Abstract
Perinatal mental health disorders are increasingly acknowledged as contributors to adverse maternal outcomes. We analyzed the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS; 2016 and 2017) to estimate hospitalization cost, length of stay, and severe maternal morbidity associated with perinatal mental health disorders overall, as well as stratified by payer and by specific mental health category. We found that individuals with mental health disorders had $458 higher costs per delivery hospitalization and 50% higher rates of severe maternal morbidity compared to those without mental health disorders. We estimate increased annual delivery hospitalization costs of $102 million in the US among individuals with perinatal mental health conditions compared to those without. Furthermore, individuals diagnosed with trauma/stress-related mental health disorders had even higher rates of hospitalization costs of $825 per delivery and 87% higher rates of severe maternal morbidity compared to those without. These findings provide important information for perinatal mental health program feasibility and cost-effectiveness analyses and suggest the need for increased focus on trauma/stress-related disorders.
Introduction
Severe maternal morbidity [SMM] has been defined as “unexpected outcomes of labor and delivery that result in significant short or long-term consequences to women’s health.”1 Examples of the conditions that constitute SMM include heart failure/arrest, hysterectomy, or the need for mechanical ventilation. The rates of occurrence of these conditions nearly tripled between 1993 and 2014, increasing from 49.5 to 144.0 per 10,000 delivers.1 Concomitant with the rate of increase of SMM has been a rise in the number of women diagnosed with perinatal mood disorders and serious mental illness during pregnancy. Prior studies have shown that these conditions also contribute to adverse maternal outcomes.2 Understanding the magnitude of the link between these trends is vital to improving perinatal health outcomes--a national priority for the United States. Research that promotes identification and treatment of perinatal mental health disorders may ultimately prevent adverse maternal and infant outcomes.3,4
Our study focuses on understanding the health and economic burdens associated with mental health disorders across the course of the pregnancy and into the postpartum period, which have important policy and programmatic implications. To determine the cost and health impacts of perinatal mental health disorders, it is critical to develop estimates of the direct cost and health outcomes associated with the disorders during the delivery hospitalization. Because approximately 42% of births are covered by Medicaid and 50% of births are covered by private (i.e., employer-sponsored or commercial) insurers,5 estimates of direct costs and health outcomes associated with mental health disorders during the delivery hospitalization are an important consideration for policy makers across public and private payers.
Previous studies have evaluated hospitalization costs associated with perinatal mental health disorders and found increased costs among deliveries to individuals with mental health disorders.2 We add to this important literature by 1) separately evaluating cost and health outcomes among deliveries with private and Medicaid coverage, 2) assessing individual mental health disorders, and 3) evaluating whether there are increased costs and adverse outcomes among individuals with more than one mental health disorder. Additionally, our study is able to capitalize on more recent data, including the first full two years of International Classification of Diseases, Tenth Revision (ICD-10) coding. Continued assessment of costs of perinatal mental health disorders overall and by individual disorders is critical for drawing public health and policy attention towards the need for prevention and treatment of perinatal mental health disorders as well as to provide cost estimates for program evaluation and planning.
Study Data and Methods
Data Source and Study Population
We analyzed hospital discharge data from the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) for the years 2016 and 2017. The NIS, produced by the Agency for Healthcare Research and Quality (AHRQ), is the largest publicly available hospital discharge dataset, and can be used to obtain national estimates of hospitalizations in the US.6 The NIS data include hospital information such as teaching status and location (i.e., rural or urban area), patient demographic information such as age and race, and ICD-10 diagnosis and procedure codes.
Our study included hospitalizations with a delivery diagnosis or a delivery diagnosis-related group code, as well as hospitalizations with a procedure code for a vaginal or cesarean delivery. We excluded 2.5% of hospitalizations with missing information for age, place of residence, length of stay, or hospitalization cost, and hospitalizations that resulted in a transfer to another hospital. We use “individuals” throughout the manuscript text to include all individuals who might need services related to pregnancy, birth, and postpartum care.
Measuring Mental Health Disorders
We defined mental health disorders using a list outlined in an AHRQ HCUP NIS statistical brief that specifically evaluated mental health disorders during inpatient stays.7 The AHRQ HCUP report includes 11 specific mental health diagnosis categories (anxiety, bipolar, depressive, disruptive/impulse-control/conduct, eating, obsessive-compulsive, personality, schizophrenia, somatic symptoms, suicidal ideation or attempt, and trauma/stress) composed of over 550 ICD-10 diagnosis codes.
In our study, we classified mental health disorders in three ways. First, we considered an individual to have a mental health disorder if there was at least one diagnosis code from the 11 mental health diagnosis categories. Second, we categorized individuals as having 0, 1, or 2 or more of the 11 mental health disorder categories. Third, we evaluated the four most common mental health diagnosis categories with a sufficient number of deliveries for analyses stratified among Medicaid- and privately-covered subsets (anxiety, depressive, bipolar, and trauma/stress-related).
Measures
Our study evaluated hospitalization cost, length of stay, and severe maternal morbidity. Severe maternal morbidity (SMM) was determined using the 21 indicators for measuring SMM using hospital discharge data that was established by the Centers for Disease Control and Prevention (CDC).1 The 21 indicators included 5 procedures (e.g., blood transfusion, ventilation, or hysterectomy) and 16 diagnosis-based indicators (e.g., heart failure/arrest or shock). To be considered SMM, a delivery must have had at least one of the 5 procedural-based indicators or must have had one of the 16 diagnosis indicators and either a long length of stay (≥5 days for cesarean delivery or ≥3 days for vaginal delivery in our study) or in-hospital death.
