To the Editor:
Crisis Standards of Care are defined as a “substantial change in health care operations” made necessary by an overwhelming public health emergency (1). The coronavirus disease (COVID-19) pandemic has created such a crisis in many countries around the world, forcing the rationing of life-saving care. Although published triage systems share some common procedures, the driving ethical principles and resulting rationing algorithms vary widely across the world and within the United States (2). Italian ICUs used age-based cutoffs (3), but most U.S. protocols do not include age as a primary criterion, instead ranking patients based on objective outcome predictors like the Sequential Organ Failure Assessment (SOFA) score or the presence of comorbidities (2, 4, 5).
Although there is an active theoretical debate over these protocols, there have been few empirical assessments of their performance (6, 7). We performed a Monte Carlo simulation of a severe ventilator shortage in a diverse, multicenter population of critically ill patients with COVID-19 receiving mechanical ventilation. The study objective was to assess the impact of four triage strategies on ventilator allocation and survival to hospital discharge across racial and ethnic groups and age.
Methods
The study included all critically ill adult patients with laboratory-confirmed COVID-19 who received mechanical ventilation at three healthcare settings in the greater Chicagoland area between March 2020 and February 2021. We extracted age, sex, self-identified racial and ethnic identity, International Classification of Diseases version 10 (ICD-10) codes for preexisting comorbidities, and SOFA score components from the electronic health record. We calculated each patient’s 24-hour maximum SOFA and used ICD-10 codes to identify a “severe” comorbidity Elixhauser threshold corresponding to a 90% predicted 1-year mortality (8).
We evaluated four ventilator allocation protocols: 1) lottery; 2) youngest first; 3) SOFA only; and 4) multiprinciple (Table 1). The SOFA-only protocol assigns priority tiers by SOFA score, with ties broken through a lottery (4). The multiprinciple protocol calculates priority scores based on categorical tiers of SOFA and the presence of severe comorbidities, with ties broken by age group (5).
Table 1.
Ventilator Allocation Protocols and Lives Saved under a 50% Ventilator Shortage
| Protocol | Rules | Average Survival (%) |
Survival by Race (%) |
Allocation by Race (%) |
||||
|---|---|---|---|---|---|---|---|---|
| Black | White | Hispanic | Black | White | Hispanic | |||
| Lottery | Random assignment | 31 (30–33) | 31 (27–35) | 31 (27–34) | 32 (27–36) | 50 (45–54) | 50 (46–54) | 50 (44–55) |
| Youngest first |
Rank by age | 35 (34–36) | 35 (32–38) | 28* (25–31) | 42† (38–45) | 50 (47–54) | 41* (37–44) | 61† (57–65) |
| SOFA only | Three SOFA tiers: | 33 (32–34) | 29* (26–32) | 36 (32–39) | 35 (31–38) | 44* (40–48) | 54† (50–58) | 53 (49–58) |
| Red: ⩽7 | ||||||||
| Yellow: 8–11 | ||||||||
| Blue: >11 | ||||||||
| Lottery tiebreaker | ||||||||
| Multiprinciple | SOFA category points: | 34 (32–35) | 29* (26–32) | 34 (31–37) | 38† (35–42) | 42* (39–46) | 51 (48–55) | 58† (54–62) |
| 1: ⩽8 | ||||||||
| 2: 9–11 | ||||||||
| 3: 12–14 | ||||||||
| 4: >14 | ||||||||
| Chronic conditions: +3 points if “severe” | ||||||||
| Age tiebreaker‡ | ||||||||
Definition of abbreviation: SOFA = Sequential Organ Failure Assessment.
Ventilator allocation protocols, average survival, survival by race/ethnicity, and allocation by race/ethnicity are presented. Allocation protocols were adapted from published state protocols, and SOFA categories used reflect the categories as defined in these blueprint protocols.
Data are presented as mean and 95% confidence intervals. The survival is measured by percentage of patients who survived to hospital discharge under a 50% ventilator shortage. Shortage of 50% indicates that only one ventilator is available for every two patients requiring mechanical ventilation. We assumed all patients who were not allocated a ventilator died.
