Abstract
Purpose
As a further step to elucidate the actual diverse spectrum of oncofertility practices for breast cancer around the globe, we present and discuss the comparisons of oncofertility practices for breast cancer in limited versus optimum resource settings based on data collected in the Repro-Can-OPEN Study Part I & II.
Methods
We surveyed 39 oncofertility centers including 14 in limited resource settings from Africa, Asia & Latin America (Repro-Can-OPEN Study Part I), and 25 in optimum resource settings from the United States, Europe, Australia and Japan (Repro-Can-OPEN Study Part II). Survey questions covered the availability of fertility preservation and restoration options offered to young female patients with breast cancer as well as the degree of utilization.
Results
In the Repro-Can-OPEN Study Part I & II, responses for breast cancer and calculated oncofertility scores showed the following characteristics: (1) higher oncofertility scores in optimum resource settings than in limited resource settings especially for established options, (2) frequent utilization of egg freezing, embryo freezing, ovarian tissue freezing, GnRH analogs, and fractionation of chemo- and radiotherapy, (3) promising utilization of oocyte in vitro maturation (IVM), (4) rare utilization of neoadjuvant cytoprotective pharmacotherapy, artificial ovary, and stem cells reproductive technology as they are still in preclinical or early clinical research settings, (5) recognition that technical and ethical concerns should be considered when offering advanced and innovative oncofertility options.
Conclusions
We presented a plausible oncofertility best practice model to guide oncofertility teams in optimizing care for breast cancer patients in various resource settings.
Keywords: Oncofertility, Breast cancer, Fertility preservation, Best practice, Limited resource settings, Optimum resource settings
Introduction
Breast cancer is the most common cancer impacting women of reproductive age [1]. Contemporary breast cancer treatment often requires aggressive gonadotoxic therapies that necessitates fertility preservation treatments for those who desire future fertility. Young women with breast cancer have a higher risk of carrying pathologic mutations in the BRCA1 or BRCA2 genes, adding further complexity to their oncofertility counseling [2]. According to the most recent international guidelines from the American Society of Clinical Oncology (ASCO) [3], the American Society for Reproductive Medicine (ASRM) [4], the European Society of Human Reproduction and Embryology (ESHRE) [5] and the European Society for Medical Oncology (ESMO) [6], several established, debatable, and experimental oncofertility options can be offered to young female patients with breast cancer to preserve and restore fertility. Established oncofertility options include embryo cryopreservation, oocyte cryopreservation, and recently ovarian tissue cryopreservation and autotransplantation. Debatable options for fertility preservation for breast cancer patients include GnRH analogs and hormonal suppression, fractionation of chemotherapy and radiotherapy. Experimental oncofertility options include oocyte in vitro maturation (IVM), artificial ovary, neoadjuvant cytoprotective pharmacotherapy, stem cell reproductive technology and others [3–6].
Despite recognition as official recommendations, oncofertility international guidelines face several challenges in practice. Over the past years, the Oncofertility Consortium has studied oncofertility practices in many countries within its Oncofertility Professional Engagement Network (OPEN) [7, 8]. Our previous studies identified a variety of standards and challenges in oncofertility practices worldwide [9–13]. Recently in our Repro-Can-OPEN Study Part I & II, we proposed installation of specific oncofertility programs for childhood, breast, and blood cancers in limited versus optimum resource settings. The main objectives of Repro-Can-OPEN Study Part I & II were to measure empirically the availability and degree of utilization of oncofertility options provided by the surveyed centers, to identify different styles of oncofertility practice for common cancers in limited and optimum resource settings, and to suggest best practice models for oncofertility care based on the results of the survey and the existing literature [14, 15].
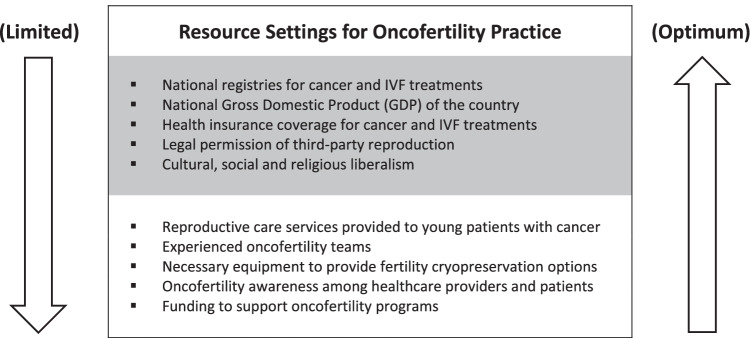
Limited resource settings include the following criteria especially in low- and middle-income countries (Fig. 1): shortage of reproductive care services provided to young patients with cancer, lack of experienced oncofertility teams and necessary equipment, lack of national registries for in vitro fertilization (IVF) and/or cancer treatments, lack of awareness among providers and patients, cultural and religious constraints, partial or complete legal prohibition of third-party reproduction, lack of insurance coverage for IVF and/or cancer treatments resulting in high out-of-pocket costs for patients, and lack of funding to support oncofertility programs. Even in developed countries, a state of limited resource settings could be experienced where access is limited or in case of sudden national disasters when most of public services including healthcare are negatively affected as occurred recently during COVID-19 pandemic and its related economic shutdown. Additionally, within developed countries there may be specific regions that may qualify as limited resource [14].
Fig. 1.
Limited versus optimum resource settings affecting oncofertility practice on national (grey) and local (white) levels
Optimum resource settings include the following criteria especially in high-income countries (Fig. 1): availability of reproductive care services provided to young patients with cancer, availability of experienced oncofertility teams and necessary equipment, presence of national registries for IVF and cancer treatments, awareness among providers and patients, minimal cultural or religious constraints, legally allowed third-party reproduction, insurance coverage for IVF and cancer treatments, and availability of funding to support oncofertility programs [15].
As a further step to reflect the actual diverse spectrum of oncofertility practices for breast cancer around the globe and to help provide a plausible oncofertility best practice model, this study sought to compare oncofertility practices for breast cancer in limited versus optimum resource settings according to data reported in the Repro-Can-OPEN Study Part I & II.
