Abstract
Objectives
This study sought to establish four aspects of feasibility for a mindful parenting program: demand for the program from parents with concerns regarding their child’s internalizing problems, acceptability of the program to those parents, preliminary efficacy, and the likelihood of successful expansion of the program to the intended population.
Methods
The study was a pilot, randomized controlled trial comparing a mindful parenting program to waitlist. Participants were parents (N = 25) of children aged 3–18 years, with self-reported concerns regarding their child’s internalizing problems, recruited from the community. Demand was assessed using recruitment and adherence rates. Acceptability was assessed using parent-reported usefulness. Preliminary efficacy was assessed using parent reports of child internalizing problems, mindful parenting, parenting stress, cognitive emotion regulation, parental experiential avoidance, and parent beliefs about child anxiety. Intervention group parents also provided weekly in-session data on coping in stressful parenting situations. The likelihood of successful expansion was assessed using qualitative feedback on whether and how the program had helped parents manage child internalizing problems, particularly anxiety.
Results
Feasibility was established for the four aspects assessed. The program was well-attended and acceptable to parents. Moderate to large effects were found in favor of the intervention group for most parent and child outcomes. Weekly data showed improved coping in difficult parenting situations. Qualitative feedback suggested that parents believed that increased acceptance and empathy had helped them cope with child internalizing problems.
Conclusions
Mindful parenting programs may assist parents of children with internalizing problems to manage parenting stress and emotionally regulate themselves, even in difficult parenting moments. They may also reduce child internalizing problems, through improved parental emotion regulation, and greater acceptance of and empathy for their child.
Trial Registration
Australian Clinical Trials Registry, registration number ACTRN12620000690954
Keywords: Mindful parenting, Child internalizing, Parenting stress, Experiential avoidance, Emotion regulation, Feasibility
Parenting stress occurs when a parent believes that the demands of parenting outweigh their current resources to manage those demands (Östberg et al., 2007). It is associated with a range of negative outcomes, including more emotional problems in parents (Skreden et al., 2012); more social, emotional, and behavioral problems in children (Anthony et al., 2005); and more negative parenting behaviors (Venta et al., 2016), which contribute to poorer outcomes for the child (Pinquart, 2017). While raising a child is stressful for most parents at least some of the time, the parenting stress literature has focused upon parents of children with externalizing problems, such as rule-breaking, aggressive, or other disruptive behavior (Achenbach & Rescorla, 2001), given the strong link between parenting stress and such problems (Barroso et al., 2018). Sources of stress for these parents include child behavioral problems and parent perceptions regarding their child’s emotional lability and negativity (Baker et al., 2003; Costa et al., 2017).
Despite there also being a moderately strong association between parenting stress and child internalizing problems (Barroso et al., 2018), such as symptoms of anxiety or depression (Achenbach & Rescorla, 2001), this connection with child internalizing has received less research attention (Rodriguez, 2011). The less overt nature of internalizing problems may mean the needs of the families managing these problems are more easily underestimated or overlooked (Clarke-Stewart et al., 2003; Rodriguez, 2011). However, internalizing disorders are amongst the most common types of mental health conditions in children (Polanczyk et al., 2015), with numerous negative outcomes for affected children (Swan & Kendall, 2016). Child internalizing problems also negatively impact families by adding to parenting stress, including by contributing to parental beliefs that the child has a difficult temperament (Fernandes et al., 2020), worries about the child’s ability to cope, and disappointment about the child not meeting expectations (Costa et al., 2006). Further, as well as parenting stress being an outcome of child internalizing, longitudinal evidence shows parenting stress is a risk factor for later child internalizing problems (Stone et al., 2016). Parents of children with internalizing difficulties should therefore be supported to reduce or manage their stress levels for their own well-being, and to reduce the risk of contributing to their child’s internalizing problems.
One factor that helps parents to cope better with stress is parental mindfulness (Campbell et al., 2017). Mindfulness in parenting involves a parent paying moment-to-moment, non-judgmental, non-reactive attention to their child (Kabat-Zinn & Kabat-Zinn, 1997), which helps them to regulate their emotional experiences as a parent and their behaviors with their child (Duncan et al., 2009). A more mindful parenting style can be developed through mindfulness training (Meppelink et al., 2016). Mindful parenting programs (MPPs) are typically based on mindfulness-based stress reduction (MBSR; Kabat-Zinn et al. 1992) and mindfulness-based cognitive therapy (Segal et al., 2013) programs, but concentrate on particular challenges faced by parents (Bögels et al., 2014). These include being aware and accepting of the “whole” child, rather than focusing on perceived weaknesses or problems, tolerating negative thoughts and emotions regarding the child, perspective-taking and empathizing with the child, and being compassionate towards the child and the self as a parent (Bögels & Restifo, 2013).
Numerous studies have investigated the benefits of MPPs over the past decade. A recent meta-analysis of these studies found that MPPs reduce parenting stress and are associated with reductions in children’s internalizing and externalizing problems (Burgdorf et al., 2019). However, most clinical programs have been run for parents of children with a primary externalizing diagnosis (for example, Jones et al., 2018). Only one published study has catered specifically for parents of children with a primary internalizing diagnosis (Racey et al., 2017). As this study did not assess parenting stress, it is not known whether MPPs reduce parenting stress specifically for parents of children with primary internalizing problems. Further, although the adolescents in Racey et al. (2017) reported fewer internalizing symptoms after the intervention, they attended a separate mindfulness course in parallel to the MPP attended by their parents, so it is not known whether their symptoms improved as a result of their own program or the MPP. Accordingly, with the exception of Racey et al., the published literature has assessed internalizing problems only as comorbid symptoms in groups of children where the majority of primary diagnoses were for externalizing disorders. More targeted research is needed to confirm whether MPPs reduce parenting stress and child internalizing problems in families whose primary concern is child internalizing.
Children with primary internalizing problems have a genetic and temperamental vulnerability to internalizing problems, which may be exacerbated by overprotective parenting (Edwards et al., 2010; Rapee, 2012). In contrast, children with comorbid internalizing problems tend to develop these as a result of their primary externalizing problems, for example when these lead to social rejection or academic problems (Willner et al., 2016). Given these different risk factors for primary and comorbid internalizing problems, MPPs could impact the internalizing problems of these two groups of children in different ways. However, the limited research regarding MPPs and child internalizing means that little is known about how mindful parenting might reduce child internalizing problems. According to Burgdorf et al.’s (2019) meta-analysis of MPPs, the majority of which related to children with primary externalizing disorders, reductions in comorbid internalizing problems were not predicted by reductions in parenting stress. Instead, Emerson et al. (2019) found they were partially explained by reductions in parental experimental avoidance, defined as a parent’s difficulty experiencing their child’s negative feelings and managing their own reactions to those negative feelings (Tiwari et al., 2008). Correlational data from community-recruited families has shown that mindful parenting is related to child internalizing problems and parental experiential avoidance, cognitive emotion regulation, and beliefs about child anxiety (Burgdorf & Szabó, 2021), which are each related to child internalizing symptoms (Drake & Ginsburg, 2012; Wald et al., 2018). Experimental research showing improvements in these parent variables following a MPP would provide further evidence of how more mindful parenting could explain reduced child internalizing in families of children with primary internalizing concerns.
As parent-only MPPs have not been studied specifically in families of children with internalizing problems, it is not known whether these programs will be viewed favorably by their parents. Parents of children who experience anxiety tend to be distressed by and avoidant of both their own and their child’s negative emotion (Tiwari et al., 2008), and to believe that shielding their child from negative experiences and distress is beneficial (Kiel et al., 2019; Rousseau & Scharf, 2017). They may, therefore, not wish to change any avoidant or (over)protective behavior associated with these beliefs by attending a MPP, which encourages parents to remain in contact with the negative emotions both of and relating to their child (Bögels & Restifo, 2013). Similarly, the tendency for parents of children suffering from depression to emotionally withdraw from their child (Yap et al., 2014) may limit parents’ desire or motivation to engage in a treatment program which emphasizes emotional connection. Further, this study proposed to recruit parents from the community, since baseline parenting stress is the same for parents of children with a mental health diagnosis and help-seeking parents without a diagnosis (Potharst et al., 2018a). As parenting programs in non-clinical settings can have high attrition rates (Axford et al., 2012), there is also uncertainty about what proportion of enrolled parents would complete the program. Prior to running a full-scale study, it would be prudent to evaluate the feasibility of a MPP for parents recruited in the community, with concerns regarding their child’s emotional well-being.
The objective of this study was therefore to investigate several aspects of the feasibility of a mindful parenting program for parents with concerns regarding their child’s internalizing problems. Despite the uncertainty, we hypothesized that a mindful parenting program for parents with concerns regarding their child’s internalizing problems would be feasible. Specifically, we expected that help-seeking parents would attend the program and find it acceptable. We also expected that the intervention group would report moderate improvements in parenting stress, parental experiential avoidance, cognitive emotion regulation and beliefs about child anxiety, small improvements in child internalizing problems, and that differences between the intervention and control groups would favor the intervention group. Last, we expected that parents would report that the program helped them manage child internalizing symptoms, including anxiety, through improved emotional awareness and acceptance.
Method
Participants
Participants were 25 parents who wished to take part in a pilot randomized controlled trial comparing an 8-week mindful parenting program to waitlist. The sample size was based on the recommendations made by Whitehead et al. (2016) for an 80% powered main trial with two-sided 5% significance, where the standardized effect sizes are expected to be small to medium. Individuals could be included in the study if they were a parent (or acting in the role of parent) with a child aged 3 to 18 years, whose primary self-reported concern regarding their child was the child’s internalizing symptoms. Exclusion criteria were (1) parent’s inadequate mastery of the English language; (2) parent or child participating in another parenting course or psychological therapy for managing child or parent well-being; (3) parent having organic brain damage; (4) parent having current or historic psychotic or bipolar disorder; (5) parent having current or recent (within last year) substance dependence; (6) parent having significant interpersonal difficulties (such as anti-social behavior); (7) parent at current, moderate to high risk of self-harm or suicide; (8) current substantial risk of abuse of any child in the family; or (9) intellectual disability in the child regarding whom assistance was sought. Intervention group parents were significantly older (M = 42.45 years, SD = 4.85) than waitlist parents (M = 37.75 years, SD = 4.67) (t(21) = 2.37, p = .03). There was no difference in the mean age of children of parents in the intervention (M = 6.27 years, SD = 1.95) and waitlist (M = 6.00 years, SD = 3.13) groups. Table 1 contains additional demographic information regarding the participants. There were no significant differences between the parent groups on these demographic variables, or on pre-program scores for any of the outcome variables.
Table 1.
