Abstract
Background
Complementary and Alternative Medicine (CAM) has gained popularity among the general population, but its acceptance and use among medical specialists have been inconclusive. This systematic review aimed to identify relevant studies and synthesize survey data on the acceptance and use of CAM among medical specialists.
Methods
We conducted a systematic literature search in PubMed and Scopus databases for the acceptance and use of CAM among medical specialists. Each article was assessed by two screeners. Only survey studies relevant to the acceptance and use of CAM among medical specialists were reviewed. The pooled prevalence estimates were calculated using random-effects meta-analyses. This review followed both PRISMA and SWiM guidelines.
Results
Of 5628 articles published between 2002 and 2017, 25 fulfilled the selection criteria. Ten medical specialties were included: Internal Medicine (11 studies), Pediatrics (6 studies), Obstetrics and Gynecology (6 studies), Anesthesiology (4 studies), Surgery (3 studies), Family Medicine (3 studies), Physical Medicine and Rehabilitation (3 studies), Psychiatry and Neurology (2 studies), Otolaryngology (1 study), and Neurological Surgery (1 study). The overall acceptance of CAM was 52% (95%CI, 42–62%). Family Medicine reported the highest acceptance, followed by Psychiatry and Neurology, Neurological Surgery, Obstetrics and Gynecology, Pediatrics, Anesthesiology, Physical Medicine and Rehabilitation, Internal Medicine, and Surgery. The overall use of CAM was 45% (95% CI, 37–54%). The highest use of CAM was by the Obstetrics and Gynecology, followed by Family Medicine, Psychiatry and Neurology, Pediatrics, Otolaryngology, Anesthesiology, Internal Medicine, Physical Medicine and Rehabilitation, and Surgery. Based on the studies, meta-regression showed no statistically significant difference across geographic regions, economic levels of the country, or sampling methods.
Conclusion
Acceptance and use of CAM varied across medical specialists. CAM was accepted and used the most by Family Medicine but the least by Surgery. Findings from this systematic review could be useful for strategic harmonization of CAM and conventional medicine practice.
Systematic review registration
PROSPERO CRD42019125628
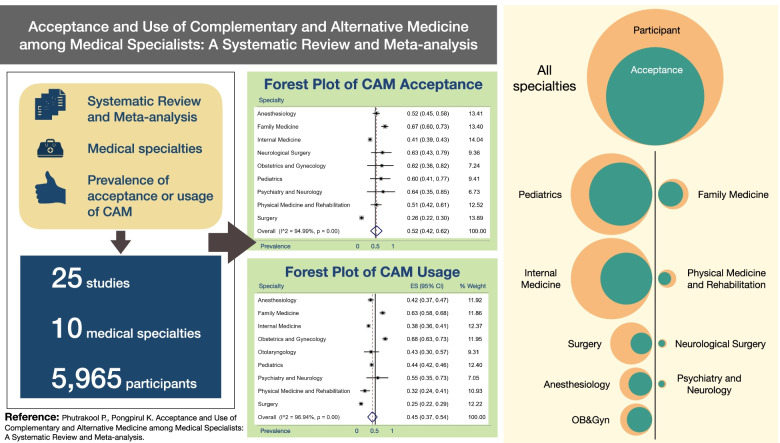
Graphical abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-021-01882-4.
Keywords: Acceptance, Use, Complementary and alternative medicine, Medical specialist
Background
Medical specialist is a healthcare professional who has undertaken specialized medical studies to diagnose, treat and prevent illness, disease, injury, and other physical and mental impairments in humans, using specialized testing, diagnostic, medical, surgical, physical, and psychiatric techniques, through application of the principles and procedures of modern medicine [1]. The specialized and general medical care have dominated as ‘conventional’ medical care in several countries, including Thailand.
Complementary and Alternative Medicine (CAM) is defined as medicine or treatment which is not considered as conventional (standard) medicine. The National Center for Complementary and Integrative Health (NCCIH) categorized most types of complementary medicines under two categories: (1) natural products and (2) mind-body practices [2]. Natural products include herbs, vitamins, minerals, and probiotics whereas mind-body practices include yoga, chiropractic, massage, acupuncture, yoga, meditation, and massage therapy. Types of CAM may vary across studies, but they overlap in most senses.
CAM is used by people throughout the world. A study showed that the prevalence estimate of CAM usage from 32 countries from all regions of the world to be 26.4%, ranging from 25.9 to 26.9%. For example, in 2013, the prevalence use of CAM in Australia, the USA, UK, and China were 34.7%, 21.0%, 23.6%, and 53.3%, respectively. The prevalence estimate of CAM satisfaction was as high as 71.9%, ranging from 71.0 to 72.7% [3].
Although patients are highly satisfied with CAM treatment, professional health care providers who are medical doctors do not offer CAM because it is not part of the standard conventional medical care. Although the majority of physicians who have used CAM were pleased with the results [4–8] and were more likely to recommend it to patients, friends, and family [9, 10] as a non-toxic treatment option; less than one third of the medical doctors were very comfortable in answering questions about CAM [9, 11–13] so patients who do not have the option to use CAM instead of standard medical care might be lost to follow-up. Some doctors are still skeptical of CAM because of a lack of specific knowledge and qualification as well as a lack of evidence from high-quality experimental studies on the efficacy of the CAM treatments [4, 12, 14, 15]. In the field of oncology, for example, the 5-year survival rate of breast cancer patients who refused standard treatment was 43.2%, compared with 81.9% of those who underwent the standard treatment [16]. When CAM was used, the 5-year survival rate was significantly worse. The 5-year survival rate of cancer patients who used CAM versus those who used standard treatment were stratified by cancer type were as follows: [17] for breast cancer 58.1% vs 86.6% (p value < 0.01; HR = 5.68), lung cancer 19.9% vs 41.3% (p value < 0.01; HR = 2.17), and colorectal cancer 32.7% vs 79.4% (p value < 0.01; HR = 4.57). On the contrary, the 28-day mortality of patient with sepsis and acute gastrointestinal injury who received CAM bundle with conventional therapy was statistically significantly lower than those who received only conventional therapy (21.2% vs 32.5%, p value = 0.038) [18]. These differential clinical benefits of CAM across various medical specialties could be partly explained by how CAM is perceived by the medical specialists in conventional medicine dominated contexts.
Several studies have surveyed the acceptance and use of CAM from laypersons [19–22] to healthcare professional perspectives [23–29]. Nonetheless, these surveys did not cover all medical specialists so the findings could not reflect the comparative acceptance and use of CAM across medical specialties. Also, previous studies could not determine whether the acceptance and use of CAM by medical specialists differ across contexts (i.e., regions and economic levels of the country) and study designs (i.e., survey and sampling methods). A better understanding of how various medical specialists perceive of CAM is strategically essential for harmonizing CAM into conventional medicine practices. This systematic review aimed to identify relevant studies and synthesize survey data on the acceptance and use of CAM among medical specialists.
