Abstract
Spindle cell hemangioma is a rare benign hemangioma. It is mainly found as small soft tissue nodules in the distal extremities, especially in the hands. The manifestation in bone is extremely rare. We present a case of spindle cell hemangioma of bone in the frontal bone. We also reviewed the literature to find the common imaging findings of intraosseous hamangiomas. The main manifestations of X-ray and CT were osteolytic lesions with soap bubble-like changes, and soft tissue mass formation. Magnetic resonance imaging mainly showed a lobulated mass with clear boundary, uneven hyperintense on T2WI, and obvious enhancement on contrast-enhanced scan. Surgical excision is curative. While this lesion is rare, it can be considered in the differential diagnosis if the characteristic imaging features are present.
Keywords: Spindle cell hemangioma, Frontal bone, Vascular tumor, Magnetic resonance imaging
Abbreviations: SCH, Spindle cell hemangioma; MRI, Magnetic resonance imaging; T1WI, T1-weighted images; T2WI, T2-weighted images; CT, Computed tomography
Introduction
Spindle cell hemangioma (SCH) is an uncommon benign tumor. It is characterized by a combination of cavernous spaces and solid areas of spindle cells and epithelioid cells [1]. Since its first description by Weiss and Enzinger as a rare type of hemangioma in 1986 [1], only a few reports have been published on intraosseous spindle cell hemangioma in the relevant English medical literature, and 1 case arises in the calcaneus [2], 1 case arises in the periosteal of the fibula [3], 1 case arises in the sacrum [4], 1 case arises in the frontal bone [5].
Herein, we reported a case with spindle cell hemangioma originating of the frontal bone.
Case report
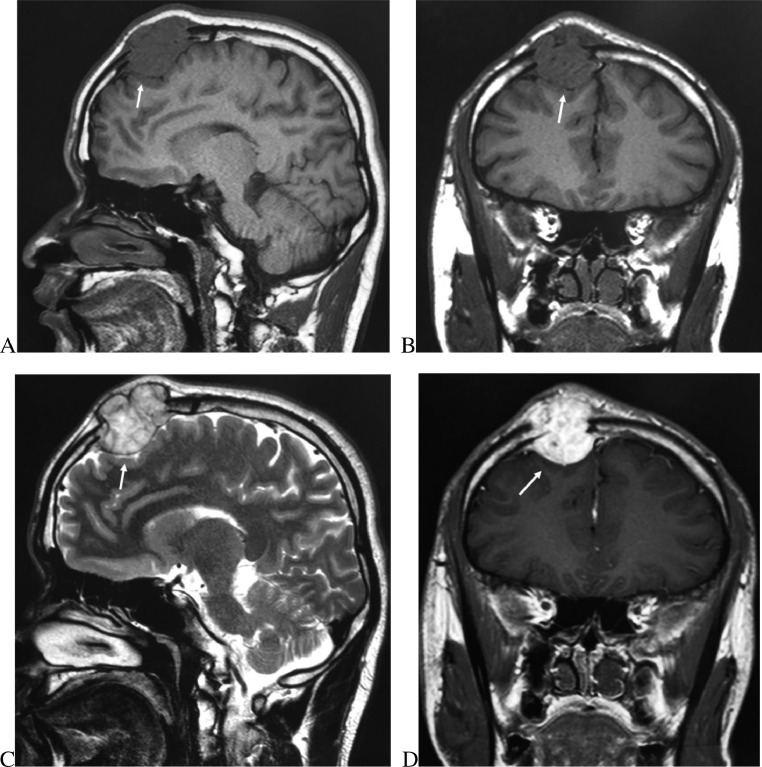
A 50-year-old man presented with a 2-month history of a painless mass in the right side of the frontal bone. Physical examination revealed a mass in the frontal, which measured approximately 4.0 × 3.5 cm, was circumscribed, soft, non-mobile, and non-tender. Laboratory data and neurologic examinations were unremarkable. Plain radiography showed that there was a large circumscribe radiolucent lesion in the right of the frontal. There was no adjacent soft tissue swelling. (Fig. 1A). CT scan of the head showed a lytic lesion in the frontal bone, with a soap bubble appearance, cortical destruction, and associated soft tissue component. (Fig. 1B-C). Contrast-enhanced MRI revealed a lobulated mass in the frontal bone, measuring 3.7 × 3.3 × 2.8 cm. The lesion was hypointense on the T1-weighted images, hyperintense on the T2-weighted images, and demonstrated avid enhancement on the postcontrast sequences. (Fig. 2A-D).