Methods
The Oncofertility Consortium sent the Repro-Can-OPEN Study questionnaire via email to 39 oncofertility centers in total; 14 oncofertility centers with limited resource settings from Africa, Asia & Latin America in Repro-Can-OPEN Study Part I, and 25 oncofertility centers with optimum resource settings from the United States, Europe, Australia and Japan in Repro-Can-OPEN Study Part II (Table 1). The Repro-Can-OPEN Study questionnaire included questions on the availability of fertility preservation options provided to young female patients with breast cancer in their reproductive years (age < 40 yr.), and whether these options are always, commonly, occasionally or rarely used. Responses from oncofertility medical teams from surveyed centers were collected, reviewed, and analyzed.
Table 1.
The 39 Surveyed Oncofertility Centers in Repro-Can-OPEN Study Part I & II
| Surveyed Oncofertility Centers with Limited Resource Settings (Repro-Can-OPEN Study Part I): (n = 14) | |
|---|---|
| 1 | National Research Center, Cairo, Egypt |
| 2 |
Aziza Othmana Hospital of Tunis, Tunisia FERTILLA, Clinique la Rose, Tunis, Tunisia |
| 3 | Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil |
| 4 |
Laboratorio de Biología Reproductiva y Preservación de la Fertilidad, Laboratorios de Investigación y Desarrollo, Universidad Peruana Cayetano Heredia, Lima, Peru Unidad de Oncología Pediátrica, Hospital Edgardo Rebagliati Martins, Lima, Peru |
| 5 | Panama Fertility, Sistema Nacional de Investigadores, Panama City, Panama |
| 6 |
Pregna Medicina Reproductiva, Buenos Aires, Argentina Hospital de Niños Ricardo Gutierrez, Buenos Aires, Argentina Procrearte, Buenos Aires, Argentina Hospital de Niños Victor J. Vilela. Rosario, Santa Fe, Argentina |
| 7 | Centro de Reproduccion Humana, Facultad de Medicina, Universidad de Valparaiso, Valparaiso, Chile |
| 8 | Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico |
| 9 |
Fertility Preservation Centre, Department of Clinical Embryology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India Department of Medical Oncology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India Mother and Child Hospital, New Delhi, India Dr. Patil's Fertility and Endoscopy Clinic, Bangalore, India Hospital Institute of Medical Sciences & SRCC children’s Hospital, Mumbai, India |
| 10 |
Vitalab Fertility Centre, Johannesburg, South Africa Department Medical Oncology, University of Witwatersrand, Johannesburg, South Africa Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa |
| 11 |
Instituto Nacional de Cancerología, Bogota, Colombia FERTIVIDA Fertility Center, Bogota, Colombia |
| 12 | Instituto Guatemalteco de Seguridad Social (IGSS), Guatemala City, Guatemala |
| 13 | Thuriah Medical Center, Riyadh, Kingdom of Saudi Arabia |
| 14 |
The Oncology and Fertility Centres of Ekocorp Plc, Eko Hospitals, Lagos, Nigeria Kingswill Specialist Hospital, Lagos, Nigeria |
| Surveyed Oncofertility Centers with Optimum Resource Settings (Repro-Can-OPEN Study Part II): (n = 25) | |
| 1 |
Oncofertility Consortium, Feinberg School of Medicine, Northwestern University, Chicago, IL 60,611, USA Ann & Robert H. Lurie Children’s Hospital of Chicago, 225 East Chicago Ave, Box 63, Chicago IL, 60,611, USA |
| 2 | Yale Fertility Center and Yale Fertility Preservation program, 200 West Campus Dr., Orange, CT 06,477, USA |
| 3 | Karolinska Institutet, Department of Oncology-Pathology and Karolinska University Hospital, Department of Reproductive Medicine, Division of Gynecology and Reproduction, SE-14186, Stockholm, Sweden |
| 4 | Department of Obstetrics and Gynecology, St. Marianna University School of Medicine, 2–16-1, Sugao, Miyamae-ku, Kawasaki, Kanagawa, Japan |
| 5 |
Department of Medical Oncology, UOC Clinica di Oncologia Medica, IRCCS Ospedale Policlinico San Martino, Genova, Italy Department of Internal Medicine and Medical Specialties (DiMI), School of Medicine, University of Genova, Genova, Italy |
| 6 |
Fertility Preservation Service, Reproductive Services Unit, Royal Women’s Hospital, Parkville, 3051, Australia Fertility Preservation Service, Melbourne IVF, East Melbourne, 3002, Australia |
| 7 | Children’s National Hospital, 111 Michigan Avenue NW, Washington, DC 20,010, USA. (ZIA# HD008985) |
| 8 | Center for Reproductive Medicine, Michigan Medicine, 475 Market Place, Building 1, Suite B, Ann Arbor, MI 48,108, USA |
| 9 | Fertility Research Centre, Royal Hospital for Women, Barker Street, Sydney, Australia |
| 10 | Stanford University Medical Center, 300 Pasteur Drive, Stanford, CA, USA |
| 11 |
University of Edinburgh, Edinburgh, UK Royal Infirmary of Edinburgh and Royal Hospital for Children and Young People, Little France Crescent, Edinburgh, UK |
| 12 | Nationwide Children’s Hospital, 700 Children's Dr., Columbus, OH 43,205, USA |
| 13 | University of Pennsylvania, Division of Reproductive Endocrinology & Infertility, 3701 Market Street, Suite 8000, Philadelphia, PA 19,104, USA |
| 14 | New York University, NYU Langone Fertility Center, 660 First Ave, 5th Floor, New York, NY 10,016, USA |
| 15 | UniKiD—Center for Reproductive Medicine, UniCareD—Center for Fertility Preservation, Düsseldorf University Hospital, Moorenstrasse 5, D-40225 Düsseldorf, Germany |
| 16 | Laboratory of Reproductive Biology, Juliane Marie Centre for Women, Children and Reproduction, University Hospital of Copenhagen, Blegdamsvej 9, DK-2100 Copenhagen, Denmark |
| 17 | Fertility Preservation Service, The Royal Children’s Hospital, Flemington Rd, Parkville, Melbourne, Vic 3054, Australia |
| 18 | University of California, San Diego, 3855 Health Sciences Drive, La Jolla, CA 92,039–0901, USA |
| 19 |
Cliniques Universitaires Saint Luc, Université Catholique de Louvain, Avenue Hippocrate, 10, 1200 Brussels, Belgium Université Catholique de Louvain, Avenue Mounier 52, 1200 Brussels, Belgium |
