Abstract
Context:
Hirschsprung's disease (HD) is a congenital anomaly affecting the enteric nervous system commonly the rectosigmoid region. Treatment is surgical where the aganglionic segment is resected, and bowel continuity is achieved by a colo-anal anastomosis. In 1999, Georgeson et al. proposed a new technique of primary laparoscopic-assisted pull through for HD as a new gold standard.
Aim of the Study:
To evaluate the outcome of the laparoscopic Duhamel procedure for the management of HD in children older than 3 years.
Methods:
This study was performed on 8 patients who were more than 3-year-old, with confirmed diagnoses of HD. Patients who initially presented with enterocolitis or obstruction were excluded from this study. In all cases, laparoscopic-assisted Duhamel was done.
Results:
We reported our results for the 1st year follow-up period and divided our results into early outcome for the first 3 months postoperative during which we had 2 cases complaining of enterocolitis that responded to conservative treatment, we observed 2 cases of perianal excoriation that responded to medical treatment while the late outcome was reported after 3 months postoperative: We had two cases with attacks of enterocolitis at 6 months and 9 months postoperatively that needed conservative treatment in the hospital in the form of parenteral antibiotics, rectal irrigation, intravenous fluids and NP0. There was neither anastomotic leak nor stenosis.
Conclusion:
Laparoscopic Duhamel for the management of HD in children older than 3 years is safe and useful procedure.
Keywords: Hirschsprung's disease, laparoscopic assisted, laparoscopic Duhamel
INTRODUCTION
Hirschsprung's disease (HD) is a congenital anomaly of the enteric nervous system characterised by the absence of parasympathetic ganglion cells in the submucous and myenteric plexuses of the intestine, usually affecting the rectosigmoid portion of the large bowel.[1] Definitive surgery for HD has been performed for many years using either Swenson, Duhamel, or Soave technique. Georgeson et al., in 1999, did the first laparoscopic-assisted endorectal pull-through for HD.[1,2] In 2008, he published his new study with some technical modifications.[3] The use of laparoscope allows taking biopsies to determine the level of aganglionosis, adequate mobilisation of the bowel with less trauma and bleeding, and in addition, is cosmetically superior.[4] In the Duhamel procedure, a short segment of the aganglionic rectum is anastomosed to pulled-down segment of the ganglionic colon (side-to-side). Duhamel procedure is a widely used procedure as it is technically easy, less anal stretching, especially in older children.[4,5,6]
The current study aimed to evaluate the surgical and functional outcome of the laparoscopic-aided Duhamel procedure for the management of HD in children older than 3 years.
METHODS
The current prospective, observational study was conducted at a Paediatric surgery tertiary Centre from July 2017 to March 2019 to allow follow-up period of at least 6 months for the last case operated upon. Informed consent was obtained from the parents. The diagnosis of HD was documented by history, clinical examination and investigations.
Included in history was the history of delayed passage off of meconium, history of constipation since birth, and attacks of enterocolitis. Clinical examination was performed to check general condition, presence of associated anomalies, abdominal examination, rectal examination to exclude signs of obstruction, and presence of impacted stools. Investigations included routine laboratory investigations, barium enema, anorectal manometry, and rectal biopsy.
Inclusion criteria included age older than 3 years. Patients who initially presented with enterocolitis or obstruction were excluded from this study.
Collected clinical data included age, gender, weight, and frequency of presenting symptoms. All patients underwent barium enema to determine the transition zone. All patients underwent preoperative rectal irrigations for 3 months using saline solution 20 ml/kg twice daily to deflate dilated colon, 2 days preoperative, we did bowel preparation which comprised of keeping the patient on clear fluids for 2 days, and colonic washouts 24 h and 12 h and on the table with normal saline 20 ml/kg, before the surgery. Prophylactic preoperative antibiotics amoxicillin, clavulanic acid, and metronidazole.
Operative procedure
Single-stage laparoscopic Duhamel procedure was performed in all our patients, except one patient with long-segment HD where the transitional zone was proximal to the transverse colon, we performed a laparoscopic diverting ileostomy, multiple seromuscular biopsies in one sitting, followed by laparoscopic Duhamel pull through and closure of ileostomy 6 months later in a second stage.
