Abstract
Background
General practitioners (GPs) play a crucial role in the fight against the COVID-19 pandemic as the first point of contact for possibly infected patients and are responsible for short and long-term follow-up care of the majority of COVID-19 patients. Nonetheless, they experience many barriers to fulfilling this role. The PRICOV-19 study investigates how GP practices in 38 countries are organized during the COVID-19 pandemic to guarantee safe, effective, patient-centered, and equitable care. Also, the shift in roles and tasks and the wellbeing of staff members is researched. Finally, PRICOV-19 aims to study the association with practice- and health care system characteristics. It is expected that both characteristics of the GP practice and health care system features are associated with how GP practices can cope with these challenges. This paper describes the protocol of the study.
Methods
Using a cross-sectional design, data are collected through an online questionnaire sent to GP practices in 37 European countries and Israel. The questionnaire is developed in multiple phases, including a pilot study in Belgium. The final version includes 53 items divided into six sections: patient flow (including appointments, triage, and management for routine care); infection prevention; information processing; communication; collaboration and self-care; and practice and participant characteristics. In the countries where data collection is already finished, between 13 and 636 GP practices per country participated in the study. Questionnaire data are linked with OECD and HSMR data regarding national policy responses to the pandemic and analyzed using multilevel models considering the system- and practice-level.
Discussion
To the best of our knowledge, the PRICOV-19 study is the largest and most comprehensive study that examines how GP practices function during the COVID-19 pandemic. Its results can significantly contribute to better preparedness of primary health care systems across Europe for future major outbreaks of infectious diseases.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-021-01587-6.
Keywords: Primary health care, General practice, Quality of care, Patient safety, Equity, Psychosocial, Infectious diseases, Multi-country, COVID-19, PRICOV-19
Background
Primary health care in times of COVID-19
On March 11th, 2020, the World Health Organization formally declared the current COVID-19 outbreak as a pandemic [1]. The pandemic’s toll on the world is unprecedented due to the infectiousness of the SARS-CoV-2 virus, high mortality rates, and unpredictable course [2–4]. To date, massive attention in research [5–7] and policy [8, 9] focuses on the hospital setting. However, only a limited percentage of COVID-19 patients worldwide are being hospitalized [5, 10]. When available, primary health care (PHC) plays a vital role in the fight against the SARS-CoV-2 virus. It is the first point of contact for possibly infected patients [11–17], and the level of care on which the short and long-term follow-up care for the majority of the patients are organized. In addition, PHC workers are gatekeepers to authorize access to hospital care and diagnostic tests [18], and by doing so they limit the risk of overwhelmed hospitals and delayed specialist treatment [19–21]. Yet, PHC workers experience many challenges to fulfill this important role [20, 22]. Research has shown that the core values of PHC [23–25] are under high pressure during the COVID-19 pandemic.
Coordination of care
During the COVID-19 pandemic, health care systems were strongly challenged to provide appropriate care to both COVID-19 patients and other patients. General practitioners (GPs), including out-of-hours doctors and doctors at prisons and nursing homes, were called to manage a growing number of health situations while reorganizing their services and altering how they provided care. Many GPs rapidly reorganized the practice, although local, regional, and national evidence-based guidelines on COVID-19 management were lacking. As a result, services and care provision reorganizations were left to the capacities of the individual GPs. In addition, GPs experienced poor coordination of COVID-19 care and often also poor communication among health care services [26], hindering care coordination. Moreover, GP practices were confronted with unprecedented organizational and structural challenges and limitations to provide high-quality care, such as limited availability of resources in terms of staff, inappropriate infrastructure, and -especially in the early phases of the pandemic- even a lack of personal protective equipment [27].
Comprehensive care
Comprehensive care means that the patient receives care planned and coordinated around their physical, mental, and cognitive health needs, considering their characteristics and context [28]. During the COVID-19 pandemic, the measures taken by the government to prevent the spread of COVID-19, such as lockdown, social distancing, and quarantine, formed on itself an additional risk factor in the context of many patients leading to a decline in physical, mental, and social wellbeing of patients [29]. GPs expressed their concerns about the health and possible collateral damage of these measures on the health of their patients, especially those already living in vulnerable situations: for instance, frail elderly living at home, victims of family violence, people with insecure housing or with limited knowledge of the local language, limited health literacy, or other incriminating social determinants of health [5, 11, 30]. Thus, GPs are uniquely positioned to identify the patients at risk for increased COVID-19 impact [22, 31]. At the same time, the changes in the organization of care taken to reduce the spreading of the virus, such as temporarily closing GP practices, canceling home visits or visits in the nursing home, or limiting the consultations to the urgent acute care or the prescription of medications, might have jeopardized the comprehensive approach of PHC.
Continuity of care
The GP ensures continuous care during illness and the patient’s general course of life. Therefore the GP works together with other health care providers through his directional role for cohesion in health care. During the COVID-19 pandemic, the continuity of care is at risk. On the one hand, patients postponed their visits to the GP due to fear of getting infected [5, 32] or because they did not want to put more burden on the system that was already overstretched [33]. On the other hand, despite recommendations [22], plenty of GP practices had to shut their doors for all planned non-essential care temporarily, and many of the planned contacts with chronic patients or planned preventive activities were temporarily reduced to providing prescriptions for medication. Recent studies describe that PHC visits decreased by more than 25% compared to the situation before the pandemic [34]. These observations have raised concerns of international experts about the sequelae arising from postponed care [5, 35, 36]. This interruption of continuity of care might have led to poor adherence to treatment and higher admission rates to the hospital [6], increased mortality and morbidity [37, 38], and higher direct and indirect costs of health conditions [39]. A recent study in Belgium and the Netherlands among the general population reported that most participants with medical conditions expressed concerns about their health due to the pandemic [40].
