Abstract
Purpose
Clinicians have increasingly encountered traumatic brain injuries (TBI) related to electric scooter (ES) accidents. In this study, we aim to identify the modifiable risk factors for ES-related TBIs.
Methods
A retrospective cohort of consecutive patients treated for ES-related traumatic brain injuries in a tertiary university hospital between May 2019 and September 2021 was identified and employed for the study. The characteristics of the accidents along with the clinical and imaging findings of the injuries were collected from the patient charts.
Results
During the study period, 104 TBIs related to ES accidents were identified. There was a high occurrence of accidents late at night and on Saturdays. In four cases, the patient’s helmet use was mentioned (3.8%). Seventy-four patients (71%) were intoxicated. At the scene of the accident, seventy-seven (74%) of the patients had a Glasgow Coma Scale score of 13–15, three patients (3%) had a score of 9–12, and two patients (2%) had a score of 3–8. The majority (83%) of TBIs were diagnosed as concussions. Eighteen patients had evidence of intracranial injuries in the imagining. Two patients required neurosurgical procedures. The estimated population standardized incidence increased from 7.0/100,000 (95% CI 3.5–11/100,000) in 2019 to 27/100,000 (95% CI 20–34/100,000) in 2021.
Conclusions
Alcohol intoxication and the lack of a helmet were common in TBIs caused by ES accidents. Most of the accidents occurred late at night. Targeting these modifiable factors could decrease the incidence of ES-related TBIs.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00701-021-05098-2.
Keywords: Traumatic brain injury, TBI, Electric scooter, Brain trauma, Traffic accident
Introduction
At the end of 2017, rental electric scooters (ESs) were first introduced into the USA as a new, nationwide means of transport. Recently, they have become a significant means of transportation for urban residents and have assumed a substantial portion of the micro-mobility market in cities worldwide.
Since the introduction of rentable ESs in Finland, there have been frequent reports of accidents in the media and a widespread debate over the legislation on ES usage. In our city, ESs have been available for rent since the beginning of May 2019. In Finland, the maximum speed of ESs is limited to 25 km per hour. In the middle of July 2021, the maximum speed was lowered to 15 km/hour during the night at weekends (Fri-Sun, from 23:00 to 05:00). By jurisdiction, ESs are treated in a similar way to bicycles concerning helmet use and intoxication. Helmets are required by law but not enforced. Driving under the influence of alcohol is forbidden but not strictly enforced unless the driver causes evident danger to the public.
The findings of a recent review suggest frequent injuries to the head and extremities in ES-related accidents [30]. The reported occurrence of head injuries has varied between 15 and 40% of all ES-related injuries [16, 31]. Since ESs have only recently been introduced to the public, up-to-date data on injury patterns of ES-related TBIs are sparse. As their national and worldwide popularity increases, it is critical to provide better evidence on the injury patterns and severity of ES-related brain traumas. This information enables estimating the burden these injuries pose to the emergency departments and the health care system. Understanding the risk factors associated with injuries may better inform public decisions, affect individual safety, and guide future policy.
In this study, we describe the characteristics of ES-related traumatic brain injuries treated in a tertiary university hospital over a 2.5-year period. We also describe modifiable risk factors for electric scooter injuries. We hypothesized that the rate of helmet usage is low, the accidents occur mainly late at night, and that the accidents are frequently involved with alcohol intoxication.
Patients and methods
Study design
This study was conducted in the city of Turku, located in Southwest Finland. Approximately 20% of the population in Turku is aged between 20 and 29 years [19]. Turku is the only city located in the region of Southwest Finland in which rentable ESs are available. Patients requiring immediate or urgent specialized care in the city of Turku can seek treatment in Turku University Hospital which is a tertiary hospital covering a city population of 194,391 in 2020. Our study center is the primary emergency department (ED) in the region, in which all traumatic injuries are treated. In 2020, a total of 1472 patients with TBIs were treated at our hospital. An institutional research board permit was obtained.
A retrospective cohort of consecutive patients was collected using patient charts from our center. We searched for patients diagnosed with intracranial injuries between 1st of May 2019 and 30th of September 2021 using International Classification of Diseases (ICD) codes S06.0-S06.9 and a keyword search for electrical scooters (electric scooter, E-scooter, etc.). After this, a keyword search without the ICD-codes was conducted for TBIs involving electrical scooters. This provided no additional patients. The involvement of an ES was then verified, and eligible patients were included in the study (Fig. 1). Patients with injuries related to non-electronic scooters, moped scooters, or other seated scooters were excluded. Follow-up visits for previous ES-related injuries were excluded.
Fig. 1.