| 20 | Fertility Clinic and Research Laboratory on Human Reproduction, CUB-Erasme Hospital, Université Libre de Bruxelles (ULB), 808 route de Lennik, 1070 Brussels, Belgium |
| 21 | Centre for Reproductive Medicine of UZ Brussel, Laarbeeklaan 101, 1090 Brussels, Belgium |
| 22 | Gynecological Endocrinology and Reproductive Medicine Division, Obstetrics and Gynecology Department, Cologne University Hospital, Cologne, Germany |
| 23 | Center for Reproduction and Transplantation, Magee-Womens Hospital, University of Pittsburgh Medical Center, 300 Halket Street, Pittsburgh, PA 15,213, USA |
| 24 |
University of Cincinnati, Department of Obstetrics and Gynecology, Division for REI, Cincinnati, OH 45,229, USA Cincinnati Children’s Hospital Medical Center, Division of Pediatric Adolescent Gynecology Pediatric, Cincinnati, OH 45,229, USA |
| 25 |
Urology Department, UCSF Medical Center, University of California, San Francisco, CA 94,143, USA Obstetrics and Gynecology Department, UCSF Medical Center, University of California, San Francisco, CA 94,143, USA |
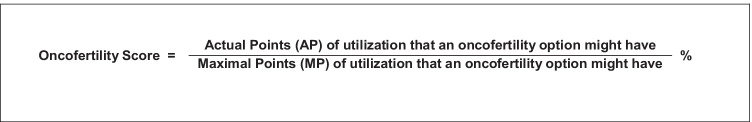
To analyze the collected data, we developed a new scoring system, ‘the oncofertility score’ [14, 15]. As previously described, the oncofertility score is a new diagnostic tool to measure the availability and degree of utilization of oncofertility options for cancer patients in a treating center, country, or group of centers or countries. Although empirical, the oncofertility score could be also used as a prognostic tool to follow up on the development of oncofertility options and strategies provided to cancer patients over time especially in absence of accurate national oncofertility registries. The oncofertility score is calculated as a percentile ratio between the actual and maximal points of utilization that an oncofertility option might have (Table 2 & Fig. 2). When a fertility preservation option is available and always used for cancer patients, it is given (Yes + + + +) that weighs 100 actual points (25 points per each +). When a fertility preservation option is available and commonly used for cancer patients, it is given (Yes + + +) that weighs 75 actual points (25 points per each +). When a fertility preservation option is available but occasionally used for cancer patients, it is given (Yes + +) that weighs 50 actual points (25 points per each +). When a fertility preservation option is available but rarely used or only used in research settings for cancer patients, it is given (Yes +) that weighs 25 actual points (25 points per each +). When a fertility preservation option is not available, it is given (No) that weighs 0 actual points. When the fertility preservation option is not available to cancer patients because it is still in the preclinical research stage, it is marked with (No*). The maximal points of utilization that an oncofertility option might have is 100 when it is available and always used for cancer patients and is given (Yes + + + +), (25 points per each +) [14, 15].
Table 2.
Oncofertility Score calculation
| Availability and utilization of an oncofertility option | Available and always used for cancer patients | Available and commonly used for cancer patients | Available but occasionally used for cancer patients | Available but rarely used or only used in research settings for cancer patients | Not available |
|---|---|---|---|---|---|
| Scale Symbol | + + + + | + + + | + + | + | - |
|
Actual Points (AP) (25 points per +) |
100 | 75 | 50 | 25 | 0 |
|
Maximal Points (MP) (100 points per + + + +) |
100 | 100 | 100 | 100 | 100 |
|
Oncofertility Score = AP/MP (%) |
100% | 75% | 50% | 25% | 0% |
Fig. 2.
Oncofertility Score calculation
In our Repro-Can-OPEN Study Part I & II, the oncofertility score was calculated as a percentile ratio between the total actual points and the total maximal points of utilization that an oncofertility option might have. The total actual points for an oncofertility option equal the sum of actual points for this option in the surveyed centers. The total maximal points for an oncofertility option equal 100 points multiplied by the number of surveyed centers [14, 15].
Results
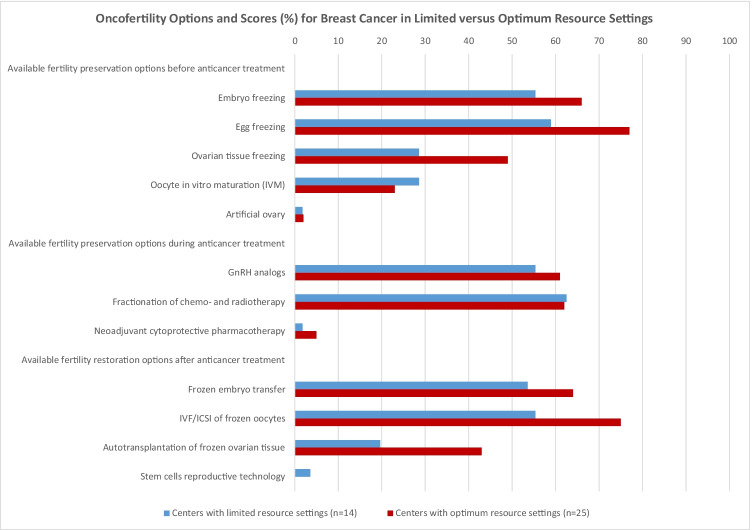
Based on data collected in the Repro-Can-OPEN Study Part I & II, all 39 surveyed centers responded to all questions. The oncofertility scores (%) for options provided to young female patients with breast cancer in the 14 centers with limited resource settings versus in the 25 centers with optimum resource settings, respectively, were as follows ( Table 3 & Fig. 3 );
Table 3.
Oncofertility Options and Scores (%) for Breast Cancer in Limited versus Optimum Resource Settings, based on empirical data from 39 surveyed centers in Repro-Can-OPEN Study Part I & II [14, 15]
| Oncofertility Options and Scores (%) for Breast Cancer | Centers with Limited Resource Settings (Repro-Can-OPEN Study I) (n = 14) |
Centers with Optimum Resource Settings (Repro-Can-OPEN Study II) (n = 25) |
|---|---|---|
| Available fertility preservation options before anticancer treatment | ||
| Embryo freezing | 55.35 | 66 |
| Egg freezing | 58.92 | 77 |
| Ovarian tissue freezing | 28.57 | 49 |
| Oocyte in vitro maturation (IVM) | 28.57 | 23 |
| Artificial ovary | 1.78 | 2 |
| Available fertility preservation options during anticancer treatment | ||
| GnRH analogs | 55.35 | 61 |
| Fractionation of chemo- and radiotherapy | 62.5 | 62 |
| Neoadjuvant cytoprotective pharmacotherapy | 1.78 | 5 |
| Available fertility restoration options after anticancer treatment | ||
| Frozen embryo transfer | 53.57 | 64 |
| IVF/ICSI of frozen oocytes | 55.35 | 75 |
| Autotransplantation of frozen ovarian tissue | 19.64 | 43 |
| Stem cells reproductive technology | 3.57 | 0 |
Fig. 3.