First contact accessibility
The accessibility of the GP practice might have been jeopardized due to the organizational changes that had to be taken to prevent the spreading of the virus. With an increased risk of inappropriate or delayed care, vulnerable patient groups might have suffered harder from the reduced access to care. In this context, the relevance of proactive provider-initiated care above and beyond demand-led routine care is widely recognized among GPs [30]. Outreach initiatives by the GP or other PHC workers can help those patients who have difficulties otherwise to access services. Outreaching initiatives might therefore be even more critical during the pandemic compared to the pre-COVID era. However, outreach work requires staff that is skilled to do this. In addition, GP practices were already facing many challenges to providing regular care routine during the exceptional circumstances of COVID-19, which may hinder taking up additional, time-consuming tasks. Also, dependent on the payment system, GPs might not be reimbursed for outreaching work. Literature on the value of capitated versus non-capitated systems during the current pandemic is divided [30, 41].
To preserve personal contact with patients, telephone and video consultations were implemented at an increased speed [34, 42–45]. However, remote consultations may negatively affect patient satisfaction and safety [44, 46, 47]. They are also out of reach for some patient groups such as the elderly, illiterate patients, or patients with no access to a computer or smartphone, increasing health inequity.
Pressure on the health of GPs
The changing organizational context and the uncertainty about how to treat (potential) COVID-19 patients also increased the complexity of the decision-making processes of GPs. In former studies, GPs have mentioned, for example, fear of missing diagnosis during telephone consultations due to language barriers or the lack of non-verbal communication [48]. Protocols may facilitate decision-making, reduce the impact on quality of care, and limit safety incidents [32]. However, in a national study in Italy, the lack of clear protocols on providing care to COVID and non-COVID patients at the beginning of the pandemic was highlighted as a significant stressor for GPs [26]. Other research indicates that healthcare professionals were inundated with guidelines by the government and health care organizations which rapidly changed [49]. Also, the closure of practices in the early stages of the pandemic led to an additional burden on GPs when trying to catch up with postponed care. This all might have resulted in increased pressure on GPs’ mental and physical health. However, we found no studies describing how GPs take care of their wellbeing and cope with the challenges in their work environment.
The need for multi-country research on the organization of primary care during the COVID-19 pandemic
Challenges in the provision of coordinated, comprehensive, continuous, and accessible care, combined with increased pressure on the wellbeing of GPs, might have jeopardized the ability of GPs to take on the role as a critical figure during the COVID-19 pandemic. Therefore, there is a need for multi-country research that focuses on how GP practices deal with the challenges the COVID-19 pandemic poses. Firstly, insights into the quality and performance of primary health care during a challenge such as the COVID-19 pandemic can help providers with reliable and sustained healthcare processes and enable them to achieve their goal of improving care delivery and enhancing patient outcomes. However, we found no studies providing insight on the different dimensions of quality of care. Also, the evidence on the results of the many innovations that have been introduced during the COVID-19 pandemic is inconsistent [34, 44, 45]. Secondly, the pandemic highlighted the increased vulnerability of some patient groups. Nevertheless, it is unclear how and to what extent GP practices have tried to reach out to vulnerable population groups during COVID-19. Thirdly, little is known about the task shifts in GP practices during the pandemic. However, the challenges of COVID-19 present a unique opportunity to rethink the professional roles of staff members in the GP practices. Fourthly, monitoring the health and wellbeing of PHC workers is crucial in a health crisis either way.
Finally, research in other disciplines of PHC has suggested that adaptions of the practice would vary among geographical areas and practice types [50, 51] or country-to-country [33]. It follows the hypotheses that the extent to which GP practices can cope with the challenges of COVID-19 depends not only on the organization of care in the GP practices but also on how the health care system responded to the pandemic. The prevailing health care system of a country in general and the characteristics of the PHC system, in particular, provide the structural framework in which high-quality care can or cannot be provided. As it is assumed that pandemics are destined to become more common in the future [52], cross-country comparative studies are crucial to verify and elaborate the current statements in the literature using in-depth analyses. However, previous research studying the organization of PHC during the COVID-19 pandemic is limited to national studies [30, 41]. We believe the results of the PRICOV-19 study will inform policymakers on how to better prepare PHC systems across Europe for future significant outbreaks of infectious diseases.
About the PRICOV-19 study
Aims and objectives
This paper summarizes the protocol of the cross-sectional PRICOV-19 study. This multi-country study aims to describe how GP practices in 38 countries* are organized during the COVID-19 pandemic to guarantee safe, effective, patient-centered, and equitable care. The study also seeks to assess the shift in roles and tasks in practice and the wellbeing of staff members during the pandemic. Finally, PRICOV-19 aims to determine which practice characteristics and health care system features are associated with safe, effective, patient-centered, and equitable health care and with the mental wellbeing of the GPs.
Research consortium
The PRICOV-19 study is initiated by Quality and Safety Ghent (Q&S Ghent), an interdisciplinary center of expertise for quality and safety in primary care and transmural care at Ghent University (Belgium). This study has formed an international research consortium with over 45 universities and research institutes from 38 countries* (see Additional file 1). The study is being conducted in 37 European countries: Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Kosovo*, Latvia, Lithuania, Luxembourg, Malta, Moldavia, North Macedonia, Norway, Poland, Portugal, Romania, Serbia, Slovenia, Spain, Sweden, Switzerland, The Netherlands, Turkey, and Ukraine; and in Israel (see Fig. 1 [53]).
Fig. 1.
