Antimicrobial resistance and One Health
Antimicrobial resistance (AMR) is a slow-moving pandemic threatening the viability of our socioeconomic prosperity and ability to effectively treat infections in humans and animals (1). Given the interconnectedness of humans, animals, and their environments, it is increasingly paramount that strategies to address AMR use a One Health approach to deal with this complex issue (2).
Human and animal health and agriculture rely heavily on the accessibility of effective antimicrobials as an important tool to treat and prevent bacterial infections in humans, animals, and crops (1). Furthermore, it is increasingly apparent that the environment has a large role in maintaining the “resistome” of AMR genes and resistant organisms (2,3). Therefore, as AMR continues to increase worldwide, global health and socio-economic impacts of AMR are projected to be substantial (1). The Pan-Canadian AMR Framework (4) and nascent Pan-Canadian Action Plan have used a One Health approach to develop integrated strategies to tackle AMR across various sectors.
Antimicrobial stewardship
Antimicrobial stewardship (AMS) programs and interventions must consider all of these important, interconnected sectors as part of their design, as AMR cannot be managed in isolation. As resistance to first-line antimicrobials is projected to increase from 26 to 40% by 2050 (1), in all sectors we must consider how to best use available products.
Antimicrobial stewardship, the “multifaceted approaches required to sustain the efficacy of antimicrobials and minimize the emergence of AMR” (5), must take responsibility for society’s management of antimicrobial use (AMU) to preserve the effectiveness of these products across the human, animal, agriculture, and environmental sectors. The concept and importance of AMS in animal health in Canada was considered at conferences in 1999, 2005, and 2011 (6–8), with movement towards a leadership plan for animal health in 2017 (9).
In 2016, the Alberta Veterinary Medical Association (ABVMA) hosted the One Health AMS Conference in collaboration with Alberta Agriculture and Forestry, and Alberta Health; this was one of the first times that Canadian leaders and subject matter experts in both animal and human health gathered to understand each other’s challenges in addressing AMR (10). This conference was followed by the Western Canadian One Health AMS Conference in Saskatchewan in 2019 (11). After the latter, there was a strong desire to continue the discussion in Canada to sustain momentum and grow the One Health influence on AMS initiatives.
2021 One Health antimicrobial stewardship conference
The ABVMA, with support from Alberta Agriculture and Forestry, the AMR — One Health Consortium, and the National Collaborating Centre for Infectious Diseases, hosted a virtual One Health AMS Conference in March 2021 (12). The objectives of this conference were to:
Provide a forum for communication about AMS across the animal, human and environmental sectors in western Canada;
Identify opportunities for One Health collaboration in stewardship activities;
Improve One Health understanding of AMR challenges facing animal, human and environmental health;
Improve awareness of implications of recent AMR and stewardship research and policy on front-line practice; and
Inform AMS practices by human, animal, and environmental sectors using evidence-based knowledge.
The virtual environment facilitated a diverse complement of speakers across the human-animal-environment AMR/AMU/AMS space. The conference included > 400 attendees from 6 continents, including 26 countries, and spanned the human, animal, and environmental health sectors. It included 24 expert speakers and 74 research abstracts/virtual presentations by PhD, MSc, and undergraduate students, and post-doctoral fellows. Presenters covered various topics encompassing areas of human and animal health, and they emphasized the importance of the environmental reservoir for AMR and implications for future AMR considerations.
The final day of the conference encouraged a new vision for AMS by asking a simple albeit critical question: “How do we move forward?” To answer this question, topics included:
social perspectives on AMS and how we must invoke strategies that influence changes from the status quo in food animal production, animal, and human health;
individual barriers to AMS, particularly psychosocial drivers of antimicrobial prescribing behaviors in human medicine;
the regulatory environment for AMU in livestock, with a view to changes in the European Union and what this could mean for Canada;
AMS perspectives from the pharmaceutical industry in the animal health sector; and
the built environment and potential for environmental exposure of AMR in both animal and human health settings.
The day concluded with a proposal to disrupt the status quo for current investment and resourcing of AMR and AMS initiatives in Canada by suggesting that a managed network model (13) could be a viable path forward.
Survey on antimicrobial stewardship perspectives, drivers, and barriers
To capitalize on the transdisciplinary conference, One Health at UCalgary designed a semi-structured questionnaire to collect information from participants, and their broader networks, during and after the conference. This anonymous questionnaire included fully informed consent and received ethical approval from the University of Calgary (REB21-0209).
Questionnaires were designed to capture perceptions of AMS, as well as perceived drivers and barriers across the One Health continuum. Conducting this research through a transdisciplinary lens is essential to identify similarities and differences among professions and sectors. Despite overwhelming agreement that AMS is important, there were disparate opinions regarding the existence of barriers towards stewardship, and whether respondents could do more personally, or if they had the required AMS support.