Oncofertility Options and Scores (%) for Breast Cancer in Limited versus Optimum Resource Settings, based on empirical data from 39 surveyed centers in Repro-Can-OPEN Study Part I & II [14, 15]
Available fertility preservation options before anticancer treatment
Embryo freezing (55.35 vs66), egg freezing (58.92 vs 77), ovarian tissue freezing (28.57 vs 49), oocyte in vitro maturation (IVM) (28.57 vs 23) and artificial ovary (1.78 vs 2).
Available fertility preservation options during anticancer treatment
GnRH analogs (55.35 vs 61), fractionation of chemo- and radiotherapy (62.5 vs 62) and neoadjuvant cytoprotective pharmacotherapy (1.78 vs 5).
Available fertility restoration options after anticancer treatment
Frozen embryo transfer (53.57 vs 64), IVF/ICSI of frozen oocytes (55.35 vs 75), autotransplantation of frozen ovarian tissue (19.64 vs 43) and stem cells reproductive technology (3.57 vs 0).
Discussion
Oncofertility options and scores for breast cancer in limited versus optimum resource settings
In our Repro-Can-OPEN Study Part I & II, the responses for breast cancer and their calculated oncofertility scores (Table 3 & Fig. 3) showed the following characteristics: (1) Higher oncofertility scores in optimum resource settings than in limited resource settings especially for established options, (2) frequent utilization of egg freezing, embryo freezing, ovarian tissue freezing, GnRH analogs, and fractionation of chemo- and radiotherapy, (3) promising utilization of oocyte in vitro maturation (IVM), (4) rare utilization of neoadjuvant cytoprotective pharmacotherapy, artificial ovary, and stem cells reproductive technology as they are still in preclinical or early clinical research settings, (5) recognition that proper technical and ethical concerns should be considered when offering advanced and innovative oncofertility options to patients including ovarian tissue freezing and autotransplantation, oocyte in vitro maturation (IVM), artificial ovary technology, neoadjuvant cytoprotective pharmacotherapy and stem cells reproductive technology. Technically, the aforementioned advanced and innovative oncofertility options are sophisticated procedures that require well-resourced oncofertility centers with expert teams of oncologists, reproductive endocrinology and infertility specialists, gynecologists, biologists, embryologists, scientists, and transplantation surgeons. Early referral of breast cancer patients to highly specialized oncofertility centers is strongly recommended.
Recently in 2019, the American Society for Reproductive Medicine Committee Opinion on fertility preservation in patients undergoing gonadotoxic therapies stated that ovarian tissue freezing and autotransplantation should be considered an established medical procedure and no longer considered experimental [4]. Afterwards in 2020, the ESHRE guideline also considered ovarian tissue freezing and autotransplantation non-experimental but used the term ‘innovative’ rather than established to reflect the evidence base [5]. However, oocyte in vitro maturation (IVM), artificial ovary technology, neoadjuvant cytoprotective pharmacotherapy and stem cells reproductive technology are still considered experimental and have limited data on efficacy, and it is essential that they are offered to patients strictly under clear ethical regulations. Obtaining ethical approval from the Institutional Review Board (IRB) or the equivalent ethics committee is essential, as is obtaining informed consent from the patients. Informed consent for experimental medical treatments and interventions should include the explanation of the procedures, benefits, risks, alternative treatments, and information about the expected outcome and costs. Several oncofertility options are expensive and not fully covered by health insurance in many states and countries, leaving many patients under acute financial pressure at the time of a life-altering cancer diagnosis. In such complex situations, doctors and patient navigators as well as patient support and advocacy organizations can play an important role in reassuring and guiding patients [16–18].
General considerations for oncofertility care of breast cancer
Based on the responses and their calculated oncofertility scores (Table 3 & Fig. 3), we propose to design and install plausible oncofertility programs for breast cancer as an extrapolation for a best practice model (Table 4). Existing literature and international oncofertility guidelines and recommendations were also considered [3–6, 19–35]. Immediately after a breast cancer diagnosis, we recommend early referrals of patients to the oncofertility team to review the cancer therapy plan and estimate the related risk of gonadotoxicity and subsequent fertility loss. The risk of anticancer therapy-induced gonadotoxicity and fertility loss depends mainly on the type and stage of the disease, type and dose of anticancer therapy as well as the age of the patient and her ovarian reserve at the time of treatment. If the risk of gonadotoxicity and fertility loss is detected or even unknown, a comprehensive multidisciplinary oncofertility strategy should be offered before, during and after anticancer therapy.
Table 4.
Suggested best practice model: Plausible fertility preservation and restoration strategies for breast cancer patients
| Cancer Patients | Before anticancer therapy (Fertility Preservation) |
During anticancer therapy (Fertility Preservation) |
After anticancer therapy (Fertility Restoration) |
|---|---|---|---|
|
Breast Cancer Patients with or without BRCA mutations |
- Egg freezing - Embryo freezing - Ovarian tissue freezing - In vitro maturation (IVM) of oocytes and vitrification - Artificial ovary technology (promising in research but not yet clinically proven) |
- GnRH analogs - Fractionation of chemo- and radiotherapy - Ovarian shielding in case of combined pelvic irradiation - Neoadjuvant cytoprotective pharmacotherapy (promising in research but not yet clinically proven) |
- Intrauterine transfer of frozen embryo - IVF/ICSI of frozen oocytes - Autotransplantation of frozen ovarian tissue (should be utilized with caution in BRCA mutations) - Stem cells (promising in research but not yet clinically proven) |
From a practical point of view, an effective oncofertility strategy should be individualized and tailored to the patient’s circumstances and it may integrate various established, debatable, and experimental options after proper counselling and obtaining informed consent from the patient. It is recommended that a proposed oncofertility strategy should include at least one cryopreservation option. After complete cure or extended remission from cancer, and when the patient decides to have biological children, a new assessment of reproductive function should be performed. If anticancer therapy-induced premature ovarian insufficiency (POI), fertility restoration may be achieved by using the cryopreserved eggs, embryos or ovarian tissue [36–38].
