have used this thought-listing procedure to derive survey respondents’ top-of-head reactions to messages (Cacioppo et al., 1997). Of the 1,113 respondents, 795 (71.4%) completed the thought-listing task by typing something into the open field. Two coders developed a coding scheme to classify responses according to whether or not they referenced recognition of cancer screening and whether or not the responses denoted awareness of changing screening guidelines. Inter-rater reliability of a subset of responses (20% of total) was sufficiently high (all kappas > 0.8), so a single coder coded the remainder of the 795 responses. We coded for five categories of responses: (1) a response that did not provide any content relevant to mammograms; (2) a response that defined mammograms, breast, or cancer but without referencing any information about screening recommendations, conflict, or controversy (e.g., “detect lumps”); (3) a response that exclusively referenced either annual screening or starting at 40 (e.g., “important to get every year”), which we categorized as not referencing changing recommendations; (4) a response that acknowledged new or changing recommendations, suggesting that the respondent was aware that the evidence base or recommendations had been changing (e.g., “isn’t necessary as often as I thought” and “I heard they do more harm than good”); and (5) a response that explicitly referenced conflict or disagreement in screening mammography (i.e., “they can’t decide when to get them”, “I have heard conflicting reports about whether they are helpful or hurtful”).
Self-Assessed Exposure Measure.
Fourth and last, we adapted the most obtrusive exposure measure, self-assessed conflict in media, from a measure validated by Nagler and Hornik (2012) about conflict over nutrition that has since been applied to conflict in multiple public health contexts (e.g., e-cigarettes; Tan et al., 2015). The item explicitly asked respondents to assess “How much conflicting or contradictory information about mammograms have you heard from… Media (e.g., print media, online news media, social media, medical websites, television).” Responses included “none”, “a little”, “some”, and “a lot.” Seventeen respondents skipped this item, so n = 1,096 for this measure.
Dependent Variables: Confusion about and Backlash Toward Mammography, Health Information in General
Following other work on conflicting information about mammography (Nagler, Yzer, et al., 2019), our two main outcome constructs are confusion and backlash. To assess confusion about breast cancer screening recommendations and research, we asked respondents to indicate their agreement with the following statements, adapted from prior work (Nagler, 2014; Nagler, Yzer, et al., 2019): “I find breast cancer screening recommendations to be confusing” (M = 2.81, SD = 0.94) and “Research findings about breast cancer screening seem to be all over the map” (M =3.07, SD = 0.86). To assess backlash toward breast cancer screening recommendations and research, we again adapted two items from prior work: “Breast cancer screening recommendations should be taken with a grain of salt” (M =2.52, SD = 0.97) and “Scientists don’t really know how you should avoid breast cancer” (M =3.05, SD = 0.92). For both confusion and backlash, we analyzed each item separately rather than combining into respective scales given the inter-item correlations (confusion items r = 0.49; backlash items r = 0.36). To measure broader confusion about and backlash toward health information or scientific recommendations more generally (i.e., potential carryover effects), we included two items: “In general, health information is confusing to me” (M =2.82, SD = 0.97) and “Scientists keep changing their minds about what people should do to keep healthy” (M =3.45, SD = 0.98). All of the above responses were measured on agree-disagree Likert scales, where 1=strongly disagree, 2=disagree, 3=neither agree nor disagree, 4=agree, and 5=strongly agree.
Other Characteristics of Respondents
GfK provided us with several demographic characteristics about respondents. These included age (measured as 18–29, 30–39, 40–49, and 50–59), gender, educational attainment (less than high school, high school, some college, or bachelor’s or more), income (in 19 increments from less than $5,000 to $175,000 or more), race (white, black, other), Hispanic/Latino ethnicity, and marital status (see Appendix Table 1).
In addition to demographic characteristics, in order to adjust for possible competing explanations for the relationship between exposure to mammography-related conflict and our dependent variables of interest, we also measured two other characteristics of participants: their average health news consumption and their confidence in institutions. Respondents’ propensity to consume health news was adapted from items included in the Annenberg National Health Communication Survey (ANHCS, 2013) and was measured as an average of responses to three items asking about the frequency with which they consumed three types of health news in the past 30 days: the health sections of print/online news sources or general magazines; print or online magazines or newsletters that have a focus on health issues; and local or national news programs which have segments that focus on health issues. Responses were not at all, less than once per week, about once per week, and a few times a week (range = 1–4). The responses formed an internally consistent scale (Cronbach’s alpha = 0.70; M =1.61, SD = 0.73). Finally, since explicitly acknowledging conflicting information in the information environment may correlate with individuals’ general skepticism or mistrust, we also measured respondents’ level of confidence in societal institutions. We measured this consistent with previous work (Nagler, 2014), which adapted items from the General Social Survey: “How much confidence do you have in each of the following institutions?” The 9 institutions included “business and industry”, “U.S. Congress”, “Schools and the educational system”, “My state health department”, “Health insurance companies”, “the health care system (doctor’s offices, hospitals)”, “the national news media”, “my local TV news”, and “science and scientists.” Responses included No confidence at all, very little confidence, some confidence, a great deal of confidence, and complete confidence (range = 1–5). Items formed an internally consistent scale (Cronbach’s alpha = 0.88; M =2.65, SD = 0.64).