Materials and methods
Protocol and registration
This systematic review has been registered in PROSPERO (CRD42019125628) and the protocol can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42019125628.
Literature search
This systematic review was conducted and reported according to the PRISMA statement as well as the Synthesis Without Meta-analysis (SWiM) guidelines [30]. A systematic literature search was performed by two independent authors (PP and KP) using PubMed and Scopus databases. The search was limited to observational studies of human subjects and the English language. The medical specialist’s perspective related to CAM studies were focused. The search strategy was based on various combinations of words and focused on two main concepts: acceptance and usage of CAM. The last search was conducted on March 1, 2019.
For the PubMed database, the following combinations were applied: ("Traditional Medicine"[All Fields] OR "Alternative Medicine"[All Fields] OR "Complementary Medicine"[All Fields] OR "Acupuncture Therapy"[All Fields] OR "Holistic Health"[All Fields] OR "Homeopathy"[All Fields] OR "Spiritual Therapies"[All Fields] OR "Faith Healing"[All Fields] OR "Yoga"[All Fields] OR "Witchcraft"[All Fields] OR "Shamanism"[All Fields] OR "Meditation"[All Fields] OR "Aromatherapy"[All Fields] OR "Medical Herbalism"[All Fields] OR "Mind-Body Therapies"[All Fields] OR "Laughter Therapy"[All Fields] OR "Hypnosis"[All Fields] OR "Tai Ji"[All Fields] OR "Tai Chi"[All Fields] OR "Relaxation Therapy"[All Fields] OR "Mental Healing"[All Fields] OR "Meditation"[All Fields]) AND ("Health care provider"[All Fields] OR "Health care providers"[All Fields] OR "Health personnel"[All Fields]) AND ("2002/01/01"[PDAT]: "2017/12/31"[PDAT]) AND "humans"[MeSH Terms].
For the Scopus database, the following combinations were applied: (ALL("Traditional Medicine") OR ALL("Alternative Medicine") OR ALL("Complementary Medicine") OR ALL("Acupuncture Therapy") OR ALL("Holistic Health") OR ALL("Homeopathy") OR ALL("Spiritual Therapies") OR ALL("Faith Healing") OR ALL("Yoga") OR ALL("Witchcraft") OR ALL("Shamanism") OR ALL("Meditation") OR ALL("Aromatherapy") OR ALL("Medical Herbalism") OR ALL("Mind-Body Therapies") OR ALL("Laughter Therapy") OR ALL("Hypnosis") OR ALL("Tai Ji") OR ALL("Tai Chi") OR ALL("Relaxation Therapy") OR ALL("Mental Healing") OR ALL("Meditation")) AND (ALL("Health care provider") OR ALL("Health care providers") OR ALL("Health personnel")) AND PUBYEAR AFT 2001 AND PUBYEAR BEF 2018 AND DOCTYPE(ar) AND INDEXTERMS("Humans")
Selection of studies
The titles and abstracts of the primary studies identified in the electronic search were screened by the same two authors. Duplicated studies were excluded. For the meta-analysis, the following inclusion criteria were set: (1) medical specialist’s perspective, (2) prevalence of acceptance or usage of CAM, (3) observational study design, and (4) published between 2002 to 2017. The following exclusion criterion was set: (1) Not relevant to the practice. We contacted the authors for studies that had incomplete and unclear information. If the authors did not respond within 14 days, we proceeded to analyze the data we had. Any disagreement was resolved through discussion and the final determination was made by the first author (PP).
Data extraction and management
Two authors worked independently to review and extract the following variables: (1) general information, including the name of the studies, authors, and publication year, (2) characteristics of the studies, including the design of the studies, sampling method, country, and setting, (3) characteristics of the participants, including sample size, response, and type of specialty, and (4) outcomes, including the prevalence of acceptance, and usage of CAM. All relevant text, tables, and figures were examined for data extraction. Discrepancies between the two reviewers were resolved by the first author (PP).
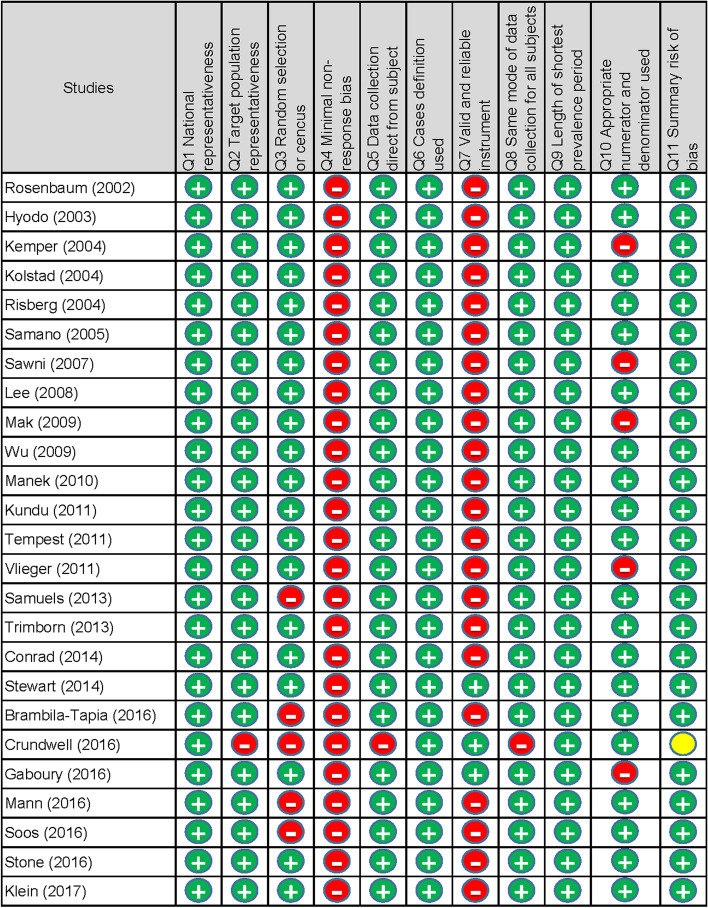
Study quality/risk of bias
We used the tool developed by Hoy et al. [31] to evaluate the study quality/risk of bias of the studies included in the analysis. The tool has 11 items: (1) national representativeness, (2) target population representativeness, (3) random selection or census undertaken, (4) minimal non-response bias, (5) data collection direct from the subject, (6) definition of the case used, (7) valid and reliable instrument, (8) the same mode of data collection for all subjects, (9) length of shortest prevalence period, (10) appropriate numerator and denominator used, and (11) summary assessment. Items 1 to 4 assessed the external validity, items 5 to 10 assessed the internal validity, and items 11 evaluated the overall study quality/risk of bias. Each item was assigned a score of 1 (high quality/low risk) or 0 (low quality/high risk), and the scores were summed to generate an overall quality score that ranged from 0 to 10. According to the overall score, we classified the studies as having a high quality/low risk of bias (>6), moderate quality/risk of bias (4 to 6), and low quality/high risk of bias (<4). Two authors (PP and KP) independently assessed the study quality/risk of bias and any disagreement was resolved by discussion and consensus.