The primary surgeon stood at the right side of the patient; the camera man was on the left side of the surgeon. Pneumoperitoneum was carried out using an open technique through the umbilicus with the pressure of 10–12 mm Hg. We introduced 2 ports, 5 mm, one was below xiphi sternum and another was at the right lower quadrant, and in only long segment HD cases we needed an additional port placed in the left lower quadrant.
In the laparoscopic part
After placement of ports, in all cases seromuscular biopsies were taken by endoscopic scissors [Figure 1] for fresh frozen section histopathological examination, the site of the biopsies was closed by vicryl violet 3/0, to decide the level of pull-through, the transitional zone was determined before devascularisation or mobilisation of the colon both visually and by intra-operative frozen section histopathological examination.
Figure 1.
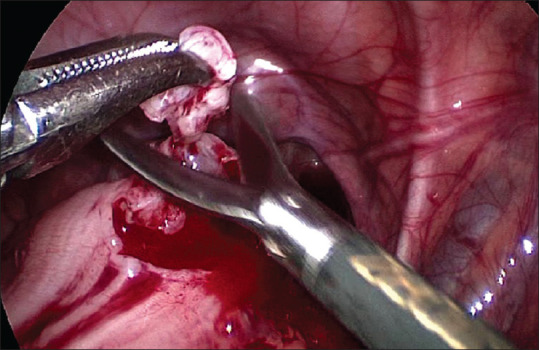
Seromuscular biopsies were taken for fresh frozen section histopathological examination by endoscopic scissors
In Rectosigmoid aganglionic; A window was made in the sigmoid mesentery and a stitch was taken through the window into the abdominal wall to elevate it and facilitate proximal and distal mobilisation of the colon, the sigmoid was mobilised. Proximal ganglionic bowel was mobilised, preserving the marginal arcade
In the long aganglionic segment in which the transitional zone was at the descending colon, we followed the same principal but with division at the splenic flexure to pull down the colon above the funnel to the pelvis without tension however, in one case where the transitional zone were at transverse colon we completed dissection of the transverse colon from gastrocolic ligament and ligation of upper left colic vessels using Ligasure preserving marginal arcade
In all cases, we incised sharply the peritoneal reflection to facilitate mobilisation of only the posterior wall of the aganglionic rectum, the posterior part of the rectum below the peritoneal reflection was mobilised as much as possible within 2–3 cm of peritoneal reflection in the retrorectal avascular plane [Figure 2], the remnant aganglionic rectum was divided by 55 mm linear cutter gastrointestinal (GI) stapler as low as possible [Figure 3] leaving short aganglionic rectal stump above colorectal anastomosis [Figure 4], after completion of laparoscopic dissection and assurance of haemostasis, the ports were left in situ and the patient's position was changed for transanal dissection of the remaining rectum.
Figure 2.
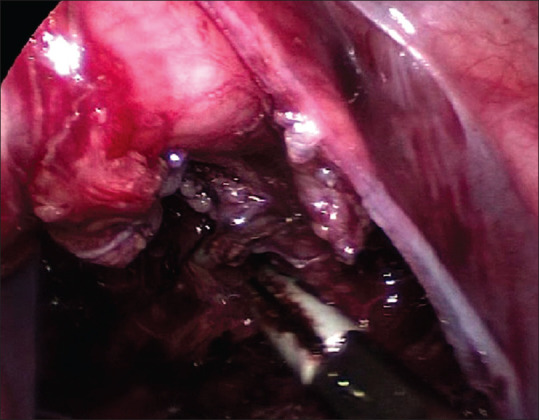
Posterior part of the rectum below the peritoneal reflection was mobilised as much as possible within 2–3 cm of peritoneal reflection in the post-rectal avascular plane
Figure 3.

The remnant aganglionic rectum was divided by 55 mm linear cutter gastrointestinal stapler as low as possible
Figure 4.
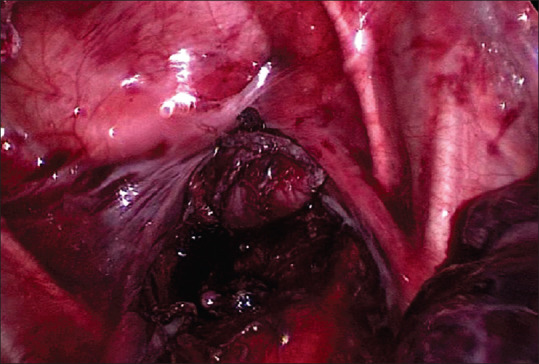
Short aganglionic rectal stump above colo-rectal anastomosis
In the transanal part
We made a curved incision in the posterior rectal wall 1 cm above the dentate line from 3' to 9' o clock position
Stay sutures were done to hold the ends of the common wall of the rectum before pulling down the new ganglionated colon without twisting in the retrorectal avascular plane. Anastomosis between the posterior rectal wall and anterior wall of the colon was performed by linear cutter GI stapler 75 mm. The anastomosis was continued with the anus.