Data Analysis
The first set of analyses consisted of estimating the frequency of the four categories of exposure to mammography conflict, for the full sample and separately for men and women, to assess whether there were differences in exposure given the likely higher salience for female respondents (Carpenter et al., 2016). Next, to assess the associations among our various measures of exposure, we produced a pairwise correlation matrix of all of the exposure measures. To assess the associations between the various sets of exposure measures and the dependent variables of interest, we estimated ordinary least squares regression models of the dependent variables on the exposure measures. We incorporated our exposure measures separately by type to avoid multicollinearity by putting all the various exposure measures in a single model (Eveland et al., 2009). All models included the following control variables: age, gender, educational attainment, income, race, Hispanic ethnicity, marital status, average health news consumption, and institutional confidence. We anticipated that the relationship between exposure to mammography conflict and cognitive responses may differ for men and women, so we also ran all regressions with interaction terms by gender.1 Finally, all results applied the GfK-provided survey weights to adjust for non-response and post-stratification adjustments based on demographic characteristics from the Current Population Survey. We used the survey functions in STATA 13 for all analyses.
Results
Addressing our first stated objective, we found that prevalence of exposure to conflicting information about mammography varied by both type of measure and, in most cases, gender, yet when looking across the four measures, overall we find that participants were exposed to moderate amounts of conflicting information about mammography (Table 1). Just under half of the sample (with no statistically significant differences by gender) reported no self-assessed exposure to conflicting information in the media, while 23.4% reported a little, 22.3% reported some, and 7.5% reported a lot. For the inferred measures, 9.3% of the sample overall was categorized as having inferred exposure to mammography-related conflict (i.e., that they had ever heard that people should not get mammograms), significantly more among women (12.2%) than men (6.0%, p = 0.002). Similarly, 36.8% of the sample was classified as having been exposed to age-related conflicting information, more among women (41.6%) than men (30.8%, p = 0.006). Just over one-quarter (27.3%) were classified as having been exposed to frequency-related conflicting information; again this was more common among women (32.7%) than men (20.6%, p < 0.001). About one-fifth (21.3%) noted that they knew someone personally who was older than 40 and had decided not to get a mammogram, more among women (28.9%) than men (13.5%, p < 0.001).
Table 1.
Prevalence of Exposure to Conflicting Information about Mammography, for Full Sample and by Gender
| Measure (n of measure) | Full sample % (N=1,113) | Women % (N=695) | Men % (N=418) | Difference by gendera |
|---|---|---|---|---|
|
| ||||
| Ecological exposure (mean)b (n = 1,103) | 60.8 | 65.0 | 56.5 | 0.015 |
|
| ||||
| Top-of-head thought-listingc (n = 795) | ||||
| References “old” only | 10.8% | 15.1% | 6.1% | 0.001 |
| References new/change | 23.6% | 29.1% | 17.6% | 0.003 |
| References conflict | 1.1% | 2.0% | 0.2% | 0.001 |
|
| ||||
| Self-assessed exposure to conflict in media (n = 1,096) | ||||
| None | 46.8% | 44.2% | 49.5% | 0.354 |
| A little | 23.4% | 25.5% | 21.1% | |
| Some | 22.3% | 22.2% | 22.4% | |
| A lot | 7.5% | 8.0% | 7.0% | |
|
| ||||
| Inferred exposure | ||||
| Mammography conflict (n = 1,018) | 9.3% | 12.2% | 6.0% | 0.002 |
| Age-related conflict (n = 891) | 36.8% | 41.6% | 30.8% | 0.006 |
| Frequency-related conflict (n = 742) | 27.3% | 32.7% | 20.6% | <0.001 |
| Personal conflict (n = 1,113) | 21.3% | 28.9% | 13.5% | <0.001 |
Based on chi-square or t-tests.
This could range from 0 for the respondent who reported no TV news watching to 414 for the respondent who reported daily TV news watching and living in the news media market with the highest volume of closed-caption keywords related to mammography during this time period.
Given the small number of respondents who explicitly referenced conflict (1.1%, n = 14), this measure is not included in subsequent analyses.
Examining respondents’ top-of-head thought-listing responses, we found that only 1.1% (n = 14) explicitly referenced conflict (i.e., in a negatively-valenced way) in their response. We therefore did not incorporate these responses into the next set of analyses. Nearly one-quarter (23.6%) referenced changing recommendations or new scientific evidence about mammograms, more among women (29.1%) than men (17.6%, p = 0.003) (Table 1). A nontrivial number of respondents commented explicitly about what could be considered the pre-2015 ACS recommendation, that women should be screened annually and starting at 40, with no mention of any change and/or conflict: 10.8% of respondents overall, more among women (15.1%) than men (6.1%, p < 0.001).
