Abstract
Objective:
To evaluate the psychological state of healthcare workers (HCWs) in the field of rehabilitation during the COVID-19 pandemic.
Methods:
Cross-sectional observational study. Sample of 334 HCWs including: nurses, medical doctors, therapists, scientists, and clerical workers working at the IRCCS San Raffaele Roma rehabilitation hospital during the second wave of the COVID-19 pandemic. Anonymous web-based questionnaire included 14-item Resilience Scale, Brief-COPE, Hospital Anxiety Depression Scale, Fear of COVID-19 Scale. Occupational and sociodemographic characteristics.
Results:
High levels of resilience, low levels of anxiety, depression, and fear were observed in the study population; the most frequently used coping strategies in the Brief-COPE were acceptance, planning, and active coping. Specifically, 87% of the participants reported a moderate to high level of resilience, with the highest level observed in nurses while physicians show the lowest level. HCWs showed symptoms of anxiety (29%), depressive symptoms (10%), and fear caused by the COVID-19 pandemic (44%). Statistically significant differences were observed between different occupations for fear (p <0.05) and resilience (p <0.01). Levels of anxiety and fear appeared to be higher in female and younger workers. The latter group - who also reported higher levels of depression - showed lower levels of resilience.
Conclusions:
In our study hospital and non-hospital workers show different emotional, cognitive, and behavioural resources when facing stressful situations, like in the case of the SARS-CoV-2 pandemics. Our results support the role of resilience and the proper use of problem-focused and emotion-focused coping strategies as protective factors from psychological distress.
Keywords: COVID-19, coping strategies, resilience, anxiety, depression, HCW
Background
The COVID-19 pandemic is still having a profound effect, not only on the physical health of the population but also on several aspects of society, including mental health (1). The climate of uncertainty and anguish leads health workers to deal with different situations of distress with limited possibilities for resolution (2).
In the emergency period, health workers are at risk of developing mental distress and psychological disorders (3, 4). Altered conditions such as emotional state of frustration, a sense of helplessness, lack of personal efficacy, anger with depressive symptoms, and anxiety state with somatisations, such as insomnia, were frequent in these workers, together with increased consumption of caffeine, and tobacco (5, 6). A Chinese study (3) evaluated the presence of depressive and anxious symptoms in 1257 health workers employed in centres involved in the management of patients with COVID-19: women, nurses, and people working in areas more directly involved in the emergency reported more intense symptoms and required psychological support. The presence of common psychological disorders in these workers - especially women and nurses - has been reported by a recent systematic review (7). The psycho-physical state of the health personnel, in terms of stress and anxiety, directly affects the efficiency of healthcare, although not everyone experiences the same effect when individual characteristics come into play (8).
Within the literature on resilience, several studies have identified genetic, biological, psychological, and environmental factors promoting resilience in individuals (9-11). Several psychologists consider resilience as a personality trait, stable over time, that moderates the negative effects of stress promoting adaptation (12-14). As opposed, other authors consider resilience as a dynamic process changing in different contexts. According to this concept, human beings are not born resilient but become resilient in the presence of adversity as a result of the contrast between risk factors and protective factors. Resilience is seen as a dynamic process that varies in different contexts (15-17). Richardson (18) seeks to overcome this contrast between innate and learnable resilient traits by arguing that resilient qualities are present to varying degrees in each of us from birth, but at the same time they can be improved throughout life. Resilience, therefore, has a dual nature of trait and process. Moreover, resilience is also defined in the literature as a protective factor against adversity and stress in HCWs, allowing them to maintain mental well-being and psychological health (19).
Considering the direct involvement of HCWs in the care of COVID-19 patients in the emergency context, personal resilience can therefore help to effectively cope with the stress caused by the pandemic (20). Available studies have identified the protective role of resilience, particularly in nurses, during disasters (19) and disease epidemics (21), suggesting that high resilience levels can help to manage and tackle stressful situations by reducing levels of dysfunctional anxiety. It is important to highlight that dysfunctional anxiety levels have been identified as precursors of psychological distress, depression, and other psychological disorders (22). Increasing this resource may influence work performance, health, and general well-being of HCWs (23).
In addition to resilience, another protective factor is coping. Generally, the concept of coping refers to the way people respond to and cope with adverse situations. Coping is a broad concept that can be understood as a strategy, a style, or a resource. Initially regarded as a relatively stable personality trait, coping was subsequently considered as a set of possible and flexible reactions to life’s challenges (24). Finally, it has come to be considered a dynamic process in which individual resources interact, the events in their objectivity, the cognitive evaluation (appraisal) that the individual makes of these events, the willingness to make efforts, the efforts actually made, and their medium- and long-term outcome (25).
