Abstract
We report on a patient who developed Legionella pneumonia after bone marrow transplantation. Despite appropriate antibiotic treatment, disease progressed. The patient developed a lung abscess from which Legionella and Prevotella were isolated. Cure was achieved by surgical resection. The resected material was sterile, but 16S ribosomal DNA analysis revealed Legionella DNA.
CASE REPORT
A 45-year-old male was admitted to the Department of Hematology, University Hospital Mainz, due to a low-grade fever (38.5°C) and an abnormal chest radiograph demonstrating infiltrates in the right lower and middle lobes accompanied by a small pleural effusion. The patient did not complain of cough. A bronchoalveolar lavage (BAL) was performed and yielded Legionella pneumophila serotype 1 and also 1,000 bacteria/ml belonging to the local oral flora and one colony of Aspergillus. Urine tested positive for Legionella antigen. Ten months prior to admission, the patient had been diagnosed with chronic myelogenous leukemia, and 4 months later he received a matched related bone marrow transplantation. After bone marrow transplantation, he developed acute grade II graft-versus-host disease of the skin and acute grade III graft-versus-host disease of the liver, which were controlled by cyclosporin A and steroids. After the diagnosis of Legionella pneumonia was established, the patient received ciprofloxacin (400 mg twice a day) and rifampicin (600 mg/day) for 2.5 weeks intravenously. The source of Legionella infection could not be determined. Water samples taken from the patient's home were negative for Legionella. Aspergillus could be demonstrated in only one BAL but not in repeated sputum cultures. However, the patient was started on itraconazole (400 mg/day). Control chest radiographs did not show progression during intravenous antibiotic therapy for Legionella. Ciprofloxacin was changed to clarithromycin because the patient had developed severe central nervous system adverse effects. He was discharged on oral rifampicin (600 mg/day) and clarithromycin (500 mg/day) for 4 weeks. A follow-up chest radiograph revealed consolidation, with a central abscess formation with a diameter of 3.5 cm. The patient was readmitted, and a BAL was performed which revealed polymorphonuclear neutrophils and less than 10,000 gram-positive bacteria/ml belonging to the physiological oral flora. Purulent material was obtained from the lung abscess by a computed tomography (CT)-guided aspirate (Fig. 1). Additionally, a biopsy of the abscess wall was performed. A Prevotella species was cultured from the purulent material, and the biopsy yielded Legionella pneumophila serogroup 1. Urine tested positive for Legionella antigen. On admission, Aspergillus was suspected to cause the abscess formation, and amphotericin (80 mg/day) was started empirically. In order to effectively treat the infection with the Prevotella and Legionella species, the patient received imipenem (0.5 g three times a day), rifampicin (600 mg/day), and roxythromycin (300 mg/day). Twelve days after initiation of therapy, the patient developed a large pleural effusion, and CT scans verified the persistence of the cavitation (size, 4 by 5 cm), accompanied by a pleural effusion (Fig. 2). Therapy was continued for 2 weeks. Due to an allergic skin reaction, imipenem was replaced by clindamycin (600 mg four times a day) and aztreonam (1 g three times a day). At this point in time, the patient complained of increasing thoracic pain. The C-reactive protein increased from 98 to 264 mg/liter, though the patient did not develop fever. He underwent thoracic surgery, and the entire middle and parts of the upper and lower lung lobes were resected. The patient recovered quickly without any signs of infection. In addition, the C-reactive protein decreased. The histopathological examination did not demonstrate any fungal hyphae in the lung tissue, and amphotericin was discontinued. Treatment with clindamycin, azactam, and rifampin was continued for another 2 weeks, and the patient was discharged in good condition.
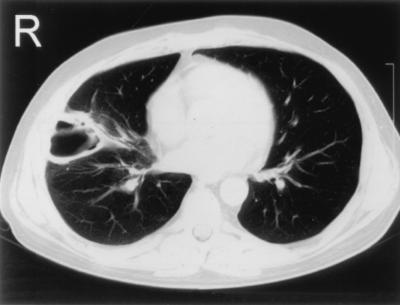
FIG. 1.
Chest CT scan demonstrating a large cavitation in the middle lobe of 4 by 5 cm.
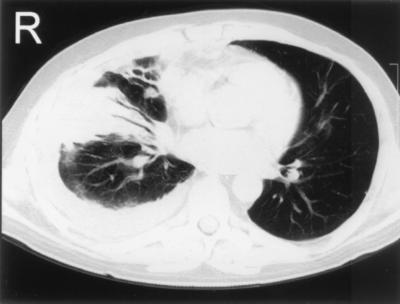
FIG. 2.
Chest CT scan showing a newly developed pleural effusion with a maximal dorsobasal extension of 2.5 cm. The cavitation is filled with parts of the pleural effusion.