Table 2 reports pairwise correlations between the various exposure measures. The ecological measure had the weakest correlations with the other exposure measures, which is consistent with its being the most distal or furthest removed, both in terms of content specificity and level of measurement. The weak to moderate correlations among the remaining categories provide some evidence of convergent validity across measures, while the absence of strong correlations suggests that the measures may be tapping into slightly different dimensions of exposure—consistent with their a priori variation in content specificity, obtrusiveness, and perceived personal salience.
Table 2.
Bivariate Correlations among Exposure Measures
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1. Ecological exposure | 1.00 | |||||||
| 2. Top-of-head thought-listing: References “old” only | .045 | 1.00 | ||||||
| 3. Top-of-head thought-listing: References new/change | .078* | −.213*** | 1.00 | |||||
| 4. Self-assessed exposure to conflict in media | .129*** | −.051 | .388*** | 1.00 | ||||
| 5. Inferred exposure: Mammography conflict | .043 | −.110** | .235*** | .308*** | 1.00 | |||
| 6. Inferred exposure: Age-related conflict | .070* | .017 | .090* | .217*** | .158*** | 1.00 | ||
| 7. Inferred exposure: Frequency-related conflict | −.006 | −.107* | .326*** | .381*** | .260*** | .205*** | 1.00 | |
| 8. Inferred exposure: Personal conflict | .104*** | .019 | .114** | .268*** | .151*** | .130*** | .202*** | 1.00 |
Note.
p<.05;
p<.01;
p<0.001
Next, turning to the second stated research objective, we assessed to what extent these various measures of exposure to conflicting information about mammography were correlated with relevant cognitions, beginning with breast cancer screening-related confusion (Table 3). After accounting for demographic and health media-related characteristics of respondents, the ecological measure of local news exposure to conflicting information was not related to either confusion item. However, respondents classified as having been exposed to overall mammogram conflict or conflict over screening frequency reported higher levels of confusion about both screening recommendations and research findings; those who reported knowing someone personally who chose not to get screened also reported higher levels of finding breast cancer screening recommendations to be confusing. For the top-of-head measures, respondents who noted changed recommendations or new evidence (suggesting this information was particularly salient to their understanding of mammograms) were also more likely to report confusion about recommendations and research, as were respondents who self-reported higher frequency of exposure to conflicting information in the media.
Table 3.
Associations of Exposure to Conflicting Information about Mammography with Breast Cancer Screening-Related Confusion
| I find breast cancer screening recommendations to be confusing |
Research findings about breast cancer screening seem to be all over the map |
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Measure | Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 |
|
| ||||||||
| Ecological exposure | 0.000 | −0.000 | ||||||
| (0.000) | (0.0004) | |||||||
| Top-of-head thought-listing | ||||||||
| References “old” only | −0.191^ | 0.020 | ||||||
| (0.107) | (0.102) | |||||||
| References new/change | 0.495*** | 0.351*** | ||||||
| (0.099) | (0.092) | |||||||
| Self-assessed exposure to conflict in media | 0.280*** (0.035) |
0.226*** (0.032) |
||||||
| Inferred exposure | ||||||||
| Mammography conflict | 0.331* | 0.298* | ||||||
| (0.146) | (0.130) | |||||||
| Age-related conflict | −0.058 | 0.049 | ||||||
| (0.081) | (0.072) | |||||||
| Frequency-related conflict | 0.260** | 0.186* | ||||||
| (0.094) | (0.088) | |||||||
| Personal conflict | 0.215* | 0.137 | ||||||
| (0.092) | (0.084) | |||||||
|
| ||||||||
| Observations | 1,059 | 718 | 774 | 1,058 | 1,060 | 719 | 773 | 1,059 |
|
| ||||||||
| R-squared | 0.021 | 0.079 | 0.083 | 0.094 | 0.057 | 0.102 | 0.105 | 0.114 |
| . | ||||||||
Note. Robust standard errors in parentheses;
p<0.001
p < 0.01
p < 0.05
p < 0.1. For each outcome, we generated four models, one for each of the four types of exposure measurement, to avoid multicollinearity (1=ecological, 2=inferred, 3=top-of-head, 4=self-assessed). All models control for age category, gender, educational attainment, income, race, marital status, average health news consumption, and institutional confidence.