Analysis
We first assessed the percent of deliveries associated with mental health disorders among individual-level and hospital-level characteristics. Next, we compared adjusted outcomes in three ways by comparing: 1) deliveries to individuals with and without mental health disorders, 2) deliveries with 0, 1, or 2+ mental health disorders, and 3) deliveries to individuals with anxiety disorders, depressive disorders, bipolar disorders, or trauma/stress-related disorders. To assess differences in cost and health outcomes among deliveries with different payers, adjusted outcomes were re-calculated separately among privately-covered (private and commercial payers) and Medicaid-covered deliveries.
Multivariable generalized linear models with a gamma distribution and a log link function were used to determine adjusted values of hospitalization cost and length of stay, and multivariable logistic models were used to determine adjusted rates of SMM. Around 0.2% of deliveries with a length of stay noted as 0 days were given a length of stay equal to 1 day in order for the generalized linear models to be conducted. A full list of control variables and their reference values can be found in Appendix Exhibit A1.8
In addition to calculating delivery hospitalization costs, we estimated the annual delivery hospitalization costs in the US using the HCUP NIS data and the cost-to-charge ratio provided by HCUP by multiplying the increased hospitalization costs among individuals with 1 or with 2+ mental health conditions relative to the costs among individuals with none by the respective number of deliveries per year.
All analyses used the complex survey weighting to account for the survey design of the HCUP NIS data, and statistical significance was determined at a significance level of 0.05. This study was deemed non-human subjects research by the University of Arkansas for Medical Sciences institutional review board.
Limitations
Although the HCUP NIS database is the largest nationally representative hospital discharge database available, the data are observational in nature and are primarily intended for billing purposes. Utilization outside of the inpatient setting, such as in freestanding birth centers, cannot be captured. However, only 1.7% of U.S. births occur outside of the hospital setting.5 Additionally, mental health disorders that are not indicated as a diagnosis on the hospitalization record cannot be otherwise identified, indicating that the frequency of mental health disorders among our study population may be underestimated. If only the most severe cases of a given mental health disorder were noted in the diagnoses, then increased per-hospitalization costs found in our study may be higher than what may be realized by individuals with less severe mental health disorders; however, undercounting mental health disorders would ultimately indicate a conservative estimate of the total increased hospitalization cost annually among deliveries to individuals with mental health disorders. Our findings should not be assumed to represent the rates of perinatal mental health disorders in the postpartum year. Relatedly, our analysis includes costs associated with delivery hospitalization alone. Previous work has used a societal perspective to identify substantial long-term health care and productivity costs for mothers with perinatal mental health conditions as well as for their children.9,10 Policy-level decisions regarding resource allocation should consider such long-term costs and recognize that our findings are simply one piece of those calculations. Another limitation is that these data do not contain all relevant patient-level information, such as the number of prenatal care visits and individual household income, educational attainment, access to housing and nutritious foods, and other social determinants of health. Finally, small sample sizes of other mental health disorder categories prevented our ability to individually analyze these disorders.
Study Results