Once the anastomosis was completed, laparoscopy was performed again to check for the orientation of the pull-through bowel. A drain was placed in the pelvis and the port sites were closed.
Postoperative care
All patients received their immediate postoperative care in the intermediate care unit. Patients were maintained on intravenous (I. V) fluid therapy with continuous nasogastric decompression and I. V. antibiotics for 48 h. Oral feeding was initiated when bowel sounds were audible.
Patients were discharged when the full oral diet was reached, rectal irrigation daily starting from day 7 post-operative to decrease the incidence of enterocolitis and after 2 weeks from discharge we taught parents to perform home dilatation with Hegar dilators, Patient's outcome was evaluated for faecal consistency, the frequency of soiling and presence of perianal skin excoriation at 3, and 6 months after the procedure.
Statistical analysis
Statistical data analysis was performed using Microsoft® Excel® 2013 (15.0.4420.1017, Microsoft corporation, Washington, USA)32-bit software. Descriptive data analysis, as well as analytical analysis, were done using analysis of variance: Single Factor test, t-test: Two-Sample Assuming Unequal Variances and F-test two-sample for variances.
RESULTS
Eight patients older than 3 years coming to a tertiary paediatric surgical Centre, 5 males and 3 females. The age of patients ranged from 3 years to 7 years. There were varieties in operating time according to the length of the aganglionic segment, average time was 2 h in cases of classic rectosigmoid Hirshsprung disease, while in cases where the funnel was extending higher the average time was 4 h.
In all our cases oral intake was started 48 h after operation. The mean hospital stay was 5 days (range 4–7 days).
Early outcome through the first 3 months postoperatively: We had 2 cases complaining of enterocolitis that responded to conservative treatment, we observed 2 cases of perianal excoriation that responded to medical treatment, while late outcome after 3 months postoperative was reported: We had 2 cases with attacks of enterocolitis at 6 months and 9 months postoperatively that needed conservative treatment after admission in the hospital, in the form of parenteral antibiotics, rectal irrigation, I. V fluids and NP0. There was neither anastomotic leak, nor stenosis.
DISCUSSION
Georgeson et al. in 2008 reported conversion from Veress needle to open transumbilical in 12 cases of laparoscopic-assisted endorectal colon pull-through,[7,8,9] In all our cases, the open technique showed safer introduction and reliability.
Some authors used laparoscopy only in case of long aganglionic segment HD, based on contrast enema study,[10,11] Ksia et al.,[12] did a transanal Soave one-stage endorectal pull-through procedure for 20 cases older than 2 years and used laparoscope only when there is difficulty in pull through while in our study, we used laparoscopy in all our cases either short or long-segment HD, to decrease the incidence of injury of the pelvic nerves, decrease anal dissection and consequently overstretching anal sphincters during rectal mobilisation from below this preserving continence.
Gerogeson and Muensterer documented (7.5%) cases with enterocolitis in his multicenter study,[9] and in Wang et al. reported 21%, but fortunately, all cases responded to conservative measures. Anastomotic stricture occurred in 13% responded to regular dilatations. Wang et al. reported perforation in one case (1.6%) and leakage in 2 cases (3.3%) that was managed by diverting colostomy,[13] while Georgeson et al. had no cases with perforation but 2 cases of leakage (2.5%). No mortality was reported in the follow-up period. Continence to stools needs longer period of follow-up especially in the younger age group,[14] The procedure is cost-effective and accepted by the parents.[15]
While in this study we have enterocolitis in 4 cases that responded to conservative measurements, Perianal excoriation occurred in 2 cases that responded to zinc oxide ointment applications and constipating agents, no anastomotic stricture, there were no cases of anastomotic leak.