Installing oncofertility programs for female patients with breast cancer
In addition to breast cancer patients, women with BRCA mutations have several concerns that can affect their reproductive potential. A recent study showed that women with BRCA mutations not only have a lower basal ovarian reserve but also are more likely to lose it after chemotherapy. These findings highlight the importance of offering fertility preservation options to such patients [39]. Furthermore, women with BRCA mutations carry significantly higher risks to develop breast and ovarian cancers (Hereditary Breast-Ovarian Cancer Syndrome; HBOC), and they should receive appropriate oncofertility care as well. According to a recent large study, the cumulative breast cancer risk is 72% for BRCA1 and 69% for BRCA2 carriers, while the cumulative ovarian cancer risk is 44% for BRCA1 and 17% for BRCA2 carriers [40].
Unique medical challenges in oncofertility programs for breast cancer exist and include (1) conventional ovarian stimulation prior to egg or embryo freezing results in elevated serum estradiol levels that should be avoided in estrogen sensitive malignancies such as breast cancer, (2) autotransplantation of frozen ovarian tissue in patients with BRCA mutations should be handled with caution due to significantly higher risks of developing ovarian cancer [41–44].
According to the aforementioned unique medical challenges as well as the responses from the 39 surveyed centers and their calculated oncofertility scores (Table 3 & Fig. 3), we suggest installing the following oncofertility programs for breast cancer as a best practice model (Table 4). Before initiation of anticancer therapy, cryopreservation of eggs or embryos should be attempted with a random-start protocol for controlled ovarian stimulation and using letrozole or tamoxifen to avoid high estradiol levels [45, 46]. Cryopreservation of ovarian tissue can be attempted especially when controlled ovarian stimulation is not feasible. In vitro maturation and further vitrification of oocytes retrieved in-vivo or ex-vivo from the extracted ovarian tissue (ovarian tissue oocytes in vitro maturation; OTO-IVM) could be attempted [47–49]. Artificial ovary technology is still experimental and cannot be relied upon alone as an effective oncofertility option. Although experimental, oocyte IVM and artificial ovary technology aim to provide safe alternatives to avoid future ovarian tissue autotransplantation and any potential risk of reintroducing malignant cells. During anticancer therapy, GnRH analog administration before and during chemotherapy should be considered for reducing the risk of POI but it should not be considered a stand-alone fertility preservation strategy. Fractionation of chemo- and radiotherapy could be attempted whenever deemed feasible by the oncologists. Neoadjuvant cytoprotective pharmacotherapy is still experimental and not yet clinically proven as an effective oncofertility option [50]. After anticancer therapy, fertility restoration may be achieved by frozen embryo transfer, or in vitro fertilization of stored oocytes. Patients with BRCA mutations could be advised to consider preimplantation genetic testing (PGT) during in vitro fertilization to avoid transmitting the mutation [51]. Autotransplantation of frozen ovarian tissue can be offered to restore fertility but it should be handled with caution in patients with BRCA mutations due to significantly higher risks of developing ovarian cancer. Proper ovarian tissue assessment in patients with BRCA mutations is mandatory to reduce the risk of reintroducing malignant cells with autotransplantation. For additional safety measures, it may be a possible option for patients with BRCA mutations to remove the transplanted ovarian tissue as well as the remaining ovary (if any) after childbearing is complete and at the time of an elective caesarian section. Stem cell reproductive technology may be promising in research settings but it is not yet clinically proven as an effective oncofertility option (Table 4).
After installation of these specific oncofertility programs for breast cancer, we encourage using the ‘oncofertility score’ as a prognostic tool to follow up on the development of these new oncofertility programs over time.
In cases where oncofertility options are rejected, contraindicated, infeasible, unsuccessful or unavailable, adoption and third-party reproduction, such as sperm, egg, and embryo donation and surrogacy can be offered as family building alternatives [11].
Limitations of Repro-Can-OPEN Study Part I & II included the small sample size (14 vs 25 surveyed centers with limited and optimum resource settings, respectively) making statistical significance difficult to attain, the empirical status of data collected on the availability and degree of utilization of oncofertility options, and lack of data on success rates of the oncofertility options due to absence of national registries for cancer and IVF treatments in many developing countries involved in the study [14, 15]. Despite challenges, many opportunities exist to improve oncofertility practice in limited resource settings and create potential for the future including improved cancer survival rates and improved success rates of several oncofertility options as well as emergence of new promising technologies. The Oncofertility Consortium will continue to engage more stakeholders from the USA and abroad to help build a sustainable oncofertility core competency worldwide according to the Oncofertility Consortium Vision 2030 [52].
Conclusion
In our Repro-Can-OPEN Study Part I & II, the responses for breast cancer and their calculated oncofertility scores showed the following characteristics: (1) higher oncofertility scores in optimum resource settings than in limited resource settings especially for established options, (2) frequent utilization of egg freezing, embryo freezing, ovarian tissue freezing, GnRH analogs, and fractionation of chemo- and radiotherapy, (3) promising utilization of oocyte in vitro maturation (IVM), (4) rare utilization of neoadjuvant cytoprotective pharmacotherapy, artificial ovary, and stem cells reproductive technology as they are still in preclinical or early clinical research settings, (5) recognition that proper technical and ethical concerns should be considered when offering advanced and innovative oncofertility options. Although challenging, oncofertility teams working in limited resource settings should be encouraged and supported. Dissemination of our comparisons and recommendations will provide efficient oncofertility edification and modeling to oncofertility teams and related healthcare providers around the globe and help them offer the best care possible to their breast cancer patients.