The relationships between exposure to conflicting information and breast cancer screening-related backlash (Table 4) are mostly similar to the results for confusion, but with a few small differences. The ecological measure of local news exposure to information about conflict was associated with lower agreement that “breast cancer screening recommendations should be taken with a grain of salt,” but was not linked to agreement that “scientists don’t know how you should avoid breast cancer.” For the inferred conflict exposure measures, individuals classified as having been exposed to overall mammography conflict or conflict over screening frequency reported more agreement that “breast cancer screening recommendations should be taken with a grain of salt,” while only the inferred exposure to conflict over screening frequency was associated with more agreement that “scientists don’t know how you should avoid breast cancer.” Respondents who volunteered information about changed recommendations or new evidence when asked to reflect on mammograms reported more agreement that “breast cancer screening recommendations should be taken with a grain of salt.” Finally, consistent with the confusion outcomes, respondents who self-reported higher frequency of exposure to conflicting information in the media were more likely to report backlash responses.
Table 4.
Associations of Exposure to Conflicting Information about Mammography with Breast Cancer Screening-Related Backlash
| Breast cancer screening recommendations should be taken with a grain of salt | Scientists really don’t know how you should avoid breast cancer | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Measure | Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 |
|
| ||||||||
| Ecological exposure | −0.001* | −0.000 | ||||||
| (0.0004) | (0.001) | |||||||
| Top-of-head thought-listing | ||||||||
| References “old” only | −0.193 | −0.194^ | ||||||
| (0.117) | (0.101) | |||||||
| References new/change | 0.264* | 0.077 | ||||||
| (0.108) | (0.100) | |||||||
| Self-assessed exposure to conflict in media | 0.157*** (0.041) |
0.123** (0.038) |
||||||
| Inferred exposure | ||||||||
| Mammography conflict | 0.312* | 0.033 | ||||||
| (0.157) | (0.138) | |||||||
| Age-related conflict | 0.003 | −0.015 | ||||||
| (0.089) | (0.084) | |||||||
| Frequency-related conflict | 0.226* | 0.268** | ||||||
| (0.109) | (0.097) | |||||||
| Personal conflict | 0.171^ | 0.140 | ||||||
| (0.103) | (0.089) | |||||||
|
| ||||||||
| Observations | 1,060 | 720 | 773 | 1,059 | 1,058 | 719 | 771 | 1,057 |
|
| ||||||||
| R-squared | 0.034 | 0.080 | 0.067 | 0.051 | 0.027 | 0.084 | 0.070 | 0.042 |
Note. Robust standard errors in parentheses;
p<0.001
p < 0.01
p < 0.05
p < 0.1. For each outcome, we generated four models, one for each of the four types of exposure measurement, to avoid multicollinearity (1=ecological, 2=inferred, 3=top-of-head, 4=self-assessed). All models control for age category, gender, educational attainment, income, race, marital status, average health news consumption, and institutional confidence.
The last set of regression results examined whether any of the measures of exposure to conflicting information about mammography were related to cognitions beyond breast cancer screening: general health information confusion and general backlash to scientists’ advice about health. Table 5 demonstrates that none of the measures of exposure to conflicting information about mammography were associated with the general health confusion item. However, at least one of the measures from each of the four categories of exposure was associated with the general backlash item (“Scientists keep changing their minds about what people should to keep healthy”). Specifically, higher levels of exposure to conflict measured as the keyword hits in respondents’ media environment, inferred exposure to conflicting information about mammogram frequency, knowing someone who decided not to get screened, noting changed recommendations or new evidence, and self-reporting higher levels of conflicting information in the media were each associated with more agreement that scientists keep changing their minds about what people should do to keep healthy. In contrast, respondents classified as having been exposed to information about conflicting ages of mammography screening reported lower agreement with this general backlash measure.
Table 5.