There were 87 questionnaire participants [Canada (n = 81), United Stated (n = 4), India (n = 1), Mexico (n = 1)], encompassing a variety of professions across the One Health spectrum, including veterinary medicine (n = 37), academia (n = 37), government (n = 12), industry (n = 12), human or veterinary medical associations (n = 9), producers (n = 6), producer associations (n = 5), veterinary technicians (n = 3), pharmacists (n = 3), physicians (n = 1), and lab technicians (n = 1) (participants could indicate > 1 profession category).
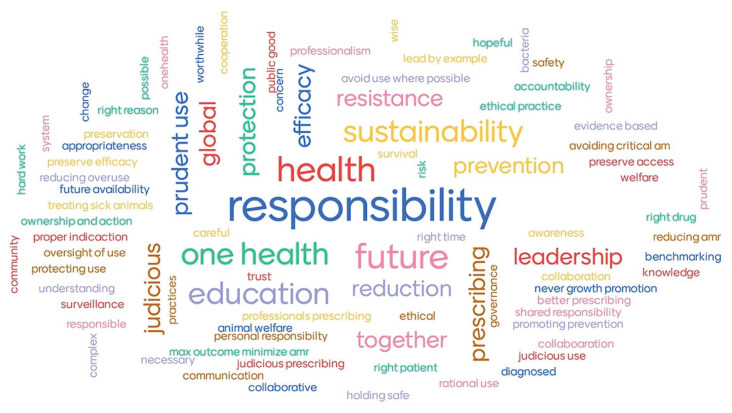
When asked what AMS meant to both the participants and their profession as a whole, the most common theme was responsibility. As reflected in Figure 1, many participants viewed the concept of stewardship to be synonymous with responsibility in terms of education and food safety, but most importantly, sustainability of AMU and preserving treatment efficacy.
Figure 1.
Word cloud developed from conference participant responses to the prompt “What does antimicrobial stewardship mean to you” (N = 39) through www.mentimiter.com
Regarding barriers to AMS, a common theme was “access,” including access to knowledge and research findings, timely diagnostics, and leadership or oversight in terms of up-to-date prescribing guidelines and agreement among experts, etc. Other identified barriers were economic, such as lack of sustained research and surveillance funding, and skilled personnel, as well as prescriber attitudes, including lack of motivation to change. Finally, when asked who should take responsibility for promoting AMS, the most common response was that everyone shares responsibility in stewardship efforts. The One Health concept was evident in responses, with responsibility being placed on antimicrobial prescribers and users in all sectors, as well as government, industry, professional associations, researchers, diagnosticians, and educators.
“I think that anyone with knowledge/expertise in antimicrobial resistance should promote antimicrobial stewardship.”
— Academic sector respondent
Outcomes and next steps
The 2021 One Health Antimicrobial Stewardship Conference was one of the most meaningful integrations across the One Health spectrum to discuss AMS in Canada. Past AMS efforts provided meaningful integration and cross-learning between human and animal health and agriculture sectors, although engagement from the environmental sector remained elusive. The knowledge gained and connections built with environmental AMR experts at this meeting were very encouraging. Future work must foster and grow these connections by engaging appropriate members from the environmental sectors of federal, provincial, and territorial governments.
Questionnaire findings indicated personal responsibility in AMS efforts is present and should be leveraged to advance current and future initiatives. However, there were also indications of cross-cutting barriers to stewardship, highlighting the importance of social science in AMR research and mitigation. Without an understanding of cross-cutting and sector-specific barriers to AMS, practical recommendations and meaningful progress cannot be made.
The proposal to challenge the status quo of current AMS policy and AMR resourcing and funding through a managed network model holds promise for future consideration. Canada’s AMR and AMS policy has been uncoordinated (14) and investment in AMR has been stagnant in the past decade (15). The success of this conference and its ongoing influence to build a strong One Health foundation for AMS efforts in Canada should be leveraged as the federal government works to finalize a Pan-Canadian AMR Action Plan. Information from the questionnaire will be finalized and published to guide further discussions of existing barriers to stewardship, as well as highlight relevant and actionable changes for implementation.
Acknowledgments
The authors acknowledge the work of the Program Planning Committee to plan this conference with input from the Steering Advisory Committee. Funding for this conference was provided by Alberta Agriculture and Forestry, with additional support from the AMR — One Health Consortium (primarily funded by the Major Innovation Fund [MIF] program of the Alberta Ministry of Jobs, Economy, and Innovation), and the National Collaborating Centre for Infectious Diseases (funded by the Public Health Agency of Canada).
