Abstract
Background
During the Coronavirus disease 2019 (COVID-19) pandemic, reports have emerged of a multisystem inflammatory syndrome in adults (MIS-A). Multisystem inflammatory syndrome in adults can affect various organ systems, including cardiovascular, gastrointestinal, and neurologic systems without significant respiratory involvement.
Case summary
A previously healthy 43-year-old man presented with fevers and abdominal pain then rapidly deteriorated into cardiogenic shock. His constellation of symptoms along with elevated inflammatory markers in the setting of a recent SARS-CoV-2 infection was consistent with the diagnosis of MIS-A. He also had a comprehensive infectious workup that was unremarkable, ruling out other potential infectious aetiologies for his presentation. He subsequently improved through supportive measures and after administration of intravenous immunoglobulin (IVIG). He later demonstrated recovery of cardiac function and cardiac magnetic resonance imaging (MRI) showed signs consistent with myocarditis.
Discussion
As the COVID-19 pandemic continues to be an ongoing issue, it is important to recognize MIS-A, a rare and potentially deadly clinical syndrome that can lead to profound cardiovascular complications. Non-invasive imaging modalities such as cardiac MRI can play a role in the identification of myocarditis. In addition to supportive management, adjunctive therapies such as IVIG may be efficacious in MIS-A and should be further investigated.
Keywords: COVID-19, SARS-CoV-2, Case report, Multisystem inflammatory syndrome, MIS-A, Myocarditis
Keywords: 6.2 Heart failure with reduced ejection fraction, 6.4 Acute heart failure, 2.3 Cardiac magnetic resonance, 6.5 Cardiomyopathy
Learning points
Multisystem inflammatory syndrome in adults (MIS-A) is a potentially fatal syndrome that can involve various organ systems, including the cardiovascular system, and can be associated with delayed-onset myocarditis.
Cases of MIS-A have been treated with intravenous immunoglobulin, corticosteroids, and IL-6 inhibition, but the efficacy of these treatments remains to be further validated.
Introduction
Several months into the coronavirus disease 2019 (COVID-19) pandemic, cases of a new multisystem inflammatory syndrome in children (MIS-C) were reported, with clinical features including shock, cardiac dysfunction, and elevated inflammatory markers.1 A new multisystem inflammatory syndrome in adults (MIS-A) has also been identified.2 Patients with MIS-A have evidence of a recent COVID-19 illness and present with fevers, elevated inflammatory markers, and various cardiovascular, gastrointestinal, dermatologic, and neurologic manifestations without significant respiratory disease.2–4 We describe a case of a patient with MIS-A who presented with profound cardiac dysfunction likely due to delayed-onset myocarditis.
Timeline
| Pre-admission |
|
| Admission |
|
| Day 2 |
|
| Day 4 |
|
| Day 5 |
|
| Day 6 |
|
| Day 7 |
|
| Day 8 |
|
| Day 11 |
|
| Day 12 |
|
| Day 22 |
|
| 11 days post-discharge |
|
Case presentation
A 43-year-old previously healthy man with mildly symptomatic SARS-CoV-2 infection 7 weeks prior presented with abdominal pain, nausea, and fever to 39.4°C; he was otherwise haemodynamically stable and had an elevated erythrocyte sedimentation rate (ESR) 90 mm/h (0–20 mm/h) and C-reactive protein (CRP) 275.1 mg/L (<1 mg/L). Abdominal computed tomography (CT) scan showed terminal ileitis and ascending colitis. Repeat SARS-CoV-2 polymerase chain reaction (PCR), multiplex stool pathogen panel, viral hepatitis panel, Clostridioides difficile assay, and blood cultures were negative. Given the improvement in pain, he left against medical advice.