Fig 1.
A-C, X-ray and CT examination of tumor (white arrow). A, X-ray showed local bone resorption and decreased density of the frontal bone. B-C, CT showed osteolytic destruction of frontal bone and formation of soft tissue mass with local soap bubble-like changes and continuous interruption of bone in the inner and outer plate.
Fig 2.
A-C, MRI examination of tumor (white arrow). A and C, Sagittal, Coronal T1WI and T2WI showed lobulated mass of frontal bone with clear boundary, hypointensity on T1WI and uneven hyperintensity on T2WI. C, Coronal enhanced T1WI showed inhomogeneous and obvious enhancement of the lesions.
(MRI = magnetic resonance imaging, T1WI = T1-weighted images, and T2WI = T2-weighted images).
Surgery and pathology
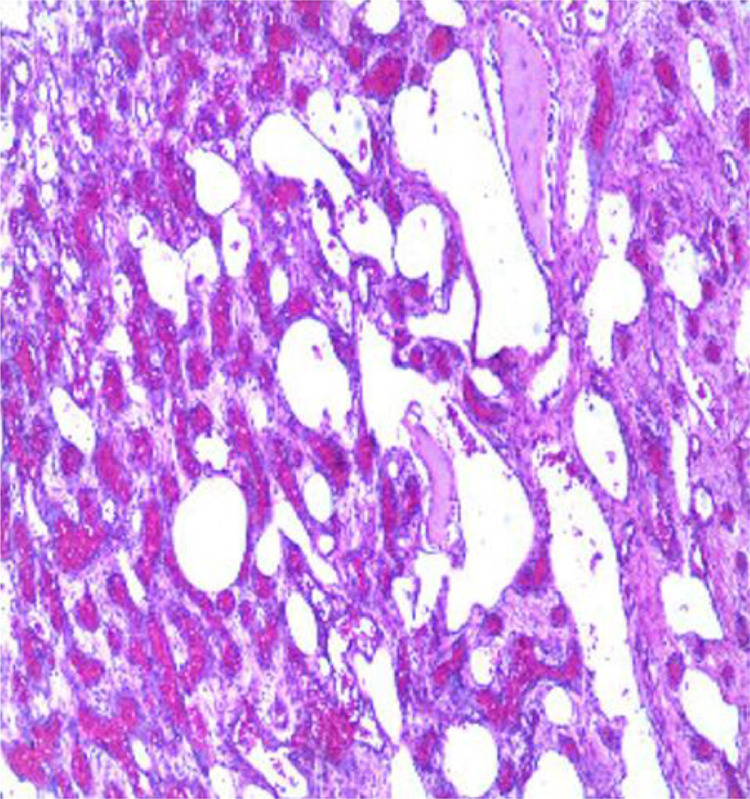
An operation was performed that the lesion was excised. Histologic examination of the obtained mass revealed Spindle cell hemangioma composed of dilated vascular spaces and a proliferation of bland appearing interspersed spindle cells (Fig. 3). Immunohistochemical analysis was diffusely positive for CD31, Action, Vimentin and focally for CD34, that they were consistent with spindle cell hemangioma
Fig 3.
Histological examination of spindle cell hemangioma. The HE staining result showed tumor cells showed spindle cell hemangioma composed of dilated vascular spaces and a proliferation of bland appearing interspersed spindle cells.
Postoperative course
The post-operative course was uneventful. Follow-up imaging revealed no evidence of recurrence. Because the tumor is benign, there's no need to state that chemotherapy or radiation weren't given!