Among our final study sample of 1,460,826 records, representing 7,304,122 hospitalizations, we found that 4.3% of pregnant individuals had one of the 11 mental health disorder categories and an additional 1.6% of the pregnant individuals had two or more of the mental health disorder categories. Appendix Exhibit A18 provides the percent of deliveries with mental health disorders among each of the individual-level and hospital-level variables. We identified three characteristics that were most strongly related to having at least 1 mental health disorder. First, individuals in our study with an indication of a substance use disorder were nearly 4 times more likely to have a mental health disorder compared to individuals without a substance use disorder (23.1% vs 5.5%). Second, among those enrolled in Medicare, 19.8% had at least one mental health disorder. (Medicare was the smallest payer category, and the small sample size prevented a deeper analysis of this group.) Third, there was a dose-response relationship between the number of other clinical comorbidities (e.g., diabetes or HIV/AIDS) and having at least 1 mental health disorder. Specifically, the percentages of deliveries with mental health disorders were 4.1%, 8.8%, 10.4%, and 16.7% among deliveries with 0, 1, 2, or 3 or more other clinical comorbidities. The comorbidities are from a list of 21 Elixhauser comorbidity indicators, which excluded indicators that overlap with SMM, mental health disorders, or substance use disorders.11 Additionally, we found a lower percentage of non-Hispanic Black (5.0%) and Hispanic (3.1%) individuals with an indicated mental health disorder compared to the percent among non-Hispanic Whites (7.8%) (Appendix Exhibit A1).8
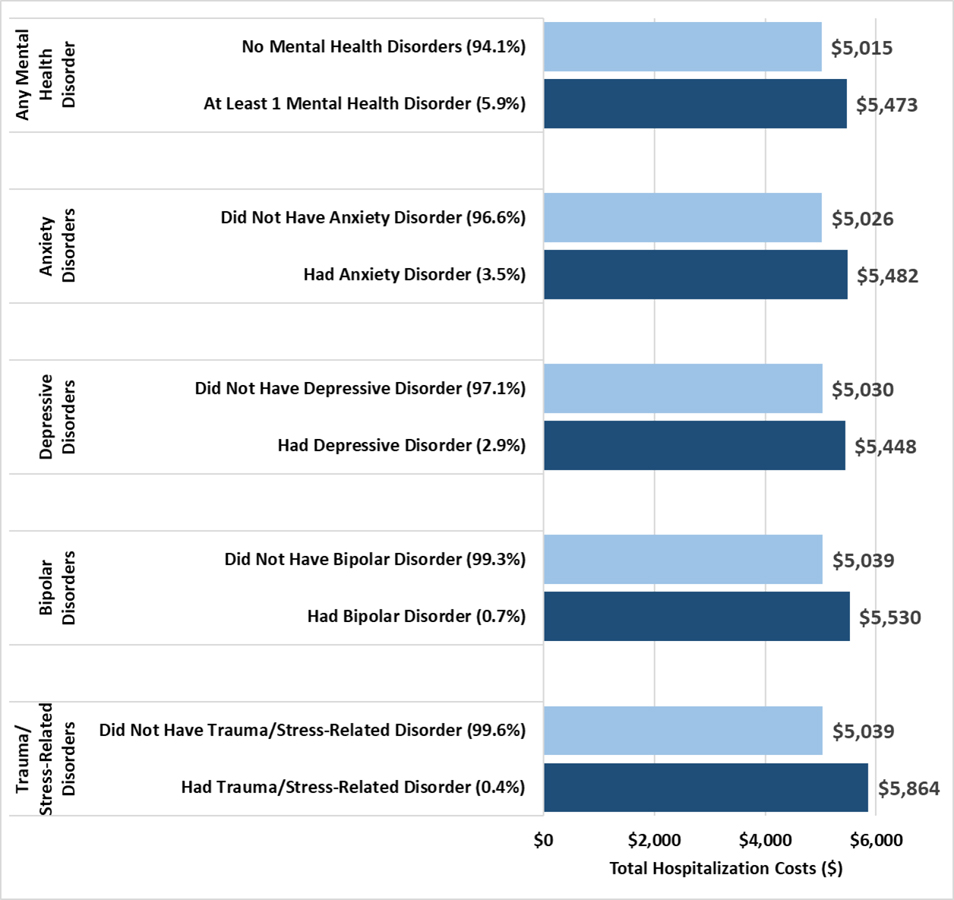
Exhibit 1 provides the differences in hospitalization cost based on different mental health disorder classifications among all payer categories. The average adjusted cost of delivery hospitalizations to individuals with at least 1 mental health disorder was $458, or 9% more than the cost to those with no mental health disorders ($5,473 vs $5,015). Prior to adjusting for patient- and hospital-level factors (covariates and unadjusted results provided in Appendix Exhibit A1 and A2),8 the hospitalization cost among individuals with at least 1 mental health disorder was $1,026, or 21% higher than the cost for individuals without mental health disorders ($6,016 vs $4,990, data not shown). We additionally found that adjusted hospitalization cost was further increased for individuals with 2 or more mental health disorders ($5,559) relative to those with 1 ($5,441) or no ($5,015) mental health disorders [results not shown]. The greatest increase in cost was associated with trauma/stress-related mental health disorders. Specifically, individuals with a trauma/stress-related disorder had adjusted hospitalization costs that were $825 greater (16%) than those without a trauma/stress-related disorder. In unadjusted costs, the difference was $2,571 (51%) (Appendix Exhibit A2).8
EXHIBIT 1.
Average Adjusted Hospitalization Costs, by Mental Health Status Designations (n=1,460,826; weighted n=7,304,122)
SOURCE: Authors’ analysis of data from the Healthcare Cost and Utilization Project, National Inpatient Sample, years 2016 and 2017.
NOTES:
Adjusted costs determined using generalized linear models with gamma distribution and log link, adjusting for age, race, primary payer, number of other (i.e., non-mental health or substance use-related) clinical comorbidities, presence of a substance use disorder, having a cesarean vs vaginal delivery, median income in the patient’s zip code of residence, hospital census region, hospital ownership, hospital teach status and rural/urban designation, safety net hospital designation, and minority hospital designation. All difference in means are statistically significant (p<0.001) using Wald tests to test for differences between average adjusted hospitalization costs between categories of each mental health grouping.