Demographic characteristics of participants
| Characteristic | Intervention group (n = 11) | Waitlist group (n = 12) | Group difference | ||
|---|---|---|---|---|---|
| n | % | n | % | χ2 (df) | |
| Child gender | 0.38 (1) | ||||
| Female | 6 | 54.5 | 5 | 41.7 | |
| Male | 5 | 45.5 | 7 | 58.3 | |
| Parent relation to child | 0.00 (1) | ||||
| Mother | 10 | 90.9 | 11 | 91.7 | |
| Father | 1 | 9.1 | 1 | 8.3 | |
| Caregiver role | 1.23 (2) | ||||
| Primary carer | 6 | 54.5 | 9 | 75.0 | |
| Equal carera | 4 | 36.4 | 2 | 16.7 | |
| Secondary carer | 1 | 9.1 | 1 | 8.3 | |
| No. of children in family | 2.04 (2) | ||||
| 1 | 1 | 9.1 | 4 | 33.3 | |
| 2 | 7 | 63.6 | 6 | 50.0 | |
| 3 | 3 | 27.3 | 2 | 16.7 | |
| Parent cultural identity | 2.96 (3) | ||||
| Australian | 10 | 90.9 | 10 | 83.3 | |
| UK | 0 | 0 | 1 | 8.3 | |
| Eastern European | 0 | 0 | 1 | 8.3 | |
| Middle Eastern | 1 | 9.1 | 0 | 0 | |
| Parent highest level of education | .01 (2) | ||||
| Post-graduate or Bachelor degree | 9 | 81.8 | 10 | 83.3 | |
| Associate degree or vocational training | 1 | 9.1 | 1 | 8.3 | |
| Secondary school or other | 1 | 9.1 | 1 | 8.3 | |
| Parent previous mental health diagnosis | 3.16 (1) | ||||
| Yes | 0 | 0 | 3 | 25.0 | |
| No | 11 | 100 | 9 | 75.0 | |
| History of mindfulness practice | 0.52 (1) | ||||
| Yes | 3 | 27.3 | 5 | 41.7 | |
| No | 8 | 72.7 | 7 | 58.3 | |
| Length of mindfulness practice | .04 (1) | ||||
| < 1 year | 2 | 66.7 | 3 | 60.0 | |
| ≥ 1 year | 1 | 33.3 | 2 | 40.0 | |
| Frequency of mindfulness practice | .04 (1) | ||||
| < monthly | 2 | 66.7 | 3 | 60.0 | |
| ≥ monthly | 1 | 33.3 | 2 | 40.0 | |
aEqual carer is a parent who reports sharing the care of their child approximately equally with another person
Procedures
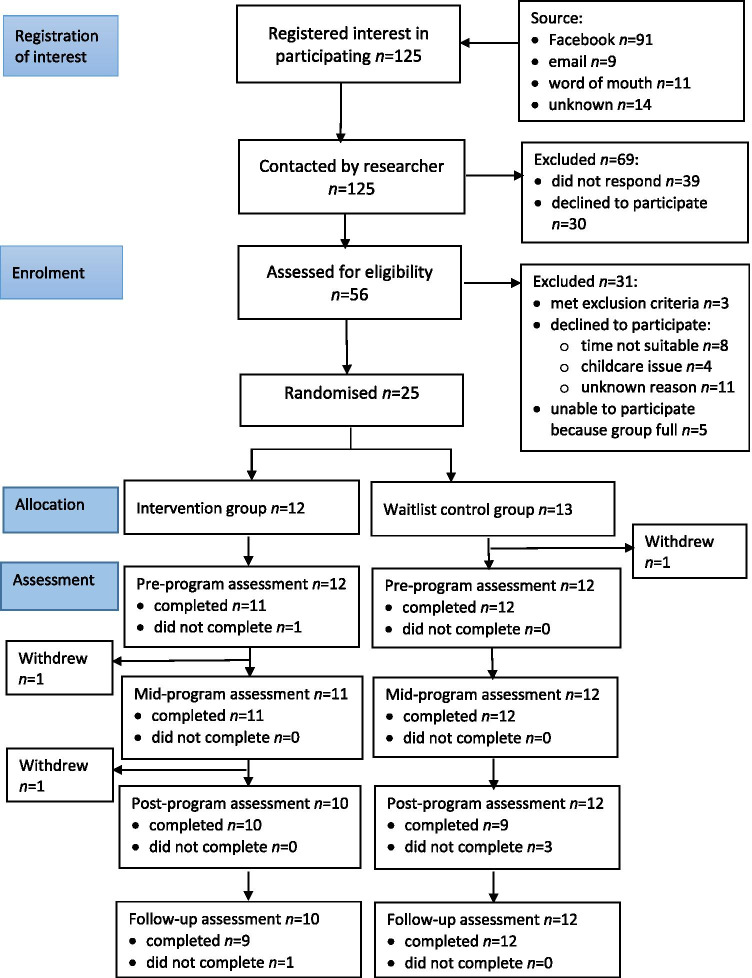
The CONSORT 2010 statement: Extension to randomized pilot and feasibility trials (Eldridge et al., 2016) was used to guide the reporting of this trial. Study advertisements were distributed to potential participants in January 2020, either by email to parents who had previously asked to be notified by the University about mindfulness programs for parents, or on Facebook. The Facebook advertisement was displayed over a 10-day period, to individuals located within the metropolitan area of Sydney, Australia, and interested in the topic areas of “Motherhood”, “Fatherhood”, “Parenting”, “Family”, or “Parents”. The advertisements directed potential participants to a registration of interest form on the data collection website Qualtrics, where they could provide contact details and access the participant information statement and consent form. Of the 125 individuals who registered their interest in participating, 56 were able to be contacted by telephone and assessed for eligibility. Of these individuals, 25 were eligible, able to attend the program on the scheduled dates, and provided consent to participate (see Fig. 1). To ensure allocation concealment during randomization, these 25 participants were randomly allocated on a 1:1 basis to the intervention (n = 12) or waitlist control (n = 13) groups using the website random.org.
Fig. 1.
Flow of participants from registration of interest to follow-up assessment
The program delivered in this study was adapted from the 8-week × 3-hour mindful parenting group program developed for parents experiencing parenting stress by Bögels & Restifo (2013). The adapted program consisted of eight weekly 2-hour group sessions: (1) Automatic pilot, (2) Beginner’s mind, (3) Reconnecting with the body, (4) Responding versus reacting, (5) Parenting patterns and schemas, (6) Conflict and parenting, (7) Love and limits, and (8) Are we there yet? A mindful path through parenting. Each session consisted of an overview of the session theme/s, group discussion of home practice exercises, formal meditation practices followed by a group inquiry regarding each practice, and mindfulness/visualization exercises and discussions related to the week’s theme. The program was run at 6.00–8.00 p.m. on Tuesdays during school term, from February to April 2020. The first five sessions were delivered face-to-face at The University of Sydney, and the remaining three sessions were conducted online using Zoom, due to the closure of the University campus during the COVID-19 pandemic. The program was offered to the control group after all data collection was completed. The program was facilitated by two of the authors, a registered clinical psychology registrar (VB) and a registered clinical psychologist (MS). Both authors have experience working with parents and in group therapy, have a personal mindfulness practice, and have completed mindful parenting teacher training with Professor Susan Bӧgels at the University of Amsterdam.
Some adaptations were made to the Bögels and Restifo (2013) program. Because the program was being run for parents concerned about their child’s emotional well-being rather than behavioral problems, in exercises which asked parents to visualize a stressful parenting situation, we used examples such as a child with anxiety refusing to separate from a parent. The weekly session length was reduced from three to two hours, as parents were recruited from the community rather than treatment clinics. We did this by shortening several formal meditation practices, including body scans and sitting meditations, and omitting the yoga practices. Facilitating the final three sessions of the program via Zoom also required some changes to program content and mode of delivery. These changes included omitting the walking meditations, using the Zoom “share screen” function as a whiteboard for parent input during group exercises, and the “breakout rooms” function for parents to work in pairs. For body scans and a standing meditation, some parents chose to turn off their camera during the practice. Apart from these changes, the online sessions were run as similarly as possible to the face-to-face sessions, including the presence of facilitators at all times. Parents were encouraged to act as if they were together in the same room with the facilitators and other group members. For example, parents were asked to find a private space for the sessions, where they could participate in meditation exercises and group discussions free from interruptions from other family members.
Measures
Feasibility
Bowen et al. (2009) outlined eight potential areas of focus for feasibility studies. We used four of these areas to assess feasibility in this study: Demand, Acceptability, Limited-efficacy testing, and Expansion. Demand relates to the likely use of an intervention by the intended population. We assessed this for parents whose primary concern regarding their child was their internalizing symptoms, through (a) recruitment rates, calculated as the proportion of parents who enrolled in the study (i) after the initial contact from the researchers, and (ii) after registering their interest in participating; (b) attendance rate, being the average attendance rate of parents over 8 sessions; (c) completion rate, being the proportion of parents completing at least 6 of the 8 sessions; (d) withdrawal rate, or the proportion of parents who withdrew from the study after randomization but before the start of the program; and (e) attrition rate, being the proportion of parents who began the program but did not attend at least 4 sessions.
Acceptability refers to the reactions of the participants to an intervention. We assessed acceptability by measuring parent perceptions of program usefulness, including in relation to the COVID-19 pandemic, based on the parent feedback form in Bögels & Restifo (2013). Parents responded to the questions (a) “Which group format did you prefer? (Face-to-face/Online); (b) “To what extent did the COVID-19 pandemic affect your ability to benefit from the program?” where 1 = Very positive impact to 7 = Very negative impact; (c) “How important has the training been for you, overall?” on a scale of 1 to 10 (1 = Not useful at all, 10 = Extremely useful); (d) “Do you feel you got something of lasting value or importance as a result of doing this program?” (yes/no); and (e) “Would you recommend the program to friends or family members?” (yes/no).
Limited-efficacy testing refers to obtaining preliminary evidence of program effects with a small sample, in order to estimate sample and effect sizes for a full-scale trial. We obtained preliminary evidence of effects through parent self-reports on the outcome measures described below. Except where otherwise indicated, all self-report questionnaires were completed by parents online, through Qualtrics. The demographic and mindfulness practice information contained in Table 1 was collected from all parents one week prior to the program. The other questionnaires were completed by all parents one week prior to the program (pre-program), after the fourth session (mid-program), upon completion (post-program), and two months after completion (follow-up). The data on weekly coping with parenting stress was collected from intervention group parents weekly, in-session.
Expansion relates to the likelihood of successfully using an existing intervention with a new population or in a different setting. We did this by collecting qualitative feedback from parents regarding whether and how the program had helped them.