Coping strategies are behavioural, cognitive, and emotional modalities put in place to manage crises, conditions and requests that are perceived and valued as distressing. According to the theoretical model of Lazarus and Folkman (26), coping can be divided, according to its function, into Problem-Focused Coping and Emotion-Focused Coping: the former includes those strategies that involve action on the environment or on the self (for example, seeking the support of others to solve the problem, cognitive restructuring) while the latter include those strategies used to regulate one’s stressful emotions (e.g., positive re-evaluation, wishful thinking, substance use, estrangement, avoidance). In the coping literature it is argued that these two dimensions, i.e., Problem-Focused Coping and Emotion-Focused Coping, are overly broad and that some strategies may reflect both types of functions (e.g., feelings). Furthermore, the effectiveness of any particular coping strategy depends on the specific stressful situation, and most crises justify both types of coping.
There are many possibilities to manage stressful situations: previous studies have shown that the most common coping strategies used by health professionals during an emergency are the acceptance of the situation, criticism, and the use of a positive perspective at work (27). Perceived social/interpersonal support, greater self-efficacy, sense of personal control, and sense of coherence are among the most important individual factors in reducing stress and anxiety and may prevent interpersonal deficits (28, 29). Psychological damage is not a temporary process (30), therefore it would be appropriate to evaluate long-term effects to provide a tool for identifying high-risk people and planning interventions.
Prior to the COVID-19 pandemic, studies had identified a protective role for psychological resilience, coping behaviours, and social support in health care workers against psychological stress (31, 32) . This has been confirmed by numerous studies conducted in the context of the COVID-19 outbreak as reported in the systematic review of quantitative studies by Labrague (33). Concerning the context of the COVID-19 emergency, several authors have studied the resilience levels and coping behaviours of healthcare professionals. As reported by Labrague and colleagues (33), the coping strategies most often used by healthcare professionals as the main response mechanisms to manage the negative mental health consequences of the COVID-19 pandemic, have been support and communication with family members, friends, and colleagues and involvement in distracting activities. High levels of resilience in HCWs have been associated with a lower incidence of pandemic-related anxiety among nurses working in hospitals (23, 34), while lower levels of coronavirus-related anxiety were associated with higher levels of resilience (35, 36). Lisi et al. (37), studied the resilience levels in Italian HCWs during the SARS-CoV-2 emergency scenario and highlighted that resilience levels were lower than in the general population and negatively correlated with individual factors, such as the degree of anxiety and depression, and environmental factors such as lack of adequate personal protective equipment (37).
The present study aims to investigate the resilience levels as well as the emotional, cognitive and behavioural resources of clinical and research workers in a centre dedicated to rehabilitation. Exploring and enhancing different individual resources can allow healthcare professionals to emerge from this challenge with new skills, greater confidence in their own abilities to provide effective care for patients. The development of preventive programs for monitoring and maintaining the mental and psychological health of health workers is a well-needed intervention for the sake of workers and, consequently, for the quality of patient care.
Methods
Design and sample
The present study is a cross-sectional study promoted by the IRCCS San Raffaele Roma and approved by the internal Ethics Committee on July 21, 2020 (RP 07/20). The study was conducted on health workers (medical doctors, nurses, and physical therapists) and non-health workers (scientists and administrative employees) of the IRCCS San Raffaele Roma during the second wave of the COVID-19 pandemic. Data collection was carried out between February and April 2021, during the period of vaccination campaign for healthcare professionals. The IRCCS San Raffaele Roma is structured in two workplaces: the clinical centre, and the research and administrative headquarter 5 kilometres apart.
Measures
Data collection has been performed through a web-based questionnaire. Participants were asked to connect to a website using a link individually sent via email, and compile anonymously a survey. Data were collected with the use of an ad hoc web-based questionnaire composed by specific validated and standardised tests. After reading the study description and signing the informed consent to participate in the study, participants filled out the questionnaire in about 15 minutes. The questionnaire consisted of two sections, A and B. Section A provided the collection of demographic data, mansion in the hospital, and a detailed description of the potential risk to be infected by the virus. Section B aimed to explore the psychological state of health professionals in terms of resilience levels and emotional, cognitive, and behavioural resources using the following tests:
Fear of COVID-19 Scale (38), validation of the Italian version by Soraci et al. (39), consists of 7 items, each rated on a Likert scale from 1 to 5 (1=strongly disagree; 2=disagree; 3= neutral; 4= agree; 5= strongly agree) depending on the degree of agreement, with the aim of assessing the levels of fear related to COVID-19.