The overview of the participating countries in the PRICOV-19 study. Created with permission from MapChart [53]
A collaboration agreement signed by all the consortium partners sets out the arrangements regarding the rights and responsibilities of all partners, including confidentiality, publication policy, use and exploitation of background and results, liabilities, and protection of personal data. In addition, the fulfillment of all requirements imposed by applicable national laws and by the ethics committee of their authority is central. All consortium partners act as joint controllers in the study.
Data management plan
The protocol of this study and the data handling protocols are described in the Data Management Plan (using DMPOnline software provided by the DMPbelgium Consortium). This living document includes all information on data management and sharing, focusing on processing collected personal data complying with the General Data Protection Regulation (GDPR). The content of the Data Management Plan is regularly reviewed in collaboration with the data protection officer of Ghent University (Belgium), and if necessary, adjustments are made.
Ethics approval and funding
The Research Ethics Committee of Ghent University Hospital approved the overall study and the Belgian data collection (project number BC-07617). The data collection in the other countries is approved by local research Ethics Committees in the respective countries if applicable (see additional file 1). All data is anonymized, and all raw data that could lead to the identification of the participants is permanently removed. PRICOV-19 is set up and implemented without external funding except for a small European General Practice Research Network (EGPRN) funding.
Methods/design
Measurement
A self-reported questionnaire is used to collect information on the level of GP practices and participant's level. For all countries, additional information on the country’s health care system, the regional and national measurements taken during the COVID-19 pandemic, and the impact of COVID-19 on the country’s population health are collected from existing data sources.
Development of the questionnaire
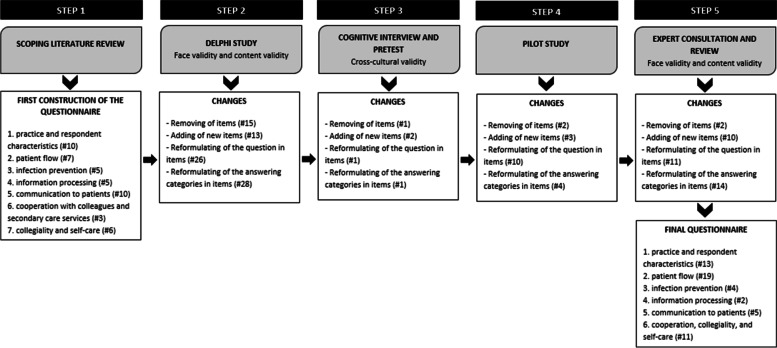
The questionnaire is developed and validated at Ghent University following a five-step procedure. Figure 2 shows the different steps taken and the changes made in each of the steps. Firstly, based on the research objectives, a scoping literature review informed the first draft of the questionnaire [54–60]. Secondly, using a Delphi procedure, a panel of five PHC experts and one methodological expert evaluated the validity of the items and the length of the questionnaire, formulated suggestions for changes, and identified missing items. Next, the research team discussed all feedback until it reached consensus, and a second version of the questionnaire was developed. Thirdly, we organized three cognitive interviews with two GPs and one non-GP to check the acceptability of the questionnaire.
Fig. 2.
The overview of the five steps in the development of the PRICOV-19 questionnaire, included the validity tests
Furthermore, an online version of the questionnaire was made using the Research Electronic Data Capture (REDCap) platform [61] and pretested in ten participants (both GPs and non-GPs). Fourthly, we used the new questionnaire version in a pilot study among a convenience sample of 159 GP practices in Flanders (Belgium). We selected GP practices from a list of training practices included in the GP training program and via the peer-learning groups of GP trainees. All selected practices received an invitation by email, including a link to the online questionnaire. Also, we introduced the study in the newsletter of the Flemish Society for General Practice. In the fifth development step, the international consortium partners reviewed the questionnaire for acceptability in their country and cultural adaptation. Finally, the research team discussed all suggested changes until it reached a consensus.
The final questionnaire consists of 53 items divided over six sections: patient flow (including appointments, triage, and safety management for routine PHC) infection prevention; information processing; communication to patients; collaboration, collegiality, and self-care; and finally, characteristics of participant and GP practice (see Additional file 2). The last section includes, among other things, the validated Mayo Clinic Wellbeing Index [62]. In addition, each partner institution could add up to three country-specific questions to the questionnaire to be used in their country.
Next, we asked all partners to translate the English version of the original questionnaire into the country’s primary spoken language(s) using the forward-backward method. As a result, the questionnaire was translated into the following 38 languages: Albanian (Kosovar version), Bulgarian, Croatian (Croatian and Bosnia and Herzegovina version), Czech, Danish, Dutch (Dutch and Flemish version), Estonian, Finnish, French (French, Walloon, Luxembourgish, and Swiss version), German (German, Austrian, Luxembourgish, and Swiss version), Greek (Greek and Cypriot), Hebrew, Hungarian, Italian, Latvian, Lithuanian, Macedonian, Norwegian, Polish, Portuguese, Romanian (Romanian and Moldovan version), Russian (Moldovan version), Serbian, Slovene, Spanish, Swedish, Turkish, and Ukrainian. Finally, the research team entered these translations into the REDCap platform, and a language- and/or country-specific link to the questionnaire was generated.