Mindful Parenting
The Interpersonal Mindfulness in Parenting Scale (IMP; Duncan, 2007, Duncan et al., 2009) assesses mindful parenting. The items are rated using a 5-point Likert scale, ranging from 1 = Never True to 5 = Always True. Fourteen items (1, 5, 9–15, 17, 19, 23, 26, 29) are reverse-coded, and higher scores indicate more mindful parenting. We used the 29-item, six-factor version of the IMP, which has the subscales Listening with Full Attention (LFA; “I rush through activities with my child without really being attentive to him/her”), Compassion for the Child (CC; “I am kind to my child when he/she is upset”), Non-judgmental Acceptance of Parental Functioning (NJAPF; “I tend to be hard on myself when I make mistakes as a parent”), Emotional Awareness of the Child (EAC; “It is hard for me to tell what my child is feeling”), Emotional Awareness of Self (EAS; “When I’m upset with my child, I notice how I am feeling before I take action”), and Emotional Non-reactivity in Parenting (ENRP; “I often react too quickly to what my child says or does”) (Burgdorf & Szabó, 2021; de Bruin et al., 2014). A total score is calculated by summing all items. The IMP has demonstrated good convergent and divergent validity (Burgdorf & Szabó, 2021; de Bruin et al., 2014). Pre-program internal consistency (Cronbach’s alpha) and reliability (McDonald’s omega; see Hayes & Coutts, 2020 and McDonald, 1999) in the current sample were α = .72, ω = .72 for LFA; α = .90, ω = .91 for CC; α = .85, ω = .86 for NJAPF; α = .82, ω = .82 for EAC; α = .81, ω = .83 for EAS; α = .80, ω = .83 for ENRP; and α = .93, ω = .92 for IMP Total. Post-program internal consistency was α = .83, ω = .86 for LFA; α = .90, ω = .90 for CC; α = .91, ω = .91 for NJAPF; α = .69, ω = .74 for EAC; α = .93, ω = .93 for EAS; α = .91, ω = .91 for ENRP; and α = .95, ω = .95 for IMP Total.
Parenting Stress
The 18-item Parental Stress Scale (PSS; Berry & Jones, 1995) measures stress associated with the parenting role, for example “I feel overwhelmed by the responsibility of being a parent”. The items are rated on a 5-point scale, going from 1 = Strongly disagree to 5 = Strongly agree. Items 1, 2, 5–8, 17, and 18 are reverse-scored, with a higher score indicating more parenting-related stress. Berry & Jones (1995) reported good convergent and discriminant validity for the PSS, and high internal consistency. In this study, pre-program α = .74 and ω = .67 and post-program α = .78 and ω = .69.
Cognitive Emotion Regulation
The Cognitive Emotion Regulation Questionnaire – Short Form (CERQ; Garnefski & Kraaij, 2006) contains 18 items measuring the cognitive emotion regulation strategies that an individual tends to use in negative situations. Responses are given on a 5-point scale ranging from 1 = (Almost) never to 5 = (Almost) always. The CERQ contains five subscales (Acceptance, Positive Refocusing, Refocus on Planning, Putting into Perspective, Positive Reappraisal) that can be combined into an Adaptive scale, measuring generally helpful strategies, for example “I think about how to change the situation”. It also contains four subscales (Self-blame, Other-blame, Rumination, Catastrophizing) that can be combined into a Maladaptive scale, measuring generally unhelpful strategies, for example “I think that basically the cause must lie within myself”. A higher scale score indicates more frequent use of the strategies in that scale. The short form CERQ has demonstrated acceptable validity and internal consistency (Garnefski & Kraaij, 2006). In this study, however, items 22 and 27 from the CERQ Adaptive scale had very low item-total correlations (.07 and −.07, respectively), so were excluded from the scale. In this study, for the shortened Adaptive scale, α = .74 and ω = .74 pre-program and α = .85, ω = .78 post-program. For the Maladaptive scale, α = .83, ω = .85 pre-program and α = .65, ω = .66 post-program.
Parental Experiential Avoidance
The Parental Acceptance and Action Questionnaire (PAAQ; Cheron et al., 2009) measures experiential avoidance in parenting, being a parent’s unwillingness to witness their child’s negative emotion and their inability to manage their own reactions to those negative feelings, for example “I try hard to avoid having my child feel depressed or anxious”. There are 15 items rated on a 7-point scale from 1 = Never true to 7 = Always true. Items 1, 5–7, 10, and 11 are reverse-scored and higher scores indicate more experiential avoidance. The items are summed to create a total score. Cheron et al. (2009) have reported the PAAQ’s concurrent validity and adequate internal consistency. In this study, pre-program α = .80, ω = .79, and post-program α = .85, ω = .84.
Parent Beliefs Regarding Child Anxiety
The Parental Attitudes, Beliefs and Understanding about Anxiety Scale (PABUA; Wolk et al., 2016) measures a parent’s beliefs and attitudes about their child’s anxiety, with three scales: Overprotection, Approach, and Distress. Wolk et al. (2016) reported the PABUA to have adequate to good internal consistency and good convergent and divergent validity, but in this study the Approach and Distress scales were excluded from analyses due to poor internal consistency and reliability (Approach: α = .46, ω = .59 pre-program and α = .49, ω = .72 post-program; Distress: α = .54, ω = .54 pre-program and α = .56, ω = .60 post-program). We therefore used only the Overprotection scale, which measures parent beliefs about the need to protect their child from anxiety. Pre-program α = .79, ω = .81 and post-program α = .77, ω = .75. The 11 items in the Overprotection scale, for example “It is important that I protect my child from feeling anxious”, are answered on a 5-point scale, from 1 = Strongly disagree to 5 = Strongly agree, with higher scores indicating less helpful beliefs about anxiety.
Child Internalizing Symptoms
We used the parent report versions of the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000, 2001) for preschool-aged children (3–5 years) and school-aged children (6–18 years), to assess child internalizing, with the broadband Internalizing Problems Scale (33 items, for example “Unhappy, sad or depressed” and “Too fearful or anxious”). The items have a 3-point response scale, where 0 = Not true (as far as you know), 1 = Somewhat or sometimes true, and 2 = Very true or often true. A higher score indicates more problems. The CBCL has strong convergent and discriminant validity and internal consistency (Achenbach & Rescorla, 2000, 2001). In this sample, the Internalizing scale had pre-program Cronbach’s alphas of .83 (school-age) and .84 (preschool-age) and post-program alphas of .85 (school-age) and .63 (preschool-age). Reliability could not be calculated using McDonald’s omega due to some items having zero variance. This is likely to be due to the restricted range of symptom severity amongst children of community-recruited families.
Weekly Coping with Parenting Stress
To investigate whether the intervention group parents were benefitting from the program at specific moments of parenting stress, not just at a general trait level, we assessed the intensity of parenting stress, and various aspects of parents’ mindfulness, weekly throughout the program in relation to specific, stressful parenting situations. At the beginning of each of the eight sessions, intervention group parents were guided to visualize a stressful or difficult situation that they had experienced in the past week with or relating to their child. They were encouraged to imagine themselves back in that situation, and to recall as vividly as possible what they were thinking and feeling at the time. In-session, immediately following that guided visualization, we assessed intensity of parenting stress (“During this difficult situation regarding your child, how intensely did you feel stressed (or overwhelmed or unable to cope)?” on a scale of 1 = Not at all to 7 = Extremely intensely). In relation to parents’ experiences during that difficult situation, we assessed (1) the ability to decenter from thoughts and emotions (“I experienced my thoughts and/or feelings as events in my mind, rather than as reflections of reality”), (2) experiential avoidance (“I wished I did not have to deal with what was happening” and “It was unpleasant or uncomfortable to experience my own emotions, and/or watch my child’s emotions”), and (3) self-regulation (“I paused to notice how I was feeling about the situation, before I did anything else”). These statements were rated on a scale of 1 = Not at all true to 7 = Extremely true. For the 5 face-to-face sessions, these assessments were completed on paper by parents individually, without discussion, with a facilitator collecting the questionnaires prior to the rest of the session proceeding. For the 3 Zoom sessions, parents received a personal link to the questionnaire on Zoom, and submitted their answers online prior to the rest of the session proceeding.
Qualitative Assessment of Pathways from Mindful Parenting to Child Internalizing
After program completion, the parents were asked the following questions online, through Qualtrics, about whether and how they believed the program had helped them as parents, including in relation to any perceived child anxiety: (1) Has your relationship with your emotions changed? If yes, how? (2) Did the program change the way you experience your child? If yes, how has this changed? (3) Do you think mindfulness can help you cope with your child’s anxiety? If yes, how do you think it will help? (4) Did the mindful parenting program change the way you view your child’s anxiety? If yes, how did this change?
The initial questions were kept short and closed (yes/no), and were then immediately followed by a broad, open question (If yes, how…?). This technique is recommended for the online collection of qualitative data, in order to sufficiently direct participants’ attention to the issues the researcher wishes them to consider, while providing participants the freedom to explain what their own thoughts or experiences were regarding those issues (Braun et al., 2020). The questions directed parents’ attention to whether they changed their relationship with their own and their child’s emotions, and whether they believed an aspect of mindfulness was behind this change, because we were interested to know whether the beliefs that parents expressed about these issues converged with any changes under the self-report measures, in particular the IMP.
Data Analyses
To examine within- and between-group differences between pre-program scores, and mid-program, post-program, and 2-month follow-up scores, we used Microsoft Excel (2003) to calculate Cohen’s d standardized mean difference effect sizes. For within-group analyses, we used the difference between time 1 and 2 means divided by the standard deviation within group and assumed a correlation of r = 0.7 to calculate the standard deviation within group (for details, see Borenstein et al., 2009). For the between-group analyses, although there were no significant differences between groups on pre-program outcome scores, this may have been partly due to the low numbers in each group. In order to account for any pre-program differences between groups, we therefore used the difference between the treatment and control group change scores, divided by the pooled pre-program standard deviations (for details, see Morris, 2008). An effect size of 0.2 represents a small effect, 0.5 a moderate effect, and 0.8 a large effect (Cohen, 1988). In line with CONSORT guidelines for reporting results of pilot trials that are not powered to test effectiveness, we did not test for statistical significance of these within- or between-group changes (Eldridge et al., 2016).
For the intervention group’s weekly coping data, we conducted repeated-measures ANOVAs using IBM SPSS Statistics for Windows (version 26), to examine the pattern of change in that data across the 8-week program. As there were numerous trends in the data that could have been reported, we have reported only the largest of the trends that reached statistical significance. We also conducted reliable change analyses of self-report outcomes for intervention group parents, using Microsoft Excel (2003). These analyses are suitable for small samples (Zahra & Hedge, 2010) and indicate whether an individual participant’s change is clinically significant, or greater than could occur due to measurement error. Reliable change occurs when the difference between a participant’s pre- and post-program scores, divided by the standard error of the difference, is greater than 1.96 (Jacobson & Truax, 1991). The standard error of the difference has been calculated using the pre-program Cronbach’s alpha, and the standard deviation of the intervention group for each measure (for details, see Busch et al., 2011).
For the qualitative investigation of possible pathways between mindful parenting and child internalizing, we used thematic analysis (Braun & Clarke, 2006) to examine parent feedback regarding changes in parenting. Following the process set out by Braun & Clarke (2006), one author (VB) and a doctoral level clinical psychology post-graduate student read the parent responses to familiarize themselves with the data, then independently coded the data by hand, based on its surface or apparent meaning (Braun & Clarke, 2006), and identified potential themes amongst the coded data. Next, these two researchers refined the list of themes by reviewing the potential themes together, checking that the individual pieces of coded data fit with the proposed themes and agreeing a final list of themes. The themes were then defined by VB and are reported in this paper.
Results
Demand
Figure 1 shows the flow of participants through the study, including registrations of interest, enrolment, allocation to groups, and measurement points. Table 2 shows participant recruitment rates by initial contact and number of registrations. Of the individuals initially contacted via Facebook, and who went on to register their interest in participating in the study, 22.0% were enrolled in the study. Overall, 2.1% of individuals contacted via Facebook enrolled in the study. For those individuals contacted by email who subsequently registered their interest in participating, 22.2% enrolled. Overall, we enrolled 3.4% of the individuals contacted by email.