Hospital Anxiety and Depression Scale (40), validation of the Italian version by Costantini et al. (41) can be used as a screening questionnaire to assess anxiety and depression and it consists of 14 questions rated from 0 to 4 according to the severity of the experienced symptoms. The scale has the objective to assess both the anxious state (7 questions) and the depressive state (7 questions). According to Costantini et al. (41), the cut-off point that maximised sensitivity (84%) and specificity (79%) was 10.
Brief-COPE (42), validation of the Italian version by Conti (4) evaluates coping strategies, and adaptation modalities (cognitive, emotional, and behavioural) used by the participant to face stressful situations. In accordance with a situational approach, coping refers to the study of individual reactions to traumatic or threatening events. The Brief-COPE consists of 28 items divided into 14 scales relating to the 14 identified coping strategies: Positive restructuring, Distracting attention, Expression, Use of instrumental support, Operational coping, Denial, Religion, Humour, Behavioural disengagement, Use of emotional support, Substance use, Acceptance, Planning, and Self-accusation. Each strategy is identified by 2 items and each item is rated on a 4 points Likert scale (1=I haven’t been doing this at all; 2= I’ve been doing this a little bit; 3=I’ve been doing this a medium amount; 4=I’ve been doing this a lot). For each strategy, the final score is given by the sum of the two related items.
14-item Resilience Scale (12), validation of the Italian version by Callegari et al. (44) evaluates the levels of resilience and consists of 14 items, each rated on a 7 point Likert scale (1= strongly disagree; 7= strongly agree), depending on the degree of agreement. Resilience refers to the ability to face the adversities of life for individual, psychic, behavioural and adaptive qualities, overcome them and come out strengthened of them. In the Italian validation study (44) 4 the mean RS-14 score found is 76.13; therefore, the sample demonstrated a moderate resilience level.
Data management and analysis
After checking non-normality data distribution with the Shapiro-Wilk test, the Kruskall-Wallis one-way analysis of variance test was applied to identify differences among occupational categories and age-class for resilience, depression, anxiety and fear of COVID-19. Age classes were defined as follows: Age-class 1 (from 23 to 39 years), Age-class 2 (from 40 to 55 years), and Age-class 3 (from 56 to 71 years). Mann-Whitney U test was used to compare resilience, depression, anxiety, and fear between genders.
Significance level was set to p<0.05 and Dunn-Bonferroni post-hoc test was performed to take multiple comparisons into consideration (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). Brief-COPE outcomes were first analysed for internal consistency by means of Alpha’s Cronbach calculation (values near to 0 and 1 mean a low and a high reliability, respectively). Subsequently, statistically significant differences among its items were evaluated with the Kruskall-Wallis and Dunn-Bonferroni post-hoc test application (p<0.05). Finally, the link between all strategies couples was evaluated by using Spearman’s rank correlation coefficient. (IBM SPSS Statistics for Windows, Version 26.0. Armonk, 196 NY: IBM Corp).
Results
All workers who accepted to participate in the study and filled in the digital questionnaire were divided by age class, occupation and gender for statistics analysis. Out of the 556 workers who received the invitation to participate, 334 joined the study (60 % of the total of the workforce). All occupational categories were represented, and the participation rate was homogeneous across categories. The study group consisted of 109 (32.6%) men and 225 (67.4%) women. Thirty-four were medical doctors (10.2%), 105 nurses (41.4%), 78 therapists (23.4%), 35 scientists (10.5%), and 82 administrative employees (24.6%). Socio-demographic characteristics of hospital and non-hospital workers, including age class, occupation, years of service, are reported in Table 1. The table also included the percentage of workers affected by COVID-19. We found that 97 participants (29%) showed anxiety symptoms (41 of them presented high anxiety symptoms), 32 (10%) showed depressive symptoms (4 of whom presented with consistent depressive symptomatology), and 147 (44%) reported fear caused by COVID-19 pandemics. The large majority of participants, i.e., 87% (291), reported a level of resilience between moderate and high.
Table 1.