Statistically significant lower survival or allocation in the racial/ethnic group than the average for the protocol (P < 0.05)
Statistically significant higher survival or allocation in the racial/ethnic group than the average for the protocol (P < 0.05)
Tiebreaker with age categories adapted from published protocols: 0–49, 50–69, 70–84, and ⩾85. If a simulated patient pair remained tied after applying the age tiebreaker, a lottery tiebreaker was applied.
The primary outcome was survival to hospital discharge estimated with a Monte Carlo simulation model. For each protocol, the model simulates a 50% ventilator shortage by 1) randomly subsampling two patients, 2) comparing their priority scores based on the protocol, 3) assigning the ventilator to the higher-priority patient, and 4) repeating this process until all study patients are sampled. We calculated the lives saved in each simulation by observing the actual survival to hospital discharge of patients assigned ventilators, assuming that patients who were not allocated a ventilator did not survive. We repeated the simulation 1,000 times for each protocol and compared the mean survival to hospital discharge between protocols overall and by age, race, and ethnicity using t tests. Significance tests were two sided with a P value threshold of <0.05.
Results
During the study period, there were 998 patients with laboratory-confirmed COVID-19 who received mechanical ventilation. The median age was 64 years (interquartile range, 53–73 yr) and mortality rate was 37.8%. The cohort was 32.2% non-Hispanic Black, 32.4% non-Hispanic White, 26.9% Hispanic, and 8.5% other. Hispanic patients (mean 56.0 yr) were significantly younger than Black patients (61.7 yr), and both groups were significantly younger than White patients (66.5 yr). Using maximum SOFA score in the first 24 hours of ICU admission, Black patients had a significantly higher score (mean 9.2) compared with Hispanic (7.5) and White patients (7.5). Black patients had higher rates of severe comorbidities (20.9%), compared with Hispanic (9.3%) and White patients (9.3%) (P < 0.001 for all comparisons above).
Under the SOFA-only protocol (score range 1–3), the mean score for Black patients was 1.95 compared with 1.67 for Hispanic patients and 1.64 for White patients. SOFA-only used a lottery tiebreaker for 18% of simulated patient pairs. Under the multiprinciple protocol (score range 1–7), the mean score was 2.59 for Black patients compared with 1.91 for Hispanic patients and 1.87 for White patients. This protocol used an age tiebreaker 15% of the time and the lottery tiebreaker 5% of the time.
When simulating a 50% ventilator shortage, the youngest-first protocol was associated with a significantly higher survival rate (34.7%) compared with all other protocols (Table 1). The multiprinciple protocol (33.5%) and the SOFA-only protocol (32.9%) had significantly higher survival than random ventilator allocation with a lottery (31.1%).
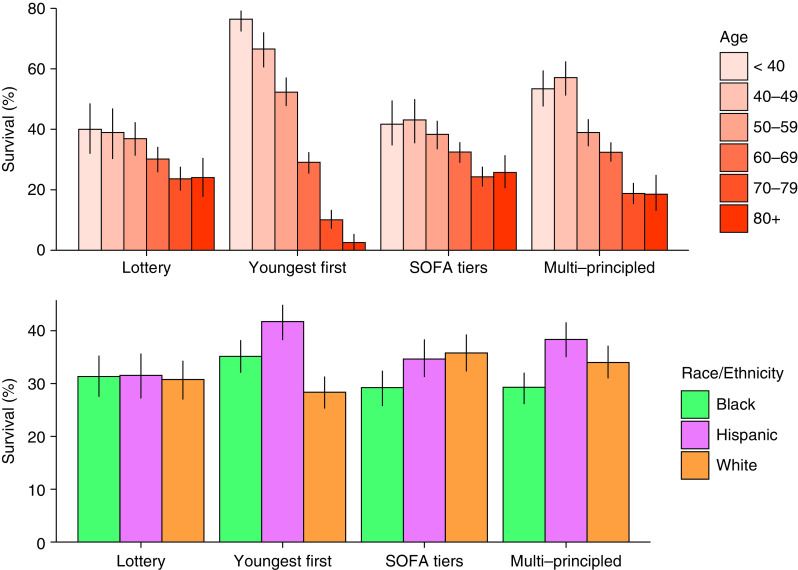
When ventilators were randomly assigned, there were no significant differences in survival in Black, White, or Hispanic patients compared with average survival (Figure 1). Black patients were less likely to receive a ventilator and had lower survival in both the SOFA-only (29% vs. 33%, P = 0.03) and multiprinciple protocols (29% vs. 34%, P = 0.008) but had average allocation and survival in the youngest-first protocol. Hispanic patients were more likely to receive a ventilator and had higher survival in the youngest-first (42% vs. 35%, P < 0.001) and multiprinciple protocol (38% vs. 34%, P = 0.007). White patients were more likely to be allocated ventilators in the SOFA-only protocol, but this did not lead to significantly higher survival.
