Abstract
Pleural effusion can rarely present as an initial manifestation of Ewing sarcoma. We illustrate a case of a young male adult who was admitted with pleural effusion that led to the diagnosis of Ewing sarcoma.
Keywords: pathology, pulmonology, bone tumors, pleural fluid (pf), ewing sarcoma (es)
Introduction
Ewing sarcoma is a malignant tumor that can arise in bones or soft tissues [1]. Despite its rarity, the Ewing sarcoma family of tumors (EFTs) are the second most common primary bone malignancy among children and adolescents [2]. They mostly affect Caucasians for unknown causes and are extremely uncommon among the African American population [3]. Usually, Ewing sarcoma arises in the long bone of the extremities and the bones of the pelvis. The spine, hands, and feet are affected much less frequently [4]. The most common symptoms are local pain and swelling in the affected area and fever, and pathological fractures may also be seen [5]. We report a case of an unusual presentation of Ewing sarcoma in a young adult who had localized chest pain and pleural effusion.
Case presentation
A previously healthy 22-year-old Indian male presented to the emergency department with a two-week history of right-sided chest and upper abdominal pain, along with intermittent fever. He denied any other related symptoms. The patient works as a driver and has no family history of malignancy. Physical examination revealed decreased chest sounds on the right lower zone. Diffuse rales and rhonchi were also noted mainly on the right lung field. The remainder of the examination was completely normal.
The laboratory tests were within normal limits, except for mild leukocytosis and increased C-reactive protein (Table 1). Chest X-ray revealed right-sided pleural effusion (Figure 1). The patient was admitted as a case of community-acquired pneumonia and started on intravenous antibiotics (amoxicillin/clavulanate, 1000 mg/200 mg). Diagnostic thoracentesis only was done, and it demonstrated hemorrhagic exudative pleural effusion (Table 1). Pleural fluid microscopic examination was negative for malignancy; it showed clusters of reactive mesothelial cells in a background of numerous inflammatory cells, mainly neutrophil polymorph. The abdominal ultrasonography revealed mild to moderate right-sided pleural effusion and a large solid mass along the right lower chest wall with possible downward extension toward the abdominal wall.
Table 1. Laboratory test values.
| Detail | Value | Normal range |
| Blood test results | ||
| White cell count | 11.7 × 103/uL | 4–10 × 103/uL |
| Hemoglobin | 14.8 g/dL | 13–17 g/dL |
| Creatinine | 61 umol/L | 62–106 umol/L |