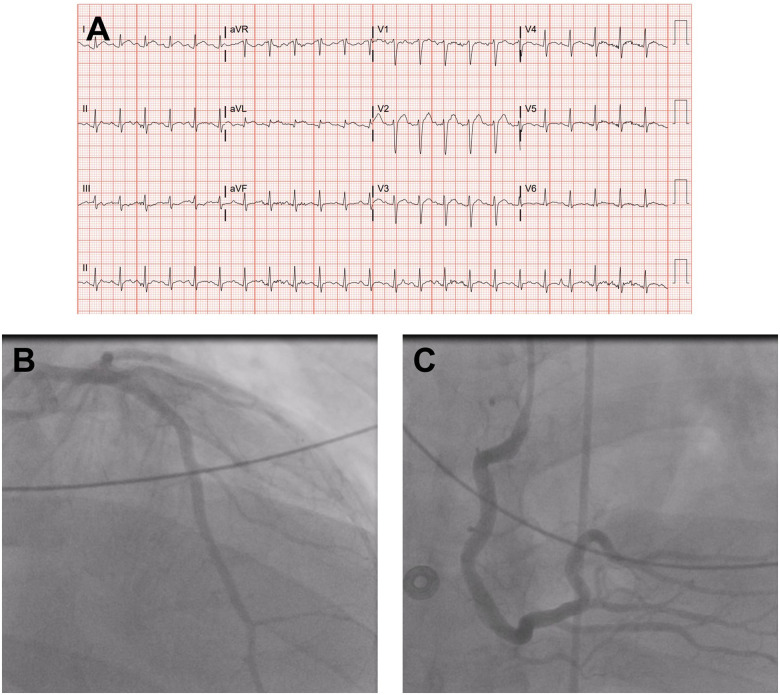
The patient subsequently returned to the emergency department with new-onset dyspnoea and orthopnoea; he was found to be hypotensive to 89/48 mmHg with anterolateral ST-elevations on electrocardiogram (Figure 1A). Chest X-ray showed a small right pleural effusion. Labs were significant for alanine aminotransferase 347 U/L, aspartate aminotransferase 396 U/L, pro B-type natriuretic peptide (proBNP) 16,618 pg/mL (<125 pg/mL), troponin T 0.07 ng/mL (<0.01 ng/mL), CRP >300 mg/L, and ESR 112 mm/h. A limited point-of-care echocardiogram showed global hypokinesis with a grossly reduced left ventricular ejection fraction (LVEF). Aspirin 324 mg was administered and he underwent left heart catheterization (LHC) which showed non-obstructive coronaries (Figure 1B,C, Video 1). During LHC, he was intubated for rapidly worsening hypoxia and work of breathing; haemodynamic instability prompted the initiation of a norepinephrine infusion and placement of an intra-aortic balloon pump (IABP). A Swan-Ganz catheter displayed elevated biventricular pressures with mean right atrial pressure 15–20 mmHg, right ventricular pressure 40/20 mmHg, pulmonary artery pressure 40/28 mmHg (mean 32 mmHg), mean pulmonary capillary wedge pressure 25–28 mmHg. A post-procedural transthoracic echocardiogram (TTE) confirmed global hypokinesis and a severely depressed LVEF 20-25% (Video 2). He later became febrile to 40.3°C requiring active external cooling and broadening of antibiotics. Labs displayed a rising white blood cell (WBC) count of 14.5 × 1000/µL, creatinine 1.95 mg/dL (prior 1.01 mg/dL) accompanied by oligoanuria despite diuretics, and arterial blood gas with mixed metabolic and respiratory acidoses with pH 7.21, pCO2 53 mmHg, pO2 83 mmHg on 60% fraction of inspired oxygen. Given suspicion for myocarditis, tests for adenovirus, parainfluenza viruses 1–4, rhinovirus, influenza A & B, human metapneumovirus, respiratory syncytial virus A & B, coxsackie B, and enterovirus were sent—all ultimately unremarkable. As vasopressor requirements increased, the decision was made to transfer the patient to our institution for consideration of advanced mechanical support and possible heart transplant evaluation.