Distribution of study subjects according to demographic and epidemiological variables
| Demographic and Epidemiological variables | Hospital workers n (%) | Non-hospital workers n (%) |
|---|---|---|
| Gender | ||
| Males | 63 (28%) | 46 (43%) |
| Females | 165 (72%) | 60 (57%) |
| Age class | ||
| 23-39 years | 95 (42%) | 35 (33%) |
| 40-55 years | 102 (45%) | 63 (59%) |
| 56-71 years | 31 (14%) | 8 (8%) |
| Occupation | ||
| Medical Doctor | 34 (15%) | 0 (0%) |
| Nurse | 105 (46%) | 0 (0%) |
| Therapist | 78 (34%) | 0 (0%) |
| Researcher | 0 (0%) | 35 (33%) |
| Administrative employee | 11(5%) | 71 (67%) |
| Years of service | 14,02 ±10,35 | 14,88 ± 9,87 |
| Workers affected by COVID-19 | ||
| Yes | 44 (19%) | 8 (8%) |
| No | 184 (81%) | 98 (92%) |
| Relatives affected by COVID-19 | ||
| Yes | 49 (21%) | 20 (19%) |
| No | 179 (79%) | 86 (81%) |
Table 2 compares psychological parameters by gender, age class, and occupation. The levels of fear and anxiety are higher in female participants (p = 0.04, p<0.001 respectively). As regards the effect of age (Table 2 A), the youngest workers reported higher levels of anxiety (p<0.001), depression (p<0.001), and fear of COVID-19 (p=0.03) when compared to other age classes. Levels of resilience are lower in the youngest age class. Table 2 B shows statistically significant differences among occupational mansions for fear of COVID-19 and resilience. Nurses exhibit the greatest resilience level, whereas medical doctors show the lowest. Dunn’s post-hoc test with Bonferroni correction reveals statistically differences between administrative employees and nurses (p<0.001), and between nurses and medical doctors (p<0.04). Furthermore, therapists appear more scared of COVID-19 compared to nurses (p=0.02). No significant differences were found among occupational categories for depression and anxiety level.
Table 2.
Mean values ± SD of psychological parameters for sample divided by A) Demographic variables, and B) Job
| A) | Female | Male | Age class 1 | Age class 2 | Age class 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilience | 78.34 | ± | 11.87 | 77.32 | ± | 10.52 | 76.03 | ± | 11.87 | 79.67 | ± | 10.85b | 77.56 | ± | 11.62 |
| Depression | 3.45 | ± | 2.61 | 3.33 | ± | 2.92 | 3.80 | ± | 2.67 | 3.33 | ± | 2.70 | 2.44 | ± | 2.63a |
| Anxiety | 6.25 | ± | 3.91 | 4.37 | ± | 3.49a | 6.49 | ± | 4.13 | 5.35 | ± | 3.70b | 4.00 | ± | 2.95a |
| Fear COVID-19 | 16.08 | ± | 5.74 | 14.24 | ± | 4.95c | 16.19 | ± | 5.41 | 15.26 | ± | 5.71 | 14.00 | ± | 5.09b |
| a p<0.001 and cp=0.04; vs. age class 1 ap<0.001 and bp=0.03; vs. age class 1 | |||||||||||||||
| B) | Nurse | M.D. | Therapist | Researcher | Administrative | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilience | 80.53 | ± | 12.24 | 74.68 | ± | 11.26c | 78.47 | ± | 10.92 | 78.17 | ± | 10.40 | 75.65 | ± | 10.79a |
| Depression | 3.38 | ± | 2.88 | 3.41 | ± | 3.19 | 3.49 | ± | 2.44 | 2.71 | ± | 2.08 | 3.67 | ± | 2.76 |
| Anxiety | 5.60 | ± | 3.89 | 5.71 | ± | 4.69 | 5.90 | ± | 3.63 | 5.09 | ± | 3.67 | 5.65 | ± | 3.86 |
| Fear COVID-19 | 14.74 | ± | 5.75 | 14.59 | ± | 5.76 | 16.94 | ± | 5.76b | 14.34 | ± | 4.98 | 15.88 | ± | 5.00 |
ap<0.001; bp=0.02; cp=0.04 vs. Nurse
In Figure 1, mean values with standard deviation for the 14 items of the Brief-COPE test are reported. The sum of scores for each strategy covers a range from 2 to 8. Kruskall-Wallis test reveals statistically significant differences among coping strategies used to tackle an emergency situation (p<0.01). In particular Acceptance, Planning and Active coping are the most used strategies; Acceptance strategies are more frequently used when compared to Planning (p<0.001) and Active coping (p<0.05). The internal consistency of this scale was confirmed by the Cronbach’s alpha in the whole sample (0.778) as well as in subgroups of interest, e.g., medical doctors (0.817) or nurses (0.761).
Figure 1.