Associations of Exposure to Conflicting Information about Mammography with General Health Information Confusion and Backlash
| In general, health information is confusing to me | Scientists keep changing their minds about what people should do to keep healthy | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Measure | Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 |
|
| ||||||||
| Ecological exposure | −0.000 | 0.001* | ||||||
| (0.001) | (0.0004) | |||||||
| Top-of-head thought-listing | ||||||||
| References “old” only | −0.040 | −0.011 | ||||||
| (0.113) | (0.138) | |||||||
| References new/change | 0.115 | 0.246* | ||||||
| (0.099) | (0.095) | |||||||
| Self-assessed exposure to conflict in media | 0.075^ (0.040) |
0.189*** (0.037) |
||||||
| Inferred exposure | ||||||||
| Mammography conflict | 0.192 | 0.103 | ||||||
| (0.136) | (0.129) | |||||||
| Age-related conflict | −0.139^ | −0.197* | ||||||
| (0.084) | (0.083) | |||||||
| Frequency-related conflict | −0.024 | 0.199* | ||||||
| (0.101) | (0.101) | |||||||
| Personal conflict | −0.062 | 0.208* | ||||||
| (0.085) | (0.088) | |||||||
|
| ||||||||
| Observations | 1,059 | 719 | 774 | 1,058 | 1,059 | 720 | 775 | 1,059 |
|
| ||||||||
| R-squared | 0.038 | 0.073 | 0.062 | 0.042 | 0.037 | 0.088 | 0.071 | 0.063 |
Note. Robust standard errors in parentheses;
p<0.001
p < 0.01
p < 0.05
p < 0.1. For each outcome, we generated four models, one for each of the four types of exposure measurement, to avoid multicollinearity (1=ecological, 2=inferred, 3=top-of-head, 4=self-assessed). All models control for age category, gender, educational attainment, income, race, marital status, average health news consumption, and institutional confidence
We estimated regression models with interactions between each of the exposure measures and gender to assess whether exposure to conflicting information about mammography had a different relationship to the outcomes for men and women. These models yielded only a single statistically significant interaction term (out of 42 tests estimated), signaling that the relationships between exposure and outcomes are substantively similar for men and for women.2
Discussion
The objectives of this study were to assess the prevalence of public exposure to conflicting information about mammography among men and women through multiple measures and to assess whether exposure was related to potentially important cognitive responses identified in past research—confusion about breast cancer screening recommendations and research, backlash toward such recommendations and research, and confusion about and backlash toward health information in general. We deployed multiple measures of conflict that vary in their obtrusiveness (how direct or indirect is the measurement, including an ecological measure, inferred measures, and a direct self-report), content specificity (how specific they are to the context of mammography conflict), and the perceived personal salience (whether respondents themselves nominate conflicting or changed recommendations as something they associate with mammograms). Considered collectively, we found moderate levels of exposure to conflicting information about mammography across measurement type. Women measured higher in exposure across all but the self-assessed measure. Interestingly, almost 30% of women identified someone in their personal networks older than 40 years old who had made a choice not to get a mammogram. Overall, these estimates represent a substantial number of Americans who have been exposed to information about the changing recommendations regarding the utility, frequency, and age of initiation of mammograms.
We found that all of the measures except the ecological measure were related to self-reported confusion about mammography screening, with higher exposure to conflicting information related to more agreement that breast cancer screening recommendations or research findings are “confusing” or “all over the map.” It is perhaps not surprising that the ecological measure was not related to confusion because it measured plausible exposure to the volume of local TV news coverage of mammograms (but not whether a respondent actually received it), and not the content of this exposure per se. Although we know from previous work that half of the TV news coverage aired around this time period in early 2016 actually referenced conflict (Nagler, Fowler, et al. 2019), actual content would vary across media markets, and so we are unable to determine the specific content to which a specific respondent would have been exposed. While the remaining measures point toward a robust relationship between exposure to conflicting information and confusion, it is important to consider that confusion in this particular context of breast cancer screening may not be normatively problematic. Given that both the USPSTF and the ACS recommendations invite women to have a personalized discussion with their health care providers, the feeling of being confused may prompt women to engage more deliberatively in a discussion of whether or not to get a mammogram or to seek more information (see, e.g., Shi et al., 2021), rather than operating only on the long-held heuristic that women should get screened every year after they turn 40.
The relationship between exposure to conflicting information and perception of backlash to screening recommendations or scientific advice, however, is potentially a more normatively concerning finding. We found robust evidence—although slightly less uniform than the confusion findings—that exposure to conflict (across multiple measures) was related to more breast cancer screening-related backlash. The ecological measure was the only one that differed from the pattern, as higher exposure to local TV news coverage was associated with less breast cancer recommendation-related backlash for one item and had no relationship with backlash for the other item.
Finally, we found that exposure to conflicting information about breast cancer screening was consistently related to the perception that scientists keep “changing their minds” about general health guidance, but was not related to respondents’ perception of general confusion about health information. This suggests that conflicting information about mammograms in the public discourse could carry over to influence the public’s general cognitions about science-based guidelines, thus adding to the growing literature documenting the potential for carryover effects (Lee et al., 2018; Nagler, 2014; Nagler, Yzer, et al., 2019; Yang et al., 2020). Other research demonstrates that the public is already somewhat skeptical about the value of evidence-based guidelines (Gerber et al., 2010), and that they are even less trusting when they believe that the government is behind research-based guidelines (Lantz et al., 2016). Future research should assess whether cumulative exposure to conflicting health information about scientific evidence, could undermine public trust in health recommendations and, in turn, potentially decrease receptivity to public health messaging even on topics for which evidence is non-conflicting.