Repeated sampling of the pleural effusion revealed no bacterial or fungal growth. Lung tissue and abscess material were also submitted for microbial diagnostics. Direct smears from the lung tissue demonstrated very thin gram-negative bacilli. Direct immunofluorescence for Legionella was negative. Aerobic cultures were performed on blood, cystine-lactose-electrolyte-deficient agar, and Sabouraud agar. Schaedler agar and thioglycolate broth were used for anaerobic cultures, and buffered charcoal-yeast extract agar cultures with and without antibiotics were performed for 10 days in order to recover Legionella. All cultures remained sterile. Genomic DNA was directly extracted from two different lung tissue specimens. 16S ribosomal DNA (rDNA) amplification and sequencing of amplification products were performed as described previously (4, 5). The first 634 bp of PCR products were sequenced, and identical 16S rDNA sequences were obtained from the two specimens. They were submitted to GenBank, and a similarity search using the BLAST program indicated a very close relationship (99% identity) to the DNA sequence of Legionella pneumophila (1).
Legionella pneumophila ranks among the three most common microbial pathogens involved in community-acquired pneumonia. Cell-mediated immunity represents the primary host defense against Legionella. Thus, Legionnaires' disease is more common and more severe in patients with depressed cell-mediated immunity, including transplant recipients, patients with AIDS, or those with drug-induced immunosuppression (8). Here we report the case of a persistent (12 weeks) Legionella infection that was refractory to treatment with conventional antibiotics.
Concomitant infection with different pulmonary or systemic pathogens may occur in Legionella pneumonia (2, 6). Abscess formation, however, has generally been regarded as a complication of monoinfection with Legionella, particularly in immunocompromised hosts (3, 7). To our knowledge, this represents the first documented case of abscess formation associated with Legionella pneumonia and accompanying Prevotella infection. Prevotella species represent an anaerobic bacterium that is mainly found in the oral cavity and ranks among the pathogens that are most frequently isolated from lung abscesses. We suspect that superinfection with this agent played a pivotal role in abscess formation in our patient.
Interestingly in this case, the patient had not been critically ill, though the abscess formation did not resolve under appropriate antibiotic therapy. Presumably, therapeutic levels of the antibiotics were not reached in the cavitation tissue. Surgery, which is not a generally recommended measure to treat lung abscesses, led to control of the infection in this case.
Antibiotic treatment probably rendered the specimens culture negative, but bacterial identification could successfully be undertaken by the direct 16S rDNA sequencing of amplification products from clinical material. The fact that only Legionella DNA could be amplified from lung tissue supports the notion that persistence of infection was due exclusively to Legionella pneumophila and not to the Prevotella superinfection.
In summary, these observations indicate that Legionella infection may persist despite appropriate treatment in immunocompromised patients and that clinical presentations may be quite benign. Lung abscess formation occurring during Legionella infection may be indicative of coinfection with other bacterial agents. When treatment with antibiotics fails to eradicate the pathogen, surgery may become an important therapeutic option. Demonstration of persistent Legionella infection may require noncultural methods like the use of 16S rDNA analysis. Thus, application of this molecular technique appears appropriate when pathological findings persist in the face of negative bacterial cultures.
Acknowledgments
We thank S. Bhakdi for helpful discussions and support.
REFERENCES
- 1.Altschul S F, Gish W, Miller W, Myers E W, Lipmann D J. Basic local alignment search tool. J Mol Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 2.Edelstein P H. Legionnaires' disease. Clin Infect Dis. 1993;16:741–749. doi: 10.1093/clind/16.6.741. [DOI] [PubMed] [Google Scholar]
- 3.Edelstein P H, Meyer R D, Finegold S M. Long-term followup of two patients with pulmonary cavitation caused by Legionella pneumophila. Am Rev Respir Dis. 1981;124:90–93. doi: 10.1164/arrd.1981.124.1.90. [DOI] [PubMed] [Google Scholar]
- 4.Edwards U, Rogall T, Blöcker H, Emde M, Böttger E C. Isolation and direct complete nucleotide determination of entire genes. Characterization of a gene coding for 16S ribosomal RNA. Nucleic Acids Res. 1989;17:7843–7853. doi: 10.1093/nar/17.19.7843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han S-R, Schindel C, Genitsariotis R, Märker-Hermann E, Bhakdi S, Maeurer M J. Identification of a unique Helicobacter species by 16S rRNA gene analysis in an abdominal abscess from a patient with X-linked hypogammaglobulinemia. J Clin Microbiol. 2000;38:2740–2742. doi: 10.1128/jcm.38.7.2740-2742.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tajuddin M J, Kallay M C, Marin M G, Poe R H. Simultaneous legionellosis and aspergillosis in an immunocompetent patient newly treated with corticosteroids. Chest. 1993;104:1929–1931. doi: 10.1378/chest.104.6.1929. [DOI] [PubMed] [Google Scholar]
- 7.Tkatch L S, Kusne S, Irish W D, Krystofiak S, Wing E. Epidemiology of legionella pneumonia and factors associated with legionella-related mortality at a tertiary care center. Clin Infect Dis. 1998;27:1479–1486. doi: 10.1086/515040. [DOI] [PubMed] [Google Scholar]
- 8.Yu V L. Legionella pneumophila (Legionnaires' disease) In: Mandell G L, Bennett J E, Dolin R, editors. Mandell, Douglas and Bennett's principles and practice of infectious diseases. New York, N.Y: Churchill Livingstone; 1995. pp. 2087–2097. [Google Scholar]