Flowchart of the patient selection. Injuries related to other transportation methods than electric scooters and follow-up visits for previous injuries were excluded
Data collection
The following data were collected: age, gender, time and date of the injury, helmet use, presence of primary unconsciousness, transportation by ambulance to the hospital, blood or breath alcohol level, Glasgow Coma Scale (GCS) score assessed at the scene of the accident or the emergency department (ED), possible other injuries sustained, the exact ICD-code, the type of radiological imaging, length of hospitalization, and interventions required for the TBI. Computed tomography (CT) and magnetic resonance imaging (MRI) scans were evaluated.
We classified the intracranial traumas according to the imaging findings: (1) loss of consciousness or concussion without CT or MRI findings (referred to as imaging negative), (2) CT or MRI diagnosed brain hemorrhages treated non-operatively (imaging positive), and (3) patients with CT and MRI diagnosed brain hemorrhages requiring operative treatment (imaging positive requiring operative treatment) [28]. The patients were also classified according to the Glasgow Coma Score addressed at the scene of the accident as follows: (1) mild TBI with GCS score 13–15, (2) moderate TBI with GCS score 9–12, and (3) severe TBI with GCS score 3–8.
Data analysis
Analysis was conducted in R (R 4.1.1, R Core Team, 2020). Descriptive analyses were reported as the means and SDs, medians and both quartiles and ranges, or absolute numbers and percentages referring to the study groups. Age-standardized rate allows comparison of incidences between different populations [6]. We calculated direct age- and sex-standardized incidence rates by multiplying the age-specific and age-sex-specific incidence rates with the corresponding age bracket weights of the European standard population (ESP) [6]. The 95% confidence intervals for European age-standardized rates (EASR) were calculated using Poisson approximation [6].
Results
Patient and event characteristics
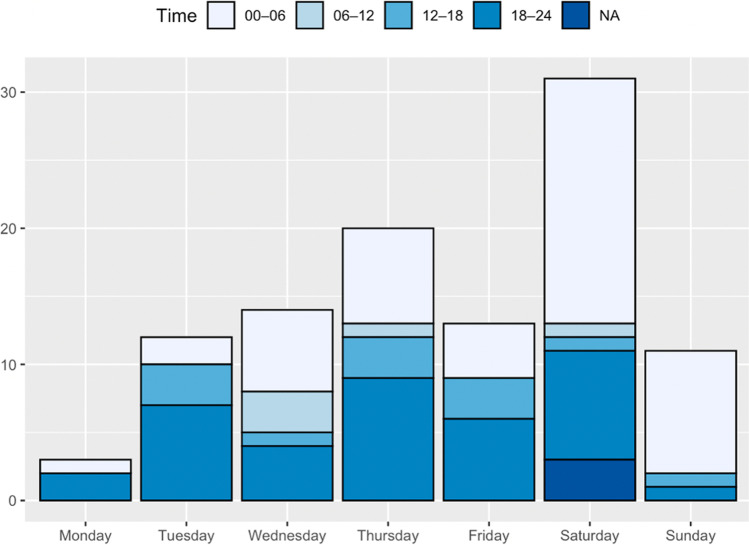
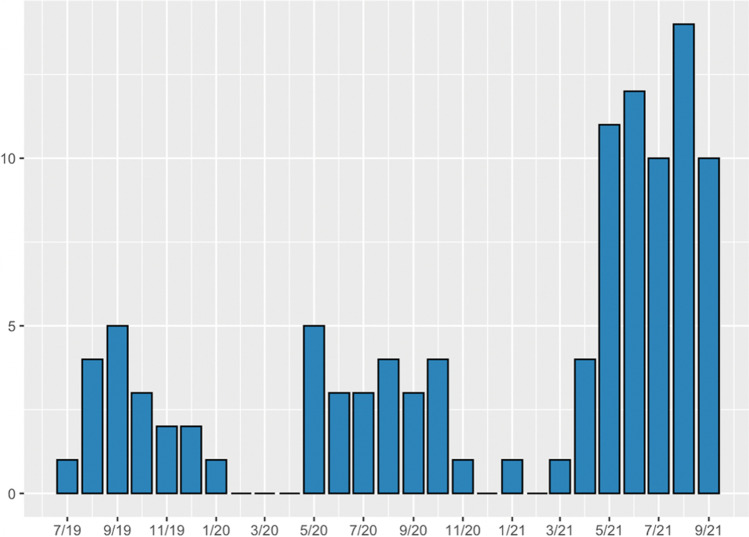
In total, 149 patients were identified, of whom after exclusion 104 were selected for the final analyses (Fig. 1). The demographic details of the patient population are presented in Table 1. There were 63 (61%) males and 41 (39%) females. The median age at the time of injury was 23.7 (range 5–71) years. Forty-nine percent of the patients were young adults, between the ages of 18 and 25. The highest prevalence was 215/100,000 in the age group of 20–25 years (264 in males and 174 in females, Table 2). The prevalence was higher in males (68 in males vs. 41 in females, Supplementary Tables I, II). The EASR during the whole study period was 44/100,000 (95%CI 35–53/100,000, Table 2). EASRs were 57/100,000 (95%CI 42–72/100,000) for males and 32/100,000 (95%CI 21–42/100,000) for females during the study period. There was an increase in the EASR from 7.0/100,00 in 2019 (95%CI 3.5–11/100,000) to 27/100,000 in 2021 (95%CI 20–34/100,000, Supplementary Tables III, V). There was a peak of injuries late at night: 81% of the accidents occurred between 6 p.m. and 6 a.m. (Fig. 2). The occurrence was the highest during Saturdays (29.8%) and Thursdays (19.2%). The injuries were most common during the summer months: 82% of the accidents occurred between May and September (Fig. 3).