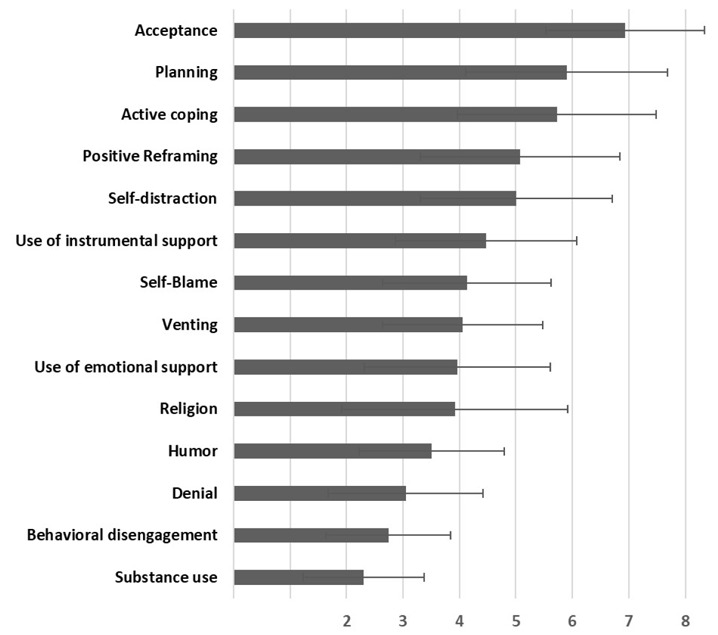
Mean values with standard deviation for the 14 items of the Brief-COPE test
The coupled correlation coefficients (Spearman’s rank correlation analysis) for the Brief-COPE strategies are shown in Table 3 and suggest high and significant correlations between Instrumental and Emotional support and between Self-distraction and Active coping strategies. Thus, we split the items of Self-distraction strategy into the two questions: one related to the engagement in their work, and another in leisure activities. A new analysis correlating separately Active coping with the two items of Self-distraction strategy, showed a stronger effect when running the analysis using the item related to the work. In the case of HCWs, devotion to work is an operative strategy to face the emergency.
Table 3.
Spearman’s rank coupled correlation coefficients of Brief-COPE items
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Positive Reframing | 1.000 | |||||||||||||
| 2 | Self-distraction | ,324** | 1.000 | ||||||||||||
| 3 | Venting | ,165** | ,274** | 1.000 | |||||||||||
| 4 | Use of instrumental support | ,380** | ,291** | ,472** | 1.000 | ||||||||||
| 5 | Active coping | ,437** | ,604** | ,229** | ,290** | 1.000 | |||||||||
| 6 | Denial | ,200** | ,203** | ,117* | ,150** | 0.030 | 1.000 | ||||||||
| 7 | Religion | ,310** | ,184** | ,163** | ,351** | ,174** | ,204** | 1.000 | |||||||
| 8 | Humour | ,192** | ,110* | ,144** | ,195** | 0.058 | 0.083 | -0.058 | 1.000 | ||||||
| 9 | Behavioural disengagement | ,109* | ,147** | ,160** | ,198** | -0.067 | ,365** | 0.072 | ,171** | 1.000 | |||||
| 10 | Use of emotional support | ,233** | ,390** | ,487** | ,708** | ,277** | ,241** | ,206** | ,209** | ,319** | 1.000 | ||||
| 11 | Substance use | -0.076 | 0.096 | 0.050 | 0.087 | -0.105 | ,136* | 0.037 | 0.091 | ,241** | ,216** | 1.000 | |||
| 12 | Acceptance | ,163** | -0.029 | 0.005 | 0.007 | ,136* | -,300** | 0.041 | -0.036 | -,215** | -,141** | -,215** | 1.000 | ||
| 13 | Planning | ,450** | ,212** | ,224** | ,320** | ,445** | -0.078 | ,167** | ,114* | -,120* | ,175** | -0.076 | ,434** | 1.000 | |
| 14 | Self-blame | ,279** | ,278** | ,455** | ,452** | ,210** | 0.037 | ,122* | ,225** | ,204** | ,403** | ,150** | -0.022 | ,344** | 1.000 |
*p<0.05, **p<0.01
Discussion
Understanding the psychological effect of working frontline during a health emergency has been the objective of most studies focused on the identification of symptoms related to the pandemics, but only a few investigated the presence of protective factors. The present study contributes to fill this gap and to provide a new perspective evaluating the role played by the level of resilience and the different coping strategies.
Our results showed that 87% of the participants reported a level of resilience between moderate and high. In particular, nurses belong to the most resilient category. Furthermore, higher levels of resilience were shown to be associated with lower levels of anxiety and depression acting as a protective factor over anxiety and depressive symptomatology, allowing a positive adaptation process to stressful conditions (45). In our study low levels of anxiety, depression, and fear of COVID-19 were observed. In accordance with published literature (7, 46), it has been observed that anxious symptomatology and fear of COVID-19 were more frequent in women, and that older workers showed fewer symptoms (47), possibly due to the longer experience with emergency situations. The percentage of depressive symptoms in our study was 10%. Our results show significantly lower levels of depressive symptoms than in previous published studies (50.4 %, 55%, and 12.2%) (3, 4, 7). In our study, compared to the literature we observed high levels of resilience and coping strategies and lower levels of anxiety, depression, and fear, implying that resilience and coping strategies could represent protective factors for healthcare workers, possibly preventing the development of long-term psychological disorders in a stressful situation such as COVID-19.