Validity of the questionnaire
The psychometric properties of the questionnaire were assessed both quantitatively and qualitatively with a focus on the validity as a theoretical and as an empirical construct (see Fig. 2). Regarding validity as a theoretical construct, the face validity and content validity were tested [63]. The face validity, does the questionnaire appears at face value to measure what it claims to, and the content validity, are items fairly representative of the entire domain the questionnaire seeks to measure [64], were evaluated in step 2 and step 5 of the development of the questionnaire. This was done respectively by Belgian PHC experts and a methodological expert and by researchers from partnering institutions, all international authorities in PHC. The interrater agreement was calculated in step 2, and the results were used to decide on the inclusion of items or groups of items [64]. Although universal guidelines are lacking [65], we used a cut-off point of 80% agreement to decide on the in-or exclusion of items in the questionnaire [64]. Next, some validity tests are performed to measure the empirical validity. The construct validity, referring to the degree to which the instrument’s items are related to a relevant theoretical construct [66–68], was increased by using the scoping review results as the theoretical basis in the first step of the development process. In addition, we included already internationally validated instruments with high construct validity, such as the Mayo Clinic Wellbeing Index [62], where possible. In the PRICOV-19 study, the research team paid attention to the cross-cultural validity of the questionnaire, the extent to which items and answer categories can be interpreted similarly in different languages [69]. In the first place, this was done by cognitive interviews. Secondly, in translating the English version of the questionnaire into the country’s primary language(s), the consortium partners used the forward-backward method [69]. Finally, the partnering institutions discussed possible ambiguities or questions where necessary.
Sampling and recruitment
In each country, the consortium partner(s) recruited GP practices following a pre-defined recruitment procedure. Drawing a randomized sample among all GP practices in the country was preferred over convenience sampling. At least six countries were able to sample the practices randomly. A mixed sample was drawn in some countries, adding a convenience sample to the random sample when the first one did not have enough participants. In about half of the countries, a convenience sample was used. In each country, the consortium partner sent out at least one reminder. In the majority of the countries, a sample was drawn from GP practices in the entire country. Only in a couple of countries, the data collection was limited to a specific region in the country. Partners logged all the steps taken in the sampling procedure. PRICOV-19 aimed to sample between 80 and 200 GP practices per country, depending on the number of GP practices. Table 1 shows more information on the sampling and recruitment in the participating countries. The response rates were calculated by the ratio of the number of GP practices that at least filled in the first part of the questionnaire to the number of GP practices that received an invitation to participate in the study. An assessment of the representativeness of the samples by consortium partners regarding their respective country is included in Additional file 3.
Table 1.
The overview of sampling procedures and response rates in the participating countries
| Country* | Sampling procedure |
Sample (Number of participants/ Number of invitations) |
Response rate (%) |
|---|---|---|---|
| Austria | Random national sample | 140/500 | 28,0 |
| Belgium | Random national sample | 370/1477 | 25,1 |
| Additional convenience sample | 109/134 | 81,3 | |
| Bosnia and Herzegovina | No information available yet | No information available yet | No information available yet |
| Bulgaria | Convenience national sample | 99/105 | 94,3 |
| Croatia | Convenience national sample | 148/1270 | 11,7 |
| Czech Republic | Random samples from 4 regions (Prague, South Bohemia, East bohemia, Central Moravia) and from the list of Young practitioners | 110/500 | 22,0 |
| Cyprus | Data collection is still ongoing | Data collection is still ongoing | Data collection is still ongoing |
| Denmark | Total population | 39/2580 | 1,5 |
| Estonia | Total population | 116/833 | 13,9 |
| Finland | Convenience national sample | 116/746 | 15,5 |
| France | No information available yet | No information available yet | No information available yet |
| Germany | Convenience sample: Erlangen - Nürnberg, München, Marburg, Hannover, Berlin, Würzburg, and Jena | 259/1669 | 15,5 |
| Greece | Random national sample | 94/100 | 94,0 |
| Hungary | Convenience national sample | 222/950 | 23,4 |
| Iceland | Convenience national sample | 31/130 | 23,8 |
| Ireland | All GPs registered in the IGCP** | 187/1538 | 12,2 |
| Israel | Convenience national sample | 87/400 | 21,8 |
| Italy | Convenience national sample | 205/800 | 25,6 |
| Kosovo* | Convenience sample: Prishtina, Peja, Gjakova, Gjilan, and Prizren | 77/105 | 73,3 |
| Latvia | Total population | 147/1600 | 9,2 |
| Lithuania | Convenience national sample | 54/240 | 22,5 |
| Luxembourg | Data collection is still ongoing | Data collection is still ongoing | Data collection is still ongoing |
| Malta | Total population | 13/ at least 200 | No information available yet |
| Moldavia | Convenience sample from 2 municipalities (Chisinau, Balti) and 35 districts (Anenii Noi, Basarabeasca, Briceni, Calarasi, Cahul, Cantemir, Causeni, Cimislia, Criuleni, Comrat, Ciadir-Lunga, Donduseni, Drochia, Dubasari, Edinet, Falesti, Floresti, Glodeni, Hincesti, Ialoveni, Nisporeni, Ocnita, Orhei, Leova, Rezina, Riscani, Singerei, Soldanesti, Soroca, Stefan Voda, Straseni, Taraclia, Telenesti, Ungheni, and Vulcanesti) | 71/293 | 24,2 |
| The Netherlands | Random national sample supplemented by a convenience sample | 165/873 | 18,9 |
| North Macedonia | Data collection is still ongoing | Data collection is still ongoing | Data collection is still ongoing |
| Norway | Total population | 144/1372 | 10,5 |
| Poland | Convenience national sample | 207/2000 | 10,4 |
| Portugal | Random national sample supplemented by a convenience sample | 223/972 | 22,9 |
| Romania | Convenience national sample | 100/400 | 25,0 |
| Serbia | Convenience national sample | 117/130 | 90,0 |
| Slovenia | Convenience national sample | 188/950 | 19,8 |
| Spain | Convenience sample | No information available yet | No information available yet |
| Sweden | Convenience national sample | 85/1180 | 7,2 |
| Switzerland | Convenience sample | 86/269 | 32,0 |
| Turkey | Convenience sample | 145/520 | 27,9 |
| Ukraine | Data collection is still ongoing | Data collection is still ongoing | Data collection is still ongoing |
| United Kingdom | Data collection is still ongoing | Data collection is still ongoing | Data collection is still ongoing |
*All references to Kosovo, whether the territory, institutions or population, in this project, shall be understood in full compliance with United Nations Security Council Resolution 1244 and the ICJ Opinion on the Kosovo declaration of independence, without prejudice to the status of Kosovo;**The Irish College of General Practitioners include approximately 90% of the GP population in Ireland
Data collection
Data collection outside Belgium, where the questionnaire was already piloted earlier, started on November 20th, 2020. The data collection period varies between countries from three to 35 weeks. In the invitation for participation, a country-specific link to the questionnaire is added. In countries with more than one official language, several links are added. Participants are asked for written informed consent on the first page of the online questionnaire. Consent is a prerequisite for participation. Per GP practice, one questionnaire is completed, preferably by a GP or by a staff member familiar with the practice organization. In the countries where data collection is already finished, between 13 and 636 GP practices per country participated in the study. In total, there are already more than 4600 completed questionnaires. All data are centrally stored on the server of Ghent University.