| NT-proBNP | 42 pg/mL | Less than 125 pg/mL |
| C-reactive protein | 182.5 mg/L | 0–5 mg/L |
| Lactate dehydrogenase | Hemolyzed | 135–225 U/L |
| Albumin | 34 g/L | 35–52 g/L |
| Glucose random | 6.2 mmol/L | 3.9–5.5 mmol/L |
| QuantiFERON-TB Gold Plus | Negative | |
| Pleural effusion | ||
| Appearance | Bloody | |
| Red cell count | 104,875/uL | |
| White cell count | 8,250/uL | |
| Neutrophils | 51% | |
| Lymphocytes | 38% | |
| Monocytes | 8% | |
| Glucose | 4.5 mmol/L | |
| Lactate dehydrogenase | 148.8 U/L | |
| pH | 7.55 | |
| Protein | 47.5 g/L | |
| Albumin | 27.5 g/L | |
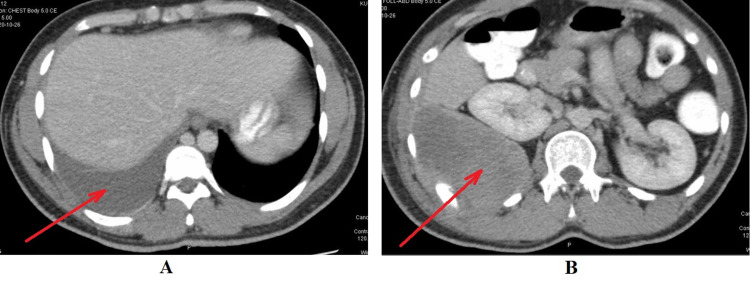
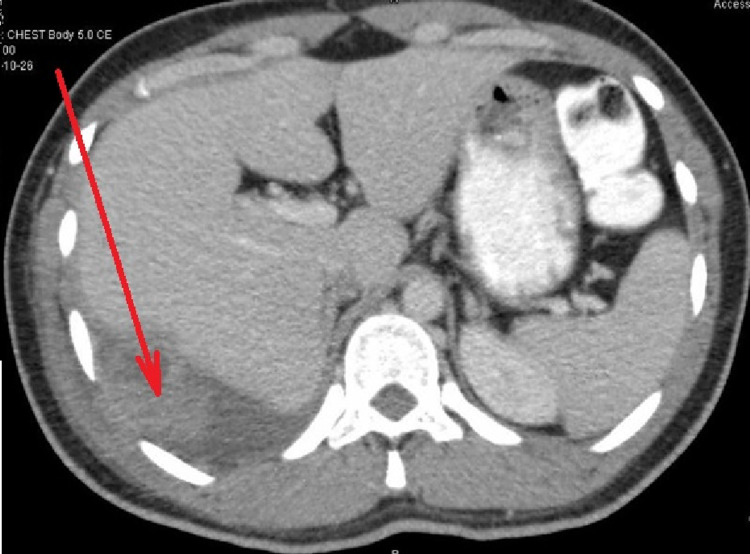
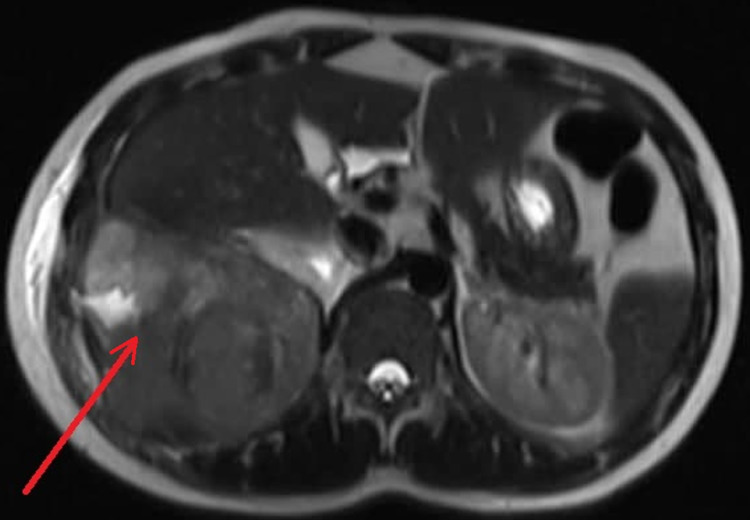
CT scan revealed an uncalcified solid heterogeneous soft tissue density lesion along the right lower posterolateral chest wall (Figure 2). The soft tissue component is predominantly bulging medially into the lower hemithorax/upper extraperitoneal abdomen. The lesion is seemingly invading the lower posterolateral pleura (Figure 3). MRI of the abdomen and pelvis showed a heterogeneous mass lesion in relation to the right lower posterolateral chest wall, which was suggestive of a soft tissue malignant lesion (Figure 4).
Figure 1. Chest X-ray shows right-sided pleural effusion with the possibility of mass lesion along the right lower hemithorax.
Figure 2. CT scan of the chest, abdomen, and pelvis. A: Mild to moderate right-sided pleural effusion (red arrow). B: Solid heterogeneous soft tissue density lesion (red arrow) along the right lower posterolateral chest wall.
Figure 3. CT scan of the chest, abdomen, and pelvis. It shows that the lesion is seemingly invading the lower posterolateral pleura (red arrow).
Figure 4. MRI of the abdomen in T2 shows a predominantly solid heterogeneous mass lesion (red arrow) noted in relation to the right lower posterolateral chest wall above and below the diaphragm with hyperintense areas that are suggestive of cystic changes toward the peripheral part.
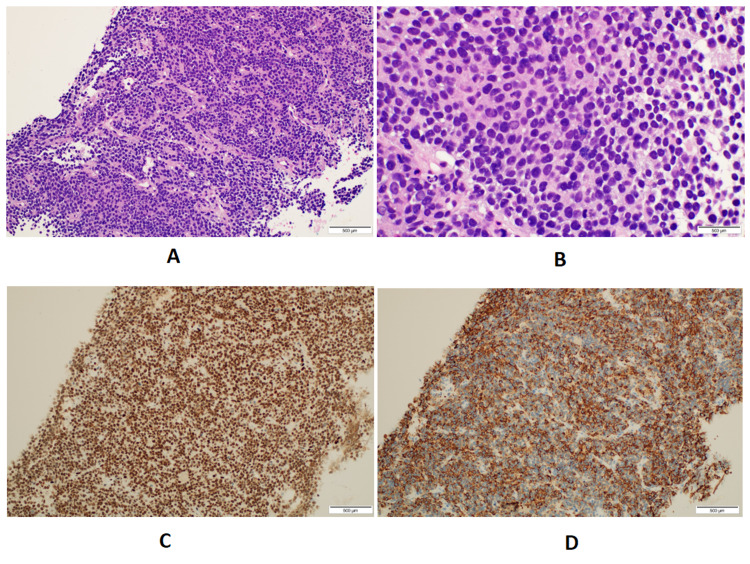
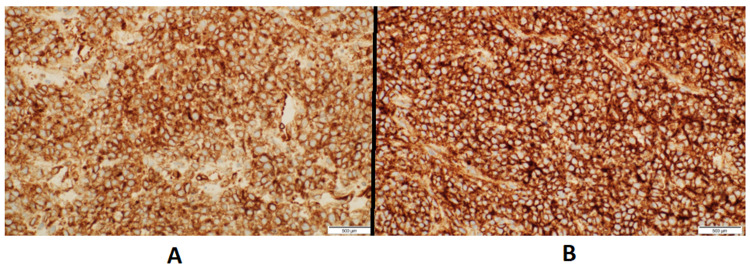
The suspected mass biopsy results revealed tumoral proliferation formed of undifferentiated small round uniform cells arranged into irregular sheets separated by fibrous bands. The tumor cells have scant clear cytoplasm with indistinct cell borders and hyperchromatic nuclei with inapparent nucleoli. The pathology findings indicated a malignant small round cell tumor, which is compatible with Ewing sarcoma (Figures 3, 4). The plan was to start chemotherapy, but the patient traveled back to have the treatment in his home country.