Conflict of interest
We assessed the conflict of interest of the authors’ declarations in the studies.
Statistical analysis
Unadjusted prevalence estimates of acceptance and usage of CAM were calculated based on the information of crude numerators and denominators provided by the studies and medical specialty [32]. Pooled prevalence was estimated from the prevalence as reported by the eligible studies. For each study and specialty, forest plots were generated displaying the prevalence with a 95% CI. The overall random-effects pooled estimate with its 95% CI were reported. To examine the magnitude of the variation between the studies, we quantified the heterogeneity by using I2 and its 95% CI.
To assess the level of heterogeneity as defined in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions, the following I2 cut-offs for 0 to 40% represented that the heterogeneity may not be important, 30 to 60% may represent moderate heterogeneity, 50 to 90% may represent substantial heterogeneity, and 75 to 100% represented that there was a considerable heterogeneity. For the X2 test, statistical heterogeneity of the included trials was assessed with a p value of less than 0.05 (statistically significant). The random-effects meta-analysis by DerSimonian and Laird method was used, and statistical heterogeneity was encountered. The meta-analysis was performed using Stata/MP software version 15 (StataCorp 2017, College Station, TX).
Additional analysis
Meta-regression was performed to investigate the pooled prevalence differences between various regions (African region, region of the Americas, Eastern Mediterranean region, European region, Southeast Asia region, Western Pacific region, and mixed region) [33], economic levels of the country (low-income, lower-middle-income, upper-middle-income, high-income, and mixed-income) [34], and the sampling method (random and convenience sampling) for each study.
Results
Selection of the studies
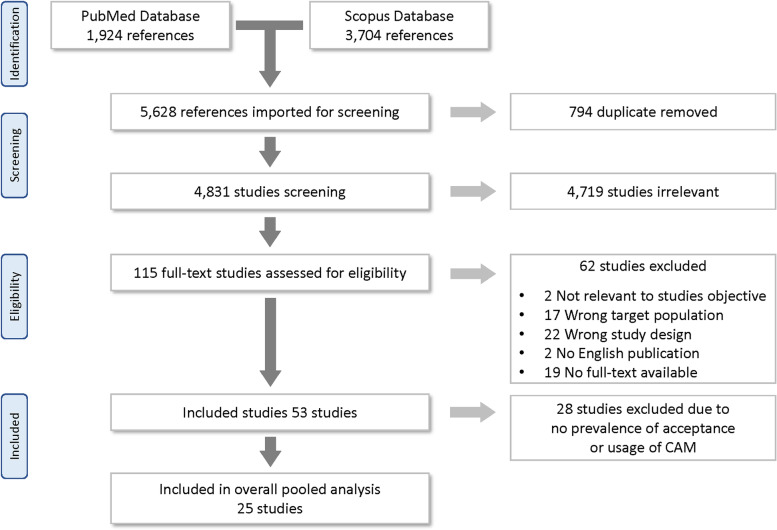
The literature search yielded 5628 articles. After 794 duplicates were removed, 4831 titles and abstracts were screened, and 4719 irrelevant articles were removed. Of 115 articles selected for full-text screening, 62 were excluded for the following reasons: two were not relevant to this study’s objective, 17 had the wrong target population, 22 did not have the study design required for this review, two study was not published in English, 19 did not have full-text available, and 28 did not provide the prevalence. Finally, a total of 25 articles, published between 2002 and 2017, fulfilled the selection criteria and were included in this meta-analysis (Fig. 1).
Fig. 1.
Selection of the studies
Characteristics of the studies
All included studies were cross-sectional. The publication years ranged from 2002 to 2017 in various countries: European region (n = 11, 44%), region of the Americas (n = 10, 40%), Western Pacific region (n = 3, 12%), and mixed region (n = 1, 4%). Twenty-three studies (88%) were from high-income countries, 2 (8%) from upper-middle income countries, and 1 (4%) was from mixed-economic level country. The included studies indicated which type of collection method was used: online survey (n = 8, 32%), postal survey (n = 8, 32%), online and postal survey (n = 3, 12%), online and phone survey (n = 1, 4%), and the collection method was not reported (n = 5, 20%). The studies included a total of 7320 participants who were categorized as medical specialty (n = 5445, 74%), and non-medical specialty (n = 1875, 26%) (Table 1).
Table 1.
Characteristics of the included studies
| First author | Year | Country | Setting | Sampling method | Survey method | Response, % | Response, n | Medical specialist, n | Citation |
|---|---|---|---|---|---|---|---|---|---|
| Rosenbaum | 2002 | USA | The University of Iowa College of Medicine | Random | Postal | 18.4% | 690 | 265 | [35] |
| Hyodo | 2003 | Japan | The Japanese oncology literature and the Nationwide association of medical centers for cancer and adult diseases | Random | Postal | 66.7% | 54 | 52 | [36] |
| Kemper | 2004 | USA | The American Academy of Pediatrics | Random | Online | 19.5% | 195 | 195 | [37] |
| Kolstad | 2004 | Norway | Five university oncology units in Norway | Random | Postal | 38.5% | 751 | 751 | [5] |
| Risberg | 2004 | Norway | Five reginal oncology centers | Random | Postal | 15.4% | 104 | 104 | [38] |
| Samano | 2005 | Brazil | Effective physician members of the Brazilian Cancer Society | Random | Postal | 61.5% | 509 | 108 | [39] |
| Sawni | 2007 | USA | The American Academy of Pediatrics | Random | Postal | 31.5% | 268 | 263 | [40] |
| Lee | 2008 | USA, China, and Taiwan | The Northern California Tumor Board meeting, China Medical University, Sun-Yat Sen Cancer Center Taiwan, Peking University Cancer Hospital China, and Peking Union Hospital China | Random | Postal | 38.0% | 95 | 95 | [15] |