Additional information on the country’s health care system, the regional and national measurements taken during the COVID-19 pandemic, and the impact of COVID-19 on the country’s population health are collected from the Organization for Economic Cooperation and Development (OECD) [70] and the ‘COVID-19 Health System Response Monitor’ (HSRM) [71].
Statistical analysis
The research team at Ghent University is responsible for all data cleaning. All incorrect or corrupted records are removed in this process, variables are recoded, and new summary variables are created. The frequency distribution of all numeric and categorical variables are calculated, and country-specific valid ranges of numeric variables are determined in consultation with the respective consortium partner. Consortium partners translate the responses on string variables from their local language into English. These are then recoded into categorical variables to guarantee the anonymity of the participants.
After finishing data collection, the research team will calculate the relationship between variables at the different levels (participant, practice, health care system), creating multilevel models considering the different levels of aggregation on country and GP practice. Statistical analysis will be performed using SPSS software (SPSS Inc., Chicago, Illinois). The criterion of statistical significance (two-fold, p) is determined at 0.05.
Discussion
To the best of our knowledge, PRICOV-19 is the largest and most comprehensive study to investigate how GP practices on the European continent and in Israel are organized during the COVID-19 pandemic to guarantee safe, effective, patient-centered, and equitable care. It is also the first study to describe on this scale how the COVID-19 pandemic contributed to a shift in roles and tasks in GP practices and to describe the wellbeing of over 4600 healthcare providers in Europe and Israel. Because of its multilevel design, PRICOV-19 can determine which practice characteristics and health care system features are associated with safe, effective, patient-centered, and equitable health care and with the mental wellbeing of the GPs. The results of this study will be crucial for the preparation of PHC systems for future epidemics and pandemics.
Relevance
GPs are placed at the center of the health care system due to their vital role during and after the COVID-19 pandemic. Nonetheless, they experience many challenges to fulfill this role. The PRICOV-19 study fills the gap in the current knowledge and meets the need for in-depth research on the organization of PHC during the COVID-19 pandemic [2, 3, 11, 16, 26, 72, 73]. The involvement of GPs in pandemic preparedness plans is widely recognized [74]. GPs are at the right spot to assess and manage infectious diseases such as seasonal influenza [4]. In addition, patients consider GPs to be a trustful source of health information [30]. This relationship of trust is crucial in the context of contact tracing and the willingness of patients to comply with governmental measures such as social isolation [4, 75–78]. It follows that thanks to the doctor-patient relationship, exacerbations of infectious diseases are quicker noticed by GPs than in emergency departments, and they are more effective in identifying possible underlying trends in community transmission [79]. However, PHC has mainly been sidelined in policy and research during the COVID-19 pandemic [16, 26]. Also, in previous significant outbreaks of infectious diseases such as SARS3 or Influenza H1N14, high-quality evidence on the most suitable approach in PHC was lacking [73].
Strengths and limitations
A public health crisis at a global level calls for international collaborations in research. The PRICOV-19 study brings together more than 45 research institutions and universities from 38 different countries. Besides Israel, all countries are located on the European continent. It follows that the study consortium includes all countries of the European Union except for Slovakia. This results in a unique and rich database with data of over 4600 GP practices and covers almost all different circumstances European PHC systems are operating under. In addition, a rigorously developed questionnaire is added to the strengths of this study.
Despite all the efforts undertaken, there are some limitations to this study. First of all, the basis for data collection in the PRICOV-19 study is a self-report questionnaire. Interpretations of the results should be formulated with awareness of the risk of social and professional desirability, which may negatively influence the truthfulness of the answers. The actual acts and measures in the participating GP practices are unknown. Consortium partners are advised to translate the original questionnaire from English into the country’s primary language(s) using the forward-backward method. However, this was not feasible in all countries. To meet this limitation, extensive pretesting took place to check the validity of the questionnaire. Secondly, we are not able to fully assess the representativeness of the sample. However, to get the best possible picture of selection bias, all partnering institutions keep a detailed logbook about their country’s sample selection and recruitment strategies. The sample is also compared to the national population of GP practices as far as possible. Thirdly, the data collection is not fully simultaneous in the different countries: the data has already been collected in some countries, and data collection is still ongoing in others.
Conclusions
GPs play a vital role in the fight against the COVID-19 pandemic as the first point of contact for possibly infected patients and in charge of short and long-term follow-up care. Nonetheless, GPs experience multiple barriers to fulfilling this role. The functioning of GP practices during the COVID-19 pandemic on the European level has been unclear, and there is a lack of data on this field. PRICOV-19 fills this gap by providing the relevant insights to inform policymakers on better preparing PHC systems across Europe for future major outbreaks of infectious diseases.
Supplementary Information
Acknowledgments
We extend our thanks to all partnering institutions of the PRICOV-19 consortium for their eagerness to collaborate and efforts to set up the PRICOV-19 study in their country.