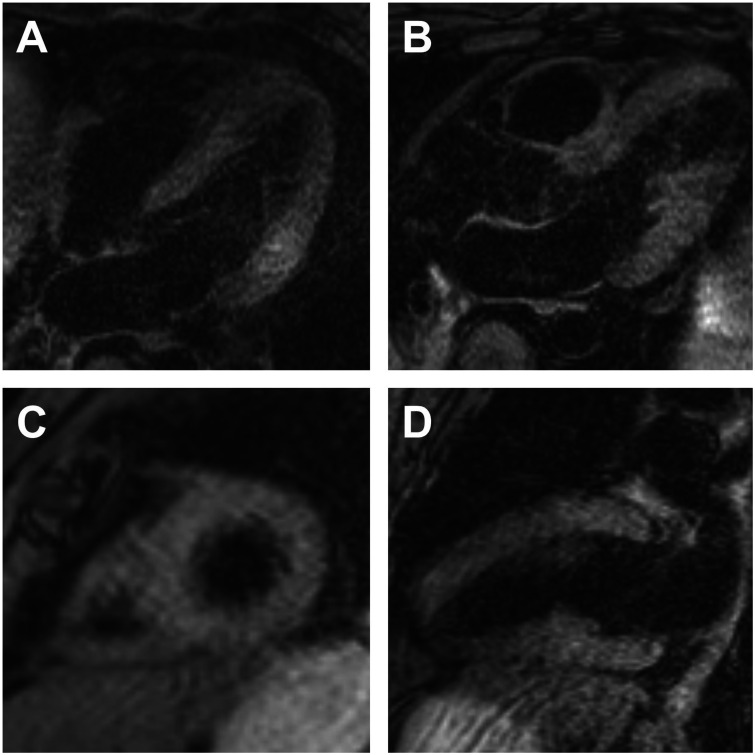
Figure 1.
(A) Electrocardiogram; left heart catheterization showing non-obstructive (B) left anterior descending artery and (C) right coronary artery.
Upon arrival at our cardiac intensive care unit, he was started on a dopamine infusion and was given a diuretic challenge which did not yield any urine output. Labs were notable for worsening creatinine 3.08 mg/dL, proBNP >70 000 pg/mL, ferritin 4311 ng/mL (30–400 ng/mL), WBC 18.0 × 1000/µL, D-dimer 2.74 mg/L FEU (≤0.5 mg/L FEU). C-reactive protein and ferritin levels were trended throughout his course (Figure 2), and the cytokine panel showed elevated soluble IL-2 receptor (sIL-2R), IL-6, IL8, and TNF-α (Table 1). HIV antibody and toxoplasma gondii IgG were negative. Given persistent hypoxaemia and anuric renal failure, continuous veno-venous haemofiltration was initiated with improvements in oxygenation and haemodynamics. IABP was removed on hospital Day 4 and TTE showed recovered LVEF 68% (Video 3). Despite haemodynamic improvement and defervescence, leucocytosis progressed with absolute neutrophilia and lymphopenia. Infectious disease was consulted, and repeat infectious workup, including tracheal aspirate SARS-CoV-2 PCR, was unrevealing; CT abdomen was unchanged and CT chest displayed bilateral infiltrates, but these were not felt to represent infectious processes. Given the constellation of rapid deterioration with profound cardiac dysfunction, gastrointestinal symptoms with signs of enteritis, increased inflammatory markers with absolute neutrophilia and lymphopenia, all in the context of a recent SARS-CoV-2 infection, his presentation was consistent with MIS-A. A joint decision was made to halt antibiotics and proceed with a single dose of 1 mg/kg intravenous immunoglobulin (IVIG) on hospital Day 5. Dopamine and norepinephrine were weaned off by Day 6, and he was extubated on Day 7. He was subsequently transitioned to intermittent haemodialysis (HD) on Day 8. Cardiac magnetic resonance imaging (MRI) on Day 11 showed diffuse myocardial oedema without delayed myocardial enhancement, findings compatible with non-ischaemic cardiomyopathy including myocarditis (Figure 3). Since the patient recovered through supportive therapies alone, an endomyocardial biopsy was deferred. He was transferred to the floor on Day 12 and discharged on Day 22 on intermittent HD. During a follow-up visit 11 days post-discharge, he reported continued weakness and shortness of breath but was gradually recovering.
