Glucocorticoids are common and powerful antiinflammatory medications. Because of their myriad effects on the immune system, they are capable of both facilitating infections and ameliorating their outcomes. In pulmonary medicine, chronic oral glucocorticoid therapy is a well-recognized risk factor for infections such as Pneumocystis pneumonia. However, glucocorticoids also serve as adjunctive treatment for severe Pneumocystis pneumonia, coronavirus disease (COVID-19) pneumonia, and chronic obstructive pulmonary disease (COPD) exacerbations. The appropriate use of inhaled glucocorticoids in chronic inflammatory lung diseases is similarly complex. Inhaled corticosteroids (ICS) are the first line of therapy for asthma, for which they improve outcomes, but their use in COPD is much more complicated. Current Global Initiative for Chronic Obstructive Lung Disease guidelines (1) recommend restricting ICS use to patients with a significant history of COPD exacerbations or peripheral eosinophilia because of the increased risk of pneumonia seen with these drugs in COPD. Thus, in COPD, we recognize that although glucocorticoids prevent and treat COPD exacerbations, they also increase the risk of pulmonary infection.
Several studies have attempted to understand the biological mechanisms by which chronic ICS use increases the risk of pneumonia in COPD, focusing, for example, on blunting of IFN responses to viruses, inhibition of macrophage-mediated bacterial clearance, and downregulation of major histocompatibility complex class II molecules (2, 3). In addition, ICS can suppress antimicrobial peptides driving the expansion of streptococci within the microbiota in mice (4). Interestingly, lower levels of some antimicrobial peptides, such as cathelicidin, are associated with increased severity of COPD exacerbations (4). In sputum samples, ICS use is associated with increased bacterial load (5) and reduced alpha diversity with increased abundance of Proteobacteria, a phylum with several common respiratory pathogens such as Haemophilus and Moraxella species (6–8). Aside from these associations with specific respiratory pathogens, other components of the respiratory microbiota are also associated with the use of ICS in COPD (9–11). When evaluated more closely, however, the antiinflammatory effects of ICS may have contrasting effects on both the lung microbiome and susceptibility to respiratory pathogens (Figure 1). On one hand, ICS use decreases airway mucus production, which improves airway clearance and decreases the availability of bacterial nutrients. This could result in reduced airway bacterial load and decreased susceptibility to respiratory pathogens. On the other hand, the effects of ICS on antibacterial peptides could lead to increased bacterial growth, promoting bacterial dominance (reduced diversity) and increasing susceptibility to pathogens. Thus, to better understand the effects of ICS use on the risk for respiratory pathogens, we need to evaluate the effects of these drugs on the respiratory microbiome as well as the host. With the growth of culture-independent approaches to characterize the lung microbiome, we now have the opportunity to explore the clinical impact of respiratory medications and determine their effect on the airway microbiota. The existing literature using upper airway or sputum samples suggests that ICS use may increase viral load, increase microbiome diversity, and increase potential respiratory pathogens. However, a major limitation in this area is the lack of randomized controlled studies of ICS use to evaluate longitudinal changes in the lower airway microbiota.
Figure 1.