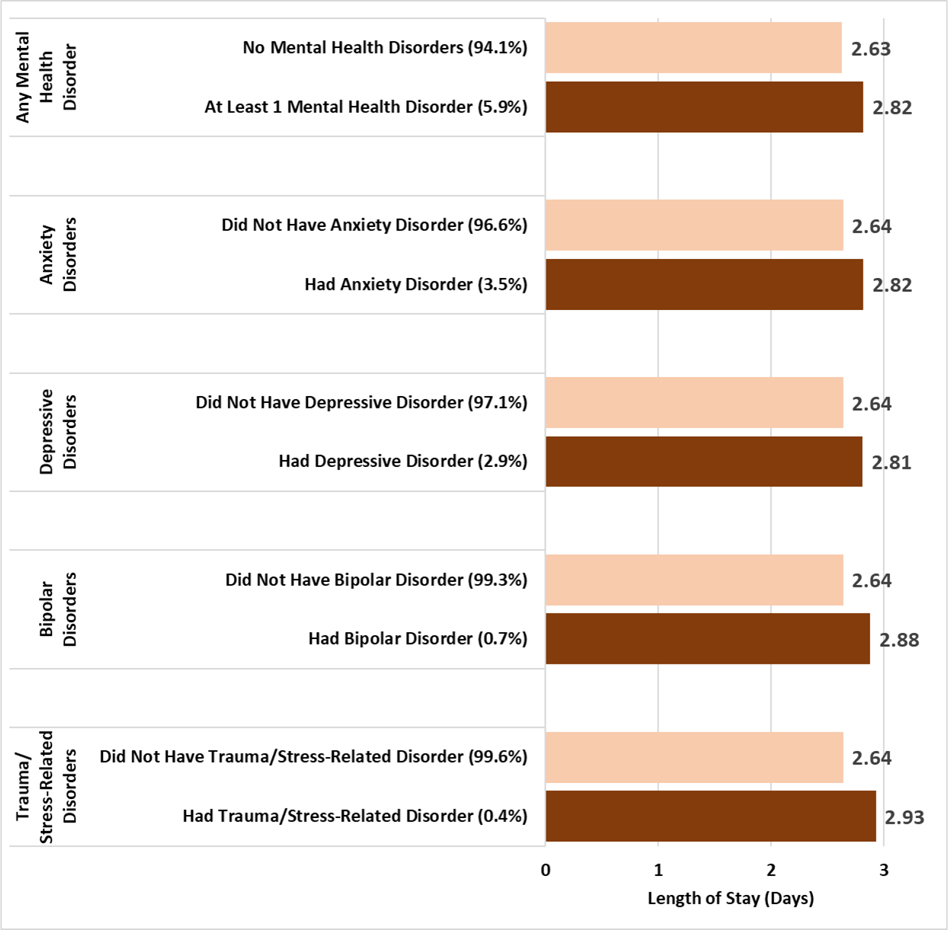
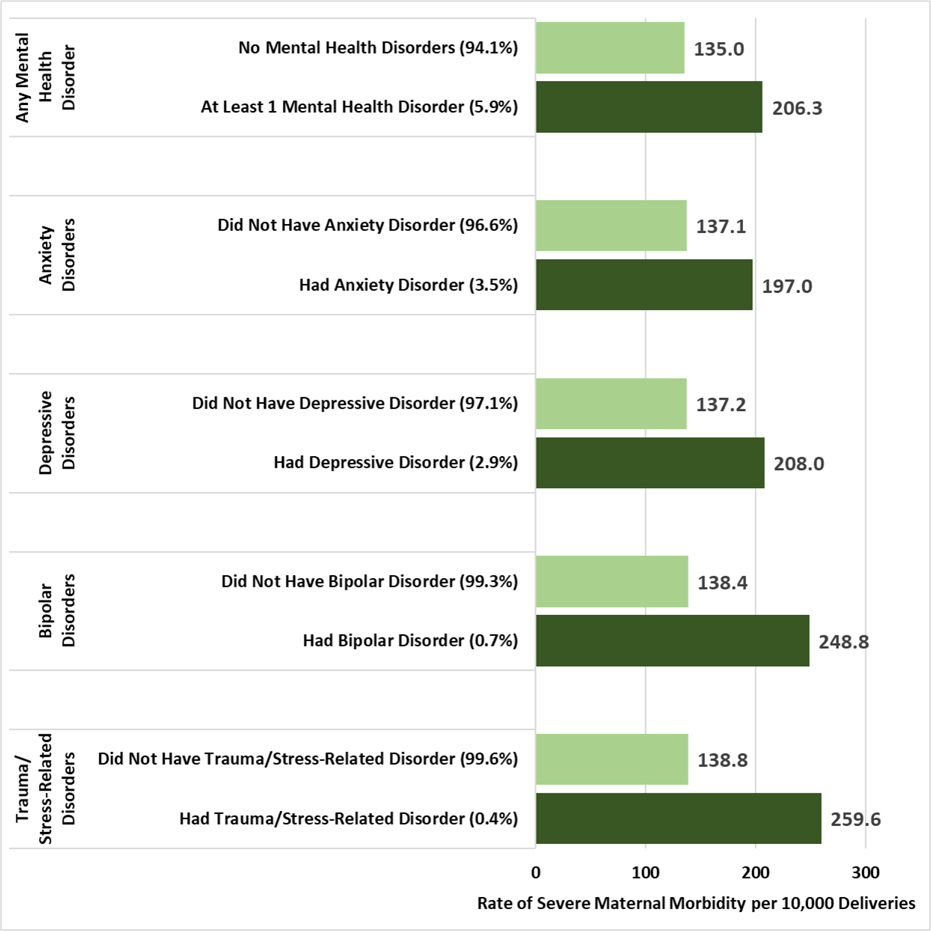
Exhibit 2, which provides adjusted lengths of stay among all payer categories, suggests that individuals with mental health disorders had around 0.2 days longer length of stay, and individuals with a trauma/stress-related mental health disorder had a length of stay that was around 0.3 days longer. Exhibit 3 provides adjusted rates of severe maternal morbidity [SMM], as defined by CDC,1 per 10,000 deliveries among all payers. Individuals with at least 1 mental health disorder had an adjusted rate of SMM that was over 50% greater than the rate of SMM among those with no mental health disorders (206.3 vs 135.0 per 10,000 deliveries). Similar to cost and length of stay, we found that having 2 or more mental health disorders was associated with a higher rate of SMM (221.8 per 10,000 deliveries) compared to those having 1 (200.6 per 10,000 deliveries) or no (135.0 per 10,000 deliveries) mental health disorders (data not shown). The largest difference in SMM was observed in individuals with a trauma/stress-related disorder, who had an 87% higher adjusted rate of SMM compared to those without a trauma/stress-related disorder (259.6 vs 138.8 per 10,000 deliveries). Unadjusted differences in lengths of stay and SMM can be found in Appendix Exhibits A3 and A4.8
EXHIBIT 2.