Table 1.
Patient characteristics
| Age, median (years), (Q1, Q3, range) | |
|---|---|
| All | 24 (20.5, 30.1, 5–70) |
| Male | 24 (21.1, 32.8, 8–55) |
| Female | 22 (20.3, 26.8, 5–70) |
| Age group (years), n (%) | |
| < 18 | 10 (9.6) |
| 18–25 | 51 (49.0) |
| 25–40 | 31 (29.8) |
| > 40 | 12 (11.5) |
| Sex | |
| Male | 63 (60.6) |
| Female | 41 (39.4) |
| Time of accident | |
| Midnight to 6 a.m | 47 (45.2) |
| 6 a.m. to noon | 5 (4.8) |
| Noon to 6 p.m | 12 (11.5) |
| 6 p.m. to midnight | 37 (35.6) |
| Unknown | 3 (2.9) |
| Day of accident | |
| Monday | 3 (2.9) |
| Tuesday | 12 (11.5) |
| Wednesday | 14 (13.5) |
| Thursday | 20 (19.2) |
| Friday | 13 (12.5) |
| Saturday | 31 (29.8) |
| Sunday | 11 (10.6) |
| Month of accident | |
| January | 1 (1.0) |
| February | 0 (0) |
| March | 1 (1.0) |
| April | 4 (3.8) |
| May | 16 (15.4) |
| June | 15 (14.4) |
| July | 14 (13.5) |
| August | 22 (21.2) |
| September | 18 (17.3) |
| October | 7 (6.7) |
| November | 4 (3.8) |
| December | 2 (1.9) |
| Intoxication | |
| No intoxication | 21 (20.2) |
| Alcohol reported | 74 (71.2) |
| < 0.5‰ | 1 (1.4) |
| 0.5–1.2‰ | 7 (9.6) |
| > 1.2‰ | 58 (79.4) |
| Alcohol reported but level unknown | 7 (9.6) |
| Unknown | 9 (8.7) |
| Helmet use | |
| Yes | 4 (3.8) |
| No | 67 (64.4) |
| Unknown | 33 (31.7) |
| Collision | |
| No | 96 (92.3) |
| Car | 5 (4.8) |
| E-scooter | 1 (1.0) |
| Bicycle | 1 (1.0) |
| Moped | 1 (1.0) |
Table 2.
European age standardized rates of all 321 ES-related TBIs in Turku 2019–2021
| Age | European standard population 2013 | Population in Turku (2020) | ES-related TBIs | Prevalence in the age group per 100,000 | European age standardized rate (EASR) |
|---|---|---|---|---|---|
| 0–4 | 5,500 | 8,014 | 0 | 0.0 | 0.0 |
| 5–9 | 5,500 | 8,372 | 2 | 23.9 | 1.3 |
| 10–14 | 5,500 | 8,052 | 7 | 86.9 | 4.8 |
| 15–19 | 6,000 | 8,775 | 9 | 102.6 | 5.6 |
| 20–24 | 6,000 | 19,995 | 43 | 215.1 | 12.9 |
| 25–29 | 6,500 | 19,069 | 17 | 89.2 | 5.4 |
| 30–34 | 7,000 | 15,181 | 9 | 59.3 | 3.9 |
| 35–39 | 7,000 | 13,266 | 5 | 37.7 | 2.6 |
| 40–44 | 7,000 | 11,419 | 1 | 8.8 | 0.6 |
| 45–49 | 7,000 | 9,781 | 2 | 20.5 | 1.4 |
| 50–54 | 6,500 | 10,578 | 7 | 66.2 | 4.6 |
| 55–59 | 6,000 | 10,809 | 1 | 9.3 | 0.60 |
| 60–64 | 5,500 | 10,435 | 0 | 0.0 | 0.0 |
| 65–69 | 5,000 | 10,560 | 0 | 0.0 | 0.0 |
| 70–74 | 9,000 | 11,317 | 1 | 8.8 | 0.44 |
| 75– > 90 | 5,500 | 18,768 | 0 | 0.0 | 0.0 |
| All ages | 100,000 | 194,391 | 104 | 53.5 | 44.2 |
Fig. 2.