An interesting issue has been found in people who have had direct experience with COVID-19. The level of depression was 3.51±0.159 for people who did not contract COVID-19 versus 2.88±0.398 (p = 0.048) for those who contracted the disease, for anxiety 5.78±0.227 versus 4.87±0.058 (p=0.042), while for fear of Covid-19 was 15.61±0.32 versus 14.77±0.09 (p>0.05 according to Mann-Whitney test). The small number of workers that were infected in our sample (16%), did not allow a high statistical significance.
Resilience, when associated with successful coping strategies, could be more effective. According to Wong (27), our study revealed that the most used strategy is Acceptance, highlighting that the first functional strategy used in a stressful situation is to be aware of the situation itself. Among the most common strategies, the attitude to identify the most suitable strategies to resolve the condition (Planning), and the attitude to focus on the situation, developing strategies to deal with it (Active coping).
Finally, we found the strongest correlations between the Use of instrumental support and the Use of emotional support (both problem-focused coping strategies) and between Active coping and Self-distraction (problem-focused coping and emotion-focused coping). The ability to rely on the help of others in difficult situations (Use of instrumental support) and seeking help and emotional support from others (Use of emotional support) are reported as the most important personal factors in reducing anxiety (28, 29). Such problem-centred coping strategies have the advantage of allowing, in the second phase of emergency, appropriate action to be taken after distress levels have somehow subsided and when appropriate action can be taken. Conversely, coping strategies that focus on emotions, such as self-distraction, can have the advantage of preventing the level of distress from becoming too overwhelming and therefore are more appropriate strategies in the early stages in response to a severe stressor, such as coping with SARS-CoV-2 pandemic. In fact, avoiding thoughts and feelings associated with an event can increase the individual’s discomfort over time, while distraction (especially distraction techniques that involve commitment to work and social activities) can be effective in dealing with particularly intense feelings and can serve to reduce discomfort. In the published literature on coping it is consistently reported that the best option is to have a flexible coping style which may involve the use of different sized strategies through the coping process, depending on the current needs of the situation (48).
The main limitation of this study is its timing, since it was not run during the first emergency wave but when most HCWs had received the vaccination, diluting the effect of the COVID-19 outbreak.
The pandemics had a different impact on different occupation categories: nurses and medical doctors had a direct therapeutic relationship with the patients, while other workers (researchers and administrative employees) experienced the emergency without any relationships with the patients. Data analysis on nurses and medical doctors revealed informative relationships between behavioural strategies in these highly exposed categories. The correlation between Use of instrumental support - Use of emotional support and Active coping - Self-distraction were observed in these two categories. In particular, in the group of nurses two other significant correlations were observed: a) the first is between Venting and Use of emotional support, suggesting the ability of nurses to express their emotions without shame by seeking help and emotional support; Venting was also related with Use of instrumental support, and b) the second between Planning and Use of instrumental support, indicating the skill to get some help for tackling the situation. Medical doctors experienced a strong correlation of Active coping, with Self-distraction, Use of instrumental support, and Venting: this finding demonstrates high the active role of medical doctors in the emergency context in spite of emotional involvement. These correlation analyses, thus, suggest that nurses are more likely to be open emotionally to people close to them, while medical doctors are prone to a more complex approach that also makes use of active strategies and greater engagement.
Conclusions
The present research provided information on the importance of preserving mental and psychological health among HCWs, possibly increasing resilience levels and coping behaviours in emergency situations. Indeed, it’s essential for health workers to be aware of their emotional, cognitive, and behavioural resources to manage work in emergency contexts like SARS-CoV-2 (49). Our study provided information about the importance of resilience and the use of specific problem-focused and emotion-focused coping strategies as protective factors from psychological distress. The implementation of psychoeducational interventions - such as individual and group skill training programs - to promote emotional, cognitive and behavioural resources should be considered not only in emergency situations, but also in situations of daily stress for a more adequate assistance to the patient care.
Acknowledgements:
We are extremely grateful to the whole staff of IRCCS San Raffaele Roma, for their dedication and for actively collaborating on the research.
Conflicts of interest:
The authors declare no conflict of interest.