Acknowledgements
Collaborators of Repro-Can-OPEN Study Part I. Salama M, Ataman-Millhouse L, Braham M, Berjeb K, Khrouf M, Rodrigues JK, Reis FM, Silva TC, Sánchez F, Romero S, Smitz J, Vásquez L, Vega M, Sobral F, Terrado G, Lombardi MG, Scarella A, Bourlon MT, Verduzco-Aguirre H, Sánchez AM, Adiga SK, Tholeti P, Udupa KS, Mahajan N, Patil M, Dalvi R, Venter C, Demetriou G, Geel J, Quintana R, Rodriguez G, Quintana T, Viale L, Fraguglia M, Coirini M, Remolina-Bonilla YA, Noguera JAR, Velásquez JC, Suarez A, Arango GD, Pineda JID, Aldecoa MDC, Javed M, Al Sufyan H, Daniels N, Oranye BC, Ogunmokun AA, Onwuzurigbo KI, Okereke CJ, Whesu TC, Woodruff TK. Collaborators of Repro-Can-OPEN Study Part II. Salama M, Laronda MM, Rowell E, Erickson L, Goldman K , Smith K, Pavone M, Duncan FE, Brannigan R, Ataman-Millhouse L, Patrizio P, Rodriguez-Wallberg KA, Okutsu-Horage Y, Suzuki N, Lambertini M, Stern C, Gomez-Lobo V, Maher JY, Hsieh MH, Moravek MB, Anazodo A, Westphal LM, Anderson RA, Wallace WH, Mitchell RT, Nahata L, Whiteside S, Senapati S, Shah DK, Gracia C, Fino ME, Blakemore JK, Quinn GP, Krüssel JS, Baston-Büst DM, Liebenthron J, Andersen CY, Kristensen SG, Mamsen LS, Jayasinghe Y, Su HI, Dolmans MM, Amorim CA, Demeestere I, De Vos M, Van Moer E, Isachenko V, Isachenko E, Mallmann P, Rahimi G, Valli-Pulaski H, Steimer SR, McMahon KV, Orwig KE, Rios JS, Smith JF, Mok-Lin E, Woodruff TK.
Declarations
Disclosure
The authors have declared no conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mahmoud Salama, Email: salamam2@msu.edu.
M. Lambertini, Email: matteo.lambertini@unige.it
MS Christianson, Email: mchris21@jhmi.edu.
Y. Jayasinghe, Email: Yasmin.jayasinghe@unimelb.edu.au
A. Anazodo, Email: Antoinette.anazodo@health.nsw.gov.au
M. De Vos, Email: Michel.devos@uzbrussel.be
F. Amant, Email: frederic.amant@uzleuven.be
C. Stern, Email: Kate.stern@mivf.com.au
L. Appiah, Email: leslie.appiah@cuanschutz.edu
T. L. Woodard, Email: tlwoodard@mdanderson.org
R. A. Anderson, Email: Richard.anderson@ed.ac.uk
L. M. Westphal, Email: lynnw@stanford.edu
R. E. Leach, Email: rleach@msu.edu
K. A. Rodriguez-Wallberg, Email: kenny.rodriguez-wallberg@ki.se
P. Patrizio, Email: pasquale.patrizio@yale.edu
Teresa K. Woodruff, Email: tkw@msu.edu
References
- 1.Fidler MM, Gupta S, Soerjomataram I, Ferlay J, Steliarova-Foucher E, Bray F. Cancer incidence and mortality among young adults aged 20–39 years worldwide in 2012: a population-based study. Lancet Oncol. 2017;18(12):1579–1589. doi: 10.1016/S1470-2045(17)30677-0. [DOI] [PubMed] [Google Scholar]
- 2.Blondeaux E, Massarotti C, Fontana V, Poggio F, Arecco L, Fregatti P, Bighin C, Giannubilo I, Ruelle T, Razeti MG, Boni L, Anserini P, Del Mastro L, Lambertini M. The PREgnancy and FERtility (PREFER) Study Investigating the Need for Ovarian Function and/or Fertility Preservation Strategies in Premenopausal Women With Early Breast Cancer. Front Oncol. 2021;11:690320. doi: 10.3389/fonc.2021.690320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, Wallace WH, Wang ET, Loren AW. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018;36(19):1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 4.Practice Committee of the American Society for Reproductive Medicine (ASRM) Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112(6):1022–1033. doi: 10.1016/j.fertnstert.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 5.ESHRE Guideline Group on Female Fertility Preservation. Anderson RA, Amant F, Braat D, D'Angelo A, de Sousa Chuva, Lopes SM, Demeestere I, Dwek S, Frith L, Lambertini M, Maslin C, Moura-Ramos M, Nogueira D, Rodriguez-Wallberg K, Vermeulen N. ESHRE guideline: female fertility preservation. Hum Reprod Open. 2020;2020(4):hoaa052. doi: 10.1093/hropen/hoaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lambertini M, Peccatori FA, Demeestere I, Amant F, Wyns C, Stukenborg JB, Paluch-Shimon S, Halaska MJ, Uzan C, Meissner J, von Wolff M, Anderson RA, Jordan K. ESMO Guidelines Committee. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2020;31(12):1664–1678. doi: 10.1016/j.annonc.2020.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Oncofertility Consortium - Michigan State University [Internet]. [cited 2021 May 14]. Available from: <http://oncofertility.msu.edu/>
- 8.Oncofertility Professional Engagement Network (OPEN) - Michigan State University [Internet]. [cited 2021 May 14]. Available from: <http://oncofertility.msu.edu/oncofertility-professional-engagement-network>
- 9.Ataman LM, Rodrigues JK, Marinho RM, et al. Creating a Global Community of Practice for Oncofertility. J Glob Oncol. 2016;2(2):83–96. doi: 10.1200/JGO.2015.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashedi A, de Roo SF, Ataman L, et al. A survey of fertility preservation options available to cancer patients around the globe. J Glob Oncol. 2018;4:1–16. doi: 10.1200/JGO.2016.008144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rashedi A, de Roo SF, Ataman L, et al. A survey of third-party parenting options associated with fertility preservation available to patients with cancer around the globe. J Glob Oncol. 2018;4:1–7. doi: 10.1200/JGO.2017.009944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salama M, Ataman L, Taha T, et al. Building Oncofertility Core Competency in Developing Countries: Experience from Egypt, Tunisia, Brazil, Peru, and Panama. J Glob Oncol. 2018;4:1–11. doi: 10.1200/JGO.17.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salama M, Ataman-Millhouse L, Sobral F, et al. Barriers and Opportunities of Oncofertility Practice in Nine Developing Countries and the Emerging Oncofertility Professional Engagement Network. J Glob Oncol. 2018;4:1–7. doi: 10.1200/JGO.18.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salama M, Ataman-Millhouse L, Braham M, et al. Installing oncofertility programs for common cancers in limited resource settings (Repro-Can-OPEN Study): An extrapolation during the global crisis of Coronavirus (COVID-19) pandemic. J Assist Reprod Genet. 