Table 2.
Participant recruitment rates
| Location of study advertisement | Initial contacts madea (n) | Registrations of interest (n) | Study enrolments (n) | Recruitment rate by contactb | Recruitment rate by registrationc |
|---|---|---|---|---|---|
| 965 | 91 | 20 | 2.1% | 22.0% | |
| 58 | 9 | 2 | 3.4% | 22.2% | |
| Otherd | - | 25 | 3 | - | 12.0% |
| Total | 1023 | 125 | 25 | 2.4% | 20.0% |
aFor email = number of study advertisement emails sent; for Facebook = number of engagements by Facebook users with the post advertising the study; benrolments as a percentage of initial contacts; cenrolments as a percentage of registrations of interest; dparents who heard about the study through word-of-mouth and independently approached the researchers; as the researchers did not initiate contact with these parents, no recruitment rate by contact is available for this category
The average attendance rate of intervention group parents (n = 12) was six out of eight sessions (75%). Two parents were unable to continue their attendance after the fourth session for reasons related to the COVID-19 pandemic. Nine of the 12 parents attended at least six sessions, giving a completion rate of 75%. One parent from each of the intervention and waitlist (n = 13) groups withdrew from the study after randomization but before the intervention began, giving a withdrawal rate of 8%. Two of the 12 intervention group parents completed less than four sessions, giving an attrition rate of 16.7%.
Acceptability
In relation to perceived usefulness of the program and the impact of COVID-19, 100% of parents reported that they preferred face-to-face over online groups. Twenty percent of parents reported that the pandemic had a very positive impact on their ability to benefit from the program, while 60% said it had a minor negative impact and 20% said it had a moderate negative impact. Despite the majority of parents reporting that the pandemic negatively affected their ability to benefit from the program, parents reported that the program had been important for them, with 20% rating the program an 8, 40% rating it a 9, and 40% rating it a 10, on a scale of 1 = Not useful at all, 10 = Extremely useful. In addition, 100% of parents reported that they believed they had got something of lasting value or importance as a result of doing the program, and 100% of parents reported that they would recommend the program to family or friends.
Limited-Efficacy Testing
The means and standard deviations for each outcome at each measurement point are shown in Table 3, for both intervention and waitlist groups. Table 4 shows the within- and between-group Cohen’s d effect sizes for the changes in those outcomes. Between-group differences all favored the intervention group. At program completion (T3), differences between the intervention and waitlist control groups were moderate to large, except for CERQ Adaptive, where the difference was small, and CBCL Pre-school Internalizing, which was negligible. At follow-up (T4), the differences remained moderate to large, except for CBCL Pre-school Internalizing and IMP Compassion for the Child, where the differences were negligible, and CERQ Adaptive, where the differences were small.
Table 3.
Means and standard deviations for child and parent outcomes, for intervention and waitlist control groups
| Pre-program (T1) | Mid-program (T2) | Post-program (T3) | Follow-up (T4) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | M | SD | n | M | SD | n | M | SD | n | |
| IMP Total | ||||||||||||
| Intervention | 93.91 | 12.28 | 11 | 101.45 | 10.70 | 11 | 106.40 | 11.23 | 10 | 108.78 | 13.99 | 9 |
| Waitlist | 93.83 | 15.04 | 12 | 96.92 | 17.98 | 12 | 91.67 | 16.82 | 9 | 96.83 | 15.01 | 12 |
| IMP LFA | ||||||||||||
| Intervention | 15.55 | 2.25 | 11 | 16.82 | 1.72 | 11 | 17.50 | 2.01 | 10 | 18.33 | 2.24 | 9 |
| Waitlist | 15.08 | 2.11 | 12 | 16.00 | 3.10 | 12 | 14.67 | 2.12 | 9 | 15.33 | 2.84 | 12 |
| IMP CC | ||||||||||||
| Intervention | 23.91 | 4.28 | 11 | 24.82 | 3.06 | 11 | 25.40 | 3.92 | 10 | 25.44 | 4.59 | 9 |
| Waitlist | 23.58 | 3.55 | 12 | 23.58 | 3.45 | 12 | 22.78 | 2.91 | 9 | 24.92 | 2.87 | 12 |
| IMP NJAPF | ||||||||||||
| Intervention | 17.18 | 4.75 | 11 | 18.55 | 4.39 | 11 | 20.50 | 3.24 | 10 | 21.56 | 4.10 | 9 |
| Waitlist | 17.33 | 4.19 | 12 | 17.33 | 5.05 | 12 | 15.78 | 5.74 | 9 | 17.17 | 4.22 | 12 |
| IMP EAC | ||||||||||||
| Intervention | 10.45 | 1.29 | 11 | 10.91 | 1.22 | 11 | 11.70 | 1.06 | 10 | 11.78 | 1.86 | 9 |
| Waitlist | 11.50 | 2.07 | 12 | 11.58 | 2.35 | 12 | 12.00 | 1.41 | 9 | 11.50 | 1.93 | 12 |
| IMP EAS | ||||||||||||
| Intervention | 11.45 | 1.69 | 11 | 13.73 | 2.00 | 11 | 14.10 | 1.79 | 10 | 13.78 | 2.44 | 9 |
| Waitlist | 11.58 | 3.06 | 12 | 12.83 | 3.07 | 12 | 11.89 | 4.88 | 9 | 12.58 | 3.80 | 12 |
| IMP ENRP | ||||||||||||
| Intervention | 15.36 | 2.66 | 11 | 16.64 | 3.11 | 11 | 17.20 | 2.62 | 10 | 17.89 | 3.14 | 9 |
| Waitlist | 14.75 | 3.96 | 12 | 15.58 | 4.78 | 12 | 14.56 | 4.59 | 9 | 15.33 | 4.05 | 12 |
| PSS | ||||||||||||
| Intervention | 44.45 | 5.05 | 11 | 41.18 | 5.49 | 11 | 37.30 | 6.58 | 10 | 34.00 | 4.97 | 9 |
| Waitlist | 44.25 | 7.81 | 12 | 44.25 | 8.78 | 12 | 44.67 | 3.97 | 9 | 43.17 | 9.08 | 12 |
| CERQ Adaptive | ||||||||||||
| Intervention | 22.45 | 5.32 | 11 | 22.09 | 4.66 | 11 | 23.30 | 7.38 | 10 | 25.00 | 6.25 | 9 |
| Waitlist | 21.75 | 4.35 | 12 | 22.17 | 3.21 | 12 | 22.00 | 2.12 | 9 | 23.58 | 4.58 | 12 |
| CERQ Maladaptive | ||||||||||||
| Intervention | 20.45 | 6.62 | 11 | 17.45 | 3.75 | 11 | 17.10 | 3.07 | 10 | 16.44 | 1.94 | 9 |
| Waitlist | 18.58 | 2.87 | 12 | 19.33 | 3.39 | 12 | 18.33 | 4.50 | 9 | 18.08 | 3.29 | 12 |
| PAAQ Total | ||||||||||||
| Intervention | 57.18 | 10.00 | 11 | 48.45 | 9.84 | 11 | 45.80 | 11.15 | 10 | 45.22 | 8.38 | 9 |
| Waitlist | 54.42 | 12.44 | 12 | 54.42 | 12.77 | 12 | 57.44 | 9.19 | 9 | 52.42 | 11.93 | 12 |
| PABUA Overprotection | ||||||||||||
| Intervention | 29.18 | 7.80 | 11 | 24.64 | 6.92 | 11 | 25.70 | 6.18 | 10 | 25.44 | 9.49 | 9 |
| Waitlist | 27.17 | 5.22 | 12 | 26.50 | 5.92 | 12 | 26.44 | 5.90 | 9 | 27.33 | 4.79 | 12 |
| CBCL School Internalizing | ||||||||||||
| Intervention | 14.63 | 7.73 | 8 | 10.63 | 4.57 | 8 | 11.86 | 3.89 | 7 | 9.50 | 4.18 | 6 |
| Waitlist | 11.17 | 5.08 | 6 | 10.60 | 7.23 | 5 | 15.50 | 10.75 | 4 | 15.20 | 13.55 | 5 |
| CBCL Preschool Internalizing | ||||||||||||
| Intervention | 15.67 | 6.66 | 3 | 17.33 | 6.66 | 3 | 15.33 | 8.34 | 3 | 15.00 | 4.58 | 3 |
| Waitlist | 16.33 | 8.59 | 6 | 14.29 | 8.50 | 7 | 15.60 | 2.70 | 5 | 16.00 | 9.61 | 7 |
IMP Total is Interpersonal Mindfulness in Parenting (IMP) Total Scale; IMP LFA is IMP Listening with Full Attention Scale; IMP CC is IMP Compassion for the Child Scale; IMP NJAPF is IMP Non-judgmental Acceptance of Parental Functioning Scale; IMP EAC is IMP Emotional Awareness of the Child Scale; IMP EAS is IMP Emotional Awareness of the Self Scale; IMP ENRP is IMP Emotional Non-reactivity in Parenting Scale; PSS is Parental Stress Scale; CERQ Adaptive is Adaptive Scale, Cognitive Emotion Regulation Questionnaire – Short Form (CERQ); CERQ Maladaptive is Maladaptive Scale, CERQ; PAAQ Total is Total Scale, Parental Acceptance and Action Questionnaire; PABUA Overprotection is Overprotection Scale, Parental Attitudes, Beliefs and Understanding about Anxiety Scale; CBCL School Internalizing is Internalizing Scale, Child Behavior Checklist (CBCL) 6–18 years; CBCL Preschool Internalizing is Internalizing Scale, CBCL 3–5 years
Table 4.