Figure 2.
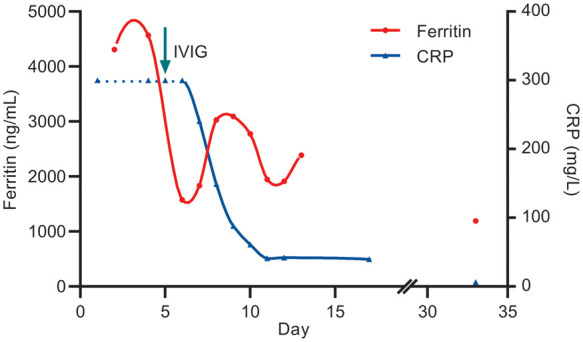
Trend of C-reactive protein and ferritin.
Table 1.
Cytokine panel
| Cytokine | pg/mL (reference range) |
|---|---|
| IL-1β | <1.0 (0.0–1.0) |
| IL-10 | 4.2 (0.0–5.0) |
| IL-2 | <1.0 (0.0–1.0) |
| sIL-2R | 21 489.0 (435.0–2347.0) |
| IFN-γ | 1.2 (0.0–4.0) |
| TNF-α | 40.3 (0.0–13.0) |
| IL-8 | 24.0 (0.0–14.0) |
| IL-6 | 48.4 (<5.0) |
Figure 3.
Cardiac magnetic resonance imaging, T2-weighted sequence (A) four-chamber view; (B) left ventricular outflow tract view; (C) short-axis stack view; (D) vertical long-axis view.
Discussion
This case illustrates a characteristic presentation of MIS-A in a young man with a recent SARS-CoV-2 infection who developed profound cardiogenic shock likely due to delayed-onset myocarditis. The Centers for Disease Control and Prevention (CDC) defines MIS-A through 5 criteria: (i) presence of a severe illness requiring hospitalization in adults ≥21 years old; (ii) a positive SARS-CoV-2 test within the last 12 weeks; (iii) severe organ dysfunction (apart from lungs); (iv) elevated inflammatory markers (including CRP, ferritin, D-dimer, IL-6); and (v) absence of severe respiratory disease, all of which our patient satisfied.2 Reported cardiac manifestations from the CDC case series included shock-requiring vasopressors, arrhythmias, elevated troponin levels, and ventricular dysfunction.2 In another case series of seven patients, all had initially decreased ventricular function requiring inotropes or vasopressors and three required IABP support; all had improvements in LVEF on repeat echocardiogram.5 In another case series, common characteristics included high-grade fever, abdominal pain, hypotension—all present in our patient; some also had COVID-19 one month prior, supportive of a delayed manifestation.6 Furthermore, cardiac MRIs consistently demonstrated findings of diffuse myocardial oedema, as was observed in our patient.6 A handful of other cases of COVID-19-associated myocardial dysfunction in adults have been described in the literature, including several cases of delayed-onset myocarditis.7–15 Given that our patient had a prolonged time period from initial diagnosis of COVID-19 to his subsequent admission for cardiogenic shock, as well as the lack of endomyocardial biopsy results, we cannot definitively establish a causal relation between COVID-19 infection and myocarditis. However, our patient did meet the criteria for COVID-19-associated MIS-A and his clinical course was consistent with prior reported cases of COVID-19-associated myocarditis. Furthermore, we had performed a comprehensive workup, which did not reveal an alternate aetiology of myocarditis.