Average Adjusted Hospital Length of Stay, by Mental Health Status Designations (n=1,460,826; weighted n=7,304,122)
SOURCE: Authors’ analysis of data from the Healthcare Cost and Utilization Project, National Inpatient Sample, years 2016 and 2017.
NOTES:
Adjusted lengths of stay determined using generalized linear models with gamma distribution and log link, adjusting for age, race, primary payer, number of other (i.e., non-mental health or substance-use related) clinical comorbidities, presence of a substance use disorder, having a cesarean vs vaginal delivery, median income in the patient’s zip code of residence, hospital census region, hospital ownership, hospital teach status and rural/urban designation, safety net hospital designation, and minority hospital designation. All difference in means are statistically significant (p<0.001) using Wald tests to test for differences between average adjusted lengths of stay between categories of each mental health grouping.
EXHIBIT 3.
Average Adjusted Rates of Severe Maternal Morbidity, by Mental Health Status Designations (n=1,460,826; weighted n=7,304,122)
SOURCE: Authors’ analysis of data from the Healthcare Cost and Utilization Project, National Inpatient Sample, years 2016 and 2017.
NOTES:
Adjusted rates of severe maternal morbidity per 10,000 deliveries determined using predicted probabilities based on logistic regressions, adjusting for age, race, primary payer, number of other (i.e., non-mental health or substance use-related) clinical comorbidities, presence of a substance use disorder, having a cesarean vs vaginal delivery, median income in the patient’s zip code of residence, hospital census region, hospital ownership, hospital teach status and rural/urban designation, safety net hospital designation, and minority hospital designation. All differences in means are statistically significant (p<0.001) using Wald tests to test for differences between average adjusted rates of severe maternal morbidity between categories of each mental health analysis grouping.
Exhibit 4 provides adjusted outcomes among privately-covered and Medicaid-covered deliveries separately. Adjusted outcomes for Medicare-covered deliveries were not calculated due to small sample size. Similar to findings among all payers, deliveries among those with a trauma/stress-related disorder had significantly higher costs and rates of SMM for both payer categories. Of note are the higher rates of mental health disorders among Medicaid-covered deliveries relative to private-covered deliveries, including higher rates of having any mental health disorder (6.3% vs 5.5%), depressive disorders (3.2% vs 2.6%), bipolar disorders (1.1% vs 0.3%, and trauma/stress-related disorders (0.5% vs 0.2%). Individuals with privately-covered deliveries had higher rates of anxiety disorders relative to individuals with Medicaid-covered deliveries (3.6% vs 3.3%). Please refer to Appendix Exhibits A5 through A78 for regression coefficients and p-values, overall and by payer.
Exhibit 4.
Average Adjusted Hospitalization Costs, Hospital Length of Stay, and Severe Maternal Morbidity, by Mental Health Status Designations and Payer
| Mental Health Grouping | Percent of Deliveries | Cost Per Stay ($) | Length of Stay (Days) | Severe Maternal Morbidity per 10,000 Deliveries |
|---|---|---|---|---|
|
| ||||
| % | Mean | Mean | Rate | |
|
| ||||
| Privately-Covered Deliveries (n=739,381; weighted n=3,696,901) | ||||
| Any Mental Health Disorder | ||||
| No | 94.6 | 5064 | 2.7 | 109.6 |
| Yes | 5.5 | 5462 | 2.8 | 163.3 |
|
| ||||
| Number of Mental Health Disorders | ||||
| 0 | 94.6 | 5064 | 2.7 | 109.6 |
| 1 | 4.1 | 5453 | 2.8 | 161.1 |
| ≥2 | 1.3 | 5489 | 2.8 | 170.1 |
|
| ||||
| Anxiety Disorder | ||||
| No | 96.4 | 5071 | 2.7 | 110.7 |
| Yes | 3.6 | 5472 | 2.8 | 161.4 |
|
| ||||
| Depressive Disorder | ||||
| No | 97.4 | 5076 | 2.7 | 111.1 |
| Yes | 2.6 | 5423 | 2.8 | 164.8 |
|
| ||||
| Bipolar Disorder | ||||
| No | 99.7 | 5084 | 2.7 | 112.3 |
| Yes | 0.3 | 5479 | 2.8 | 179.0 |
|
| ||||
| Trauma-Related Disorder | ||||
| No | 99.8 | 5083 | 2.7 | 112.3 |
| Yes | 0.2 | 5972 | 2.9 | 204.0 |
|
Medicaid-Covered Deliveries (n=633,091; weighted n=3,165,452) | ||||
| Any Mental Health Disorder | ||||
| No | 93.7 | 4998 | 2.6 | 164.2 |
| Yes | 6.3 | 5471 | 2.8 | 239.7 |
|
| ||||
| Number of Mental Health Disorders | ||||
| 0 | 93.7 | 4998 | 2.6 | 164.2 |
| 1 | 4.5 | 5423 | 2.8 | 234.2 |
| ≥2 | 1.8 | 5586 | 2.9 | 253.3 |
|
| ||||
| Anxiety Disorder | ||||
| No | 96.7 | 5013 | 2.6 | 166.7 |
| Yes | 3.3 | 5487 | 2.8 | 233.6 |
|
| ||||
| Depressive Disorder | ||||
| No | 96.8 | 5014 | 2.6 | 166.6 |
| Yes | 3.2 | 5469 | 2.8 | 241.1 |
|
| ||||
| Bipolar Disorder | ||||
| No | 98.9 | 5023 | 2.6 | 168.0 |
| Yes | 1.1 | 5484 | 2.9 | 258.0 |
|
| ||||
| Trauma/Stress-Related Disorder | ||||
| No | 99.5 | 5024 | 2.6 | 168.4 |
| Yes | 0.5 | 5808 | 2.9 | 275.4 |
SOURCE:
Authors’ analysis of data from the Healthcare Cost and Utilization Project, National Inpatient Sample, years 2016 and 2017.