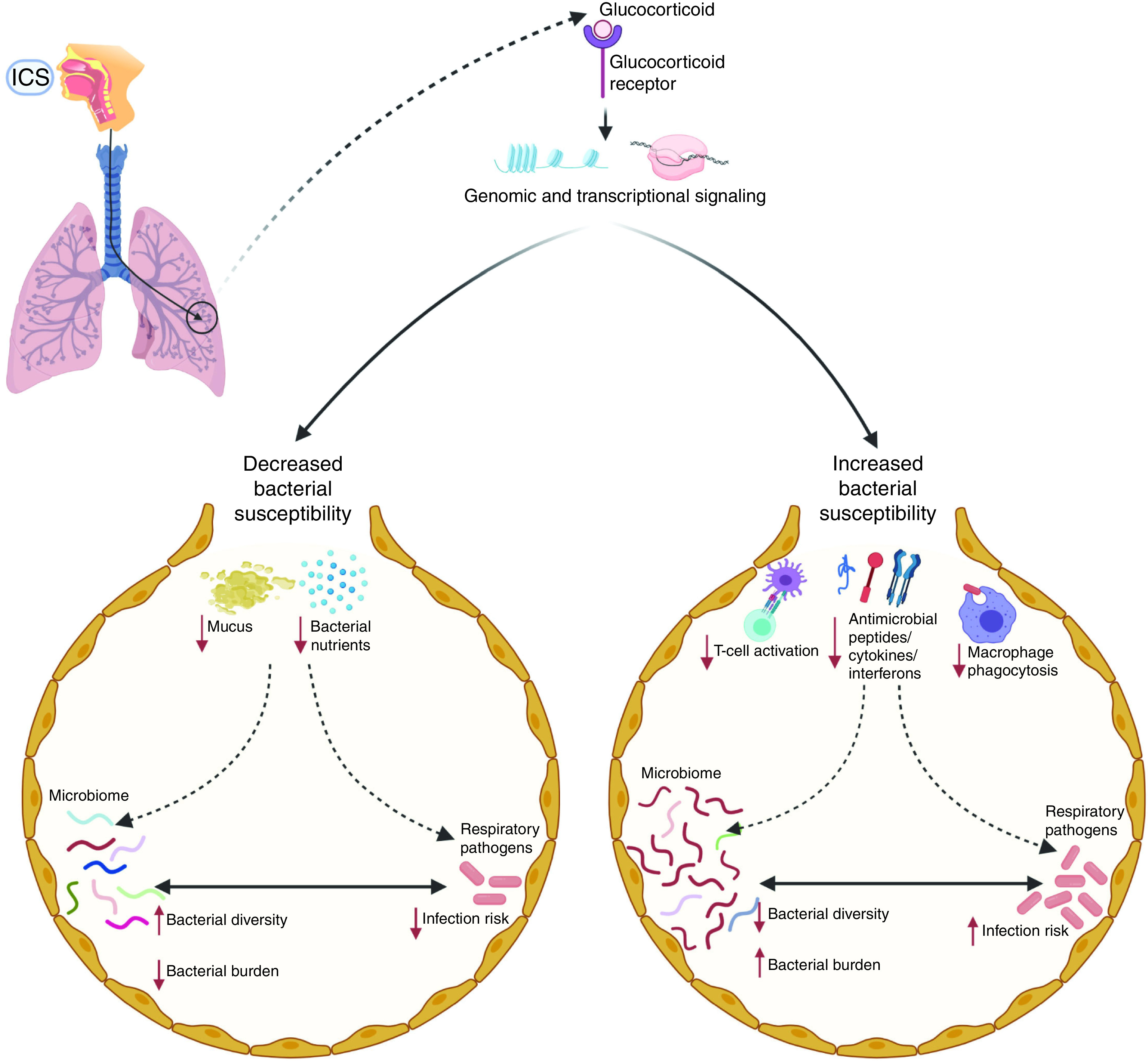
Schematic representation of the potentially dichotomous role of inhaled corticosteroids (ICS) in the lower airway microbial host interphase in chronic obstructive pulmonary disease. On the left, ICS use reduces host susceptibility to microbes by reducing mucus secretion and bacterial nutrients, which can lead to a decrease in microbial burden and a more diverse microbiota. On the right, ICS affects the immune response with suppression of antimicrobial molecules, macrophage phagocytosis, and blunting IFN responses. These effects can collectively lead to the “blooming” of certain microbes within the lung microbiota (thus reducing diversity) and increase the risk of infection.