Cohen’s d within- and between-group effect sizes for child and parent outcomes
| Outcomes | Within-group effectsa | Between-group effectsb | ||||||
|---|---|---|---|---|---|---|---|---|
| T1-T2 | T2-T3 | T3-T4 | T1-T3 | T1-T4 | T1 | T3 | T4 | |
| IMP Total | 0.84 | 0.48 | 0.35 | 0.96 | 1.15 | 0.01 | 1.02 | 0.83 |
| IMP LFA | 0.64 | 0.26 | 0.54 | 0.67 | 0.82 | 0.22 | 1.04 | 1.12 |
| IMP CC | 0.28 | 0.25 | 0.01 | 0.48 | 0.48 | 0.08 | 0.56 | 0.05 |
| IMP NJAPF | 0.39 | 0.41 | 0.28 | 0.65 | 0.98 | −0.03 | 1.05 | 0.98 |
| IMP EAC | 0.31 | 0.50 | 0.05 | 0.77 | 0.78 | −0.60 | 0.42 | 0.74 |
| IMP EAS | 0.86 | 0.15 | −0.15 | 0.94 | 0.90 | −0.05 | 0.90 | 0.51 |
| IMP ENRP | 0.60 | 0.89 | 0.28 | 0.67 | 0.93 | 0.18 | 0.58 | 0.52 |
| PSS | 0.57 | 0.56 | 0.43 | 0.89 | 1.18 | 0.03 | 1.10 | 1.36 |
| CERQ Adaptive | −0.07 | 0.19 | 0.21 | 0.16 | 0.31 | 0.19 | 0.12 | 0.14 |
| CERQ Maladaptive | 0.47 | 0.09 | 0.20 | 0.47 | 0.55 | −0.37 | 0.60 | 0.67 |
| PAAQ Total | 0.76 | 0.31 | 0.07 | 0.77 | 0.86 | −0.24 | 1.22 | 0.85 |
| PABUA Overprotection | 0.83 | −0.18 | 0.04 | 0.43 | 0.42 | −0.31 | 0.40 | 0.57 |
| CBCL School Internalizing | 0.55 | −0.29 | 0.39 | 0.26 | 0.40 | −0.51 | 0.98 | 1.27 |
| CBCL Preschool Internalizing | −0.27 | 0.25 | 0.03 | 0.03 | 0.19 | 0.08 | 0.04 | 0.04 |
aWithin-group, a negative effect size indicates a deterioration in the outcome; bbetween-group, a negative effect size indicates that the effect favors the waitlist control group; T1 pre-program; T2 mid-program; T3 post-program; T4 2-month follow-up; IMP Total is Interpersonal Mindfulness in Parenting (IMP) Total Scale; IMP LFA is IMP Listening with Full Attention Scale; IMP CC is IMP Compassion for the Child Scale; IMP NJAPF is IMP Non-judgmental Acceptance of Parental Functioning Scale; IMP EAC is IMP Emotional Awareness of the Child Scale; IMP EAS is IMP Emotional Awareness of the Self Scale; IMP ENRP is IMP Emotional Non-reactivity in Parenting Scale; PSS is Parental Stress Scale; CERQ Adaptive is Adaptive Scale, Cognitive Emotion Regulation Questionnaire – Short Form (CERQ); CERQ Maladaptive is Maladaptive Scale, CERQ; PAAQ Total is Total Scale, Parental Acceptance and Action Questionnaire; PABUA Overprotection is Overprotection Scale, Parental Attitudes, Beliefs and Understanding about Anxiety scale; CBCL School Internalizing is Internalizing Scale, Child Behavior Checklist (CBCL) 6–18 years; CBCL Preschool Internalizing is Internalizing Scale, CBCL 3–5 years
In relation to within-group changes, the intervention group outcomes generally improved from pre- to mid-program (T1-T2) and from mid- to post-program (T2-T3). At program completion (T1-T3), the intervention group showed moderate to large improvements from pre-program on all outcomes except CBCL Pre-school Internalizing, which showed negligible change, and CBCL School Internalizing and CERQ Adaptive, which both showed small improvements. Small to moderate improvements then continued to be made on most outcomes between program completion and 2-month follow-up (T3-T4), such that at follow-up (T1-T4), the improvements from pre-program remained moderate to large, except for CBCL Pre-school Internalizing and CERQ Adaptive, which were small.
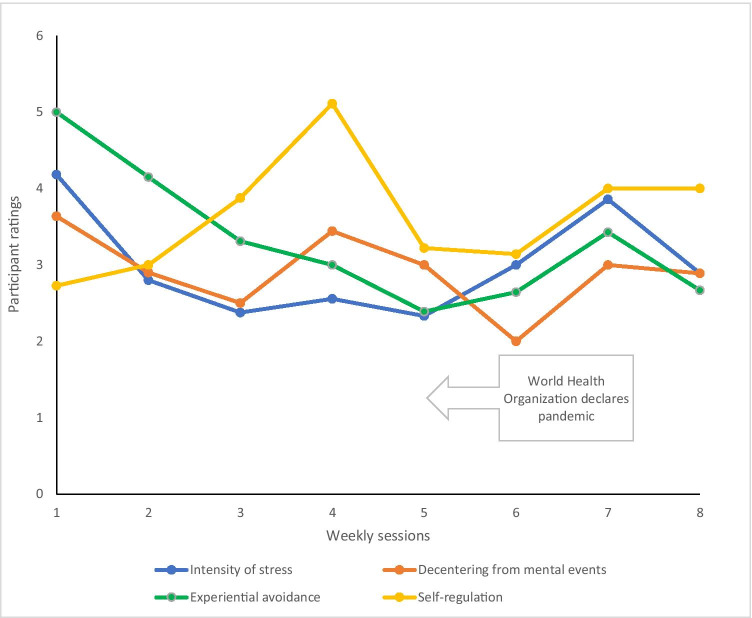
Figure 2 shows the pattern of weekly change in intensity of stress, experiential avoidance, self-regulation, and decentering from mental events, for specific moments of parenting stress experienced by parents. Intensity of stress fell from weeks 1 (M = 4.18, SD = 1.40) to 8 (M = 2.89, SD = 1.22) in a strong cubic pattern (p < .001, ŋp2 = .80). In those stressful situations, experiential avoidance also fell (week 1 M = 5.00, SD = 1.10; week 8 M = 2.67, SD = 1.02) in a strong quadratic (p < .001, ŋp2 = .78) manner, while self-regulation increased (week 1 M = 2.73, SD = 1.62; week 8 M = 4.00, SD = 1.34) in a strong cubic (p = .02, ŋp2 = .41) manner. However, parents’ ability to decenter from mental events deteriorated from week 1 (M = 3.64, SD = 1.36) to week 8 (M = 2.89, SD = 1.30), with no particular pattern evident in this deterioration (all ps > .05). The patterns indicate that over the course of the program, parents experienced improvements in intensity of stress, experiential avoidance, and self-regulation, albeit with some deterioration in the week leading up to and immediately after the declaration of the COVID-19 pandemic.
Fig. 2.
Participant change in intensity of stress and mindfulness, in stressful parenting situations. Note. Lower scores represent less intense stress and experiential avoidance, but poorer self-regulation and decentering
Based on the reliable change analyses, Table 5 shows the proportions of intervention group participants who reliably improved, improved, did not change, deteriorated, and reliably deteriorated, on each outcome. Post-program, reliable improvements were seen in 20% of participants on the Parenting Stress Scale, 50% or more of participants on the IMP Total and Emotional Awareness of Self, and PAAQ Total scales, and in 10–40% of participants on the remaining seven parent outcomes listed in Table 5. At follow-up, the proportions were similar, with reliable improvements in 55% or more of participants on the Parenting Stress Scale, IMP Total and Emotional Non-reactivity in Parenting, and PAAQ Total, and in 11–33% of participants on the remaining eight outcomes. Reliable deterioration was seen in one participant at post-program, for PAAQ Total, and by that same participant and one other at follow-up, for PAAQ Total and CERQ Adaptive. For child outcomes post-program, one of seven school-aged children (14%) and one of three preschool-aged children (33%) showed reliable improvement in internalizing symptoms. At follow-up, two of six school-age children (33%) and none of three preschool-aged children showed reliable improvements.
Table 5.
Reliability of change on each outcome in intervention group participants, from pre- to post-program, and pre-program to follow-up
| Outcomes | Reliable improvementa | Improvementb | No changec | Deteriorationd | Reliable deterioratione | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1-T3 | T1-T4 | T1-T3 | T1-T4 | T1-T3 | T1-T4 | T1-T3 | T1-T4 | T1-T3 | T1-T4 | |||||||||||
| n/nf | % | n/n | % | n/n | % | n/n | % | n/n | % | n/n | % | n/n | % | n/n | % | n/n | % | n/n | % | |
| IMP Total | 7/10 | 70.0 | 6/9 | 66.7 | 3/10 | 30.0 | 3/9 | 33.3 | 0/10 | 0.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP LFA | 4/10 | 40.0 | 3/9 | 33.3 | 3/10 | 30.0 | 6/9 | 66.7 | 2/10 | 20.0 | 0/9 | 0.0 | 1/10 | 10.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP CC | 2/10 | 20.0 | 2/9 | 22.2 | 3/10 | 30.0 | 4/9 | 44.4 | 3/10 | 30.0 | 1/9 | 11.1 | 2/10 | 20.0 | 2/9 | 22.2 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP NJAPF | 3/10 | 30.0 | 2/9 | 22.2 | 5/10 | 50.0 | 6/9 | 66.7 | 1/10 | 10.0 | 1/9 | 11.1 | 1/10 | 10.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP EAC | 4/10 | 40.0 | 1/9 | 11.1 | 3/10 | 30.0 | 4/9 | 44.4 | 2/10 | 20.0 | 4/9 | 44.4 | 1/10 | 10.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP EAS | 5/10 | 50.0 | 2/9 | 22.2 | 4/10 | 40.0 | 5/9 | 55.6 | 1/10 | 10.0 | 2/9 | 22.2 | 0/10 | 0.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| IMP ENRP | 4/10 | 40.0 | 5/9 | 55.6 | 4/10 | 40.0 | 1/9 | 11.1 | 1/10 | 10.0 | 3/9 | 33.3 | 1/10 | 10.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| PSS | 2/10 | 20.0 | 5/9 | 55.6 | 7/10 | 70.0 | 4/9 | 44.4 | 0/10 | 0.0 | 0/9 | 0.0 | 1/10 | 10.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 |
| CERQ Adaptive | 1/10 | 10.0 | 3/9 | 33.3 | 4/10 | 40.0 | 2/9 | 22.2 | 1/10 | 10.0 | 2/9 | 22.2 | 4/10 | 40.0 | 1/9 | 11.1 | 0/10 | 0.0 | 1/9 | 11.1 |
| CERQ Maladaptive | 2/10 | 20.0 | 2/9 | 22.2 | 4/10 | 40.0 | 3/9 | 33.3 | 1/10 | 10.0 | 2/9 | 22.2 | 3/10 | 30.0 | 2/9 | 22.2 | 0/10 | 0.0 | 0/9 | 0.0 |
| PAAQ Total | 8/10 | 80.0 | 7/9 | 77.8 | 1/10 | 10.0 | 1/9 | 11.1 | 0/10 | 0.0 | 0/9 | 0.0 | 0/10 | 0.0 | 0/9 | 0.0 | 1/10 | 10.0 | 1/9 | 0.0 |
| PABUA Overprotection | 2/10 | 20.0 | 1/9 | 11.1 | 4/10 | 40.0 | 5/9 | 55.6 | 0/10 | 0.0 | 1/9 | 11.1 | 4/10 | 40.0 | 2/9 | 22.2 | 0/10 | 0.0 | 0/9 | 0.0 |
| CBCL School Internalizing | 1/7 | 14.3 | 2/6 | 33.3 | 4/7 | 57.1 | 1/6 | 16.7 | 1/7 | 14.3 | 2/6 | 33.3 | 1/7 | 14.3 | 1/6 | 16.7 | 0/7 | 0.0 | 0/6 | 0.0 |
| CBCL Preschool Internalizing | 1/3 | 33.3 | 0/3 | 0.0 | 0/3 | 0.0 | 1/3 | 33.3 | 0/3 | 0.0 | 1/3 | 33.3 | 2/3 | 66.7 | 1/3 | 33.3 | 0/3 | 0.0 | 0/3 | 0.0 |
aStandardized difference score (Δ) shows improvement ≥ 1.96; bΔ shows improvement > 0 but < 1.96; cΔ = 0; dΔ shows deterioration > 0 but < 1.96; eΔ shows deterioration ≥ 1.96; fn/n is the number of participants with change at each level, out of the number of participants for whom data was available; IMP Total is Interpersonal Mindfulness in Parenting (IMP) Total Scale; IMP LFA is IMP Listening with Full Attention Scale; IMP CC is IMP Compassion for the Child Scale; IMP NJAPF is IMP Non-judgmental Acceptance of Parental Functioning Scale; IMP EAC is IMP Emotional Awareness of the Child Scale; IMP EAS is IMP Emotional Awareness of the Self Scale; IMP ENRP is IMP Emotional Non-reactivity in Parenting Scale; PSS is Parental Stress Scale; CERQ Adaptive is Adaptive Scale, Cognitive Emotion Regulation Questionnaire – Short Form (CERQ); CERQ Maladaptive is Maladaptive Scale, CERQ; PAAQ Total is Total Scale, Parental Acceptance and Action Questionnaire; PABUA Overprotection is Overprotection Scale, Parental Attitudes, Beliefs and Understanding about Anxiety Scale; CBCL School Internalizing is Internalizing Scale, Child Behavior Checklist (CBCL) 6–18 years; CBCL Preschool Internalizing is Internalizing Scale, CBCL 3–5 years
Expansion
Ten of the 11 intervention group parents provided post-program feedback regarding whether and how their parenting changed after the program, including in relation to perceived child anxiety. Six themes were identified in this feedback: present-moment awareness, intensity of emotional experience, acceptance, self-regulation, empathy, and self-compassion. Table 6 describes these themes and gives examples illustrating each one.