Daily prevalence and the time of the ES-related injuries. NA = Day known; exact time not available
Fig. 3.
Monthly prevalence. The prevalence of ES-related TBIs increased towards the end of the study period and was lower in the winter months. Rentable ESs were generally not available during the snow cover
The majority of the patients (64%) did not wear a helmet at the time of the accident and in only four cases was the patient’s use of a helmet mentioned (3.8%). No information concerning helmet usage was available for 33 patients (32%). Ten cases involved riding the scooter with two persons onboard (9.6%). Primary unconsciousness was reported in 33 (32%) patients. GCS addressed at the scene of the accident was 13–15 for seventy-seven (74%) patients, 9–12 for three (3%) patients, and 3–8 for two (2%) patients. In 22% of the cases, GCS was not reported. Seventy-four patients (71%) were brought to ED by ambulance. Forty-nine patients were discharged directly from ED without head imaging or imaging findings. In patients requiring surveillance, 36 were discharged during the first 24 h. Fourteen patients required surveillance for one to seven days (mean 2.0, range 1–). Three patients required longer surveillance and were discharged after seven, eight, and 14 days. None of the patients had ongoing antithrombotic medication.
In total, 74% of the patients were under the influence of alcohol. The mean alcohol level in breath or blood was 1.8‰ (range, 0.3–3.6) in intoxicated patients. Fifty-eight (77%) intoxicated patients had alcohol concentrations higher than 1.2‰. As mentioned, 81% of the accidents occurred between 6 p.m. and 6 a.m. In these cases, 86% of the patient were under the influence of alcohol. In one patient, there was a report of cannabis use in addition to alcohol intoxication.
Ten patients had a cranial fracture, nine had a maxillofacial fracture, and three had both skull and maxillofacial fractures. Two patients required operative treatment for maxillofacial fractures. Other fractures involved scapula, proximal phalange, and rib fractures.
Traumatic brain injuries (TBIs)
A CT scan was performed on 80 patients and an MRI scan on two patients. Twenty-two patients (21%) were clinically evaluated and required no imaging. Most injuries were diagnosed as concussions (86 cases, 82%, Table 3). In patients with CT or MRI scans, 64 patients (78%) had no traumatic intracranial findings. Eighteen patients had imaging positive intracranial injury (Table 4). Two of those patients required neurosurgical procedures. Imaging positive injuries were as follows: diffuse traumatic brain injury in three patients (3%), brain contusion in seven patients (7%), epidural hemorrhage in one patient (1%), traumatic subdural hemorrhage in seven patients (7%), and traumatic subarachnoid hemorrhage in seven patients (7%). One patient required hematoma evacuation after which an intracranial pressure monitoring was installed. The patient remained under surveillance in the neurosurgical department for two days. Another patient required intracranial pressure monitoring and remained under surveillance for seven days. Eighty-nine percent of the imaging positive patients were under the influence of alcohol (mean alcohol level 1.8‰.).
Table 3.
Injury characteristics
| n (%) | |
|---|---|
| Transport to emergency department | |
| Ambulance | 74 (71.2) |
| Ambulatory | 30 (28.8) |
| GCS score at the scene of the accident | |
| 13–15 | 77 (74.0) |
| 9–12 | 3 (2.9) |
| 3–8 | 2 (1.9) |
| Unknown | 22 (21.2) |
| Primary unconsciousness | |
| Yes | 33 (31.7) |
| No | 54 (51.9) |
| Unknown | 17 (16.3) |
| Traumatic brain injuries (ICD-10) | |
| Concussion (S06.0) | 86 (82.7) |
| Diffuse traumatic brain injury (S06.2) | 3 (2.9) |
| Brain contusion (S06.3) | 7 (6.7) |
| Epidural hemorrhage (S06.4) | 1 (1.0) |
| Traumatic subdural hemorrhage (S06.5) | 7 (6.7) |
| Traumatic subarachnoid hemorrhage (S06.6) | 7 (6.7) |
| Cranial fractures | |
| Yes | 22 (21.2) |
| Cranial | 10 (45.5) |
| Maxillofacial | 9 (40.9) |
| Both | 3 (13.6) |
| No | 82 (78.8) |
| Other fractures | |
| Yes | 3 (2.9) |
| Upper extremity | 2 (66.6) |
| Rib | 1 (33.3) |
| No | 101 (97.1) |
| Radiological imaging | |
| Yes | 82 (78.8) |
| CT | 80 (97.6) |
| MRI | 2 (2.4) |
| No | 22 (21.2) |
| Imaging | |
| Imaging negative | 64 (78.0) |
| Imaging positive | 16 (19.5) |
| Imaging positive requiring neurosurgical treatment | 2 (2.4) |
| Length of hospital stay | |
| < 4 h | 49 (47.1) |
| 4–24 h | 38 (36.5) |
| 1–7 days | 14 (13.5) |
| > 7 days | 3 (2.9) |
GCS, Glasgow Coma Scale
Table 4.