NOTES:
Adjusted costs and lengths of stay determined using generalized linear models with gamma distribution and log link. Adjusted rates of severe maternal mortality per 10,000 deliveries determined using predicted probabilities based on logistic regressions. All models were adjusted for age, race, number of other (i.e., non-mental health or substance use-related) clinical comorbidities, presence of a substance use disorder, having a cesarean vs vaginal delivery, median income in the patient’s zip code of residence, hospital census region, hospital ownership, hospital teach status and rural/urban designation, safety net hospital designation, and minority hospital designation. Regressions for privately- and Medicaid-covered deliveries were conducted separately. Regressions were not completed for Medicare-covered deliveries, given the small sample size of this population. All differences in means are statistically significant (p<0.001) using Wald tests to test for differences between average adjusted hospitalization costs between categories of each mental health grouping.
Extrapolating the findings to the number of deliveries in hospitals in the US each year with one (average n=163,035) or two or more (average n=60,298) mental health disorders, we estimate $102 million ($229 million unadjusted) in increased hospitalization costs annually associated with delivery hospitalizations among individuals with mental health disorders, including $42 million ($108 million unadjusted) associated with privately-covered deliveries and $49 million ($101 million unadjusted) associated with Medicaid-covered deliveries (see Appendix Exhibit A8 for details).8
Discussion
In this analysis of nationally representative hospital discharge data, we found higher hospitalization cost, length of stay, and severe maternal morbidity among individuals with mental health disorders relative to those without mental health disorders. Our study adds to the literature that evaluates outcomes during delivery hospitalizations among individuals with mental health disorders by assessing outcomes among those with multiple mental health disorders as well as outcomes associated with the four most common mental health disorders in our sample. As expected, we found an increase in the cost, length of stay, and SMM among individuals with multiple mental health disorders, and we estimate over $102 million annually in adjusted increased hospitalization costs among deliveries to individuals with mental health disorders. The nearly $500 difference in hospitalization cost per delivery (nearly 10% greater cost) for individuals with mental health disorders in addition to the increased length of stay and risk of SMM are certainly a small portion of the increased cost and adverse outcomes among this population and their infants, as many adverse events and their sequelae continue to occur well into the postpartum year and beyond.10,12
In our study, the mental health disorders most strongly associated with adverse maternal outcomes and increased hospitalization cost were trauma/stress-related disorders. This category includes 19 ICD-10 diagnosis codes related to post-traumatic stress, adjustment disorder, reactions to severe stress, and dissociative amnesia.7 Despite this list of 19 codes within the trauma/stress related disorder category, 68% of individuals had the specific (one ICD-10 code) diagnosis of unspecified post-traumatic stress disorder,13 suggesting that populations with unspecified post-traumatic stress disorder may be an important population to focus on for targeted research and/or perinatal mental health programs. The second most common diagnosis among the trauma/stress-related disorders were adjustment disorders, present in 31% of the deliveries with a diagnosis for trauma/stress disorder. Most perinatal mental health evaluations, programs, and bundles of care focus on depression and anxiety as these two disorders are the most commonly assessed and diagnosed mental health disorders among pregnant individuals. Such programs should certainly continue; however, additional research efforts and programs aimed to help improve outcomes among individuals with traumatic experiences may be an important next step in perinatal mental health. Our finding of increased risk of adverse maternal outcomes among individuals with trauma/stress-related disorders aligns with previous work that suggested a potential mechanism for increased rates of adverse outcomes among individuals with post-traumatic stress disorders may be associated with higher cortisol levels.14,15,16 A recent call to action recognized the need for improved efforts to prevent adverse maternal outcomes among individuals with post-traumatic stress disorder through earlier recognition and treatment, but the article also notes that additional research may be needed to guide recommended practice among this population.17 Our study provides valuable information regarding cost of hospitalization and rates of SMM that may ultimately serve as a data point in cost-effectiveness analyses that evaluate treatment for perinatal post-traumatic stress disorder.