In the current issue of the Journal, Leitao Filho and colleagues (pp. 1143–1152) address some of these limitations with a randomized trial of the effects of ICS plus long-acting β2-agonist (LABA) therapy versus LABA alone on the clinically stable COPD lung microbiome (12). All participants underwent a 4-week run-in period during which they discontinued ICS use and initiated a LABA (formoterol). After the run-in period, participants underwent baseline bronchoscopy for microbiome sampling and were then randomized 1:1:1 to budesonide/formoterol, fluticasone propionate/salmeterol, or formoterol alone for 12 weeks. A follow-up bronchoscopy for microbiome sampling was performed 12 weeks after randomization. The primary study outcome was a change in the lung microbiome alpha diversity (intrasample taxonomic diversity) or microbiome composition over 12 weeks of treatment between the ICS/LABA groups and the LABA-only group. Although the authors did not demonstrate significant changes in these microbiome measures as a result of ICS/LABA versus LABA use, they observed that fluticasone/salmeterol treatment was associated with a relative reduction in alpha diversity compared with the formoterol alone group. These results appear to be due to the unexpected increase in alpha diversity among the control (LABA only) group during the 12-week treatment duration despite the 4-week run-in period. In secondary analyses, longitudinal changes in the alpha diversity of the airway microbiome were positively correlated with increased post-bronchodilator FEV1. These data suggest that the loss of microbial community diversity may be an important factor in the responsiveness to bronchodilators. In addition, the fluticasone/salmeterol group had a greater number of microbial shifts from baseline compared with both formoterol and budesonide/formoterol. The authors did not see similar trends in the budesonide/formoterol group, indicating that some of these observations might be specific to the steroid or LABA formulation rather than class effects.
Of course, this study also has several limitations, which provide opportunities for further work. The authors may have been underpowered to detect differences in the lower airway microbiota, particularly in their subgroup analyses comparing ICS/LABA formulations, a major challenge for studies requiring invasive procedures. Prior ICS use was not evenly distributed among all three groups, and this imbalance may have influenced some of the baseline results. A sizeable minority of subjects dropped out during the run-in period, perhaps because they did not tolerate ICS withdrawal. We therefore remain unaware of potentially significant microbiome responses among subjects who could not tolerate ICS withdrawal. Furthermore, differences in LABA formulation, drug delivery device, and steroid potency were present across the three groups and may have influenced the study findings (13).
Given the multiple mechanisms by which glucocorticoids influence the immune system and the paradoxical benefits and harms of ICS therapy in stable COPD, it should come as no surprise that Leitao Filho and colleagues did not observe a clear uniform ICS-associated signal in their lung microbiome samples. Nevertheless, this paper moves the field of human interventional lung microbiome studies forward. Longitudinal lower airway microbiome sampling from human subjects with moderate or severe COPD in a randomized controlled fashion is a significant accomplishment. An important consideration for future research should be concomitant evaluation of host inflammatory endotype. Longitudinal studies using more advanced high-throughput multiomic technologies that can simultaneously evaluate both the host and microbial environment have the capacity to better characterize the impact of chronic therapies on the microbiome in COPD. As a proof of concept, a randomized controlled trial of azithromycin in early COPD showed that part of the antiinflammatory effect of macrolides might be driven by their effects on the lower airway microbiome by affecting the production of antiinflammatory metabolites of bacterial origin (14). Such studies may offer the possibility to directly analyze the interaction between the microbiota and the host, leading to identification of treatable traits and personalized approaches, such as identification of subjects with greater chances to benefit from ICS.
As we learn more about the risks and benefits of ICS use in COPD, there is mounting evidence that ICS alter the lung microbiome via multiple mechanisms. This study represents the first attempt to address the outcome of ICS use on the lower airway microbiome in a longitudinal, randomized, and controlled fashion. As we work to decrease the risks and maximize the benefits of ICS use, microbiome-based personalized medicine approaches may help us understand who benefits most from ICS use.
Footnotes
Supported by NIH grant R01 HL125816.