Takawira et al.[16] found that haematoxylin and eosin-stained fresh frozen sections remain the criterion standard for its highest sensitivity and specificity, intra-operative fresh frozen section histological examination allowed proper identification of the normal ganglionic level so that no remnant aganglionosis was missed; in support of such a policy, throughout the follow-up period, no patient developed recurrent constipation. Moreover, Takahashi et al.[17] and Bonnard et al.[18] found that laparoscopic biopsy-taking can aid diagnosis and decision-making in HD cases, while, Thomson et al.[19] conducted a meta-analysis for the outcomes following totally Transanal endorectal pull-through versus Transanal endorectal pull-through with any form of laparoscopic assistance for infants with uncomplicated HD, and found no significant differences concerning postoperative enterocolitis, faecal incontinence, or constipation but in this study we depended on contrast enema, anorectal manometry and biopsy with histology for the diagnosis of HD also, laparoscopic biopsy-taking can aid diagnosis with intra-operative fresh frozen section histological examination allowed proper identification of the normal ganglionic level and decision-making, especially in cases with ill-defined funnel with contrast enema.
Travassos et al.[20] reported the Duhamel operation is the best procedure for a 'failed' Swenson operation, long-segment HD, total colonic agangliosis and in cases of difficult mucosectomy via repetitive attack of enterocolitis make the dissection difficult and grossly dilated hypertrophic rectum, while in this study, we did laparoscopic Duhamel in cases of older children to minimise pelvic dissection stressing on preserving continence
Singh et al. 2017[21] reported late referral of most neonates presenting with recurrent enterocolitis, colonic perforations, so they preferred staged Duhamel procedure, after decompressing colostomy was done, also they have no frozen sections, while in this study we did Duhamel procedure in all 7 cases on one stage depending on rectal wash for 3–6 months before surgery to reduce colonic caliber, frozen section was mandatory in all our cases, only in one case of long-segment HD where transitional zone proximal to the transverse colon, we did laparoscopic diverting ileostomy, multiple seromuscular biopsies in one sitting then after 6 months we did laparoscopic Duhamel pull through and closure of ileostomy in other stage.
CONCLUSION
Laparoscopic Duhamel for the management of HD more than 3 years is safe, feasible procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mabula JB, Kayange NM, Manyama M, Chandika AB, Rambau PF, Chalya PL. Hirschsprung's disease in children: A five year experience at a university teaching hospital in northwestern Tanzania. BMC Res Notes. 2014;7:410. doi: 10.1186/1756-0500-7-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soret R, Mennetrey M, Bergeron KF, Dariel A, Neunlist M, Grunder F, et al. Ente-Hirsch study group. A collagen VI-dependent pathogenic mechanism for Hirschsprung's disease. J Clin Invest. 2015;125:4483–96. doi: 10.1172/JCI83178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fukuzawa M. Progress in the treatment of and research on Hirschsprung's disease. Nihon Geka Gakkai Zasshi. 2014;115:312–6. [PubMed] [Google Scholar]
- 4.Saleh W, Rasheed K, Mohaidly MA, Kfoury H, Tariq M, Rawaf AA, et al. Management of Hirschsprung's disease: A comparison of Soave's and Duhamel's pull-through methods. Pediatrics Surg Int. 2004;20:590–3. doi: 10.1007/s00383-004-1237-0. [DOI] [PubMed] [Google Scholar]
- 5.Antao B, Roberts J. Laparoscopic-assisted transanal endorectal coloanal anastomosis for Hirschsprung's disease. J Laparoendosc Adv Surg Tech A. 2005;15:75–9. doi: 10.1089/lap.2005.15.75. [DOI] [PubMed] [Google Scholar]