It is important to interpret these key findings with some limitations in mind. First, given the cross-sectional survey design, these findings cannot be used to draw conclusions that exposure to conflict is causally related to confusion or backlash. Except for the ecological measure, the exposure items and the outcome items were contemporaneously measured on the cross-sectional survey. This means that, for example, the questions earlier in the survey may have primed respondents to report more confusion later, or that some underlying construct related to both confusion and exposure explains the relationship (i.e., omitted variable bias). We attempted to guard against this by including a range of more and less obtrusively measured exposure measures. We also controlled for a robust set of individual characteristics, including respondents’ age, education level, health media exposure, and trust in institutions. Future research, using experimental methods or longitudinal study designs, should be conducted to examine whether exposure to conflicting information is causally related to domain-specific cognitive outcomes that may carry over into other health-related attitudes and behaviors. Second, survey space constraints limited the number of items we could use to assess our outcomes of interest. Future studies that develop and validate multi-item scales to capture cognitive outcomes such as confusion and backlash are needed (e.g., Jensen et al., 2020). Third, our study does not answer the question of which measure is “best”, as a comparative validity study might. We recommend more work be undertaken on measurement of exposure to conflict—given the continuing persistence of conflict in the information environment (see, e.g., Nagler et al., 2020)—and, particularly, to assess whether there are meaningful differences across different conceptualizations of conflict, like decisional versus informational conflict. Last, reactions to conflicting information related to mammograms may vary not only by gender (as tested here) but also by age or other characteristics, like health literacy or socioeconomic position; these are all important objectives for future research.
Using multiple and varied measurement approaches informed by research on media exposure measurement (Nagler, 2017; Niederdeppe, 2014), this study provides the first nationally representative estimates of public exposure to mammography-related conflict. Overall, we find substantial reports of exposure to conflicting information about mammography, as well as generally consistent results linking such exposure with two cognitive responses, confusion about and backlash toward breast cancer screening. These observational findings corroborate recent experimental evidence documenting undesirable effects of exposure to conflicting information about mammography (Nagler, Yzer, et al., 2019). Results also suggest that exposure to conflict could carry over to shape the public’s perceptions of science-based health guidance more generally—a particularly concerning finding, given evidence that the public is exposed to conflicting information across a range of health topics, including nutrition (Lee et al., 2018; Nagler, 2014), medications (Carpenter et al., 2014; Hameen-Anttila et al., 2014), e-cigarettes (Tan et al., 2015), and, most recently, COVID-19 (Nagler et al., 2020). Future research that considers how such exposure could compound across topics to produce negative cognitive and behavioral effects, as well as how such impacts could be mitigated, is warranted.
Acknowledgments
We thank Kari Mentzer for her work coding responses to the thought-listing exercise, Laura Baum for project support, and Jiani Yu on data management support during the early phase of this project. We also thank Karla Kerlikowske, Skip Lupia, Gary Schwitzer, Jonathan Slater, and Beth Virnig for their contributions to survey design. This work was supported by a Research Scholar Grant, RSG-14-166-01-CPPB, from the American Cancer Society (P.I.: S.E.G.). Additional support was provided by a grant from the National Cancer Institute (5R21CA218054-02; PI: RHN). This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
In other work both by this team (Nagler, Fowler and Gollust 2017) and others (Abelson et al., 2018), mammogram history has emerged as an important factor predicting attitudes about mammograms. As an exploratory analysis and to be consistent with this other work, we estimated models restricting to women in which we added mammogram history as a covariate and an interaction term with exposure. We report on these exploratory findings as a note in Results.
We also estimated models restricted to women only within the age group for whom we asked about their own mammogram status (women aged 30–59, n = 554). These models allowed us to ascertain whether women who routinely get mammograms (64.9% in this subsample) have a different response to exposure to conflict than those who do not, by estimating interaction terms between each of the exposure measures and mammogram screening status. The results are suggestive that exposure to conflict may have a different association with backlash for women who get an annual mammogram, with statistically significant interaction terms for two of the measures of conflict on the “scientists don’t know how you should avoid breast cancer” and “scientists keep changing their minds about what people should do to keep healthy” items. However, these are exploratory analyses, and we were not powered to assess interaction terms by screening behavior for women only. Future research should explore whether mammogram-related conflicting information differs in its effects on women based on their screening behaviors.
We have no conflicts of interest to disclose.
Contributor Information
Sarah E. Gollust, Division of Health Policy and Management, University of Minnesota School of Public Health
Erika Franklin Fowler, Department of Government, Wesleyan University.