Abbreviations
- GP
General practitioner
- GP practice
General practice
- PHC
Primary health care
- PRICOV-19
Quality and safety in PRImary care in times of COVid-19
Authors’ contributions
PVB, ZKK, and SW led the conceptualization and design of the study. EVP, ZKK, and SW developed the funding application. SW and EVP lead the coordination of the study. EVP and SW wrote the draft. PVB and ZKK critically reviewed it and provided comments to improve the paper. Finally, all authors read and approved the final manuscript.
Funding
The PRICOV-19 study is mainly set up and implemented without external funding except for the small grant of the European General Practice Research Network (EGPRN). Consequently, the study is relying almost entirely on the goodwill, contribution, and funding of the partnering institutions.
Availability of data and materials
All data are centrally stored on the Ghent University server (Belgium). All data is anonymized at Ghent University, and all raw data that could lead to the identification of the participants is permanently removed. Researchers from partnering institutions will be able to access non-identifiable data from their national database after data cleaning. A reasonable request is required to access non-identifiable data by users who are external to the PRICOV-19 consortium. Access will be subject to a data transfer agreement and following approval from the principal investigator of the PRICOV-19 study.
Declarations
Ethics approval and consent to participate
The overall study is approved by the Research Ethics Committee of Ghent University Hospital (project number BC-07617). Each partnering institution has obtained ethical approval in their country, if applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
All references to Kosovo, whether the territory, institutions or population, in this project, shall be understood in full compliance with United Nations Security Council Resolution 1244 and the ICJ Opinion on the Kosovo declaration of independence, without prejudice to the status of Kosovo.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . WHO director-General's opening remarks at the media briefing on COVID-19-11 march 2020. Geneva: Switzerland; 2020. [Google Scholar]
- 2.de Sutter A, Llor C, Maier M, Mallen C, Tatsioni A, van Weert H, et al. Family medicine in times of ‘COVID-19’: a generalists' voice. Taylor & Francis; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar R, Nedungalaparambil NM, Mohanan N. Emergency and primary care collaboration during COVID-19 pandemic: a quick systematic review of reviews. J Family Med Prim Care. 2020;9(8):3856. doi: 10.4103/jfmpc.jfmpc_755_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali MK, Shah DJ, Del Rio C. Preparing primary care for COVID-20. J Gen Intern Med. 2020;49:1–2. [DOI] [PMC free article] [PubMed]
- 5.Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–133. doi: 10.1080/13814788.2020.1820479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gray R, Sanders C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J Interprof Care. 2020;34(5):672–678. doi: 10.1080/13561820.2020.1823948. [DOI] [PubMed] [Google Scholar]
- 7.Abrashkin KA, Zhang J, Poku A. Acute, post-acute, and primary care utilization in a home-based primary care program during COVID-19. The Gerontologist. 2021;61(1):78–85. doi: 10.1093/geront/gnaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dutour M, Kirchhoff A, Janssen C, Meleze S, Chevalier H, Levy-Amon S, et al. Family medicine practitioners’ stress during the COVID-19 pandemic: a cross-sectional survey. BMC Fam Pract. 2021;22(1):1–8. doi: 10.1186/s12875-021-01382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nacoti M, Ciocca A, Giupponi A, Brambillasca P, Lussana F, Pisano M, et al. At the epicenter of the Covid-19 pandemic and humanitarian crises in Italy: changing perspectives on preparation and mitigation. NEJM Catalyst Innov Care Deliv. 2020;1(2).
- 10.Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. Bmj. 2020;368. [DOI] [PubMed]
- 11.Windak A, Frese T, Hummers E, Klemenc Ketis Z, Tsukagoshi S, Vilaseca J, et al. Academic general practice/family medicine in times of COVID-19–perspective of WONCA Europe. Eur J Gen Pract. 2020;26(1):182–188. doi: 10.1080/13814788.2020.1855136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mash B. Addendum: primary care management of the coronavirus (COVID-19) S Afr Fam Pract. 2020;62(1):1. doi: 10.4102/safp.v62i1.5115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krist AH, DeVoe JE, Cheng A, Ehrlich T, Jones SM. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann Family Med. 2020;18(4):349–354. doi: 10.1370/afm.2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Primary health care and health emergencies. Geneva: World Health Organization; 2018.
- 15.Sarti TD, Lazarini WS, Fontenelle LF, Almeida APSC. What is the role of primary health care in the COVID-19 pandemic? SciELO Public Health. 2020. [DOI] [PubMed]
- 16.Park S, Elliott J, Berlin A, Hamer-Hunt J, Haines A. Strengthening the UK primary care response to covid-19. Bmj. 2020;370. [DOI] [PubMed]
- 17.Li D. First in, last out – the role of family doctors in the fight against novel coronavirus. World Organization of Family Doctors, WONCA; 2020. [Google Scholar]
- 18.Greenfield G, Foley K, Majeed A. Rethinking primary care's gatekeeper role. Bmj. 2016;354:i4803. doi: 10.1136/bmj.i4803. [DOI] [PubMed] [Google Scholar]
- 19.Qiu H, Tong Z, Ma P, Hu M, Peng Z, Wu W, et al. Intensive care during the coronavirus epidemic. Springer; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kearon J, Risdon C. The role of primary care in a pandemic: reflections during the COVID-19 pandemic in Canada. J Prim Care Community Health. 2020;11:2150132720962871. doi: 10.1177/2150132720962871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helgeland J, Telle KE, Grøsland M, Huseby BM, Håberg S, Lindman AS. Admissions to Norwegian hospitals during the COVID-19 pandemic. Scand J Public Health. 2021:14034948211000813. [DOI] [PubMed]
- 22.Kidd M. Australia’s primary care COVID-19 response. Aust J Gen Pract. 2020;49. [DOI] [PubMed]
- 23.Starfield B. Primary care: balancing health needs, services, and technology. USA: Oxford University Press; 1998. [Google Scholar]
- 24.O’Malley AS, Rich EC, Maccarone A, DesRoches CM, Reid RJ. Disentangling the linkage of primary care features to patient outcomes: a review of current literature, data sources, and measurement needs. J Gen Intern Med. 2015;30(3):576–585. doi: 10.1007/s11606-015-3311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Starfield B. Primary care: concept, evaluation, and policy. New York: Oxford University Press; 1992.