Table 6.
Themes identified in parent feedback regarding the impact of the mindful parenting program (N = 10)
| Theme (n)a | Description of theme | Excerpt of parent feedback |
|---|---|---|
|
Present-moment awareness (5) |
Describes parents’ increased awareness and understanding of their current experience and how this impacts their parenting |
P2: It has given me a chance to assess how I am feeling which [drives] my decisions P6: Allows me to understand my reaction to it [my child’s anxiety] |
|
Intensity of emotional experience (5) |
Captures parents’ reports of less intense emotional experiences in parenting, and their increased understanding of these experiences |
P1: Less angry P7: You react with much less anxiety yourself P11: I see his anxiety as a normal but not a stressful issue |
|
Acceptance (7) |
Parents’ reported becoming more tolerant and accepting of difficult emotions and situations |
P8: They’re the same emotions, but I’m trying to sit with them before reacting now P10: Felt not so overwhelmed about having to problem solve it [my child’s anxiety]/her |
|
Self-regulation (6) |
Describes parents’ enhanced ability to consciously respond, rather than automatically react, to their child |
P3: Being able to take time and think before I respond to her reactions P9: More patience to help her work through anxiety, opens up new options |
|
Empathy (8) |
Parents described having a broader perspective of their child, being more understanding of them and more able to empathize with them |
P6: Allowed me to reconnect with the bigger picture of my child’s life, beyond the one issue P8: I’ve taken more time to really appreciate her P10: To become more empathetic about my child’s feelings and understanding … while at times hard to understand, give her the space and time to explain them |
| Self-compassion (2) | Parents reported feeling less isolated in dealing with their child’s difficulties |
P7: I found that … we are not alone in the anxiety struggle P11: I’m less hard on myself when things don’t go right |
aNumber of parents whose comments identified the theme
Discussion
This study investigated the feasibility of a mindful parenting program for parents concerned about their child’s internalizing problems. We explored demand for the program success by measuring recruitment, attendance, completion and attrition rates, and acceptability of the program by obtaining feedback on usefulness. To explore ways that mindful parenting might reduce child internalizing, we sought estimates of likely effect sizes in a future definitive trial of the program, for changes in child internalizing problems, mindful parenting, parenting stress, parental experiential avoidance, cognitive emotion regulation, and beliefs about child anxiety. We also used qualitative feedback from parents to explore whether and how mindful parenting might help them cope with child internalizing problems, particularly anxiety.
As hypothesized, there is demand for the program from parents concerned about their child’s internalizing symptoms. The recruitment rates were 2.1% (by Facebook advertisement) and 3.4% (by email). While low, these rates compare favorably to the mean rate of 7% reported in a review of studies using Facebook to recruit for health research (Whitaker et al., 2017). The great majority of the reviewed studies involved only online surveys, whereas this study involved attending a 16-hour program in addition to the collection of data at four points over a four-month period. The attendance and completion rates in this study were both 75%. This rate is acceptable compared to rates reported by other mindful parenting intervention studies, for example, 50% attended at least 4 of 8 sessions in Bögels et al. (2008), 74% attended at least 4 of 8 sessions in Mann et al. (2016), and 84% completed at least 6 of 8 sessions in Racey et al. (2017). While the completion rate was lower than that in Racey et al., this was at least partly attributable to the declaration of the COVID-19 pandemic, which prevented two parents (16.7% of the group) from attending after the fifth session. Acceptability is indicated by parent-reported usefulness of the program. Despite most parents believing the pandemic negatively impacted their ability to benefit from the program, all still found the program to be of lasting value and would recommend it to others, suggesting that a mindful parenting program can be helpful even at times of heightened general stress.
Concerning preliminary effects, compared to waitlist, the intervention group reported large reductions in internalizing problems for their school-aged children (6–18 years). Existing studies have shown reduced internalizing problems in groups of children with externalizing problems or mixed diagnoses (Haydicky et al., 2015), so the present results suggest these reductions also occur for children with primary internalizing concerns. However, despite the preliminary evidence of treatment success at the group level, the low rates of reliable improvement at the individual level indicate that a substantial proportion of children did not benefit from their parents doing the program. This is consistent with findings from other studies, which typically show quite low rates of improvement with reliable change analyses, even for evidence-based child treatments (Smith & Jensen-Doss, 2017). For preschool-aged (3–5 years) children, the symptom reductions were negligible. Due to the dearth of research on the differential impacts of mindful parenting for children of particular developmental stages, it is unclear why the program appeared to benefit only the older group. One study of developmentally delayed preschool children found less internalizing problems after their parents attended a MBSR program (McGregor et al., 2020). The discrepancy between that study and the present one could be due to low baseline levels of internalizing problems in the present sample of preschool children, particularly compared to the higher rates for developmentally delayed children (Van Steensel et al., 2011), such that there was limited scope for improvement in the present sample. Alternatively, since none of the preschool children had reliably reduced internalizing symptoms at follow-up, it is possible that the program did not meet the needs of parents with younger children. Older children are generally more likely to be classified as improved under reliable change analyses, so more targeted programs may be needed for younger children (Smith & Jensen-Doss, 2017), including in mindful parenting programs.
There were moderate to large improvements in all facets of mindful parenting, and overall mindful parenting reliably improved in 70% of parents. This suggests the program was successful in its aim to develop parents’ ability to broaden their attentional focus and acceptance regarding their child. There were also moderate to large reductions in parenting stress, parental experiential avoidance, maladaptive cognitive emotion regulation and unhelpful beliefs regarding child anxiety, and a small increase in adaptive cognitive emotion regulation. These results provide tentative evidence that mindful parenting is at least as useful for parents concerned about child internalizing, as for those managing child externalizing, since the latter group of parents have typically reported only small to moderate reductions in parenting stress, psychopathology, and negative parenting style (Bӧgels et al., 2014). The results also suggest that improved parental emotion regulation may be one way in which mindful parenting can reduce child internalizing symptoms. By building parents’ ability to tolerate difficult emotions, the program may help parents to model more helpful, active coping strategies for their child, instead of the avoidant coping behaviors that tend to maintain internalizing symptoms (Tiwari et al., 2008). Parental modelling of strategies predicts the child’s use of strategies and the child’s internalizing symptoms (Gunzenhauser et al., 2014; Wald et al., 2018).
This study went beyond showing general trait improvements. The weekly coping data showed that, even with pandemic-related uncertainty occurring throughout the program, parents felt less intensely stressed and were less experientially avoidant and more self-regulated, in specific, difficult parenting moments. The program therefore appears to help parents respond to their children in a more helpful manner, even at times of heightened stress when this might otherwise have been too difficult. This is particularly important in relation to parents of children with internalizing problems, since they are more likely to interpret situations in a threatening manner (Creswell et al., 2005) and to intervene in difficult situations, for example by physically or emotionally removing themselves or their child from the situation, which can contribute to or maintain child internalizing problems (McLeod et al., 2007; Tiwari et al., 2008). This could be explained by the program successfully broadening parents’ attentional focus and acceptance regarding their child, so they become more receptive to experience (Bishop et al., 2004). This would allow for less threatening evaluations of particular situations, and therefore lowered stress appraisals (Weinstein et al., 2009) and less need for avoidant, overprotective, or other unhelpful parenting behavior (Tiwari et al., 2008).
Finally, based on the qualitative feedback, it appears likely that a mindful parenting program would be successful with parents of children with primary internalizing concerns. Parent feedback regarding how the program helped them to cope with their child’s internalizing symptoms raised six themes that overlapped somewhat with the six facets of the IMP (de Bruin et al., 2014). The two most commonly identified themes were acceptance and empathy, which was similar to the acceptance and emotional awareness that we expected. Acceptance and the theme self-compassion together reflect the IMP facet Non-judgmental Acceptance of Parental Functioning (NJAPF), which captures a parent’s ability to be accepting and compassionate regarding themself as a parent. The identification of the themes acceptance and self-compassion is consistent with evidence from earlier studies, which have found NJAPF to be the aspect of mindful parenting most predictive of child internalizing problems (Burgdorf & Szabó, 2021). The theme empathy encompasses the Emotional Awareness of the Child (EAC) and Compassion for the Child facets of the IMP. After NJAPF, EAC is the only other facet of mindful parenting that has been found to predict child internalizing problems (Burgdorf & Szabó, 2021). Lack of awareness regarding a child’s anxiety could result in a parent failing to help the child manage that anxiety or managing it unhelpfully (Hurrell et al., 2017). Conversely, more aware or empathic parents can help reduce child anxiety, for example by providing an appropriate level of encouragement for their child to approach anxiety-inducing situations, allowing gradual exposures to such situations (Settipani & Kendall, 2017). Greater empathy may also reduce child internalizing by increasing the child’s perception of parental warmth or support (Flory, 2004; Stern et al., 2015), which is longitudinally associated with reductions in child internalizing problems (Pinquart, 2017).