We found lower indicated rates of mental health conditions among deliveries to individuals of color, which aligns with previous evaluations.2 However, these results should be taken with caution and warrant further evaluation given under-recognition, diagnosis, and treatment of mental health disorders among populations of color, potentially a result of long-standing stigmas and biases associated with mental health disorders.4,18,19
Policy Implications
Leading maternal health advocates, including the American College of Obstetricians and Gynecologists (ACOG) and the American College of Nurse-Midwives, recognize the importance of prenatal and postpartum depression screening. The Council on Patient Safety in Women’s Health Care developed the Maternal Mental Health: Perinatal Depression and Anxiety safety bundle to ensure that health care providers are prepared to identify and address perinatal depression and anxiety.20 The patient safety bundle includes information regarding tools for screening as well as care management resources for individuals who screen positive. Our findings suggest that an opportunity exists to expand existing perinatal safety bundles to include screening for trauma/stress-related disorders and to include resources for individuals who may have a history of trauma. Previous studies have found higher rates of trauma-related disorders among people of color, individuals with low incomes, and those who are unhoused or incarcerated; as such, implementing policies that increase trauma-informed perinatal care may serve as an important approach for reducing adverse maternal outcomes overall and in terms of disparities.16,21,22 Health systems and programs that provide perinatal care should be trained in and adopt trauma-informed care approaches to support an environment that recognizes the signs of trauma and ultimately seeks to avoid re-traumatization across the perinatal care experience.22 Relatedly, to improve identification of mental health disorders and treatment through culturally congruent care, educational efforts must improve clinicians’ understanding of how signs and symptoms of mental health disorders may present differently for individuals with different cultural backgrounds, and that disclosure by individuals may be influenced by stigma, bias, and discrimination.23
Policy efforts should aim to improve continuity of insurance coverage and the provision of care between pregnancies. A life course perspective that includes coverage of mental health services may ultimately prevent pregnancy complications by identifying and managing physical and mental health disorders prior to and in between pregnancies and by acknowledging that some individuals may face multiple accumulating oppressors that ultimately impact their pregnancy outcomes.24 Furthermore, expansion of care beyond the usual 6-week provision of postnatal care in the Medicaid population may prevent the relatively high percentage of maternal deaths associated with mental health disorders occurring in the postpartum year.4,25,26 Currently, few states provide Medicaid-coverage beyond the required 60-days postpartum period; the American Rescue Plan Act of 2021 enables states to file a State Plan Amendment to their Medicaid program to provide full coverage to all pregnant individuals through 12 months postpartum beginning in April 2022 and sun-setting in 2027.27 It is estimated that 50% of maternal mortality occurs after the day of delivery and throughout one year postpartum, with approximately 12% occurring at least 6 weeks (43 days) after delivery.28 In 2020, California opted to extended coverage 12-months postpartum for individuals with a mental health disorder.29 States with budget constraints could also follow a similar condition-specific targeted approach by providing extended coverage for individuals with noted physical and mental health conditions.
Payers and policy makers should additionally continue efforts to increase insurance coverage for innovative prenatal and perinatal care models, such as midwifery-led models of care, group prenatal care, and doulas.30 Group prenatal care models may provide social support and connections within the health care system that serve an important role in reducing stress and anxiety related to pregnancy.31 Similarly, doulas may provide pregnant and postpartum individuals with emotional and social support to navigate their pregnancies; however, few Medicaid programs currently cover doula services.32–34
Finally, to adequately address any population health issue, comprehensive and consistent data are essential. Efforts to increase data collection and reporting of mental health disorders during the perinatal period are necessary and should include improved identification of recent (or current) pregnancy among individuals who die of substance use, overdose, self-harm, or homicide.4 While introduction of the checkbox on the death certificate to identify whether an individual was pregnant within the last year was an important first step, not all states have adopted the standardized version of this question.35 Furthermore, the analyses of maternal mortality by the CDC often exclude death due to incidental causes, such as suicide and overdose.28
Conclusions
Delivery hospitalizations to individuals with mental health disorders had 50% higher rates of severe maternal morbidity and $458 higher costs ($1,026 unadjusted), with an estimated increased cost of $102 million annually in the US. Individuals with trauma/stress-related mental health disorders had nearly twice the rates of severe maternal morbidity and $825 higher hospitalization costs ($2,571 unadjusted) compared to individuals without trauma-stress-related disorders, suggesting increased need for prevention and intervention. These findings provide a foundation for information needed for perinatal mental health program feasibility and cost-effectiveness analyses across payers. The lower identified rates of mental health disorders noted among individuals of color indicates the need for improved recognition of mental health disorders among this population.
Supplementary Material
Endnotes
- 1.Centers for Disease Control and Prevention (CDC). Severe maternal morbidity in the United States [Internet]. Atlanta (GA): CDC; [last reviewed 2021 Feb 2; cited 2021 Apr 15]. Available from: https://www.cdc.gov/reproductivehealth/MaternalInfantHealth/SevereMaternalMorbidity.html [Google Scholar]
- 2.McKee K, Admon LK, Winkelman TN, Muzik M, Hall S, Dalton VK, et al. Perinatal mood and anxiety disorders, serious mental illness, and delivery-related health outcomes, United States, 2006–2015. BMC Womens Health. 2020;20(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19(3):313–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mangla K, Hoffman MC, Trumpff C, O’Grady S, Monk C. Maternal self-harm deaths: an unrecognized and preventable outcome. Obstet Gynecol. 2019;221(4):295–303. [DOI] [PubMed] [Google Scholar]
- 5.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Division of Vital Statistics. Births: final data for 2019. Natl Vital Stat Rep. 2021;70(2):1–50. [PubMed] [Google Scholar]
- 6.Healthcare Cost and Utilization Project. Overview of the National (Nationwide) Inpatient Sample (NIS) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; [last modified 2021 Apr 5; cited 2021 Apr 15]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp [Google Scholar]
- 7.Owens PL, Fingar KR, McDermott KW, Muhuri PK, Heslin KC. Inpatient stays involving mental and substance use disorders, 2016 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; Mar 2019. (HCUP statistical brief #249). Available from: www.hcup-us.ahrq.gov/reports/statbriefs/sb249-mental-substance-use-disorder-hospital-stays-2016.pdf [PubMed] [Google Scholar]
- 8.To access the appendix, click on the appendix link in the box to the right of the article online.