References
- 1.Zhao Y, Cui C, Zhang K, et al. COVID19: A Systematic Approach to Early Identification and Healthcare Worker Protection. Front Public Health. 2020;8:205. doi: 10.3389/fpubh.2020.00205. doi:10.3389/fpubh.2020.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rapporto ISS COVID-19, n 1/2020; n.2 Rev./2020; n.3 Rev./2020. (2020) [Google Scholar]
- 3.Lai J, Ma S, Wang Y, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. Mar 2 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. doi:10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang WR, Wang K, Yin L, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. doi:10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kushal A GS, Mehta M, Singh MM. Study of Stress among Health Care Professionals: A Systemic Review. International Journal of Research Foundation of Hospital and Healthcare Administration. 2018;6(1):6–11. doi:10.5005/jp-journals-10035-1084. [Google Scholar]
- 6.Lancee WJ, Maunder RG, Goldbloom DS. Coauthors for the Impact of SS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. Jan 2008;59(1):91–5. doi: 10.1176/ps.2008.59.1.91. doi:10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res. Sep 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. doi:10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu X, Kakade M, Fuller CJ, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. Jan 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. doi:10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaffee SR, Caspi A, Moffitt TE, Polo-Tomas M, Taylor A. Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: a cumulative stressors model. Child Abuse Negl. Mar 2007;31(3):231–53. doi: 10.1016/j.chiabu.2006.03.011. doi:10.1016/j.chiabu.2006.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry. Feb 2004;161(2):195–216. doi: 10.1176/appi.ajp.161.2.195. doi:10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- 11.Iacoviello BM, Charney DS. Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. Eur J Psychotraumatol. 2014:5. doi: 10.3402/ejpt.v5.23970. doi:10.3402/ejpt.v5.23970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. Winter 1993;1(2):165–78. [PubMed] [Google Scholar]
- 13.Miller TW. Advances in understanding the impact of stressful life events on health. Hosp Community Psychiatry. Jun 1988;39(6):615–22. doi: 10.1176/ps.39.6.615. doi:10.1176/ps.39.6.615. [DOI] [PubMed] [Google Scholar]
- 14.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. doi:10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 15.Fine SB. Resilience and human adaptability: who rises above adversity? 1990 Eleanor Clarke Slagle Lecture. Am J Occup Ther. Jun 1991;45(6):493–503. doi: 10.5014/ajot.45.6.493. doi:10.5014/ajot.45.6.493. [DOI] [PubMed] [Google Scholar]
- 16.Garmezy N. Children in poverty: resilience despite risk. Psychiatry. Feb 1993;56(1):127–36. doi: 10.1080/00332747.1993.11024627. doi:10.1080/00332747.1993.11024627. [DOI] [PubMed] [Google Scholar]
- 17.Rutter M. Resilience, competence, and coping. Child Abuse Negl. Mar 2007;31(3):205–9. doi: 10.1016/j.chiabu.2007.02.001. doi:10.1016/j.chiabu.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol. Mar 2002;58(3):307–21. doi: 10.1002/jclp.10020. doi:10.1002/jclp.10020. [DOI] [PubMed] [Google Scholar]
- 19.Labrague LJ, Hammad K, Gloe DS, et al. Disaster preparedness among nurses: a systematic review of literature. Int Nurs Rev. Mar 2018;65(1):41–53. doi: 10.1111/inr.12369. doi:10.1111/inr.12369. [DOI] [PubMed] [Google Scholar]
- 20.Cooper AL, Brown JA, Rees CS, Leslie GD. Nurse resilience: A concept analysis. Int J Ment Health Nurs. Aug 2020;29(4):553–575. doi: 10.1111/inm.12721. doi:10.1111/inm.12721. [DOI] [PubMed] [Google Scholar]
- 21.Louise Duncan D. What the COVID-19 pandemic tells us about the need to develop resilience in the nursing workforce. Nurs Manag (Harrow) Jun 2 2020;27(3):22–27. doi: 10.7748/nm.2020.e1933. doi:10.7748/nm.2020.e1933. [DOI] [PubMed] [Google Scholar]
- 22.Teles MA, Barbosa MR, Vargas AM, et al. Psychosocial work conditions and quality of life among primary health care employees: a cross sectional study. Health Qual Life Outcomes. May 15 2014;12:72. doi: 10.1186/1477-7525-12-72. doi:10.1186/1477-7525-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J Nurs Manag. Oct 2020;28(7):1653–1661. doi: 10.1111/jonm.13121. doi:10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eckenrode J. The social context of coping. New York: Plenum; 1991. [Google Scholar]
- 25.Skinner E, Edge K. Coping and development across the life span. International Journal of Behavioural Development. 1998;22:225–366. [Google Scholar]
- 26.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. pp. 1–456. [Google Scholar]