Characteristics of imaging positive patients
| Gender | Age | Time of the incident | Type of accident | Alcohol level | Reported helmet use | Primary GCS* | Primary unconsciousness | Fracture | Transportation to the ED | Imaging | Description of the findings | Operative treatment | Length of hospital stay |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | 55 | 18–24 | Fall | 2.2 | No | 13–15 | Yes | Maxillofacial | Ambulance | CT | Traumatic subarachnoid hemorrhage of 2.8 mm and brain contusion | No | 6 h |
| Male | 38 | 00–06 | Fall | 2.9 | No | 13–15 | No | Cranial | Ambulance | CT | CT Brain contusion of 0.97 ml | No | 2 days |
| Male | 33 | 18–24 | Fall | 3.6 | No | 13–15 | Yes | Cranial | Ambulance | CT | Traumatic subdural hemorrhage and brain contusion | No | 2 days |
| Female | 44 | 00–06 | Fall | 1.1 | No | 13–15 | No | Maxillofacial | Ambulance | CT | Diffuse brain injury | No | 8 days |
| Male | 22 | 00–06 | Fall | 1.1 | Unknown | 13–15 | Yes | Cranial | Ambulance | CT | Traumatic subarachnoid hemorrhage | No | 2 days |
| Male | 39 | 06–12 | Fall | 2.0 | No | 13–15 | Unknown | None | Ambulance | CT | Traumatic subarachnoid hemorrhage and brain contusion | No | Until morning |
| Female | 20 | 00–06 | Fall | 2.4 | No | 3–8 | Yes | Cranial | Ambulance | CT | Traumatic subdural hemorrhage and traumatic subarachnoid hemorrhage of 11 mm | Intracranial pressure monitoring | 7 days |
| Female | 20 | 00–06 | Fall | 1.7 | No | 9–12 | Unknown | None | Ambulance | MRI | Diffuse brain injury | No | Until morning |
| Male | 21 | 18–24 | Fall | 0 | Unknown | 13–15 | Yes | Cranial | Ambulatory | CT | Brain contusion of 14 ml | No | Until morning |
| Male | 27 | 00–06 | Fall | 1.8 | No | 13–15 | Yes | Cranial | Ambulance | CT | Traumatic subdural hemorrhage of 5.9 mm | No | 2 days |
| Male | 14 | 18–24 | Collision with a motorbike | 0 | No | 9–12 | Yes | Cranial | Ambulance | CT | Traumatic subdural hemorrhage of 8.0 mm | No | 14 days |
| Male | 24 | 00–06 | Fall | 2.0 | No | 14 | Yes |
Maxillofacial and Cranial |
Ambulance | CT | Traumatic subdural hemorrhage of 6.0 mm, traumatic subarachnoid hemorrhage, and brain contusion | No | 2 days |
| Male | 23 | 00–06 | Fall | 2.7 | Unknown | 9 | Yes | None | Ambulance | CT | Traumatic subarachnoid hemorrhage | No | 2 days |
| Male | 48 | 00–06 | Fall | 2.2 | No | 15 | No |
Maxillofacial and cranial |
Ambulance | CT | Traumatic subarachnoid hemorrhage | Hematoma evacuation and intracranial pressure monitoring | 2 days |
| Female | 19 | 00–06 | Fall | 1.5 | No | 5 | Yes | None | Ambulance | CT | Traumatic subarachnoid hemorrhage | No | 2 days |
| Male | 50 | 18–24 | Fall | 2.8 | No | 13–15 | Yes | Maxillofacial and cranial | Ambulance | CT | Traumatic subarachnoid hemorrhage | No | 4 days |
| Male | 19 | 00–06 | Fall | 1.7 | No | 13–15 | Unknown | Maxillofacial | Ambulance | CT and MRI | Traumatic subarachnoid hemorrhage | Surgical treatment of maxillofacial fractures | 2 days |
| Male | 48 | 18–24 | Fall | 1.5 | No | 13–15 | No | Rib | Ambulance | CT | Traumatic subarachnoid hemorrhage | Surgical treatment for fractured scapula | 1 day |
*Glasgow Coma Scale, exact score if known
Discussion
The present study demonstrates an evident increase in the incidence of ES-related TBIs in our institute between 2019 and 2021. The accident patterns were as we hypothesized: high alcohol levels and lack of helmet use were prominently present in patients with ES-related TBIs. Moreover, most accidents occurred during the summer months and late at night.