| Mak | 2009 | Australia | The Australasian Faculty of Rehabilitation Medicine, The Royal Australasia College of Physicians | Random | Online | 38.3% | 36 | 36 | [41] |
| Wu | 2009 | USA | The Washington State of Association of Neurological Surgeons | Random | Online | 67.0% | 65 | 65 | [42] |
| Manek | 2010 | USA | The practicing rheumatologists in the United States | Random | Postal | 40.3% | 381 | 381 | [6] |
| Kundu | 2011 | USA | The Seattle Children’s Hospital | Random | Online | 43.7% | 213 | 213 | [43] |
| Tempest | 2011 | England | A urologist practicing in three English training deaneries | Random | Online and Phone | 13.4% | 88 | 88 | [44] |
| Vlieger | 2011 | Netherlands | The Dutch Society of Paediatrics | Random | Online | Not indicated denominator | 170 | 170 | [45] |
| Samuels | 2013 | Israel | Member of the Obstetricians and gynecologists (board-certified specialists or residents) were recruited from 7 medical centers in Southern, Central, and Northern Israel | Convenience | Not indicated | 18.5% | 648 | 648 | [46] |
| Trimborn | 2013 | Germany | A German employee visiting the occupational health service of the university hospital | Convenience | Not indicated | 75.7% | 258 | 258 | [8] |
| Conrad | 2014 | Germany | The German Society for Palliative Care | Random | Online | 86.7% | 117 | 40 | [47] |
| Stewart | 2014 | Scotland | The care of pregnant women in the Grampian region of North-East Scotland | Random | Online and postal | 72.0% | 126 | 96 | [48] |
| Brambila-Tapia | 2016 | Mexico | The Primary and secondary care hospitals in Guadalajara | Convenience | Not indicated | 13.0% | 547 | 120 | [49] |
| Crundwell | 2016 | UK | The Clinical staff at Cambridge University Hospital’sotolaryngology and audiology departments | Convenience | Not indicated | 23.7% | 343 | 343 | [10] |
| Gaboury | 2016 | Canada | The College des medecins du Quebec | Random | Online | 100.0% | 207 | 107 | [50] |
| Mann | 2016 | USA | pain medicine fellowship at the American College of Graduate Medical Education | Convenience | Online and postal | 53.3% | 856 | 856 | [7] |
| Soos | 2016 | Hungary | Four Hungarian universities and other eleven surgery wards and intensive care departments participated in the study | Convenience | Online and postal | 61.5% | 509 | 101 | [51] |
| Stone | 2016 | Australia | All faculties, fellows, and residents presented at a single anesthesia grand rounds of Johns Hopkins University | Random | Not indicated | 70.3% | 102 | 102 | [52] |
| Klein | 2017 | Germany | The Research Group on Gynecological Oncology of the German Cancer Society | Random | Online | 38.1% | 24 | 24 | [14] |
The included studies had the following medical specialties: internal medicine (11 studies, n = 2253), pediatrics (6 studies, n = 2,130), obstetrics and gynecology (6 studies, n = 707), anesthesiology (4 studies, n = 342), surgery (3 studies, n = 564), family medicine (3 studies, n = 296), physical medicine and rehabilitation (3 studies, n = 104), psychiatry and neurology (2 studies, n = 22), otolaryngology (1 study, n = 49), and neurological surgery (1 study, n = 24) (Table 2)
Table 2.
The number of medical specialists according to the American Board of Medical Specialties
| No. | American Board of Medical Specialties | Studies | Participants |
|---|---|---|---|
| 1 | Allergy and Immunology | - | - |
| 2 | Anesthesiology | 4 | 342 |
| 3 | Colon and Rectal Surgery | - | - |
| 4 | Dermatology | - | - |
| 5 | Emergency Medicine | - | - |
| 6 | Family Medicine | 3 | 296 |
| 7 | Internal Medicine | 11 | 2,108 |
| 8 | Medical Genetics and Genomics | - | - |
| 9 | Neurological Surgery | 1 | 24 |
| 10 | Nuclear Medicine | - | - |
| 11 | Obstetrics and Gynecology | 5 | 326 |
| 12 | Ophthalmology | - | - |
| 13 | Orthopaedic Surgery | - | - |
| 14 | Otolaryngology - Head and Neck Surgery | 1 | 49 |
| 15 | Pathology | - | - |
| 16 | Pediatrics | 6 | 2,130 |
| 17 | Physical Medicine and Rehabilitation | 3 | 104 |
| 18 | Plastic Surgery | - | - |
| 19 | Preventive Medicine | - | - |
| 20 | Psychiatry and Neurology | 2 | 22 |
| 21 | Radiology | - | - |
| 22 | Surgery | 3 | 564 |
| 23 | Thoracic Surgery | - | - |
| 24 | Urology | - | - |
| Total | 39 | 5,965 | |
Based on the specialty
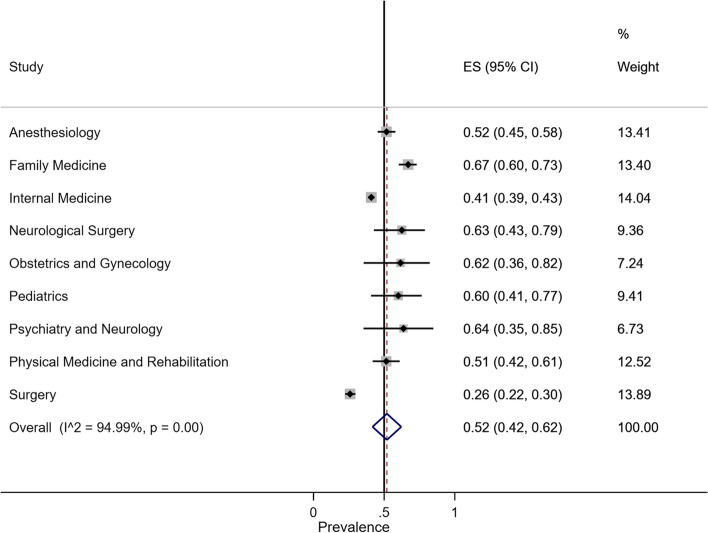
Prevalence of CAM acceptance
The overall random-effect pooled prevalence of CAM acceptance in medical specialty was 52% (95% CI, 42–62%). The prevalence of CAM acceptance in Family Medicine was 67% (95% CI, 60–73%), Psychiatry and Neurology was 64% (95% CI, 35–85%), Neurological Surgery was 63% (95% CI, 43–79%), Obstetrics and Gynecology was 62% (95% CI, 36–82%), Pediatrics was 60% (95% CI, 41–77%), Anesthesiology was 52% (95% CI, 45–58%), Physical Medicine and Rehabilitation was 51% (95% CI, 42–61%), Internal Medicine was 41% (95% CI, 39–43%), and Surgery was 26% (95% CI, 22–30%). The overall heterogeneity was significant (I2 = 94.99%, p value < 0.001) (Fig. 2).
Fig. 2.