- 6.Arts E, Botden SM, Lacher M, Sloots P, Stanton MP, Sugrman I, et al. Duhamel versus transanal endorectal pull through (TERPT) for the surgical treatment of Hirschsprung's disease. Tech Coloproctol. 2016;20:677–82. doi: 10.1007/s10151-016-1524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Georgeson KE, Fuefner MM, Hardin WD. Primary laparoscopic pull-through for Hirschsprung's disease in infants and children. J Pediatr Surg. 1995;30:1017–21. doi: 10.1016/0022-3468(95)90333-x. [DOI] [PubMed] [Google Scholar]
- 8.Gerogeson KE, Cohen RD, Hebra A, Jona JZ, Powell DM, Rothenberg SS, et al. Primary laparoscopic endorectal colon pull-through for Hirschsprung's disease: A new gold standard. Ann Surg. 1999;229:678–82. doi: 10.1097/00000658-199905000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerogeson KE, Muensterer OJ. Holschnider AM, Puri P, editors. Laparoscopic Assisted Transanal Pull-through for Hirschsprung's Disease. Hirschsprung's Disease and Allied disorders. (3rd ed) 2008 Springer;(Ch. 23):323–33. [Google Scholar]
- 10.Hadidi A. Transanal endorectal pull-through for Hirschsprung's disease: Experience with 68 patients. J Pediatr Surg. 2003;38:1337–40. doi: 10.1016/s0022-3468(03)00392-0. [DOI] [PubMed] [Google Scholar]
- 11.Langer JC, Minkes RK, Mazziot MV, Skinner MA, Winthrop AL. Transanal one-stage Soave procedure for infants with Hirschsprung's disease. J Pediatr Surg. 34:148–51. doi: 10.1016/s0022-3468(99)90246-4. [DOI] [PubMed] [Google Scholar]
- 12.Ksia A, Yengui H, Saad MB, Sahnoun L, Maazoun K, Rachida L, et al. Soave transanal one-stage endorectal pull-through in the treatment of Hirschsprung's disease of the child above two-year-old: A report of 20 cases. Afr J Paediatr Surg. 2013;10:362–6. doi: 10.4103/0189-6725.125449. [DOI] [PubMed] [Google Scholar]
- 13.Wang NL, Lee HC, Yeh ML, Chang PY, Sheu JC. Experience with primary laparoscopy-assisted endorectal pull-through for Hirschsprung's disease. Pediatr Surg Int. 2004;20:118–22. doi: 10.1007/s00383-003-1102-6. [DOI] [PubMed] [Google Scholar]
- 14.Fujiwaraa N, Kaneyama K. Comparative study of laparoscopic-assisted pull-through and open pullthrough for Hirschsprung's disease with special reference to postoperative faecal incontinence. J Pediatr Surg. 2007;42:2071–4. doi: 10.1016/j.jpedsurg.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 15.Bufo AJ, Chen MK, Shah R, Gross E, Cyr N, Lobe TE. Analysis of the costs of surgery for Hirschsprung's disease: One-stage laparoscopic pull-through versus two-stage Duhamel procedure. Clin Pediatr (Phila) 1999;38:593–6. doi: 10.1177/000992289903801004. [DOI] [PubMed] [Google Scholar]
- 16.Takawira C, D’Agostini S, Shenouda S, Persad R, Sergi C. Laboratory procedures update on Hirschsprung disease. J Pediatr Gastroenterol Nutr. 2015;60:598–605. doi: 10.1097/MPG.0000000000000679. [DOI] [PubMed] [Google Scholar]
- 17.Takahashi T, Kato Y, Okazaki T, Koga H, Lane GJ. Patchy innervation confirmed in pull-through bowel with normal conventional biopsy results in Hirschsprung's disease − The benefit of circumferential biopsying. Hepatogastroenterology. 2013;60:1014–7. doi: 10.5754/hge11238. [DOI] [PubMed] [Google Scholar]
- 18.Bonnard A, Terrasa JB, Viala J, Aizenfisz S, Berrebi D, Ghoneimi AE. Abdominal cellulitis following a laparoscopic procedure: A rare and severe complication. European J Pediatr Surg Rep. 2014;2:67–70. doi: 10.1055/s-0033-1363777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomson D, Allin B, Long AM, Bradnock T, Walker G, Knight M. Laparoscopic assistance for primary transanal pull-through in Hirschsprung's disease: A systematic review and meta-analysis. BMJ Open. 2015;5:e006063. doi: 10.1136/bmjopen-2014-006063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Travassos DV, Bax NM, Van der Zee DC. Duhamel procedure: A comparative retrospective study between an open and a laparoscopic technique. Surg Endosc. 2007;21:2163–5. doi: 10.1007/s00464-007-9317-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh S, Wakhlu A, Ahmad I, Srivastava NK. The laparoscopic assisted Duhamel pull through procedure for hirschsprung's disease: Our technique and short term results. J Pediatr Neonatal Care. 2017;7:00281. DOI: 10.15406/jpnc.2017.07.00281. [Google Scholar]