Common ES-related injuries include head traumas, TBIs, and fractures [18]. Previous studies have reported a high incidence of head injuries and TBIs in ES accidents [11, 20, 26, 32]. Head traumas, half of which included TBI, were the most common reason for ED visits for ES injuries in a study of 70,544 cases [7]. A recent case series described 13 severe injuries, which required neurosurgical intervention including skull fractures, central cord syndrome, and vertebral compression fractures related to ES injuries [23]. In that study, one patient was pronounced dead on arrival due to epidural hematoma resulting in midline shift and bilateral frontal subarachnoid hemorrhages [23]. In our study, eighteen patients had imaging positive injuries with two patients requiring neurosurgical procedures. Most patients in this study were under the age of 30 years. TBIs are a major cause of death and disability in the younger adult population [4, 12, 14]. Although the long-term effects were not assessed in our study, previous results show that young patients can be vulnerable to long-term difficulties due to a lack of coping skills [5]. Both upper and lower extremity fractures requiring operative treatment are reported in ES-related accidents [8, 24, 29]. In our cohort, the low incidence of upper extremity fractures may indicate that these patients may not have been able to react to the sudden fall or collision.
Although ES-related injuries make up only a minor portion of all ED visits for traumatic injuries, the increasing trend in the current study and previous studies is alarming [7, 9, 17]. A recent study showed a twofold increase in the incidence of E-scooter-related injuries in the USA between 2018 and 2019 [7]. According to a recent study, the incidence of ES-related injuries increased from 2.42 in 2017 to 8.63 per 100,000 person-years in the USA [9]. As ES usage is becoming increasingly popular, a parallel increase would be expected to occur in the rates of ES-related accidents and TBIs. There was an increasing trend of cases towards the end of the study period, which is likely related to the increased number of ESs and the loosening of the Covid-19 pandemic restrictions. We presume that the ES-related incident numbers in our city could have been higher without the Covid-19 restrictions limiting bar and nightclub visits. This was supported by the substantial increase in accidents in the latter months of the study during which the Covid-19 restrictions were relaxed. Lowering the maximum nighttime speed of the ESs in July 2021 did not seem to reduce the incidence of TBIs in our study. We did not access the incidence of other ways of micro-transportation during the study period. Previous studies have compared ES and bicycle accidents. Studies show that the estimated ED presentation rates per million miles traveled citywide were higher among e-scooter riders than cyclists (RR 3.76; 95% CI, 3.08–4.59) and the ES riders are far less likely to wear helmets [3]. Trip purposes also vary, as bicycles are mainly used to commute to/from work and ESs are mainly used for social reasons and personal business [3, 10]. Cyclists are more frequently injured on the road in incidents involving motor vehicles, and e-scooter riders sustain more injuries on sidewalks without the involvement of other road users. Compared to bicycle accidents, e-scooter accidents more commonly occur on weekends and in association with alcohol [10].
Based on previous research, ES-related accidents are more frequent when compared to cycling or pedestrian accidents [31]. Similar to the findings of the present study, typical ES accidents occur in the summertime, late at night during the end of the week [26, 32]. Conditions such as cold weather, snow, and pandemic quarantine restrictions have been associated with lower rates of ES accidents [26, 32].
Electric scooter accidents are predominantly reported to involve only the scooter rider [2, 25, 26, 31]. In the current study, 92% of cases did not involve other road users, which indicates that most of the accidents result from handling errors. Furthermore, in 90% of the cases, there was a single person on board. Most ES-related injuries were related to alcohol intoxication in previous studies [7, 10, 20, 22, 31]. Our study showed a similar pattern, with 71% of the accidents involving alcohol intoxication. Noticeably, in alcohol-related accidents, the majority (79%) of patients had a breath or blood alcohol content higher than 1.2‰. In Finland, a law prohibits serving alcohol after 4 am, which forces bars and nightclubs to close and appears to demonstrate a significant contrast in the injury rates between 0–6 a.m. and 6–12 a.m. Alcohol intoxication is associated with an elevated risk for TBIs [13, 27]. A fivefold risk for TBI was observed in intoxicated patients in a previous study on ES-related injuries [32]. Another significant factor offering protection from TBIs is helmet use, which reduces the risk of serious head and facial injuries [21]. The helmet usage in ES-related accidents is strikingly low [1, 10, 15, 20, 30]. Supportive to our findings of reported helmet use (3.8%), data from 16 studies (n = 1656) showed that only 4.5% of cases of ES accidents involved helmet use [30]. The use of helmets might have been under-reported in our study, as the data on helmet use was missing in 33% of the cases.