Forest plot of CAM acceptance by specialty
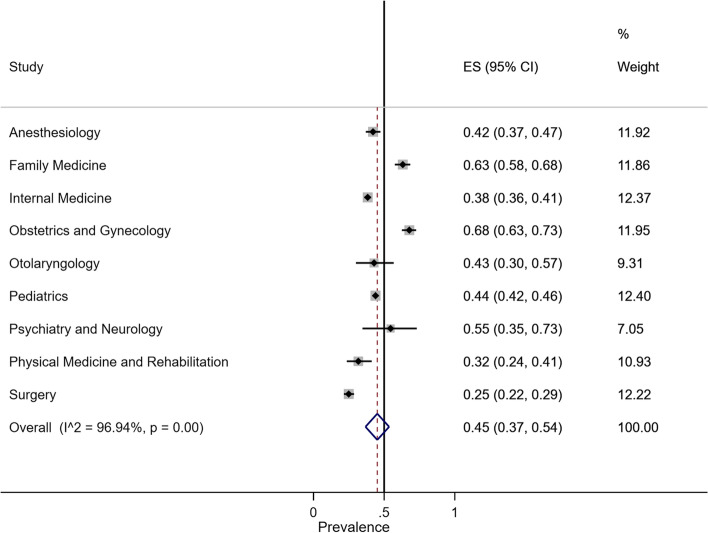
Prevalence of CAM usage
The overall random-effect pooled prevalence of CAM usage in medical specialty was 45% (95% CI, 37–54%). The prevalence of CAM usage in Obstetrics and Gynecology was 68% (95% CI, 63–73%), Family Medicine was 63% (95% CI, 58–68%), Psychiatry and Neurology was 55% (95% CI, 35–73%), Pediatrics was 44% (95% CI, 42–46%), Otolaryngology was 43% (95% CI, 30–57%), Anesthesiology was 42% (95% CI, 37–47%), Internal Medicine was 38% (95% CI, 36–41%), Physical Medicine and Rehabilitation was 32% (95% CI, 24–41%), and Surgery was 25% (95% CI, 22–29%). The overall heterogeneity was significant (I2 = 94.90%, p value < 0.001) (Fig. 3).
Fig. 3.
Forest plot of CAM usage by specialty
Based on the studies
Prevalence of CAM acceptance
The overall random-effect pooled prevalence of CAM acceptance was 54% (95% CI, 36–73%) (Fig. 4a). Twelve studies provided CAM acceptance: five studies in the European region, five studies in the region of the Americas, and two studies in the Western Pacific region. The pooled prevalence of the European region, region of the Americas, and Western Pacific region that accepted CAM were 60% (95% CI, 36–83%), 54% (95% CI, 39–68%), and 20% (95% CI, 17–22%), respectively (Fig. 4b). All 12 studies were done in high-income economic countries (Fig. 4c). Based on the sampling method, the pooled prevalence of random sampling method, and non-random sampling method were 54% (95% CI, 30–77%), and 55% (95% CI, 44–67%), respectively (Fig. 4d). The overall heterogeneity was significant (I2 = 99.14%, p value < 0.001) as was the between-group heterogeneity (p value < 0.001). Meta-regression showed that there were no significant differences in the pooled prevalence of CAM acceptance by region, economic levels of the country, and the sampling method (Table 3).
Fig. 4.
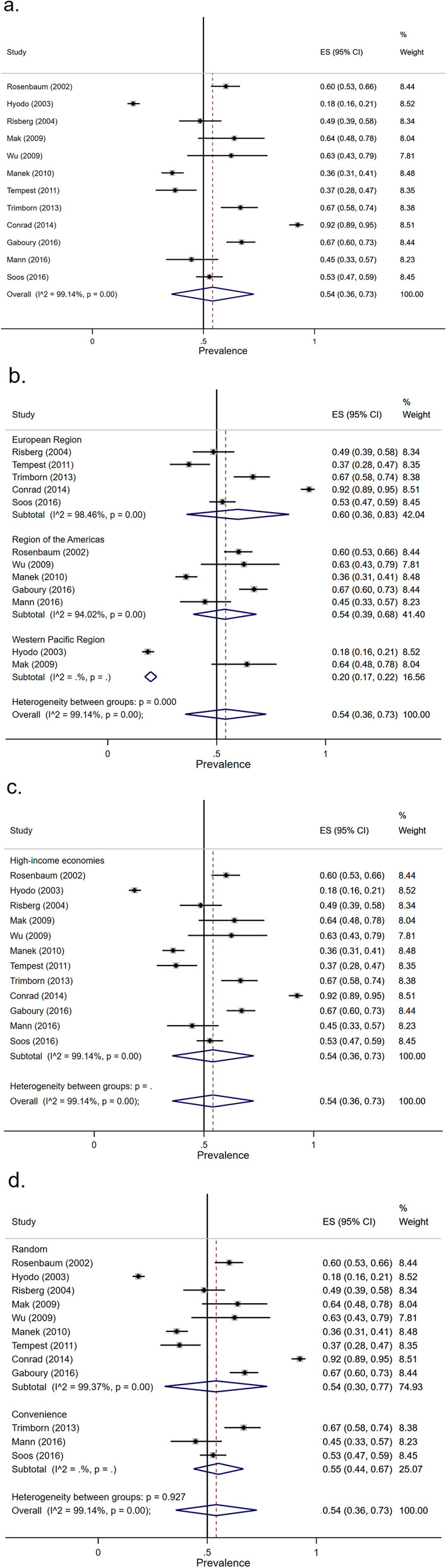
Forest plot of CAM acceptance
Table 3.
Subgroup analysis
| Subgroup | No. of studies (no. of MS) | Difference in pooled prevalence (95% CI) | p-value |
|---|---|---|---|
| CAM acceptance | |||
| Region | |||
| Region of the Americas | 5 (842) | 0.00 (-0.28, 0.27) | 0.979 |
| European Region | 5 (846) | 0.10 (-0.16, 0.36) | 0.405 |
| Western Pacific Region | 2 (787) | -0.18 (-0.51, 0.16) | 0.271 |
| Sampling method | |||
| Random sampling | 9 (2032) | -0.01 (-0.32, 0.30) | 0.943 |
| CAM usage | |||
| Region | |||
| Region of the Americas | 8 (2435) | 0.12 (-0.08, 0.31) | 0.222 |
| European Region | 9 (1460) | 0.04 (-0.16, 0.24) | 0.706 |
| Western Pacific Region | 3 (883) | -0.17 (-0.45, 0.10) | 0.204 |
| Mixed region | 1 (95) | -0.36 (-0.79, 0.07) | 0.098 |
| Economic levels of country | |||
| Upper-middle-income economies | 2 (195) | 0.24 (-0.08, 0.56) | 0.133 |
| High-income economies | 18 (4583) | -0.03 (-0.32, 0.25) | 0.804 |
| Mixed-income economies | 1 (95) | -0.36 (-0.79, 0.07) | 0.098 |
| Sampling method | |||
| Random sampling | 15 (4101) | -0.03 (-0.25, 0.19) | 0.802 |
Abbreviations: CI confidence interval
Prevalence of CAM usage
The overall random-effect pooled prevalence of CAM usage was 52% (95% CI, 42–62%) (Fig. 5a). Twenty-one studies provided CAM usage information: nine studies in the European region, eight studies in the region of the Americas, three studies in the Western Pacific region, and one study in the mixed region. The pooled prevalence of European region, region of the Americas, Western Pacific region, and mixed region that used CAM were 54% (95% CI, 37–71%), 59% (95% CI, 46–73%), 37% (95% CI, 18–56%), and 18% (95% CI, 11–27%), respectively (Fig 5b). All 18 studies were conducted in high-income economic countries, two studies were conducted in upper-middle-income economic countries, and one study was conducted in a mixed-income economic country. The pooled prevalence of high-income economic countries, upper-middle-income economic, and mixed-income economic countries that used CAM was 52% (95% CI, 41–62%), 74% (95% CI, 67–80%), and 18% (95% CI, 11–27%), respectively (Fig. 5c). Based on the sampling method, the pooled prevalence of the random sampling method, and non-random sampling method were 51% (95% CI, 39–64%), and 54% (95% CI, 38–70%), respectively (Fig. 5d). The overall heterogeneity was significant (I2 = 98.29%, p value < 0.001) as was between-group heterogeneity (p value < 0.001). Meta-regression showed that there were no significant differences in the pooled prevalence of CAM usage by region, economic levels of the country, and the sampling method (Table 3).