Patients with MIS-A have been treated with a combination of IVIG, corticosteroids, and the IL-6 inhibitor tocilizumab.2,5,7 Our patient received a single dose of IVIG, with a sustained reduction in CRP (Figure 2) along with clinical improvement; however, the efficacy of such therapies remains to be further elucidated. As COVID-19 continues to be globally prevalent, clinicians should consider MIS-A as a diagnosis in similar clinical syndromes.
Lead author biography

Miles Shen is an Internal Medicine resident at Yale New Haven Hospital. He graduated from Princeton University in 2014 with a BA in Molecular Biology then earned his medical degree at Rutgers New Jersey Medical School in 2020. His particular interests lie in cardiovascular diseases and critical care.
Supplementary material
Supplementary material is available at European Heart Journal—Case Reports online.
Slide sets: A fully edited slide set detailing these cases and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for the submission and publication of this case, including images, has been obtained from the patient in line with COPE guidance.
Funding: None declared.
Conflict of interest: None declared.
Supplementary Material
References
- 1.Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al. ; California MIS-C Response Team. COVID-19–associated multisystem inflammatory syndrome in children—United States, March–July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morris SB, Schwartz NG, Patel P, Abbo L, Beauchamps L, Balan S. et al. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 Infection — United Kingdom and United States, March–August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1450–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP. et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med 2020;382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J. et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chau VQ, Giustino G, Mahmood K, Oliveros E, Neibart E, Oloomi M. et al. Cardiogenic shock and hyperinflammatory syndrome in young males with COVID-19. Circ: Heart Failure 2020;13: [DOI] [PubMed] [Google Scholar]
- 6.Hékimian G, Kerneis M, Zeitouni M, Cohen-Aubart F, Chommeloux J, Bréchot N. et al. Coronavirus disease 2019 acute myocarditis and multisystem inflammatory syndrome in adult intensive and cardiac care units. Chest 2021;159:657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veyseh M, Webster P, Blanco I.. COVID-19-associated inflammatory syndrome in an adult woman with unexplained multiple organ failure: staying vigilant for COVID-19 complications as the pandemic surges. BMJ Case Rep 2021;14:e242034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newton-Cheh C, Zlotoff DA, Hung J, Rupasov A, Crowley JC, Funamoto M.. Case 24-2020: a 44-year-old woman with chest pain, dyspnea, and shock. N Engl J Med 2020;383:475–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaigany S, Gnirke M, Guttmann A, Chong H, Meehan S, Raabe V. et al. An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19. The Lancet 2020;396:e8–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vujaklija Brajković A, Zlopaša O, Gubarev Vrdoljak N, Goran T, Lovrić D, Radonić R.. Acute liver and cardiac failure in multisystem inflammatory syndrome in adults after COVID-19. Clin Res Hepatol Gastroenterol 2021;45:101678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamada Y, Fujinami K, Eguchi T, Takefuji H, Mori N.. Multisystem inflammatory syndrome in adults after Mild SARS-CoV-2 infection, Japan. Emerg Infect Dis 2021;27:1740–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tung-Chen Y, Algora-Martín A, Rodríguez-Roca S, Díaz de Santiago A.. COVID-19 multisystemic inflammatory syndrome in adults: a not to be missed diagnosis. BMJ Case Rep 2021;14:e241696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mieczkowska K, Zhu TH, Hoffman L, Blasiak RC, Shulman KJ, Birnbaum M. et al. Two adult cases of multisystem inflammatory syndrome associated with SARS-CoV-2. JAAD Case Rep 2021;10:113–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bajaj R, Sinclair HC, Patel K, Low B, Pericao A, Manisty C. et al. Delayed-onset myocarditis following COVID-19. Lancet Respir Med 2021;9:e32–e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gulersen M, Staszewski C, Grayver E, Tam Tam H, Gottesman E, Isseroff D. et al. Coronavirus disease 2019 (COVID-19)-related multisystem inflammatory syndrome in a pregnant woman. Obstet Gynecol 2021;137:418–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.