Figure 5. Pathological findings of the mass biopsy: A: Sheets of the densely cellular undifferentiated tumor with stromal fibrous strands (H&E: ×20). B: Sheets of small, round, uniform cells with scant clear cytoplasm and indistinct cell membranes with occasional mitosis. C: Immunohistochemical stain for FLI-1 shows diffuse and strong nuclear staining of the tumor cells (H&E: ×20). D: Immunohistochemical stain for CKAE1/3 shows diffuse and strong cytoplasmic staining of the tumor cells (H&E: ×20).
Figure 6. Pathological findings of the mass biopsy: A: Immunohistochemical stain for BCL-2 shows diffuse and strong membranous staining of the tumor cells (H&E: ×40). B: Immunohistochemical stain for CD99 shows diffuse and strong membranous staining of the tumor cells (H&E: ×40).
Discussion
Extraskeletal Ewing sarcoma is well known among adolescents, which usually presents with localized mass [6]. Pleural effusion is a quite rare presentation of Ewing sarcoma and can be easily missed especially in patients who are from endemic areas of tuberculosis, which is usually one of the main causes of exudative pleural effusion [7]. This advocates the importance of considering Ewing sarcoma in the cases of bloody pleural effusion in young adult patients. Histopathological examination of any hemorrhagic pleural fluid is crucially important in such cases to avoid the catastrophic overlook of malignancy [8]. In our case, although the pleural fluid was negative for malignant cells, it was eventually found to have resulted from the malignant mass of Ewing sarcoma.
The definition of malignant pleural effusion clearly states that the fluid must contain malignant cells [9]. However, in the presence of a highly suspected mass, a pleural fluid with negative malignant cells is called a para-malignant effusion [10]. Para-malignant pleural effusion can range from concordant exudate to transudate with mediastinal lymphadenopathy as the most common cause [11]. It occurs as a result of multiple mechanisms, including when malignant cells lose adhesion and dislodgement from the primary tumor site, blood vessel wall penetrating/migrating through the pleura, and induction of angiogenesis [12,13]. In our case, Ewing sarcoma was located in the chest wall and caused a para-malignant pleural effusion, which is a very rare behavior and also a rare location to arise from.
Other extremely rare locations of Ewing sarcoma were reported, such as the parotid gland [14], jejunum [15], and stomach [16]. Moreover, Ewing sarcoma was reported to be localized intracranially in a four-year-old boy [17]. Another case of epidural Ewing sarcoma in a 45-year-old woman that caused paresthesia and urinary retention was also reported as one of the rarest presentations of Ewing sarcoma [18].
Although both skeletal and extraskeletal Ewing sarcoma have generally the same treatment approaches, extraskeletal Ewing sarcoma tends to be more aggressive with a higher probability for local recurrence and metastasis [19]. Interestingly, however, overall survival of five years was found to be the same in both types [20]. Our patient refused to commence the chemotherapy regimen and preferred to fly back to his home country; therefore, we could not follow him up and reevaluate his case.