- 27.Wong TW, Yau JK, Chan CL, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. Feb 2005;12(1):13–8. doi: 10.1097/00063110-200502000-00005. doi:10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Conversano C, Marchi L, Miniati M. Psychological distress among healthcare professionals involved in the COVID-19 emer-gency: Vulnerability and resilience factors. Clin Neuropsychiatry. 2020;17:94–96. doi: 10.36131/CN20200212. doi:doi.org/10.36131/CN20200212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Leo A, Cianci E, Mastore P, Gozzoli C. Protective and Risk Factors of Italian Healthcare Professionals during the COVID-19 Pandemic Outbreak: A Qualitative Study. Int J Environ Res Public Health. Jan 8 2021;18(2) doi: 10.3390/ijerph18020453. doi:10.3390/ijerph18020453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanghera J, Pattani N, Hashmi Y, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting-A Systematic Review. J Occup Health. Jan 2020;62(1):e12175. doi: 10.1002/1348-9585.12175. doi:10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pincha Baduge MS, Morphet J, Moss C. Emergency nurses’ and department preparedness for an ebola outbreak: A (narrative) literature review. Int Emerg Nurs. May 2018;38:41–49. doi: 10.1016/j.ienj.2017.12.002. doi:10.1016/j.ienj.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 32.De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): A rapid systematic review. PLoS One. 2020;15(12):e0244052. doi: 10.1371/journal.pone.0244052. doi:10.1371/journal.pone.0244052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J Nurs Manag. Oct 2021;29(7):1893–1905. doi: 10.1111/jonm.13336. doi:10.1111/jonm.13336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Labrague LJ, De Los Santos JAA. Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nurs. May 2021;38(3):382–389. doi: 10.1111/phn.12841. doi:10.1111/phn.12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khalaf OO, Khalil M A, Abdelmaksoud R. Coping with Depression and Anxiety in Egyptian Physicians during COVID-19 Pandemic. Middle East Current Psychiatry. 2020 doi:10.1186/s43045-020-00070-9. [Google Scholar]
- 36.Mosheva M, Hertz-Palmor N, Dorman Ilan S, et al. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depression and Anxiety. 2020 doi: 10.1002/da.23085. doi:https://doi.org/10.1002/da.23085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lisi L, Ciaffi J, Bruni A, et al. Levels and Factors Associated with Resilience in Italian Healthcare Professionals during the COVID-19 Pandemic: A Web-Based Survey. doi: https://doi.org/10.3390/bs10120183 . [DOI] [PMC free article] [PubMed]
- 38.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. Mar 27 2020:1–9. doi: 10.1007/s11469-020-00270-8. doi:10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soraci P, Ferrari A, Abbiati FA, et al. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int J Ment Health Addict. May 4 2020:1–10. doi: 10.1007/s11469-020-00277-1. doi:10.1007/s11469-020-00277-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. Jun 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. doi:10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 41.Costantini M, Musso M, Viterbori P, et al. Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer. May 1999;7(3):121–7. doi: 10.1007/s005200050241. doi:10.1007/s005200050241. [DOI] [PubMed] [Google Scholar]
- 42.Carver CS. You want to measure coping but your protocol’s too long: consider the Brief-COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. doi:10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 43.Conti. Italian collection of the assessment scales in psychiatry. 2000 [Google Scholar]
- 44.Callegari C, Bertu L, Lucano M, Ielmini M, Braggio E, Vender S. Reliability and validity of the Italian version of the 14-item Resilience Scale. Psychol Res Behav Manag. 2016;9:277–284. doi: 10.2147/PRBM.S115657. doi:10.2147/PRBM.S115657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foster K, Roche M, Giandinoto JA, Furness T. Workplace stressors, psychological well-being, resilience, and caring behaviours of mental health nurses: A descriptive correlational study. Int J Ment Health Nurs. Feb 2020;29(1):56–68. doi: 10.1111/inm.12610. doi:10.1111/inm.12610. [DOI] [PubMed] [Google Scholar]
- 46.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. Aug 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. doi:10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luceno-Moreno L, Talavera-Velasco B, Garcia-Albuerne Y, Martin-Garcia J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int J Environ Res Public Health. Jul 30 2020;17(15) doi: 10.3390/ijerph17155514. doi:10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dubow EF, Rubinlicht M. Coping. Encyclopedia of Adolescence. 2011;3:109–118. doi:10.1016/B978-0-12-373951-3.00107-1. [Google Scholar]
- 49.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. Mar 26 2020;368:m1211. doi: 10.1136/bmj.m1211. doi:10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]