Parent feedback also raised themes of present-moment awareness, intensity of emotional experience (including less intense stress), and self-regulation. The intensity of emotional experience and self-regulation themes were similar to the Emotional Awareness of Self and Emotional Non-reactivity in Parenting IMP facets. Although some studies have found that parenting stress does not predict child internalizing (Burgdorf et al., 2019; Emerson et al., 2019), there may be an indirect link, through self-regulation. Stress makes it more difficult for parents to use appropriate strategies to regulate their own emotional state and behaviors (Crandall et al., 2015; Raio et al., 2013). As self-regulation influences how parents respond to a child’s negative emotions, and the development of a child’s own regulatory skills (Morris et al., 2017), it plays a crucial role in the child’s well-being, including their level of anxiety (Morris et al., 2017; Wald et al., 2018). Accordingly, less stressed parents can better self-regulate, thus lowering their child’s risk of anxiety. Present-moment awareness was similar to the IMP Listening with Full Attention facet (LFA), although unlike LFA, it related to the parents’ attention for their own, rather than their child’s, present experiences. A heightened awareness of their own experience and how it affects their parenting may also improve parental self-regulation, by allowing more conscious responding to the child, for example with more positive and less negative behaviors, which both predict lower child internalizing problems over time (Pinquart, 2017). Overall, the qualitatively identified themes support the quantitative data in suggesting that mindful parenting may help reduce child internalizing symptoms by improving parents’ ability to regulate themselves and by improving their emotional connection with their child.
Limitations and Future Research
There were several limitations related to assessment, in this study. The post-program internal consistencies and reliabilities for the CERQ Maladaptive and CBCL Internalizing (preschool) scales were relatively low. This could have impacted the accuracy of effects found for these two outcomes. Common method bias is also likely to have affected the effect estimates. For example, using parents as the sole respondents may have inflated effects due to the tendency to respond in a positive way or social desirability (Podsakoff et al., 2012). Parents invested significant time in the 8-week program, which may have led them to report greater improvements in the measured outcomes than actually occurred. Future studies could reduce the impact of this bias by including different respondents (Podsakoff et al., 2012), such as partners or children of participating parents, for example regarding the child’s internalizing symptoms and their perceptions of any change in the participating parent. The qualitative data was collected from parents online, using a small number of open-ended questions. While the use of online questionnaires for collecting qualitative data is convenient for parents and can provide rich data (Braun et al., 2020), it is also possible that parents may have given less thought to their answers or provided less detail in this online format, than if they were interviewed by a researcher.
There were also limitations related to the sample. As we used a community-recruited sample, it is suggested that the study be replicated in a clinical sample, for example with parents of children with a diagnosed internalizing disorder. It is also important to note that the proportion of fathers participating in this study was very low (8%), with only 1 father participating in each group. Mothers report higher levels of mindful parenting than fathers (Moreira & Canavarro, 2015), and there is no evidence as to the structure of mindful parenting in fathers (Burgdorf & Szabó, 2021). The present results may therefore not be indicative of the outcomes for fathers, either due to differences between mothers and fathers in baseline levels, or in the structure, of mindful parenting. Similarly, the sample was homogenous in that it consisted largely of parents with a tertiary education, who identified culturally as “Australian”. Replication of the study in different population groups is necessary, as parental engagement with parenting programs can be affected by factors including education, socio-economic status, and cultural values (Axford et al., 2012). Accordingly, although promising, the improvements in parent and child outcomes in this small feasibility sample must be regarded as preliminary, until replicated in a definitive trial of the program for this population of parents.
Author Contribution
VB: designed the study, co-facilitated the program, collected and analyzed the data, and wrote and revised the manuscript. MA: reviewed the statistical analyses and each version of the manuscript. MS: reviewed and revised the study design, co-facilitated the program, and reviewed the statistical analyses and each version of the manuscript. All authors approved the final version of the manuscript for submission.
Funding
The corresponding author is supported by a Research Training Program scholarship.
Declarations
Ethics
Ethical approval (793/2019) was obtained from the Human Research Ethics Committee of The University of Sydney. Informed written consent was obtained from all participants in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. University of Vermont, Research Centre for Children, Youth, and Families; 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. University of Vermont, Research Centre for Children, Youth, and Families; 2001. [Google Scholar]
- Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, Shaffer S. The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Infant and Child Development. 2005;14:133–154. doi: 10.1002/icd.385. [DOI] [Google Scholar]
- Axford N, Lehtonen M, Kaoukji D, Tobin K, Berry V. Engaging parents in parenting programs: Lessons from research and practice. Children and Youth Services Review. 2012;34:2061–2071. doi: 10.1016/j.childyouth.2012.06.011. [DOI] [Google Scholar]
- Baker BL, McIntyre L, Blacher J, Crnic K, Edelbrock C, Low C. Pre-school children with and without developmental delay: Behaviour problems and parenting stress over time. Journal of Intellectual Disability Research. 2003;47:217–230. doi: 10.1046/j.1365-2788.2003.00484.x. [DOI] [PubMed] [Google Scholar]
- Barroso NE, Mendez L, Graziano PA, Bagner DM. Parenting stress through the lens of different clinical groups: A systematic review & meta-analysis. Journal of Abnormal Child Psychology. 2018;46:449–461. doi: 10.1007/s10802-017-0313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry JO, Jones WH. The Parental Stress Scale: Initial psychometric evidence. Journal of Social and Personal Relationships. 1995;12:463–472. doi: 10.1177/2F0265407595123009. [DOI] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. doi: 10.1093/clipsy/bph077. [DOI] [Google Scholar]
- Bögels SM, Hellemans J, van Deursen S, Romer M, van der Meulen R. Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting and marital functioning. Mindfulness. 2014;5:536–551. doi: 10.1007/s12671-013-0209-7. [DOI] [Google Scholar]
- Bögels SM, Hoogstad B, van Dun L, de Schutter S, Restifo K. Mindfulness training for adolescents with externalising disorders and their parents. Behavioural and Cognitive Psychotherapy. 2008;36:193–209. doi: 10.1017/S1352465808004190. [DOI] [Google Scholar]
- Bögels SM, Restifo K. Mindful parenting in mental health care. Springer; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. John Wiley; 2009. [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, Bakken S, Kaplan CP, Squiers L, Fabrizio C, Fernandez M. How we design feasibility studies. American Journal of Preventive Medicine. 2009;36:452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Braun V, Clarke V, Boulton E, Davey L, McEvoy C. The online survey as a qualitative research tool. International Journal of Social Research Methodology. 2020 doi: 10.1080/13645579.2020.1805550. [DOI] [Google Scholar]
- Burgdorf V, Szabó M. The Interpersonal Mindfulness in Parenting Scale in mothers of children and infants: Factor structure and associations with child internalizing problems. Frontiers in Psychology. 2021 doi: 10.3389/fpsyg.2020.633709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgdorf V, Szabó M, Abbott MJ. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Frontiers in Psychology. 2019;10:1336. doi: 10.3389/fpsyg.2019.01336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch AM, Wagener TL, Gregor KL, Ring KT, Borrelli B. Utilizing reliable and clinically significant change criteria to assess for the development of depression during smoking cessation treatment: The importance of tracking idiographic change. Journal of Addictive Behavior. 2011;36:1228–1236. doi: 10.1016/j.addbeh.2011.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell K, Thoburn JW, Leonard HD. The mediating effects of stress on the relationship between mindfulness and parental responsiveness. Couple and Family Psychology: Research and Practice. 2017;6:48–59. doi: 10.1037/cfp0000075. [DOI] [Google Scholar]
- Cheron DM, Ehrenreich JT, Pincus DB. Assessment of parental experiential avoidance in a clinical sample of children with anxiety disorders. Child Psychiatry and Human Development. 2009;40:383–403. doi: 10.1007/s10578-009-0135-z. [DOI] [PubMed] [Google Scholar]
- Clarke-Stewart KA, Allhusen VD, McDowell DJ, Thelen L, Call JD. Identifying psychological problems in young children: How do mothers compare with child psychiatrists? Journal of Applied Developmental Psychology. 2003;23:589–624. doi: 10.1016/S0193-3973(03)00006-6. [DOI] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioural sciences. Routledge; 1988. [Google Scholar]
- Costa AP, Steffgen G, Ferring D. Contributors to well-being and stress in parents of children with autism spectrum disorder. Research in Autism Spectrum Disorders. 2017;37:61–72. doi: 10.1016/j.rasd.2017.01.007. [DOI] [Google Scholar]
- Costa NM, Weems CF, Pellerin K, Dalton R. Parenting stress and childhood psychopathology: An examination of specificity to internalizing and externalizing symptoms. Journal of Psychopathology and Behavioral Assessment. 2006;28:113–122. doi: 10.1007/s10862-006-7489-3. [DOI] [Google Scholar]
- Crandall A, Deater-Deckard K, Riley AW. Maternal emotion and cognitive control capacities and parenting: A conceptual framework. Developmental Review. 2015;36:105–126. doi: 10.1016/j.dr.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell C, Schniering CA, Rapee RM. Threat interpretation in anxious children and their mothers: Comparison with nonclinical children and the effects of treatment. Behaviour Research and Therapy. 2005;43:1375–1381. doi: 10.1016/j.brat.2004.10.009. [DOI] [PubMed] [Google Scholar]
- de Bruin EI, Zijlstra BJH, Geurtzen N, van Zundert RMP, van de Weijer-Bergsma E, Hartman EE, Nieuwesteeg AM, Duncan LG, Bögels SM. Mindful parenting assessed further: Psychometric properties of the Dutch version of the Interpersonal Mindfulness in Parenting Scale (IMP) Mindfulness. 2014;5:200–212. doi: 10.1007/s12671-012-0168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake KL, Ginsburg GS. Family factors in the development, treatment, and prevention of childhood anxiety disorders. Clinical Child and Family Psychology Review. 2012;15:144–162. doi: 10.1007/s10567-011-0109-0. [DOI] [PubMed] [Google Scholar]
- Duncan, L. G. (2007). Assessment of mindful parenting among parents of early adolescents: Development and validation of the Interpersonal Mindfulness in Parenting Scale (Publication number: 3380731) [Doctoral dissertation, Pennsylvania State University]. ProQuest LLC.