Rebekah H. Nagler, Hubbard School of Journalism and Mass Communication, University of Minnesota
References
- Abelson J, Tripp L, Brouwers MC, Pond G, & Sussman J. (2018). Uncertain times: A survey of Canadian women’s perspectives toward mammography screening. Preventive Medicine, 112, 209–215. 10.1016/j.ypmed.2018.04.021 [DOI] [PubMed] [Google Scholar]
- ANHCS. (2013). Annenberg National Health Communication Survey (ANHCS) 2005–2012 dataset. http://anhcs.asc.upenn.edu. [DOI] [PubMed]
- Cacioppo JT, von Hippel W, & Ernst JM (1997). Mapping cognitive structures and processes through verbal content: The thought-listing technique. Journal of Consulting and Clinical Psychology, 65(6), 928–940. 10.1037//0022-006x.65.6.928 [DOI] [PubMed] [Google Scholar]
- Carpenter DM, Elstad EA, Blalock SJ, & DeVellis RF (2014). Conflicting medication information: Prevalence, sources, and relationship to medication adherence. Journal of Health Communication, 19(1), 67–81. 10.1080/10810730.2013.798380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter DM, Geryk LL, Chen AT, Nagler RH, Dieckmann NF, & Han PK (2016). Conflicting health information: A critical research need. Health Expectations, 19(6), 1173–1182. 10.1111/hex.12438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2020). What Is Breast Cancer Screening? https://www.cdc.gov/cancer/breast/basic_info/screening.htm. [Google Scholar]
- Chang C. (2015). Motivated processing: How people perceive news covering novel or contradictory health research findings. Science Communication, 37(5), 602–634. 10.1177/1075547015597914 [DOI] [Google Scholar]
- Chong D. (2019). Competitive framing in political decision making. Oxford Research Encyclopedia of Politics. 10.1093/acrefore/9780190228637.013.964 [DOI] [Google Scholar]
- Clark D, Nagler RH, & Niederdeppe J. (2019). Confusion and nutritional backlash from news media exposure to contradictory information about carbohydrates and dietary fats. Public Health Nutrition, 22(18), 3336–3348. 10.1017/S1368980019002866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeAngelis CD, & Fontanarosa PB (2010). US Preventive Services Task Force and breast cancer screening. Journal of the American Medical Association, 303(2), 172–173. 10.1001/jama.2009.1990 [DOI] [PubMed] [Google Scholar]
- Dixon GN, & Clarke CE (2012). Heightening uncertainty around certain science: Media coverage, false balance, and the autism-vaccine controversy. Science Communication, 35(3), 358–382. 10.1177/1075547012458290 [DOI] [Google Scholar]
- Ellsberg D. (1961). Risk, ambiguity, and the savage axioms. The Quarterly Journal of Economics, 75(4), 643–669. http://qje.oxfordjournals.org/content/75/4/643.abstract [Google Scholar]
- Eveland WP, Hutchens MJ, & Shen F. (2009). Exposure, attention, or “use” of news? Assessing aspects of the reliability and validity of a central concept in political communication research. Communication Methods and Measures, 3(4), 223–244. 10.1080/19312450903378925 [DOI] [Google Scholar]
- Gans HJ (1979). Deciding What’s News. Northwestern University Press. [Google Scholar]
- Gerber AS, Patashnik EM, Doherty D, & Dowling C. (2010). A national survey reveals public skepticism about research-based treatment guidelines. Health Affairs, 29(10), 1882–1884. 10.1377/hlthaff.2010.0185 [DOI] [PubMed] [Google Scholar]
- Gollust SE, Nagler RH, & Fowler EF (2020). The emergence of COVID-19 in the U.S.: A public health and political communication crisis. Journal of Health Politics, Policy and Law, 45(6), 303–314. 10.1215/03616878-8641506 [DOI] [PubMed] [Google Scholar]
- Han PK, Kobrin SC, Klein WM, Davis WW, Stefanek M, & Taplin SH (2007). Perceived ambiguity about screening mammography recommendations: Association with future mammography uptake and perceptions. Cancer Epidemiology, Biomarkers, and Prevention, 16(3), 458–466. 10.1158/1055-9965.epi-06-0533 [DOI] [PubMed] [Google Scholar]
- Han PK, Moser RP, & Klein WM (2007). Perceived ambiguity about cancer prevention recommendations: Associations with cancer-related perceptions and behaviours in a US population survey. Health Expectations, 10(4), 321–336. 10.1111/j.1369-7625.2007.00456.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson M, & Kadiyala S. (2017). When guidelines conflict: A case study of mammography screening initiation in the 1990s. Womens Health Issues, 27(6), 692–699. 10.1016/j.whi.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen JD, & Hurley RJ (2012). Conflicting stories about public scientific controversies: Effects of news convergence and divergence on scientists’ credibility. Public Understanding of Science, 21(6), 689–704. 10.1177/0963662510387759 [DOI] [PubMed] [Google Scholar]