2020;37(7):1567–1577. doi: 10.1007/s10815-020-01821-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Practice Committee of the Oncofertility Consortium Installing oncofertility programs for common cancers in optimum resource settings (Repro-Can-OPEN Study Part II): a committee opinion. J Assist Reprod Genet. 2021;38(1):163–176. doi: 10.1007/s10815-020-02012-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anazodo A, Laws P, Logan S, Saunders C, Travaglia J, Gerstl B, Bradford N, Cohn R, Birdsall M, Barr R, Suzuki N, Takae S, Marinho R, Xiao S, Qiong-Hua C, Mahajan N, Patil M, Gunasheela D, Smith K, Sender L, Melo C, Almeida-Santos T, Salama M, Appiah L, Su I, Lane S, Woodruff TK, Pacey A, Anderson RA, Shenfield F, Ledger W, Sullivan E. How can we improve oncofertility care for patients? A systematic scoping review of current international practice and models of care. Hum Reprod Update. 2019;25(2):159–179. doi: 10.1093/humupd/dmy038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anazodo A, Laws P, Logan S, Saunders C, Travaglia J, Gerstl B, Bradford N, Cohn R, Birdsall M, Barr R, Suzuki N, Takae S, Marinho R, Xiao S, Chen QH, Mahajan N, Patil M, Gunasheela D, Smith K, Sender L, Melo C, Almeida-Santos T, Salama M, Appiah L, Su I, Lane S, Woodruff TK, Pacey A, Anderson RA, Shenfield F, Sullivan E, Ledger W. The Development of an International Oncofertility Competency Framework: A Model to Increase Oncofertility Implementation. Oncologist. 2019. pii: theoncologist.2019–0043. [DOI] [PMC free article] [PubMed]
- 18.Salama M, Woodruff TK. Anticancer treatments and female fertility: clinical concerns and role of oncologists in oncofertility practice. Expert Rev Anticancer Ther. 2017;17(8):687–692. doi: 10.1080/14737140.2017.1335199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, Pentheroudakis G; ESMO Guidelines Working Group. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi160-vi170. [DOI] [PubMed]
- 20.Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K; American Society of Clinical Oncology. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;1;31(19):2500–2510. [DOI] [PMC free article] [PubMed]
- 21.Practice Committee of American Society for Reproductive Medicine Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2013;100(5):1214–1223. doi: 10.1016/j.fertnstert.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 22.Ethics Committee of American Society for Reproductive Medicine Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2013;100(5):1224–1231. doi: 10.1016/j.fertnstert.2013.08.041. [DOI] [PubMed] [Google Scholar]
- 23.Martinez F. Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Hum Reprod. 2017;32(9):1802–1811. doi: 10.1093/humrep/dex218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coccia PF, Pappo AS, Beaupin L, Borges VF, Borinstein SC, Chugh R, Dinner S, Folbrecht J, Frazier AL, Goldsby R, Gubin A, Hayashi R, Huang MS, Link MP, Livingston JA, Matloub Y, Millard F, Oeffinger KC, Puccetti D, Reed D, Robinson S, Rosenberg AR, Sanft T, Spraker-Perlman HL, von Mehren M, Wechsler DS, Whelan KF, Yeager N, Gurski LA, Shead DA. Adolescent and Young Adult Oncology, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16(1):66–97. doi: 10.6004/jnccn.2018.0001. [DOI] [PubMed] [Google Scholar]
- 25.Donnez J, Dolmans MM. Fertility Preservation in Women. N Engl J Med. 2017;377(17):1657–1665. doi: 10.1056/NEJMra1614676. [DOI] [PubMed] [Google Scholar]
- 26.Schüring AN, Fehm T, Behringer K, Goeckenjan M, Wimberger P, Henes M, Henes J, Fey MF, von Wolff M. Practical recommendations for fertility preservation in women by the FertiPROTEKT network. Part I: Indications for fertility preservation. Arch Gynecol Obstet. 2018;297(1):241–255. doi: 10.1007/s00404-017-4594-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Wolff M, Germeyer A, Liebenthron J, Korell M, Nawroth F. Practical recommendations for fertility preservation in women by the FertiPROTEKT network. Part II: fertility preservation techniques. Arch Gynecol Obstet. 2018;297(1):257–267. doi: 10.1007/s00404-017-4595-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Wolff M, Andersen CY, Woodruff TK, Nawroth F. FertiPROTEKT, Oncofertility Consortium and the Danish Fertility-Preservation Networks - What Can We Learn From Their Experiences? Clin Med Insights Reprod Health. 2019;13:1179558119845865. doi: 10.1177/1179558119845865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van der Ven H, Liebenthron J, Beckmann M, et al. Ninety-five orthotopic transplantations in 74 women of ovarian tissue after cytotoxic treatment in a fertility preservation network: tissue activity, pregnancy and delivery rates. Hum Reprod. 2016;31(9):2031–2041. doi: 10.1093/humrep/dew165. [DOI] [PubMed] [Google Scholar]
- 30.Dittrich R, Kliesch S, Schüring A, et al. Fertility Preservation for Patients with Malignant Disease. Guideline of the DGGG, DGU and DGRM (S2k-Level, AWMF Registry No. 015/082, November 2017) - Recommendations and Statements for Girls and Women. Geburtshilfe Frauenheilkd. 2018;78(6):567–584. [DOI] [PMC free article] [PubMed]
- 31.Lotz L, Dittrich R, Hoffmann I, Beckmann MW. Ovarian Tissue Transplantation: Experience From Germany and Worldwide Efficacy. Clin Med Insights Reprod Health. 2019;13:1179558119867357. doi: 10.1177/1179558119867357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodriguez-Wallberg KA, Tanbo T, Tinkanen H, et al. Ovarian tissue cryopreservation and transplantation among alternatives for fertility preservation in the Nordic countries - compilation of 20 years of multicenter experience. Acta Obstet Gynecol Scand. 2016;95(9):1015–1026. doi: 10.1111/aogs.12934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodriguez-Wallberg KA, Marklund A, Lundberg F, et al. A prospective study of women and girls undergoing fertility preservation due to oncologic and non-oncologic indications in Sweden-Trends in patients' choices and benefit of the chosen methods after long-term follow up. Acta Obstet Gynecol Scand. 2019;98(5):604–615. doi: 10.1111/aogs.13559. [DOI] [PubMed] [Google Scholar]