Fig. 5.
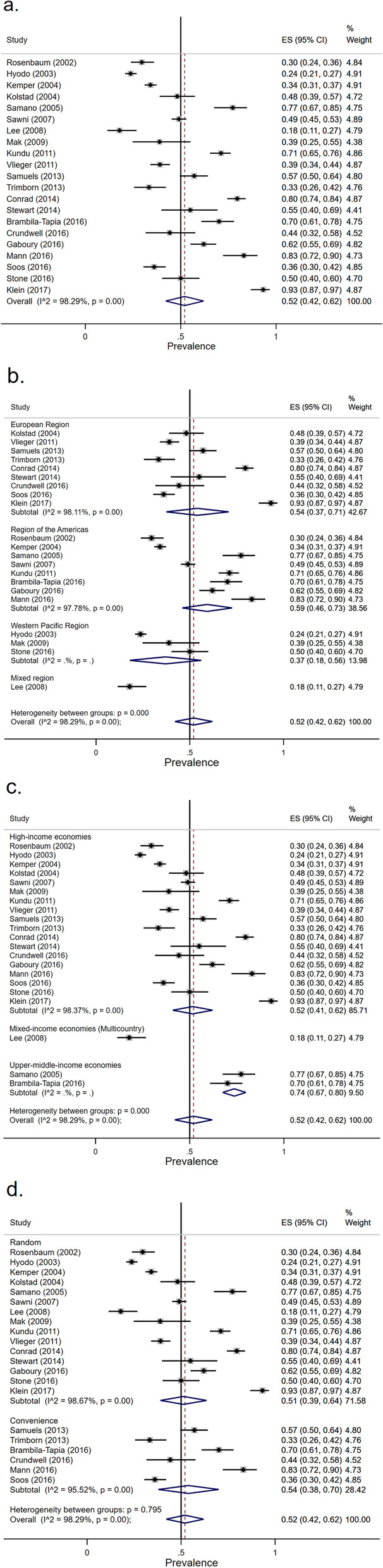
Forest plot of CAM usage
Assessment of study quality/risk of bias/conflict of interest
A total of 24 (96%) studies were categorized as high quality/low risk of bias, whereas one (4%) was categorized as moderate quality/moderate risk of bias. No study met the criteria of low quality/high risk of bias (Fig 6). Only five studies (20%) declared that there were conflicts of interest.
Fig. 6.
Study quality/risk of bias of the included studies
Discussion
This study is the first of its kind to compare the acceptance and use of CAM across various medical specialties in different contexts. As nearly three-quarters of the specialties accepted CAM more than 50% whereas nearly a third were using CAM more than 50%.
The synthesis of all prevalence estimates of acceptance and usage was 52% and 45%, respectively. The highest prevalence of acceptance was in Family Medicine, followed by Psychiatry and Neurology, Neurological Surgery, Obstetrics and Gynecology, Pediatrics, Anesthesiology, Physical Medicine and Rehabilitation, Internal Medicine, and Surgery. The highest prevalence of usage was in Obstetrics and Gynecology, followed by Family Medicine, Psychiatry and Neurology, Pediatrics, Otolaryngology, Anesthesiology, Internal Medicine, Physical Medicine and Rehabilitation, and Surgery. These findings were useful in terms of improving care plan, decision-making processes, and communication in terms of CAM between the doctors and the patients.
All of the medical specialties mentioned above had a higher prevalence of acceptance than the prevalence of CAM use, except for Obstetrics and Gynecology because the gynecologic oncologists have used CAM to treat a large number of breast cancer patients [14]. There was a small difference in the prevalence (<5%) between the acceptance and the usage in Family Medicine (4%), Obstetrics and Gynecology (4%), Internal Medicine (3%), and Surgery (1%).
A highest difference of prevalence of CAM acceptance and usage was in the field of Physical Medicine and Rehabilitation (19%). This difference may be due to the reduction in the use of acupuncture in the academic hospitals [7] as well as personal use. Nearly two thirds of the rehabilitation physicians advised against the use of CAM as a therapeutic option [41]. The lowest prevalence of acceptance and usage of CAM was observed in Surgery. This relatively low prevalence compared to other medical specialties may be due to the belief that CAM products were ineffective. Many surgeons lacked information regarding CAM usage.
The acceptance of CAM was neutral in European region and region of the Americas. The World Health Organization reported that the prevalence of CAM usage in the European region, region of the Americas, and Western Pacific region in 2018 was 89%, 80%, and 95%, respectively [33], while this review found that the corresponding prevalence was 54%, 59%, and 37%, respectively. The lower prevalence may be from the dominating studies that were conducted before 2010 whereas CAM has used more often after 2010.
The variation of prevalence of CAM used was investigated in relation to the economic level of the countries. There was a higher prevalence of CAM use in the upper-middle-income economies than the high-income economies which may be due to cultural, historical influences, and implementation of CAM in the national health system as seen in Brazil [39] and Mexico [49].
Our study has some limitations that should be considered when interpreting the findings. Only two databases—PubMed and Scopus—were included so this review might have missed some relevant studies that were indexed elsewhere. Nonetheless, both databases were considered efficiently sufficient and most relevant to our research question within a specific domain [53]. While Web of Science and Scopus share several common features, Scopus is a relatively smaller database but covers more modern studies than Web of Science. The included studies did not cover some medical specialties that might have different acceptance and usage of CAM. Therefore, the prevalence of acceptance and usage of CAM in these populations need additional surveys. The prevalence of acceptance in some specialties like Neurological Surgery, Obstetrics and Gynecology, Otolaryngology, Pediatrics, and Psychiatry and Neurology was reported by a single study, thus limiting the generality of such findings. High heterogeneity of acceptance and usage of CAM between medical specialty referred to the variation in professional characteristic and practice, measurement methods, and study questionnaire. Most of the studies were from high-income economic countries. There were no studies from low-middle and low-income economic countries which is of concern. We found that no studies compared the relevant demographic characteristics between the responders and non-responders that would increase non-response bias when estimating the prevalence of CAM use. Although most of the studies demonstrated low risk of bias, over 88% of the studies did not use a validated instrument. Finally, the conflict of interest was not declared in more than 80% of the studies which may result in unintentional bias in the collection, analysis, and interpretation of the data. This can consequently lead to claims that the CAM used was beneficial because the researcher and/or entity may have a financial or management interest in the CAM used.