Limitations
This study was limited by the retrospective study design. There may have been patients with ES-related TBIs without proper diagnose codes and/or description of the accident in the patient charts. We did not assess the long-term outcomes of the injuries. Primary imaging findings, GCS on arrival, and the need for operative management can be used for assessing the potential severity of the TBIs; however, using these markers alone does not justify any conclusions on how severe or mild a TBI will be in a follow-up [28]. This was a consecutive patient series treated in a single hospital during a 2.5-year period. We did not assess the prevalence of TBIs related to other transportation methods. We do not have information on the rate of use and numbers of rentable ESs in our area.
Conclusions
Our results show a high rate of alcohol intoxication and lack of helmet use in patients with brain injuries related to electric scooters. The incidence increased towards the end of the study period. Imaging positive injuries were present in 18 patients. These results may be used to inform the public and legislators about the risk of traumatic brain injuries related to electric scooter accidents. We hypothesize that targeting the modifiable factors such as helmet use, preventing driving while intoxicated, and restricting nighttime use could decrease ES-related brain injuries.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Dr. Jussi Posti for his help on this article.
Abbreviations
- CT
Computer tomography
- EASR
European age-standardized rates
- ED
Emergency department
- ES
Electric scooter
- ESP
European Standard Population
- GCS
Glasgow Coma Scale
- MRI
Magnetic resonance imaging
- TBI
Traumatic brain injury
Funding
Open Access funding provided by University of Turku (UTU) including Turku University Central Hospital. Dr. Saarinen has received research funding from NuVasive Inc. not related to the present study. Funding was received from The Päivikki and Sakari Sohlberg Foundation and Vappu Uuspää Foundation for this study.
Declarations
Informed consent
No patients were contacted. Therefore, no informed consent was required from the patients.
Footnotes
This article is part of the Topical Collection on Brain trauma
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Blomberg SNF, Rosenkrantz OCM, Lippert F, Christensen HC. Injury from electric scooters in Copenhagen: a retrospective cohort study. BMJ open. 2019;9:e033988. doi: 10.1136/bmjopen-2019-033988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brownson AB, Fagan PV, Dickson S, Civil ID. Electric scooter injuries at Auckland City Hospital. NZ Med J. 2019;132:62–72. [PubMed] [Google Scholar]
- 3.Cicchino JB, Kulie PE, McCarthy ML. Injuries related to electric scooter and bicycle use in a Washington, DC, emergency department. Traffic Inj Prev. 2021;22:401–406. doi: 10.1080/15389588.2021.1913280. [DOI] [PubMed] [Google Scholar]
- 4.Coronado VG, Xu L, Basavaraju S v, et al. Surveillance for traumatic brain injury-related deaths; United States, 1997–2007 [PubMed]
- 5.Doser K, Poulsen I, Wuensch A, Norup A. Psychological outcome after severe traumatic brain injury in adolescents and young adults: The chronic phase. Brain Inj. 2018;32:64–71. doi: 10.1080/02699052.2017.1363408. [DOI] [PubMed] [Google Scholar]
- 6.Eurostat. Revision of the European Standard Population-Report of Eurostat’s task force
- 7.Farley KX, Aizpuru M, Wilson JM, et al. Estimated incidence of electric scooter injuries in the US from 2014 to 2019. JAMA Netw Open. 2020;3:e2014500–e2014500. doi: 10.1001/jamanetworkopen.2020.14500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ishmael CR, Hsiue PP, Zoller SD, et al. An early look at operative orthopaedic injuries associated with electric scooter accidents: bringing high-energy trauma to a wider audience. JBJS. 2020;102:e18. doi: 10.2106/JBJS.19.00390. [DOI] [PubMed] [Google Scholar]
- 9.Kappagantu A, Yaremchuk K, Tam S. Head and neck injuries and electronic scooter use in the United States. The Laryngoscope [DOI] [PubMed]
- 10.Kleinertz H, Ntalos D, Hennes F, et al. Accident Mechanisms and Injury Patterns in E-Scooter Users: A Retrospective Analysis and Comparison with Cyclists. Dtsch Arztebl Int. 2021;118:117. doi: 10.3238/arztebl.m2021.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kosola S, Salminen P, Laine T. Heading for a fall—moped and scooter accidents from 2002 to 2007. Scand J Surg. 2009;98:175–179. doi: 10.1177/145749690909800309. [DOI] [PubMed] [Google Scholar]