Conclusions
We demonstrate in this case the wide variety of Ewing sarcoma presentations, with more focus on pleural effusion as an interesting and unusual feature, especially in young adult patients. These cases can be overlooked, especially when the fluid is negative for malignant cells, which may delay the diagnosis and result in an awfully bad prognosis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Extraskeletal neoplasm resembling Ewing’s sarcoma. Angervall L, Enzinger FM. Cancer. 1975;36:1–240. doi: 10.1002/1097-0142(197507)36:1<240::aid-cncr2820360127>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 2.Ries LA, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, Bunin GR. Published Online First. Bethesda, USA: National Cancer Institute (NCI); 1999. Cancer incidence and survival among children and adolescents: United States SEER Program 1975-1995. [Google Scholar]
- 3.Ewing sarcoma demonstrates racial disparities in incidence-related and sex-related differences in outcome: an analysis of 1631 cases from the SEER database, 1973-2005. Jawad MU, Cheung MC, Min ES, Schneiderbauer MM, Koniaris LG, Scully SP. Cancer. 2009;115:3526–3536. doi: 10.1002/cncr.24388. [DOI] [PubMed] [Google Scholar]
- 4.Soft tissue Ewing’s sarcoma. Characterization in established cultures and xenografts with evidence of a neuroectodermic phenotype. Llombart-Bosch A, Carda C, Peydro-Olaya A, Noguera R, Perez-Bacete M, Pellin A, Boix J. Cancer. 1990;66:2589–2601. doi: 10.1002/1097-0142(19901215)66:12<2589::aid-cncr2820661223>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 5.Extraosseous Ewing’s sarcoma. A study of 42 cases. Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA. Cancer. 1989;64:1548–1553. doi: 10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 6.Extraskeletal Ewing's sarcoma: a report of 18 cases and literature review. Xie CF, Liu MZ, Xi M. Chin J Cancer. 2010;29:420–424. doi: 10.5732/cjc.009.10402. [DOI] [PubMed] [Google Scholar]
- 7.Tuberculous pleural effusion. Zhai K, Lu Y, Shi HZ. J Thorac Dis. 2016;8:0–94. doi: 10.21037/jtd.2016.05.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ewing's sarcoma presenting as pleural effusion. Kushwaha RA, Sainalabdeen S, Anand S, Husain N. Oman Med J. 2011;26:362–364. doi: 10.5001/omj.2011.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Management of malignant pleural effusion. Kastelik JA. Lung. 2013;191:165–175. doi: 10.1007/s00408-012-9445-1. [DOI] [PubMed] [Google Scholar]
- 10.Advanced malignant lung disease: what the specialist can offer. Gompelmann D, Eberhardt R, Herth FJ. Respiration. 2011;82:111–123. doi: 10.1159/000329703. [DOI] [PubMed] [Google Scholar]
- 11.Pleural fluid characteristics of paramalignant effusion. Gurung P, Goldblatt MR, Huggins JT, Doelken P, Sahn SA. Chest. 2009;136:44. [Google Scholar]
- 12.Pathogenesis of malignant pleural effusions and talc pleurodesis. Antony VB. Pneumologie. 1999;53:493–498. doi: 10.1055/s-1999-9040. [DOI] [PubMed] [Google Scholar]
- 13.Pathophysiology of the pleura. Jantz MA, Antony VB. Respiration. 2008;75:121–133. doi: 10.1159/000113629. [DOI] [PubMed] [Google Scholar]
- 14.Primary extraskeletal Ewing sarcoma of the parotid gland. Gulsen S, Vicdan H. Ear Nose Throat J. 2021;100:147–149. doi: 10.1177/0145561319876922. [DOI] [PubMed] [Google Scholar]
- 15.Extraskeletal Ewing sarcoma of the jejunum: a case report. Cantu C, Bressler E, Dermawan J, Paral K. Perm J. 2019;23:18–255. doi: 10.7812/TPP/18-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gastrointestinal: multi-modality imaging of extraskeletal Ewing sarcoma of the stomach. Hopp AC, Nguyen BD. J Gastroenterol Hepatol. 2019;34:1273. doi: 10.1111/jgh.14638. [DOI] [PubMed] [Google Scholar]
- 17.Extraskeletal, intradural, non-metastatic Ewing's sarcoma. Case report. Ottóffy G, Komáromy H. Ideggyogy Sz. 2020;73:286–288. doi: 10.18071/isz.73.0268. [DOI] [PubMed] [Google Scholar]
- 18.[Epidural extraskeletal Ewing sarcoma. Case report and literature review]. [Article in Spanish] García-Moreno R, Bernal-García LM, Pineda-Palomo M, Botana-Fernández M, Gilete-Tejero IJ, Cabezudo-Artero JM. Neurocirugia (Astur) 2015;26:151–156. doi: 10.1016/j.neucir.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Extraskeletal Ewing's sarcoma family of tumors in adults: prognostic factors and clinical outcome. Tural D, Molinas Mandel N, Dervisoglu S, et al. Jpn J Clin Oncol. 2012;42:420–426. doi: 10.1093/jjco/hys027. [DOI] [PubMed] [Google Scholar]
- 20.Outcomes of extraskeletal vs. skeletal Ewing sarcoma patients treated with standard chemotherapy protocol. Salah S, Abuhijla F, Ismail T, et al. Clin Transl Oncol. 2020;22:878–883. doi: 10.1007/s12094-019-02202-y. [DOI] [PubMed] [Google Scholar]