Figure 1.
Survival to hospital discharge by age, race, and ethnicity by allocation protocol in a Monte Carlo simulation of a 50% ventilator shortage. Black refers to non-Hispanic Black patients and White refers to non-Hispanic White patients. In lottery allocation, survival was 40% in patients younger than 40 years compared with 24% in patients 80 years or older. In youngest-first, survival was 76% in patients younger than 40 years compared with 2.6% in patients 80 years or older. In the multiprinciple protocol with an age tiebreaker, survival was 53% in patients younger than 40 years compared with 19% in patients 80 years or older. In lottery allocation, survival was not significantly different between racial and ethnic groups (average survival 31%). In the SOFA-only protocol, survival to discharge was 29% for Black patients compared with 35% for Hispanic patients and 36% for White patients. In the multiprinciple protocol, survival was 29% for Black patients compared with 38% for Hispanic patients and 34% for White patients. SOFA = Sequential Organ Failure Assessment.
In a sensitivity analysis, we found that the results were robust when assuming 10% survival without ventilator allocation (compared with 0% in the primary analysis).
Discussion
In this Monte Carlo simulation of a severe ventilator shortage in a Chicagoland population of patients with COVID-19, a youngest-first allocation system saved the most lives but led to significantly lower allocation and survival in the oldest patients. A lottery system of random ventilator allocation saved the fewest lives but had equal survival by race/ethnicity. Black patients had equivalent survival when given equal access to ventilators in a lottery system but lower survival in triage systems that used SOFA scores. Finally, critically ill Black and Hispanic patients requiring mechanical ventilation were younger than White patients and were most likely to be allocated ventilators in the youngest-first system.
Recent studies of general ICU patients without COVID-19 and a mixed population of ICU patients with and without COVID-19 in a single healthcare system found minimal or no association between race/ethnicity and priority tier (6, 7). The inequities in survival found in our study are likely attributable to differences in study population and the simulation methodology. Our study population was restricted to patients with COVID-19 who received mechanical ventilation but constituted a broadly representative sample from multiple healthcare systems across Chicago. In addition, our methodology simulates the triage process and may have exposed inefficiencies and disparities missed with traditional regression analysis.
“Color-blind” allocation protocols can unintentionally exacerbate health inequities. For example, Black patients in our cohort had higher SOFA scores and higher prevalence of comorbidities leading to lower priority for ventilators and lower survival. If applied to populations similar to our cohort, many U.S. ventilator allocation protocols would amplify existing healthcare disparities, layering inequitable resource allocation onto the current disproportionate health impact of the pandemic on disadvantaged communities (9).
Although youngest-first saved the most lives, U.S. state protocols either ignore age or use it as a secondary criterion (2). Proponents of prioritizing younger critically ill patients for treatment argue that they are worse off because they have not lived through all life’s stages (10–12). In our population, youngest-first resulted in higher survival in Black and Hispanic patients, reflecting the relatively younger age of Black and Hispanic patients developing severe COVID-19 disease.
Our study is limited by 1) only including patients with COVID-19 infection, 2) a lack of standard intubation criteria across hospital systems, and 3) a static simulation model. We cannot generalize these findings to all patients who would need mechanical ventilation in other crisis scenarios. Future work is required to develop dynamic simulation models that reevaluate patients during their hospital course.