- 12.Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. The Lancet Neurol. 2008;7:728–741. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 13.Madan AK, Yu K, Beech DJ. Alcohol and drug use in victims of life-threatening trauma. J Trauma Acute Care Surg. 1999;47:568–571. doi: 10.1097/00005373-199909000-00026. [DOI] [PubMed] [Google Scholar]
- 14.Majdan M, Plancikova D, Brazinova A, et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. The Lancet Public Health. 2016;1:e76–e83. doi: 10.1016/S2468-2667(16)30017-2. [DOI] [PubMed] [Google Scholar]
- 15.Mayhew LJ, Bergin C. Impact of e-scooter injuries on emergency department imaging. J Med Imaging Radiat Oncol. 2019;63:461–466. doi: 10.1111/1754-9485.12889. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell G, Tsao H, Randell T, et al. Impact of electric scooters to a tertiary emergency department: 8-week review after implementation of a scooter share scheme. Emerg Med Australas. 2019;31:930–934. doi: 10.1111/1742-6723.13356. [DOI] [PubMed] [Google Scholar]
- 17.Moftakhar T, Wanzel M, Vojcsik A, et al. Incidence and severity of electric scooter related injuries after introduction of an urban rental programme in Vienna: a retrospective multicentre study. Arch Orthop Trauma Surg. 2021;141:1207–1213. doi: 10.1007/s00402-020-03589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Namiri NK, Lui H, Tangney T, et al. Electric scooter injuries and hospital admissions in the United States, 2014–2018. JAMA Surg. 2020;155:357–359. doi: 10.1001/jamasurg.2019.5423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Official Statistics of Finland (OSF): Population structure. https://pxnet2.stat.fi/PXWeb/pxweb/en/StatFin/
- 20.Oksanen E, Turunen A, Thorén H. Assessment of Craniomaxillofacial injuries after electric scooter accidents in Turku, Finland, in 2019. J Oral Maxillofac Surg. 2020;78:2273–2278. doi: 10.1016/j.joms.2020.05.038. [DOI] [PubMed] [Google Scholar]
- 21.Olivier J, Creighton P. Bicycle injuries and helmet use: a systematic review and meta-analysis. Int J Epidemiol. 2017;46:278–292. doi: 10.1093/ije/dyw153. [DOI] [PubMed] [Google Scholar]
- 22.Puzio TJ, Murphy PB, Gazzetta J, et al. The electric scooter: a surging new mode of transportation that comes with risk to riders. Traffic Inj Prev. 2020;21:175–178. doi: 10.1080/15389588.2019.1709176. [DOI] [PubMed] [Google Scholar]
- 23.Schlaff CD, Sack KD, Elliott R-J, Rosner MK. Early experience with electric scooter injuries requiring neurosurgical evaluation in District of Columbia: a case series. World Neurosurg. 2019;132:202–207. doi: 10.1016/j.wneu.2019.08.237. [DOI] [PubMed] [Google Scholar]
- 24.Shichman I, Shaked O, Factor S, et al. Epidemiology of fractures sustained during electric scooter accidents: a retrospective review of 563 cases. JBJS. 2021;103:1125–1131. doi: 10.2106/JBJS.20.01746. [DOI] [PubMed] [Google Scholar]
- 25.Shiffler K, Mancini K, Wilson M, et al. Intoxication is a significant risk factor for severe Craniomaxillofacial injuries in standing electric scooter accidents. J Oral Maxillofac Surg. 2021;79:1084–1090. doi: 10.1016/j.joms.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Störmann P, Klug A, Nau C, et al. Characteristics and injury patterns in electric-scooter related accidents—a prospective two-center report from Germany. J Clin Med. 2020;9:1569. doi: 10.3390/jcm9051569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tagliaferri F, Compagnone C, Korsic M, et al. A systematic review of brain injury epidemiology in Europe. Acta Neurochir. 2006;148:255–268. doi: 10.1007/s00701-005-0651-y. [DOI] [PubMed] [Google Scholar]
- 28.Tenovuo O, Diaz-Arrastia R, Goldstein LE, et al. Assessing the severity of traumatic brain injury—time for a change? J Clin Med. 2021;10:148. doi: 10.3390/jcm10010148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tischler EH, Tsai SHL, Wolfert AJ, et al. Orthopedic fracture hospitalizations are revving up from E-Scooter related injuries. Journal of Clinical Orthopaedics and Trauma 2021; 101607 [DOI] [PMC free article] [PubMed]
- 30.Toofany M, Mohsenian S, Shum LK, et al. Injury patterns and circumstances associated with electric scooter collisions: a scoping review. Injury prevention [DOI] [PMC free article] [PubMed]
- 31.Trivedi TK, Liu C, Antonio ALM, et al. Injuries associated with standing electric scooter use. JAMA Netw Open. 2019;2:e187381–e187381. doi: 10.1001/jamanetworkopen.2018.7381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uluk D, Lindner T, Dahne M, et al. E-scooter incidents in Berlin: an evaluation of risk factors and injury patterns. Emergency medicine journal [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.