Originally Published in Press as DOI: 10.1164/rccm.202109-2024ED on September 23, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J . 2019;53:1900164. doi: 10.1183/13993003.00164-2019. [DOI] [PubMed] [Google Scholar]
- 2. Stolberg VR, McCubbrey AL, Freeman CM, Brown JP, Crudgington SW, Taitano SH, et al. Glucocorticoid-augmented efferocytosis inhibits pulmonary pneumococcal clearance in mice by reducing alveolar macrophage bactericidal function. J Immunol . 2015;195:174–184. doi: 10.4049/jimmunol.1402217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. van de Garde MD, Martinez FO, Melgert BN, Hylkema MN, Jonkers RE, Hamann J. Chronic exposure to glucocorticoids shapes gene expression and modulates innate and adaptive activation pathways in macrophages with distinct changes in leukocyte attraction. J Immunol . 2014;192:1196–1208. doi: 10.4049/jimmunol.1302138. [DOI] [PubMed] [Google Scholar]
- 4. Singanayagam A, Glanville N, Cuthbertson L, Bartlett NW, Finney LJ, Turek E, et al. Inhaled corticosteroid suppression of cathelicidin drives dysbiosis and bacterial infection in chronic obstructive pulmonary disease. Sci Transl Med . 2019;11:eaav3879. doi: 10.1126/scitranslmed.aav3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Garcha DS, Thurston SJ, Patel AR, Mackay AJ, Goldring JJ, Donaldson GC, et al. Changes in prevalence and load of airway bacteria using quantitative PCR in stable and exacerbated COPD. Thorax . 2012;67:1075–1080. doi: 10.1136/thoraxjnl-2012-201924. [DOI] [PubMed] [Google Scholar]
- 6. Wang Z, Bafadhel M, Haldar K, Spivak A, Mayhew D, Miller BE, et al. Lung microbiome dynamics in COPD exacerbations. Eur Respir J . 2016;47:1082–1092. doi: 10.1183/13993003.01406-2015. [DOI] [PubMed] [Google Scholar]
- 7. Huang YJ, Sethi S, Murphy T, Nariya S, Boushey HA, Lynch SV. Airway microbiome dynamics in exacerbations of chronic obstructive pulmonary disease. J Clin Microbiol . 2014;52:2813–2823. doi: 10.1128/JCM.00035-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Contoli M, Pauletti A, Rossi MR, Spanevello A, Casolari P, Marcellini A, et al. Long-term effects of inhaled corticosteroids on sputum bacterial and viral loads in COPD. Eur Respir J. 2017;50:1700451. doi: 10.1183/13993003.00451-2017. [DOI] [PubMed] [Google Scholar]
- 9. Pragman AA, Kim HB, Reilly CS, Wendt C, Isaacson RE. The lung microbiome in moderate and severe chronic obstructive pulmonary disease. PLoS One . 2012;7:e47305. doi: 10.1371/journal.pone.0047305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pragman AA, Knutson KA, Gould TJ, Hodgson SW, Isaacson RE, Reilly CS, et al. Chronic obstructive pulmonary disease upper airway microbiome is associated with select clinical characteristics. PLoS One . 2019;14:e0219962. doi: 10.1371/journal.pone.0219962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pragman AA, Kim HB, Reilly CS, Wendt C, Isaacson RE. Chronic obstructive pulmonary disease lung microbiota diversity may be mediated by age or inhaled corticosteroid use. J Clin Microbiol . 2015;53:1050. doi: 10.1128/JCM.03320-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leitao Filho FS, Takiguchi H, Akata K, Ra SW, Moon J-Y, Kim HK, et al. Effects of inhaled corticosteroid/long-acting β2-agonist combination on the airway microbiome of patients with chronic obstructive pulmonary disease: a randomized controlled clinical trial (DISARM) Am J Respir Crit Care Med . 2021;204:1143–1152. doi: 10.1164/rccm.202102-0289OC. [DOI] [PubMed] [Google Scholar]
- 13. Hozawa S, Terada M, Hozawa M. Comparison of budesonide/formoterol Turbuhaler with fluticasone/salmeterol Diskus for treatment effects on small airway impairment and airway inflammation in patients with asthma. Pulm Pharmacol Ther . 2011;24:571–576. doi: 10.1016/j.pupt.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 14. Segal LN, Clemente JC, Wu BG, Wikoff WR, Gao Z, Li Y, et al. Randomised, double-blind, placebo-controlled trial with azithromycin selects for anti-inflammatory microbial metabolites in the emphysematous lung. Thorax . 2017;72:13–22. doi: 10.1136/thoraxjnl-2016-208599. [DOI] [PMC free article] [PubMed] [Google Scholar]