Conclusions
Acceptance and use of CAM varied across medical specialties. Based on available survey data, CAM was accepted and used the most by Family Medicine but the least by Surgery. Findings from this systematic review could be useful for strategic harmonization of CAM and conventional medicine practice.
Supplementary Information
Additional file 2. The citation for the Synthesis Without Meta-analysis explanation and elaboration article is: Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J, Welch V, Thomson H. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline BMJ 2020;368:l6890 https://doi.org/10.1136/bmj.l6890.
Acknowledgements
We thank Dr. Kulthanit Wanaratna and Dr. Monthaka Teerachaisakul of the Department of Thai Traditional and Alternative Medicine, Ministry of Public Health for their administrative supports.
Authors’ contributions
Phutrakool P conceptualized and designed the study, collected the data, analyzed and interpreted the data, drafted the article, and finalized the manuscript for submission. Pongpirul K conceptualized and designed the study, collected the data, analyzed and interpreted the data, drafted the article, and finalized the manuscript for submission.
Funding
This study received financial support from the Ratchadapiseksompotch Fund, Faculty of Medicine, Chulalongkorn University (Grant Number RA62/059), and Department of Thai Traditional and Alternative Medicine, Ministry of Public Health. The sponsors have no involvement in the systematic search, abstract screening, data extraction, or manuscript preparation. Phutrakool P received the 90th anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Supported by Ratchadapiseksompotch Fund, Faculty of Medicine, Chulalongkorn University (Grant Number RA62/059), and Department of Thai Traditional and Alternative Medicine, Ministry of Public Health. The sponsors have no involvement in the systematic search, abstract screening, data extraction, or manuscript preparation. PRISMA 2009 Checklist statement: Uploaded
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO European health information at your fingertips. 2020; Available from: https://gateway.euro.who.int/en/indicators/hlthres_242-specialist-medical-practitioners-total/.
- 2.Complementary, Alternative, or Integrative Health: What’s In a Name? 2020; Available from: https://nccih.nih.gov/health/integrative-health.
- 3.Peltzer K, Pengpid S. Prevalence and determinants of traditional, complementary and alternative medicine provider use among adults from 32 countries. Chin J Integr Med. 2018;24(8):584–590. doi: 10.1007/s11655-016-2748-y. [DOI] [PubMed] [Google Scholar]
- 4.Asadi-Pooya AA, et al. Complementary and alternative medicine in epilepsy: a global survey of physicians' opinions. Epilepsy Behav. 2021;117:107835. doi: 10.1016/j.yebeh.2021.107835. [DOI] [PubMed] [Google Scholar]
- 5.Kolstad A, et al. Use of complementary and alternative therapies: a national multicentre study of oncology health professionals in Norway. Support Care Cancer. 2004;12(5):312–318. doi: 10.1007/s00520-004-0590-9. [DOI] [PubMed] [Google Scholar]
- 6.Manek NJ, et al. What rheumatologists in the United States think of complementary and alternative medicine: results of a national survey. BMC Complement Altern Med. 2010;10:5. doi: 10.1186/1472-6882-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mann B, Burch E, Shakeshaft C. Attitudes toward acupuncture among pain fellowship directors. Pain Med. 2016;17(3):494–500. doi: 10.1093/pm/pnv001. [DOI] [PubMed] [Google Scholar]
- 8.Trimborn A, et al. Attitude of employees of a university clinic to complementary and alternative medicine in oncology. Ann Oncol. 2013;24(10):2641–2645. doi: 10.1093/annonc/mdt299. [DOI] [PubMed] [Google Scholar]
- 9.Babbar S, Williams KB, Maulik D. Complementary and alternative medicine use in modern obstetrics: a survey of the central Association of Obstetricians & gynecologists members. J Evid Based Complement Altern Med. 2017;22(3):429–435. doi: 10.1177/2156587216671215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crundwell G, Baguley DM. Attitudes towards and personal use of complementary and alternative medicine amongst clinicians working in audiovestibular disciplines. J Laryngol Otol. 2016;130(8):730–733. doi: 10.1017/S0022215116008471. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, et al. Using a survey to characterize rehabilitation Professionals' perceptions and use of complementary, integrative, and alternative medicine. J Altern Complement Med. 2020;26(8):663–665. doi: 10.1089/acm.2019.0383. [DOI] [PubMed] [Google Scholar]
- 12.Land MH, Wang J. Complementary and alternative medicine use among allergy practices: results of a Nationwide survey of allergists. J Allergy Clin Immunol Pract. 2018;6(1):95–98 e3. doi: 10.1016/j.jaip.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Stub T, et al. Complementary and conventional providers in cancer care: experience of communication with patients and steps to improve communication with other providers. BMC Complement Altern Med. 2017;17(1):301. doi: 10.1186/s12906-017-1814-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klein E, et al. Gynecologic oncologists' attitudes and practices relating to integrative medicine: results of a nationwide AGO survey. Arch Gynecol Obstet. 2017;296(2):295–301. doi: 10.1007/s00404-017-4420-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee RT, et al. An international pilot study of oncology physicians' opinions and practices on complementary and alternative medicine (CAM) Integr Cancer Ther. 2008;7(2):70–75. doi: 10.1177/1534735408319059. [DOI] [PubMed] [Google Scholar]
- 16.Joseph K, et al. Outcome analysis of breast cancer patients who declined evidence-based treatment. World J Surg Oncol. 2012;10:118. doi: 10.1186/1477-7819-10-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson SB, et al. Use of alternative medicine for cancer and its impact on survival. JNCI: J Natl Cancer Inst. 2018;110(1):121–124. doi: 10.1093/jnci/djx145. [DOI] [PubMed] [Google Scholar]
- 18.Xing X, et al. Traditional Chinese medicine bundle therapy for septic acute gastrointestinal injury: a multicenter randomized controlled trial. Complement Ther Med. 2019;47:102194. doi: 10.1016/j.ctim.2019.102194. [DOI] [PubMed] [Google Scholar]
- 19.Lanski SL, et al. Herbal therapy use in a pediatric emergency department population: expect the unexpected. Pediatrics. 2003;111(5 Pt 1):981–985. doi: 10.1542/peds.111.5.981. [DOI] [PubMed] [Google Scholar]
- 20.Callahan LF, et al. Use of complementary and alternative medicine among patients with arthritis. Prev Chronic Dis. 2009;6(2):A44. [PMC free article] [PubMed] [Google Scholar]
- 21.Chase DM, et al. Appropriate use of complementary and alternative medicine approaches in gynecologic cancers. Curr Treat Options in Oncol. 2014;15(1):14–26. doi: 10.1007/s11864-013-0269-x. [DOI] [PubMed] [Google Scholar]