- 26.Kurotschka PK, Serafini A, Demontis M, Serafini A, Mereu A, Moro MF, et al. General Practitioners' experiences during the first phase of the COVID-19 pandemic in Italy: a critical incident technique study. Front Public Health. 2021;9:19. doi: 10.3389/fpubh.2021.623904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 28.Haggerty JL, Beaulieu M-D, Pineault R, Burge F, Lévesque J-F, Santor DA, et al. Comprehensiveness of care from the patient perspective: comparison of primary healthcare evaluation instruments. Healthcare. Policy. 2011;7(Spec Issue):154. [PMC free article] [PubMed] [Google Scholar]
- 29.Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:113462. doi: 10.1016/j.psychres.2020.113462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, Wouters E, et al. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21(1):1–6. doi: 10.1186/s12875-020-01326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jani A. Preparing for COVID-19’s aftermath: simple steps to address social determinants of health. J R Soc Med. 2020;113(6):205–207. doi: 10.1177/0141076820921655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khan N, Jones D, Grice A, Alderson S, Bradley S, Carder P, et al. A brave new world: the new normal for general practice after the COVID-19 pandemic. BJGP Open. 2020;4(3). [DOI] [PMC free article] [PubMed]
- 33.Huston P, Campbell J, Russell G, Goodyear-Smith F, Phillips RL, van Weel C, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4). [DOI] [PMC free article] [PubMed]
- 34.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(10):e2021476–e202147e. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feral-Pierssens A-L, Claret P-G, Chouihed T. Collateral damage of the COVID-19 outbreak: expression of concern. Eur J Emerg Med. 2020;27. [DOI] [PMC free article] [PubMed]
- 36.Coma E, Mora N, Méndez L, Benítez M, Hermosilla E, Fàbregas M, et al. Primary care in the time of COVID-19: monitoring the effect of the pandemic and the lockdown measures on 34 quality of care indicators calculated for 288 primary care practices covering about 6 million people in Catalonia. BMC Fam Pract. 2020;21(1):208. doi: 10.1186/s12875-020-01278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91(5):434–437. doi: 10.1093/jnci/91.5.434. [DOI] [PubMed] [Google Scholar]
- 38.Chen S-C, Liu W-C, Chang J-M, Chou M-C, Lin M-Y, Hwang S-C, et al. Early nephrology referral is associated with prolonged survival in hemodialysis patients even after exclusion of lead-time bias. Am J Med Sci. 2010;339(2):123–126. doi: 10.1097/MAJ.0b013e3181c0678a. [DOI] [PubMed] [Google Scholar]
- 39.Golestaneh L, Alvarez PJ, Reaven NL, Funk SE, McGaughey KJ, Romero A, et al. All-cause costs increase exponentially with increased chronic kidney disease stage. Am J Manag Care. 2017;23(10 Suppl):S163–SS72. [PubMed] [Google Scholar]
- 40.van Ballegooijen H, Goossens L, Bruin RH, Michels R, Krol M. Concerns, quality of life, access to care and productivity of the general population during the first 8 weeks of the coronavirus lockdown in Belgium and the Netherlands. BMC Health Serv Res. 2021;21(1):1–8. doi: 10.1186/s12913-021-06240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Korneta P, Kludacz-Alessandri M, Walczak R. The impact of COVID-19 on the performance of primary health care service providers in a capitation payment system: a case study from Poland. Int J Environ Res Public Health. 2021;18(4):1407. doi: 10.3390/ijerph18041407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Southampton: NIHR Journals Library; 2018. [PubMed]
- 43.Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract. 2016;66(648):e460–e4e6. doi: 10.3399/bjgp16X685597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang W, Cheng B, Zhu W, Huang X, Shen C. Effect of telemedicine on quality of Care in Patients with coexisting hypertension and diabetes: a systematic review and Meta-analysis. Telemed J E Health. 2021;27(6):603–614. doi: 10.1089/tmj.2020.0122. [DOI] [PubMed] [Google Scholar]
- 45.Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care Physicians' experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(Suppl):S61–s70. doi: 10.3122/jabfm.2021.S1.200517. [DOI] [PubMed] [Google Scholar]
- 46.Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract. 2005;55(521):956–961. [PMC free article] [PubMed] [Google Scholar]
- 47.Jones D, Neal RD, Duffy SR, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. Lancet Oncol. 2020;21(6):748–750. doi: 10.1016/S1470-2045(20)30242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020;10(6):e039674. doi: 10.1136/bmjopen-2020-039674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sahu AK, Nayer J, Aggarwal P. Novel coronavirus: a capsule review for primary care and acute care physicians. J Family Med Prim Care. 2020;9(4):1820. doi: 10.4103/jfmpc.jfmpc_217_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baumann S, Gaucher L, Bourgueil Y, Saint-Lary O, Gautier S, Rousseau A. Adaptation of independent midwives to the COVID-19 pandemic: a national descriptive survey. Midwifery. 2021;94:102918. doi: 10.1016/j.midw.2020.102918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saint-Lary O, Gautier S, Le Breton J, Gilberg S, Frappé P, Schuers M, et al. How GPs adapted their practices and organisations at the beginning of COVID-19 outbreak: a French national observational survey. BMJ Open. 2020;10(12):e042119. doi: 10.1136/bmjopen-2020-042119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tollefson J. Why deforestation and extinctions make pandemics more likely. Nature. 2020;584(7820):175–176. doi: 10.1038/d41586-020-02341-1. [DOI] [PubMed] [Google Scholar]
- 53.MapChart. Europe. https://mapchartnet/2021. Create your own custom map.