- 34.Gellert SE, Pors SE, Kristensen SG, Bay-Bjørn AM, Ernst E, Yding AC. Transplantation of frozen-thawed ovarian tissue: an update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J Assist Reprod Genet. 2018;35(4):561–570. doi: 10.1007/s10815-018-1144-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahmad MF, Sugishita Y, Suzuki-Takahashi Y, Sawada S, Iwahata H, Shiraishi E, Takae S, Horage-Okutsu Y, Suzuki N. Case Report: Young Adults With Breast Cancer: A Case Series of Fertility Preservation Management and Literature Review. Front Med (Lausanne) 2021;6(8):670872. doi: 10.3389/fmed.2021.670872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rodriguez-Wallberg KA, Eloranta S, Krawiec K, Lissmats A, Bergh J, Liljegren A. Safety of fertility preservation in breast cancer patients in a register-based matched cohort study. Breast Cancer Res Treat. 2018;167(3):761–769. doi: 10.1007/s10549-017-4555-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marklund A, Eloranta S, Wikander I, Kitlinski ML, Lood M, Nedstrand E, Thurin-Kjellberg A, Zhang P, Bergh J, Rodriguez-Wallberg KA. Efficacy and safety of controlled ovarian stimulation using GnRH antagonist protocols for emergency fertility preservation in young women with breast cancer-a prospective nationwide Swedish multicenter study. Hum Reprod. 2020;35(4):929–938. doi: 10.1093/humrep/deaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marklund A, Lundberg FE, Eloranta S, Hedayati E, Pettersson K, Rodriguez-Wallberg KA. Reproductive Outcomes After Breast Cancer in Women With vs Without Fertility Preservation. JAMA Oncol. 2021;7(1):86–91. doi: 10.1001/jamaoncol.2020.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oktay KH, Bedoschi G, Goldfarb SB, Taylan E, Titus S, Palomaki GE, Cigler T, Robson M, Dickler MN. Increased chemotherapy-induced ovarian reserve loss in women with germline BRCA mutations due to oocyte deoxyribonucleic acid double strand break repair deficiency. Fertil Steril. 2020;113(6):1251–1260.e1. doi: 10.1016/j.fertnstert.2020.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. JAMA. 2017;317(23):2402–2416. doi: 10.1001/jama.2017.7112. [DOI] [PubMed] [Google Scholar]
- 41.Lambertini M, Goldrat O, Ferreira AR, et al. Reproductive potential and performance of fertility preservation strategies in BRCA-mutated breast cancer patients. Ann Oncol. 2018;29(1):237–243. doi: 10.1093/annonc/mdx639. [DOI] [PubMed] [Google Scholar]
- 42.Lambertini M, Goldrat O, Toss A, et al. Fertility and pregnancy issues in BRCA-mutated breast cancer patients. Cancer Treat Rev. 2017;59:61–70. doi: 10.1016/j.ctrv.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 43.Rodriguez-Wallberg KA, Oktay K. Fertility preservation and pregnancy in women with and without BRCA mutation-positive breast cancer. Oncologist. 2012;17(11):1409–1417. doi: 10.1634/theoncologist.2012-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lambertini M, Di Maio M, Poggio F, et al. Knowledge, attitudes and practice of physicians towards fertility and pregnancy-related issues in young BRCA-mutated breast cancer patients. Reprod Biomed Online. 2019;38(5):835–844. doi: 10.1016/j.rbmo.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 45.Rodgers RJ, Reid GD, Koch J, Deans R, Ledger WL, Friedlander M, Gilchrist RB, Walters KA, Abbott JA. The safety and efficacy of controlled ovarian hyperstimulation for fertility preservation in women with early breast cancer: a systematic review. Hum Reprod. 2017;32(5):1033–1045. doi: 10.1093/humrep/dex027. [DOI] [PubMed] [Google Scholar]
- 46.Bonardi B, Massarotti C, Bruzzone M, Goldrat O, Mangili G, Anserini P, Spinaci S, Arecco L, Del Mastro L, Ceppi M, Demeestere I, Lambertini M. Efficacy and Safety of Controlled Ovarian Stimulation With or Without Letrozole Co-administration for Fertility Preservation: A Systematic Review and Meta-Analysis. Front Oncol. 2020;10:574669. doi: 10.3389/fonc.2020.574669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kedem A, Yerushalmi GM, Brengauz M, et al. Outcome of immature oocytes collection of 119 cancer patients during ovarian tissue harvesting for fertility preservation. J Assist Reprod Genet. 2018;35(5):851–856. doi: 10.1007/s10815-018-1153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fasano G, Dechène J, Antonacci R, et al. Outcomes of immature oocytes collected from ovarian tissue for cryopreservation in adult and prepubertal patients. Reprod Biomed Online. 2017;34(6):575–582. doi: 10.1016/j.rbmo.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 49.Pereira N, Hubschmann AG, Lekovich JP, Schattman GL, Rosenwaks Z. Ex vivo retrieval and cryopreservation of oocytes from oophorectomized specimens for fertility preservation in a BRCA1 mutation carrier with ovarian cancer. Fertil Steril. 2017;108(2):357–360. doi: 10.1016/j.fertnstert.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 50.Yu KD, Ge JY, Liu XY, Mo M, He M, Shao ZM; SPECTRUM Investigators. Cyclophosphamide-free Adjuvant Chemotherapy for Ovarian Protection in Young Women with Breast Cancer: a Randomized Phase 3 Trial. J Natl Cancer Inst. 2021 Apr 2:djab065. 10.1093/jnci/djab065. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 51.Vuković P, Peccatori FA, Massarotti C, Miralles MS, Beketić-Orešković L, Lambertini M. Preimplantation genetic testing for carriers of BRCA1/2 pathogenic variants. Crit Rev Oncol Hematol. 2021;157:103201. doi: 10.1016/j.critrevonc.2020.103201. [DOI] [PubMed] [Google Scholar]
- 52.Woodruff TK, Ataman-Millhouse L, Acharya KS, et al. A View from the past into our collective future: the oncofertility consortium vision statement. J Assist Reprod Genet. 2021;38(1):3–15. doi: 10.1007/s10815-020-01983-4. [DOI] [PMC free article] [PubMed] [Google Scholar]