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
Funding was provided by the Alberta Veterinary Medical Association, Alberta Agriculture and Forestry, Antimicrobial Resistance (AMR) — One Health Consortium, primarily funded by the Major Innovation Fund (MIF) program of the Alberta Ministry of Jobs, Economy, and Innovation (JEI), and the National Collaborating Centre for Infectious Diseases.
References
- 1.Council of Canadian Academies. When antibiotics fail: The Expert Panel on the Potential Socio-Economic Impacts of Antimicrobial Resistance in Canada. Ottawa, Ontario: Council of Canadian Academies; 2019. [Google Scholar]
- 2.McCubbin KD, Anholt RM, de Jong E, et al. Knowledge gaps in the understanding of antimicrobial resistance in Canada. [Last accessed December 15, 2021];Front Public Health. 2021 9:726484. doi: 10.3389/fpubh.2021.726484. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2021.726484/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim DW, Cha CJ. Antibiotic resistome from the One-Health perspective: Understanding and controlling antimicrobial resistance transmission. Exp Mol Med. 2021;53:301–309. doi: 10.1038/s12276-021-00569-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Government of Canada. Tackling antimicrobial resistance and antimicrobial use: A pan-Canadian framework for action. Guelph, Ontario: Public Health Agency of Canada; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weese SJ, Page SW, Prescott JF. Antimicrobial stewardship in animals. In: Giguère S, Prescott JF, Dowling PM, editors. Antimicrobial Therapy in Veterinary Medicine. Vol. 5. Hoboken, New Jersey: John Wiley & Sons; 2013. pp. 113–117. [Google Scholar]
- 6.Prescott JF, Dowling PM. Agriculture’s role in managing antimicrobial resistance: Conference report. Can Vet J. 2000;41:191–197. [PMC free article] [PubMed] [Google Scholar]
- 7.Prescott JF, Reid-Smith R, McClure JT. Conference report. Agriculture’s role in managing antimicrobial resistance: The road to prudent use. October 23–26, 2005, Toronto, Canada. Can Vet J. 2006;47:335–341. [PMC free article] [PubMed] [Google Scholar]
- 8.Prescott JF, Szkotnicki J, McClure JT, Reid-Smith R, Léger DF. Conference Report: Antimicrobial stewardship in Canadian agriculture and veterinary medicine: How is Canada doing and what still needs to be done? Can Vet J. 2012;53:402–407. [PMC free article] [PubMed] [Google Scholar]
- 9.Otto SJG, Szkotnicki J, McElwain C, So I, Weese JS, Prescott JF. Building the antimicrobial stewardship leadership plan for animal health in Canada (workshop, Ottawa, October 3–4, 2017) Can Vet J. 2018;59:746–748. [PMC free article] [PubMed] [Google Scholar]
- 10.One Health Alberta. ABVMA (Alberta Veterinary Medical Association) One Health Alberta Antimicrobial Stewardship Workshop — 2016 Areas of Consensus c2016 [monograph on the Internet] [Last accessed December 15, 2021]. Available from: https://ohab.ca/2016-areas-of-consensus/
- 11.Saskatchewan Epidemiology Association. Western Canadian One Health Antimicrobial Stewardship Conference: Inspiring and aligning action. c2019. [Last accessed December 15, 2021]. [monograph on the Internet]. Available from: https://www.saskepi.ca/home/2018-conference-2018-conference/ams-conference/
- 12.Babujee A, Naum K, Forseille J, Buote P, Dalton D, Otto SJG. One Health Antimicrobial Stewardship Conference — Alberta 2021 Report. Alberta Veterinary Medical Association; c2021. [Last accessed December 15, 2021]. [monograph on the Internet]. Available from: https://ohab.ca/ohasc-2021-report/ [Google Scholar]
- 13.Ferlie E, Fitzgerald L, McGivern G, Dopson S, Bennet C. Making Wicked Problems Governable?: The Case of Managed Networks in Health Care. 1st ed. Oxford, England: Oxford University Press; 2013. [Google Scholar]
- 14.Van Katwyk SR, Grimshaw JM, Hoffman SJ. Ten years of inaction on antimicrobial resistance: An environmental scan of policies in Canada from 2008 to 2018. Health Policy. 2020;15:48–62. doi: 10.12927/hcpol.2020.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Otto SJG, Miazga-Rodriguez M, Saxinger LM. Progress on integrated antimicrobial resistance and antimicrobial use surveillance in Canada (2014–2019) c2020. [Last accessed December 15, 2021]. [monograph on the Internet]. Available from: https://nccid.ca/publications/progress-on-integrated-antimicrobialresistance-and-antimicrobial-use-surveillance-in-canada/