- Jensen JD, Giorgi EA, Jackson JR, Berger J, Katz RA, & Mobley AR (2020). Revisiting nutrition backlash: Psychometric properties and discriminant validity of the nutrition backlash scale. Nutrition, 78, 110949. 10.1016/j.nut.2020.110949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi MT, & Hay JL (2012). Awareness of the 2009 US Preventive Services Task Force recommended changes in mammography screening guidelines, accuracy of awareness, sources of knowledge about recommendations, and attitudes about updated screening guidelines in women ages 40–49 and 50+. BMC Public Health, 12, 899. 10.1186/1471-2458-12-899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz PM, Evans WD, Mead H, Alvarez C, & Stewart L. (2016). Knowledge of and attitudes toward evidence-based guidelines for and against clinical preventive services: Results from a national survey. The Milbank Quarterly, 94(1), 51–76. 10.1111/1468-0009.12181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CJ, Nagler RH, & Wang N. (2018). Source-specific exposure to contradictory nutrition information: Documenting prevalence and effects on adverse cognitive and behavioral outcomes. Health Communication, 33(4), 453–461. 10.1080/10410236.2016.1278495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran MB, Frank LB, Zhao N, Gonzalez C, Thainiyom P, Murphy ST, & Ball-Rokeach SJ (2016). An argument for ecological research and intervention in health communication. Journal of Health Communication, 21(2), 135–138. 10.1080/10810730.2015.1128021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH (2014). Adverse outcomes associated with media exposure to contradictory nutrition messages. Journal of Health Communication, 19(1), 24–40. 10.1080/10810730.2013.798384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH (2017). Measurement of media exposure. In Matthes J, Davis CS, & Potter RF (Eds.), The International Encyclopedia of Communication Research Methods; (pp. 1–21). 10.1002/9781118901731.iecrm0144 [DOI] [Google Scholar]
- Nagler RH, Fowler EF, & Gollust SE (2017). Women’s awareness and responses to messages about breast cancer overdiagnosis and overtreatment: Results from a 2016 national survey. Medical Care, 55(10), 879–885. 10.1097/MLR.0000000000000798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, Fowler EF, Marino NM, Mentzer KM, & Gollust SE (2019). The evolution of mammography controversy in the news media: A content analysis of four publicized screening recommendations, 2009 to 2016. Womens Health Issues, 29(1), 87–95. 10.1016/j.whi.2018.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, & Hornik RC (2012). Measuring media exposure to contradictory health information: A comparative analysis of four potential measures. Communication Methods and Measures, 6(1), 56–75. 10.1080/19312458.2011.651348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, & LoRusso SM (2018). Conflicting information and message competition in health and risk messaging. In Parrott R. (Ed.), The Oxford encyclopedia of health and risk message design and processing (pp. 353–372). Oxford University Press. 10.1093/acrefore/9780190228613.013.292 [DOI] [Google Scholar]
- Nagler RH, Vogel RI, Gollust SE, Rothman AJ, Fowler EF, & Yzer MC (2020). Public perceptions of conflicting information surrounding COVID-19: Results from a nationally representative survey of U.S. adults. PLoS One, 15(10), e0240776. 10.1371/journal.pone.0240776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, Yzer MC, & Rothman AJ (2019). Effects of media exposure to conflicting information about mammography: Results from a population-based survey experiment. Annals of Behavioral Medicine, 53(10), 896–908. 10.1093/abm/kay098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute (n.d.). Cancer Stat Facts: Female Breast Cancer. Retrieved April 5, 2021, from: https://seer.cancer.gov/statfacts/html/breast.html.
- Niederdeppe J. (2014). Conceptual, empirical, and practical issues in developing valid measures of public communication campaign exposure. Communication Methods and Measures, 8(2), 138–161. 10.1080/19312458.2014.903391 [DOI] [Google Scholar]
- Niederdeppe J, Gollust SE, & Barry CL (2014). Inoculation in competitive framing: Examining message effects on policy preferences. Public Opinion Quarterly, 78(3), 634–655. http://poq.oxfordjournals.org/content/78/3/634.abstract [Google Scholar]
- Patterson RE, Satia JA, Kristal AR, Neuhouser ML, & Drewnowski A. (2001). Is there a consumer backlash against the diet and health message? Journal of the American Dietetic Association, 101(1), 37–41. 10.1016/s0002-8223(01)00010-4 [DOI] [PubMed] [Google Scholar]
- Shi W, Nagler RH, Fowler EF, & Gollust SE (2021). Predictors of women’s awareness of the benefits and harms of mammography screening and associations with confusion, ambivalence, and information seeking. Health Communication, 36(3), 303–314. 10.1080/10410236.2019.1687129 [DOI] [PubMed] [Google Scholar]
- Squiers LB, Holden DJ, Dolina SE, Kim AE, Bann CM, & Renaud JM (2011). The public’s response to the US Preventive Services Task Force’s 2009 recommendations on mammography screening. American Journal of Preventive Medicine, 40(5), 497–504. 10.1016/j.amepre.2010.12.027 [DOI] [PubMed] [Google Scholar]
- Tan AS, Lee CJ, & Bigman CA (2015). Public support for selected e-cigarette regulations and associations with overall information exposure and contradictory information exposure about e-cigarettes: Findings from a national survey of U.S. adults. Preventive Medicine, 81, 268–274. 10.1016/j.ypmed.2015.09.009 [DOI] [PubMed] [Google Scholar]
- Yang Q, Herbert N, Yang S, Alber J, Ophir Y, & Cappella JN (2020). The role of information avoidance in managing uncertainty from conflicting recommendations about electronic cigarettes. Communication Monographs, 1–23. 10.1080/03637751.2020.1809685 [DOI] [PMC free article] [PubMed] [Google Scholar]