- 54.Reiman T, Pietikainen E, Oedewald P. Multilayered approach to patient safety culture. Qual Saf Health Care. 2010;19(5):e20. doi: 10.1136/qshc.2008.029793. [DOI] [PubMed] [Google Scholar]
- 55.Institute of Medicine Committee on Quality of Health Care . Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 56.Dovey S, Meyers D, Phillips R, Green L, Fryer G, Galliher J, et al. A preliminary taxonomy of medical errors in family practice. BMJ Qual Saf. 2002;11(3):233–238. doi: 10.1136/qhc.11.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sorra J, Franklin M, Streagle S. Medical office survey on patient safety culture. 2008. [Google Scholar]
- 58.Schäfer WL, Boerma WG, De Maeseneer J, Greß S, Heinemann S, Rotar-Pavlic D, et al. QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract. 2011;12(1):115. doi: 10.1186/1471-2296-12-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Allen J, Gay B, Crebolder H, Heyrman J, Svab I, Ram P. The European definition of general practice/ family medicine. Barcelona: Wonca Europe; 2011. [Google Scholar]
- 61.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dyrbye LN, Satele D, Shanafelt T. Ability of a 9-item well-being index to identify distress and stratify quality of life in US Workers. J Occup Environ Med. 2016;58(8):810–817. doi: 10.1097/JOM.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 63.Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22(4):195–201. doi: 10.4103/1117-1936.173959. [DOI] [PubMed] [Google Scholar]
- 64.Sangoseni O, Hellman M, Hill C. Development and validation of a questionnaire to assess the effect of online learning on behaviors, attitude and clinical practices of physical therapists in United States regarding of evidence-based practice. Internet J Allied Health Sci Pract. 2013;11:1–12. [Google Scholar]
- 65.Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–212. doi: 10.1111/j.1365-2648.2006.03716.x. [DOI] [PubMed] [Google Scholar]
- 66.DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 67.Colliver JA, Conlee MJ, Verhulst SJ. From test validity to construct validity … and back? Med Educ. 2012;46(4):366–371. doi: 10.1111/j.1365-2923.2011.04194.x. [DOI] [PubMed] [Google Scholar]
- 68.Smith GT. On construct validity: issues of method and measurement. Psychol Assess. 2005;17(4):396–408. doi: 10.1037/1040-3590.17.4.396. [DOI] [PubMed] [Google Scholar]
- 69.Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268–274. doi: 10.1111/j.1365-2753.2010.01434.x. [DOI] [PubMed] [Google Scholar]
- 70.Reibling N, Ariaans M, Wendt C. Worlds of healthcare: a healthcare system typology of OECD countries. Health policy (Amsterdam, Netherlands) 2019;123(7):611–620. doi: 10.1016/j.healthpol.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 71.Eurohealth . COVID-19 health system response monitor. 2020. [Google Scholar]
- 72.Goodyear-Smith F, Kinder K, Mannie C, Strydom S, Bazemore A, Phillips RL. Relationship between the perceived strength of countries’ primary care system and COVID-19 mortality: an international survey study. BJGP Open. 2020;4(4). [DOI] [PMC free article] [PubMed]
- 73.Wong WC, Wong SY, Lee A, Goggins WB. How to provide an effective primary health care in fighting against severe acute respiratory syndrome: the experiences of two cities. Am J Infect Control. 2007;35(1):50–55. doi: 10.1016/j.ajic.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rohilla J, Tak P, Jhanwar S, Hasan S. Primary care physician's approach for mental health impact of COVID-19. J Family Med Prim Care. 2020;9(7):3189. doi: 10.4103/jfmpc.jfmpc_513_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Daumas RP, Silva GA, Tasca R, Leite IC, Brasil P, Greco DB, et al. The role of primary care in the Brazilian healthcare system: limits and possibilities for fighting COVID-19. Cadernos Saúde Pública. 2020;36:e00104120. doi: 10.1590/0102-311X00104120. [DOI] [PubMed] [Google Scholar]
- 76.Bhattacharyya O, Agarwal P. Adapting primary care to respond to COVID-19. Can Fam Physician. 2021;23.
- 77.Schwartz J, Yen M-Y. Toward a collaborative model of pandemic preparedness and response: Taiwan's changing approach to pandemics. J Microbiol Immunol Infect. 2017;50(2):125–132. doi: 10.1016/j.jmii.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Muldoon LK, Hogg WE, Levitt M. Primary care (PC) and primary health care (PHC) Can J Public Health. 2006;97(5):409–411. doi: 10.1007/BF03405354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lam LT, Chua YX, Tan DH. Roles and challenges of primary care physicians facing a dual outbreak of COVID-19 and dengue in Singapore. Fam Pract. 2020;37(4):578–579. doi: 10.1093/fampra/cmaa047. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are centrally stored on the Ghent University server (Belgium). All data is anonymized at Ghent University, and all raw data that could lead to the identification of the participants is permanently removed. Researchers from partnering institutions will be able to access non-identifiable data from their national database after data cleaning. A reasonable request is required to access non-identifiable data by users who are external to the PRICOV-19 consortium. Access will be subject to a data transfer agreement and following approval from the principal investigator of the PRICOV-19 study.