- 22.Bauml JM, et al. Do attitudes and beliefs regarding complementary and alternative medicine impact its use among patients with cancer? A cross-sectional survey. Cancer. 2015;121(14):2431–2438. doi: 10.1002/cncr.29173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Godin G, et al. Intention to encourage complementary and alternative medicine among general practitioners and medical students. Behav Med. 2007;33(2):67–77. doi: 10.3200/BMED.33.2.67-79. [DOI] [PubMed] [Google Scholar]
- 24.Chen L, et al. A survey of selected physician views on acupuncture in pain management. Pain Med. 2010;11(4):530–534. doi: 10.1111/j.1526-4637.2010.00815.x. [DOI] [PubMed] [Google Scholar]
- 25.Chang KH, et al. Complementary and alternative medicine use in oncology: a questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11:196. doi: 10.1186/1471-2407-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gardiner P, et al. Family medicine residency program directors attitudes and knowledge of family medicine CAM competencies. Explore (NY) 2013;9(5):299–307. doi: 10.1016/j.explore.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jakovljevic MB, et al. Cross-sectional survey on complementary and alternative medicine awareness among health care professionals and students using CHBQ questionnaire in a Balkan country. Chin J Integr Med. 2013;19(9):650–655. doi: 10.1007/s11655-013-1434-6. [DOI] [PubMed] [Google Scholar]
- 28.Loh KP, et al. Medical students' knowledge, perceptions, and interest in complementary and alternative medicine. J Altern Complement Med. 2013;19(4):360–366. doi: 10.1089/acm.2012.0014. [DOI] [PubMed] [Google Scholar]
- 29.Munstedt K, et al. Complementary and alternative medicine (CAM) in obstetrics and gynaecology: a survey of office-based obstetricians and gynaecologists regarding attitudes towards CAM, its provision and cooperation with other CAM providers in the state of Hesse, Germany. Arch Gynecol Obstet. 2014;290(6):1133–1139. doi: 10.1007/s00404-014-3315-4. [DOI] [PubMed] [Google Scholar]
- 30.Campbell M, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoy D, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 32.American Board of Medical Specialty . ABMS guide to medical specialties. 2019. [Google Scholar]
- 33.World Health Organization . WHO global report on traditional and complementary medicine 2019. 2019. [Google Scholar]
- 34.World Bank . World Bank country and lending groups. 2019. [Google Scholar]
- 35.Rosenbaum ME, et al. Academic physicians and complementary and alternative medicine: an institutional survey. Am J Med Qual. 2002;17(1):3–9. doi: 10.1177/106286060201700102. [DOI] [PubMed] [Google Scholar]
- 36.Hyodo I, et al. Perceptions and attitudes of clinical oncologists on complementary and alternative medicine: a nationwide survey in Japan. Cancer. 2003;97(11):2861–2868. doi: 10.1002/cncr.11402. [DOI] [PubMed] [Google Scholar]
- 37.Kemper KJ, O'Connor KG. Pediatricians' recommendations for complementary and alternative medical (CAM) therapies. Ambul Pediatr. 2004;4(6):482–487. doi: 10.1367/A04-050R.1. [DOI] [PubMed] [Google Scholar]
- 38.Risberg T, et al. Knowledge of and attitudes toward complementary and alternative therapies; a national multicentre study of oncology professionals in Norway. Eur J Cancer. 2004;40(4):529–535. doi: 10.1016/j.ejca.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 39.Samano ES, et al. Use of complementary and alternative medicine by Brazilian oncologists. Eur J Cancer Care (Engl) 2005;14(2):143–148. doi: 10.1111/j.1365-2354.2005.00524.x. [DOI] [PubMed] [Google Scholar]
- 40.Sawni A, Thomas R. Pediatricians' attitudes, experience and referral patterns regarding complementary/alternative medicine: a national survey. BMC Complement Altern Med. 2007;7:18. doi: 10.1186/1472-6882-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mak JC, et al. Perceptions and attitudes of rehabilitation medicine physicians on complementary and alternative medicine in Australia. Intern Med J. 2009;39(3):164–169. doi: 10.1111/j.1445-5994.2008.01734.x. [DOI] [PubMed] [Google Scholar]
- 42.Wu C, et al. A survey of complementary and alternative medicine (CAM) awareness among neurosurgeons in Washington state. J Altern Complement Med. 2009;15(5):551–555. doi: 10.1089/acm.2008.0427. [DOI] [PubMed] [Google Scholar]
- 43.Kundu A, et al. Attitudes, patterns of recommendation, and communication of pediatric providers about complementary and alternative medicine in a large metropolitan children's hospital. Clin Pediatr (Phila) 2011;50(2):153–158. doi: 10.1177/0009922810384724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tempest H, et al. Acupuncture in urological practice--a survey of urologists in England. Complement Ther Med. 2011;19(1):27–31. doi: 10.1016/j.ctim.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 45.Vlieger AM, van Vliet, Jong MC. Attitudes toward complementary and alternative medicine: a national survey among paediatricians in the Netherlands. Eur J Pediatr. 2011;170(5):619–624. doi: 10.1007/s00431-010-1331-3. [DOI] [PubMed] [Google Scholar]
- 46.Samuels N, et al. Use of and attitudes toward complementary and alternative medicine among obstetricians in Israel. Int J Gynaecol Obstet. 2013;121(2):132–136. doi: 10.1016/j.ijgo.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 47.Conrad AC, et al. Attitudes of members of the German Society for Palliative Medicine toward complementary and alternative medicine for cancer patients. J Cancer Res Clin Oncol. 2014;140(7):1229–1237. doi: 10.1007/s00432-014-1656-9. [DOI] [PubMed] [Google Scholar]
- 48.Stewart D, et al. Healthcare professional views and experiences of complementary and alternative therapies in obstetric practice in north East Scotland: a prospective questionnaire survey. Bjog. 2014;121(8):1015–1019. doi: 10.1111/1471-0528.12618. [DOI] [PubMed] [Google Scholar]
- 49.Brambila-Tapia AJ, et al. Attitudes, knowledge, use, and recommendation of complementary and alternative medicine by health professionals in Western Mexico. Explore (NY) 2016;12(3):180–187. doi: 10.1016/j.explore.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 50.Gaboury I, et al. Complementary and alternative medicine: do physicians believe they can meet the requirements of the college des medecins du Quebec? Can Fam Physician. 2016;62(12):e772–e775. [PMC free article] [PubMed] [Google Scholar]
- 51.Soos SA, et al. Complementary and alternative medicine: attitudes, knowledge and use among surgeons and anaesthesiologists in Hungary. BMC Complement Altern Med. 2016;16(1):443. doi: 10.1186/s12906-016-1426-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stone AB, et al. Are anesthesia providers ready for hypnosis? Anesthesia Providers' attitudes toward hypnotherapy. Am J Clin Hypn. 2016;58(4):411–418. doi: 10.1080/00029157.2015.1136589. [DOI] [PubMed] [Google Scholar]
- 53.Albahri AS, et al. IoT-based telemedicine for disease prevention and health promotion: state-of-the-art. J Netw Comput Appl. 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. The citation for the Synthesis Without Meta-analysis explanation and elaboration article is: Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J, Welch V, Thomson H. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline BMJ 2020;368:l6890 https://doi.org/10.1136/bmj.l6890.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.