- Duncan LG, Coatsworth J, Greenberg MT. A model of mindful parenting: Implications for parent-child relationships and prevention research. Clinical Child and Family Psychology Review. 2009;12:255–270. doi: 10.1007/s10567-009-0046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards SL, Rapee RM, Kennedy S. Prediction of anxiety symptoms in preschool-aged children: Examination of maternal and paternal perspectives. Journal of Child Psychology & Psychiatry. 2010;51:313–321. doi: 10.1111/j.1469-7610.2009.02160.x. [DOI] [PubMed] [Google Scholar]
- Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., Lancaster, G. A., on behalf of the PAFS consensus group. (2016). CONSORT 2010 statement: Extension to randomized pilot and feasibility trials. British Medical Journal, 355.10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed]
- Emerson, L. M., Aktar, E., de Bruin, E., Potharst, E., & Bögels, S. (2019). Mindful parenting in secondary child mental health: Key parenting predictors of treatment effects. Mindfulness. https://doi.org/10/1007/s12671-019-01176-w
- Fernandes DV, Canavarro MC, Moreira H. The mediating role of parenting stress in the relationship between anxious and depressive symptomatology, mothers’ perception of infant temperament, and mindful parenting during the postpartum period. Mindfulness. 2020 doi: 10.1007/s12671-020-01327-4. [DOI] [Google Scholar]
- Flory V. A novel clinical intervention for severe childhood depression and anxiety. Clinical Child Psychology and Psychiatry. 2004;9:9–23. doi: 10.1177/1359104504039167. [DOI] [Google Scholar]
- Garnefski N, Kraaij V. Cognitive Emotion Regulation Questionnaire - Development of a short 18-item version (CERQ-short) Personality and Individual Differences. 2006;41:1045–1053. doi: 10.1016/j.paid.2006.04.010. [DOI] [Google Scholar]
- Gunzenhauser C, Fäsche A, Friedlmeier W, von Suchodoletz A. Face it or hide it: Parental socialization of reappraisal and response suppression. Frontiers in Psychology. 2014;4:1–14. doi: 10.3389/fpsyg.2013.00992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydicky J, Shecter C, Wiener J, Ducharme JM. Evaluation of MBCT for adolescents with ADHD and their parents: Impact on individual and family functioning. Journal of Child and Family Studies. 2015;24:76–94. doi: 10.1007/s10826-013-9815-1. [DOI] [Google Scholar]
- Hayes AF, Coutts JJ. Use omega rather than Cronbach’s alpha for estimating reliability. But…. Communication Methods and Measures. 2020;14:1–24. doi: 10.1080/19312458.2020.1718629. [DOI] [Google Scholar]
- Hurrell KE, Houwing FL, Hudson JL. Parental meta-emotion philosophy and emotion coaching in families of children and adolescents with an anxiety disorder. Journal of Abnormal Child Psychology. 2017;45:569–582. doi: 10.1007/s10802-016-0180-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jones L, Gold E, Totsika V, Hastings RP, Jones M, Griffiths A, Silverton S. A mindfulness parent wellbeing course: Evaluation of outcomes for parents of children with autism and related disabilities recruited through special schools. European Journal of Special Needs Education. 2018;33:16–30. doi: 10.1080/08856257.2017.1297571. [DOI] [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, Lenderking WR, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Kabat-Zinn M. Everyday blessings. The inner work of mindful parenting. First Trade; 1997. [Google Scholar]
- Kiel EJ, Wagers KB, Luebbe AM. The Attitudes About Parenting Strategies for Anxiety Scale: A measure of parenting attitudes about protective and intrusive behavior. Assessment. 2019;26:1504–1523. doi: 10.1177/2F1073191117719513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J, Kuyken W, O’Mahen H, Ukoumunne OC, Evans A, Ford T. Manual development and pilot randomised controlled trial of mindfulness-based cognitive therapy versus usual care for parents with a history of depression. Mindfulness. 2016;7:1024–1033. doi: 10.1007/s12671-016-0543-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP. Test theory: A unified treatment. Lawrence Erlbaum; 1999. [Google Scholar]
- McLeod BD, Weisz JR, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McGregor HA, Sanner CM, Neece CL. Effects of MBSR parent intervention on internalizing problems in children: ASD status as a moderator. Journal of Mental Health Research in Intellectual Disabilities. 2020;13:343–363. doi: 10.1080/19315864.2020.1815913. [DOI] [Google Scholar]
- Meppelink R, de Bruin EI, Wanders-Mulder FH, Vennik CJ, Bögels SM. Mindful parenting training in child psychiatric settings: Heightened parental mindfulness reduces parents’ and children’s psychopathology. Mindfulness. 2016;7:680–689. doi: 10.1007/s12671-016-0504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira H, Canavarro MC. Individual and gender differences in mindful parenting: The role of attachment and caregiving representations. Personality and Individual Differences. 2015;87:13–19. doi: 10.1016/j.paid.2015.07.021. [DOI] [Google Scholar]
- Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods. 2008;11:364–386. doi: 10.1177/1094428106291059. [DOI] [Google Scholar]
- Morris AS, Criss MM, Silk JS, Houltberg BJ. The impact of parenting on emotion regulation during childhood and adolescence. Child Development Perspectives. 2017;11:233–238. doi: 10.1111/cdep.12238. [DOI] [Google Scholar]
- Östberg M, Hagekull B, Hagelin E. Stability and prediction of parenting stress. Infant and Child Development. 2007;16:207–223. doi: 10.1002/icd.516. [DOI] [Google Scholar]
- Pinquart M. Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta-analysis. Marriage & Family Review. 2017;53:613–640. doi: 10.1080/01494929.2016.1247761. [DOI] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology. 2012;63:539–569. doi: 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology & Psychiatry. 2015;56:345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Potharst ES, Aktar E, Rexwinkel M, Rigterink M, Bögels SM. Mindful with your baby: Feasibility, acceptability and effects of a mindful parenting group training for mothers and their babies in a mental health context. Mindfulness. 2017;8:1236–1250. doi: 10.1007/s12671-017-0699-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potharst ES, Baartmans JMD, Bögels SM. Mindful parenting training in a clinical versus non-clinical setting: An explorative study. Mindfulness. 2018 doi: 10.1007/s12671-018-1021-1. [DOI] [Google Scholar]
- Potharst ES, Zeegers M, Bögels SM. Mindful with your toddler group training: Feasibility, acceptability, and effects on subjective and objective measures. Mindfulness. 2018 doi: 10.1007/s12671-018-1073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racey DN, Fox J, Berry VL, Blockley KV, Longridge RA, Simmons JL, Janssens A, Kuyken W, Ford TJ. Mindfulness-based cognitive therapy for young people and their carers: A mixed-method feasibility study. Mindfulness. 2017 doi: 10.1007/s12671-017-0842-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raio CM, Orederu TA, Palazzolo L, Shurick AA, Phelps EA. Cognitive emotion regulation fails the stress test. PNAS Proceedings of the National Academy of Sciences of the United States of America. 2013;110:15139–15144. doi: 10.1073/pnas.1305706110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee, R.M. (2012). Anxiety disorders in children and adolescents: Nature, development, treatment and prevention. In J.M. Rey (Ed.), IACAPAP e-Textbook of Child and Adolescent Mental Health. Retrieved from https://iacapap.org/content/uploads/F.1-Anxiety-Disorders-2018-UPDATE.pdf
- Robinson M, Neece CL. Marital satisfaction, parental stress, and child behavior problems among parents of young children with developmental delays. Journal of Mental Health Research in Intellectual Disabilities. 2015;8:23–46. doi: 10.1080/19315864.2014.994247. [DOI] [Google Scholar]
- Rodriguez CM. Association between independent reports of maternal parenting stress and children’s internalizing symptomatology. Journal of Child and Family Studies. 2011;20:631–639. doi: 10.1007/s10826-010-9438-8. [DOI] [Google Scholar]
- Rousseau S, Scharf M. Why people helicopter parent? An actor–partner interdependence study of maternal and paternal prevention/promotion focus and interpersonal/self-regret. Journal of Social and Personal Relationships. 2017;35:919–935. doi: 10.1177/0265407517700514. [DOI] [Google Scholar]
- Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2013). Mindfulness-based cognitive therapy for depression (2nd ed.). The Guilford Press.
- Settipani CA, Kendall PA. The effect of child distress on accommodation of anxiety: Relations with maternal beliefs, empathy, and anxiety. Journal of Clinical Child & Adolescent Psychology. 2017;46:810–823. doi: 10.1080/15374416.2015.1094741. [DOI] [PubMed] [Google Scholar]
- Skreden M, Skari H, Malt UF, Pripp AH, Bjӧrk MD, Faugli A, Emblem R. Parenting stress and emotional wellbeing in mothers and fathers of preschool children. Scandinavian Journal of Public Health. 2012;40:596–604. doi: 10.1177/1403494812460367. [DOI] [PubMed] [Google Scholar]
- Smith AM, Jensen-Doss A. Youth psychotherapy outcomes in usual care and predictors of outcome group membership. Psychological Services. 2017;14:66–76. doi: 10.1037/ser0000115. [DOI] [PubMed] [Google Scholar]
- Stern JA, Borelli JL, Smiley PA. Assessing parental empathy: A role for empathy in child attachment. Attachment and Human Development. 2015;17:1–22. doi: 10.1080/14616734.2014.969749. [DOI] [PubMed] [Google Scholar]
- Stone LL, Mares SHW, Otten R, Engels RCME, Janssens JMAM. The co-development of parenting stress and childhood internalizing and externalizing problems. Journal of Psychopathology and Behavioral Assessment. 2016;38:76–86. doi: 10.1007/s10862-015-9500-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suveg C, Shaffer A, Morelen D, Thomassin K. Links between maternal and child psychopathology symptoms: Mediation through child emotion regulation and moderation through maternal behavior. Child Psychiatry and Human Development. 2011;42:507–520. doi: 10.1007/s10578-011-0223-8. [DOI] [PubMed] [Google Scholar]
- Swan AJ, Kendall PC. Fear and missing out: Youth anxiety and functional outcomes. Clinical Psychology Science and Practice. 2016;23:417–435. doi: 10.1111/cpsp.12169. [DOI] [Google Scholar]
- Tiwari S, Podell JC, Martin ED, Mychailyszyn MP, Furr JM, Kendall PC. Experiential avoidance in the parenting of anxious youth: Theory, research, and future directions. Cognition and Emotion. 2008;22:480–496. doi: 10.1080/02699930801886599. [DOI] [Google Scholar]
- Van Steensel FJ, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review. 2011;14:302–17. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venta A, Velez L, Lau J. The role of parental depressive symptoms in predicting dysfunctional discipline among parents at high-risk for child maltreatment. Journal of Child and Family Studies. 2016;25:3076–3082. doi: 10.1007/s10826-016-0473-y. [DOI] [Google Scholar]
- Wald N, Carthy T, Shenaar-Golan V, Tadmor-Zisman Y, Ziskind M. Influence of maternal negative emotion reactivity and cognitive reappraisal on child anxiety disorder. Depression and Anxiety. 2018;35:353–359. doi: 10.1002/da.22745. [DOI] [PubMed] [Google Scholar]
- Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43:374–385. doi: 10.1016/j.jrp.2008.12.008. [DOI] [Google Scholar]
- Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: A systematic review. Journal of Medical Internet Research. 2017;19:e290. doi: 10.2196/jmir.7071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Statistical Methods in Medical Research. 2016;25:1057–1073. doi: 10.1177/0962280215588241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willner CJ, Gatze-Kopp LM, Bray BC. The dynamics of internalizing and externalizing comorbidity across the early school years. Developmental Psychopathology. 2016;28:1033–1052. doi: 10.1017/S0954579416000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolk CB, Caporino NE, McQuarrie S, Settipani CA, Podell JL, Crawley S, Beidas RS, Kendall PC. Parental Attitudes, Beliefs, and Understanding of Anxiety (PABUA): Development and psychometric properties of a measure. Journal of Anxiety Disorders. 2016;39:71–78. doi: 10.1016/j.janxdis.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap MBH, Pilkington PD, Ryan SM, Jorm AF. Parental factors associated with childhood anxiety, depression and internalizing problems: A systematic review and meta-analysis. Journal of Affective Disorders. 2014;175:424–440. doi: 10.1016/j.jad.2015.01.050. [DOI] [PubMed] [Google Scholar]
- Zahra D, Hedge C. The Reliable Change Index: Why isn’t it more popular in academic psychology? PsyPAG Quarterly. 2010;76:14–19. [Google Scholar]