In conclusion, in a Monte Carlo simulation model of ventilator allocation, systematic triage protocols saved more lives than a lottery. Youngest-first saved the most lives and did not exacerbate racial disparities. SOFA-only and multiprinciple protocols saved fewer lives than youngest-first and reduced ventilator allocation and survival in Black patients. Through simulation modeling, we found the ethical trade-offs between existing allocation protocols.
Footnotes
Supported by American Thoracic Society ATS-GSK Research Grant in COVID-19 (S.V.B.); NIH grants T32 HL007605 (S.V.B., W.D.M., and X.H.), R01 LM013337 (Y.L.), R21 HD096402 (L.N.S.-P.), P30 DK092949 (M.E.P.), K08 HL150291 (W.F.P.), and P30 DK114857 (K.N.M.); and funding from the National Palliative Care Research Center (K.N.M.).
Author Contributions: Study concept and design; acquisition of data; first drafting of the manuscript; and administrative, technical, and material support: S.V.B., Y.L., and W.F.P. Analysis and interpretation of data: all authors. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: S.V.B., Y.L., X.H., and W.F.P. Obtained funding: S.V.B. and W.F.P. Study supervision: M.E.P., C.M.C., K.N.M., and W.F.P. S.V.B., Y.L., and W.F.P. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Originally Published in Press as DOI: 10.1164/rccm.202106-1453LE on September 9, 2021
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Institute of Medicine. [DOI] [Google Scholar]
- 2. Piscitello GM, Kapania EM, Miller WD, Rojas JC, Siegler M, Parker WF. Variation in ventilator allocation guidelines by US state during the coronavirus disease 2019 pandemic: a systematic review. JAMA Netw Open . 2020;3:e2012606. doi: 10.1001/jamanetworkopen.2020.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med . 2020;382:1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 4.New York State Department of Health and New York State Task Force on Life and the Law Update Ventilator Allocation Guidelines 2015. [accessed 2021 Oct 19]. Available from: https://health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf
- 5. Daugherty Biddison EL, Faden R, Gwon HS, Mareiniss DP, Regenberg AC, Schoch-Spana M, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest . 2019;155:848–854. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 6. Wunsch H, Hill AD, Bosch N, Adhikari NKJ, Rubenfeld G, Walkey A, et al. Comparison of 2 triage scoring guidelines for allocation of mechanical ventilators. JAMA Netw Open . 2020;3:e2029250. doi: 10.1001/jamanetworkopen.2020.29250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gershengorn HB, Holt GE, Rezk A, Delgado S, Shah N, Arora A, et al. Assessment of disparities associated with a crisis standards of care resource allocation algorithm for patients in 2 US hospitals during the COVID-19 Pandemic. JAMA Netw Open . 2021;4:e214149. doi: 10.1001/jamanetworkopen.2021.4149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Snow GL, Bledsoe JR, Butler A, Wilson EL, Rea S, Majercik S, et al. Comparative evaluation of the clinical laboratory-based Intermountain risk score with the Charlson and Elixhauser comorbidity indices for mortality prediction. PLoS One . 2020;15:e0233495. doi: 10.1371/journal.pone.0233495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. White DB, Lo B. Mitigating inequities and saving lives with ICU triage during the COVID-19 pandemic. Am J Respir Crit Care Med . 2021;203:287–295. doi: 10.1164/rccm.202010-3809CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daniels N.2007.
- 11.Persad G, Joffe S.Allocating scarce life-saving resources: the proper role of age J Med Ethics [online ahead of print] 22 Mar 2021; DOI: 10.1136/medethics-2020-106792. [DOI] [PubMed] [Google Scholar]
- 12. Antiel RM, Curlin FA, Persad G, White DB, Zhang C, Glickman A, et al. Should pediatric patients be prioritized when rationing life-saving treatments during COVID-19 pandemic. Pediatrics . 2020;146:e2020012542. doi: 10.1542/peds.2020-012542. [DOI] [PubMed] [Google Scholar]