- 9.Luca DL, Margiotta C, Staatz C, Garlow E, Christensen A, Zivin K. Financial toll of untreated perinatal mood and anxiety disorders among 2017 births in the United States. Am. J. Public Health. 2020. Jun;110(6):888–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer A, Knapp M, Parsonage M. Lifetime costs of perinatal anxiety and depression. J Affect Disord. 2016;192:83–90. [DOI] [PubMed] [Google Scholar]
- 11.Elixhauser Comorbidity Software for ICD-10-CM (version 2019) Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp [PubMed] [Google Scholar]
- 12.Zanardi DM, Santos JP, Pacagnella RC, Parpinelli MA, Silveira C, Andreucci CB, et al. Long-term consequences of severe maternal morbidity on infant growth and development. Matern. Child Health J, (2021). 25(3), 487–96. [DOI] [PubMed] [Google Scholar]
- 13.The report used to determine mental health disorders in our paper included acute and chronic post-traumatic stress disorder in the anxiety disorder group. We conducted a sensitivity analysis to assess whether moving these two ICD-10 codes to the trauma/stress-related disorders grouping impacted our study. We noted minimal impact, with 202 individuals being newly included in the trauma/stress-related disorder group and 132 individuals being removed from the anxiety disorders group.
- 14.Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol. 2001;97(1):17–22. [DOI] [PubMed] [Google Scholar]
- 15.Seng JS, Li Y, Yang JJ, King AP, Low LMK, Sperlich M, et al. Gestational and postnatal cortisol profiles of women with posttraumatic stress disorder and the dissociative subtype. J Obstet Gynecol Neonatal Nurs. 2018;47(1):12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seng JS, Kohn-Wood LP, McPherson MD, Sperlich M. Disparity in posttraumatic stress disorder diagnosis among African American pregnant women. Arch Womens Ment Health. 2011;14(4):295–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canfield D, Silver RM. Detection and prevention of postpartum posttraumatic stress disorder: a call to action. Obstet Gynecol. 2020. Nov;136(5):1030–5. [DOI] [PubMed] [Google Scholar]
- 18.Schiff DM, Nielsen T, Hoeppner BB, Terplan M, Hansen H, Bernson D, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA network open. 2020;3(5):e205734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, Adams AS. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kendig S, Keats JP, Hoffman MC, Kay LB, Miller ES, Simas TAM, et al. Consensus bundle on maternal mental health: perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2017;46(2):272–81. [DOI] [PubMed] [Google Scholar]
- 21.Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol. 2009;114(4):839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mosley EA, Lanning RK. Evidence and guidelines for trauma-informed doula care. Midwifery. 2020;83:102643. [DOI] [PubMed] [Google Scholar]
- 23.Lara-Cinisomo S, Clark CT, Wood J. Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: Addressing stigma is not enough. Womens Health Issues. 2018;28(3):201–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fuentes-Afflick E, Perrin JM, Moley KH, Díaz Á, McCormick MC, Lu MC. Optimizing health and well-being for women and children: commentary highlights interventions and recommends key improvements in programs and policies to optimize health and well-being among women and children in the United States. Health Aff. 2021;40(2):212–8. [DOI] [PubMed] [Google Scholar]
- 25.Creanga AA. Maternal mortality in the United States: a review of contemporary data and their limitations. Clin Obstet Gynecol. 2018;61(2):296–306. [DOI] [PubMed] [Google Scholar]
- 26.Daw JR, Winkelman TN, Dalton VK, Kozhimannil KB, Admon LK. Medicaid expansion improved perinatal insurance continuity for low-income women. Health Aff (Millwood). 2020;39(9):1531–9. [DOI] [PubMed] [Google Scholar]
- 27.Congress.gov. HR 1319—American Rescue Plan Act of 2021. [cited 2021 Jun 21]. Available from: https://www.congress.gov/bill/117th-congress/house-bill/1319
- 28.Petersen EE, Davis NL, Goodman D, Shanna Cox S, Johnston EM, Johnston E, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckert E. Despite many states doing what they can, the federal government must act now to extend postpartum Medicaid coverage. Health Affairs Blog [blog on the Internet]. 2020. Dec 8. [cited 2021 Apr 15]. Available from: https://Www.healthaffairs.org/do/10.1377/hblog20201207.582148/full/ [Google Scholar]
- 30.Aspen Health Strategy Group. Weil AR, Reichert AJ, editors. Reversing the U.S. Maternal Mortality Crisis. Washington, DC: The Aspen Institute; 2021. Available from: https://www.aspeninstitute.org/publications/reversing-the-u-s-maternal-mortality-crisis/ [Google Scholar]
- 31.Gareau S, Lòpez-De Fede A, Loudermilk BL, Cummings TH, Hardin JW, Picklesimer AH, et al. Group prenatal care results in Medicaid savings with better outcomes: a propensity score analysis of CenteringPregnancy participation in South Carolina. Matern Child Health J. 2016;20(7):1384–93. [DOI] [PubMed] [Google Scholar]
- 32.Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.:CD003766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozhimannil KB, Hardeman RR. Coverage for doula services: How state Medicaid programs can address concerns about maternity care costs and quality. Birth. 2016. Jun;43(2):97–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore JE, George KE, Bakst C, Shea K. Improving maternal health access, coverage, and outcomes in Medicaid: a resource for state Medicaid agencies and Medicaid managed care organizations [Internet]. Washington, DC: Institute for Medicaid Innovation; 2020. Available from: https://Www.medicaidinnovation.org/_images/content/2020-IMI-Improving_Maternal_Health_Access_Coverage_and_Outcomes-report.pdf [Google Scholar]
- 35.Hoyert DL, Uddin SF, Miniño AM. Evaluation of the pregnancy status checkbox on the identification of maternal deaths. Natl Vital Stat Rep. 2020;69(1):1–23. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.