Discussion
Spindle cell hemangioma, which is characterized by a combination of cavernous spaces and solid areas of spindle cells and epithelioid cells is an uncommon vascular lesion that was first described in 1986[1]. This entity was originally believed to be a tumor with limited metastatic potential, but now it is regarded as a benign vascular lesion and not a low-grade angiosarcoma [6]. While the course is benign, the lesion tends to recur [7]. It generally occurs as cutaneous or subcutaneous nodules in young adults and typically arises in the subcutis of the distal extremities, particularly the hand. Spindle cell hemangioma of bone is more common in women, the incidence in women is 2 ∼ 3 times higher than that in men, and can occur at any age, but middle-aged patients are the most common, and the peak age of onset is about 40 years old. There are no specific symptoms in the clinic. Combined with the literature cases, there were 5 patients, 1 male and 4 female, aged from 35 to 65 years old, with an average age of 46 years old.
About their image performance is rarely reported based on our extensive search of the English-language literature. Imaging studies on spindle cell hemangiomas of bone have rarely been described, and only four previous reports have included imaging findings of spindle cell hemangiomas of bone [2], [3], [4] (Table 1). The lesion can look aggressive, with osseous destruction and a soft tissue component. The lesions are typically hypointense on T1-weighted imaging, heterogenous on T2-weighted imaging, and demonstrate enhancement on post-contrast sequences. The imaging differential diagnosis of spindle cell hemangioma in the frontal bone includes eosinophilic granuloma and metastatic tumors. The eosinophilic granuloma of the skull, which usually occurs in male children, shows osteolytic destruction of the skull, penetrates the internal and external plate of the skull, and the "button-like" dead bone can be seen inside. there is no sclerotic edge around the focus, the edge is smooth, and the shape of the soft tissue mass is regular. The edge is smooth. Skull metastases, mostly in elderly patients, have a history of primary tumor, osteolytic bone destruction, and there are no residual bone fragments inside.
Table 1.
Clinical and imaging data for intraosseous spindle cell hemangioma in bone.
| Author | Age (years)/gender | Location | Sings,symtoms and size | Imaging apperance | Treatment | Recurrence | Follow-up(months) |
|---|---|---|---|---|---|---|---|
| Andrea Winter,B.A. et al [4] | 31/F | Sacrum | Low-back and left lower-extremity pain in the S-1 distribution without weakness or bowel or bladder dysfunction. This lesion were 3.7×7.6cm in anteroposterior and transverse dimensions |
A large osteolytic sacral lesion extending from S-1 to S-3, hypointense on T1- and mildly hyperintense on T2-weighted images, and avidly enhancing on the postcontrast T1-weighted images. | Embolization and excision | No | 9 |
| Shinji Tsukamoto et al [3] | 49/F | Periosteal of fibula | Pain and swelling, no pain at rest, but felt pain during and after exercise. A fixed,very firm, tender mass of about 5cm. |
Plain radiography showed that there was a large circumscribed radiolucent lesion on the surface of the fibula with a loculated soap bubble appearance. CT revealed a surface lesion with cortical destruction and periosteal. MRI revealed a lobulated tumor on the surface of the bone, homogenous intermediate intensity on T1, nonhomogenous high intensity on T2,a diffuse enhancement of tumor matrix with Gd-DTPA on T1-weighted fat-suppression imaging. | Excision | No | 10 |
| Michiyuki Hakozaki et al [2] | 65/F | Calcaneus | Pain, the pain on weight bearing and did not pain on rest. This esion were 4.6 × 3.1 × 2.8 cm. | Plain radiography revealed an osteolytic lesion with soap bubble–like multilocular appearance and a thinned lateral cortical bone in the left calcaneus. MRI revealed an intraosseous tumor in the left calcaneus,low intensity on T1,high intensity with mixed low and intermediate intensity on T2,marginal enhancement on gadoliniumenhanced, T1-weighted fat-suppression imaging. |
At 21 months after the biopsy, curettage of the tumor with argon beam coagulator treatment and an autogenous iliac bone graft with β-tricalcium phosphate. |
NO | 18 |
| Wu Jun et al [5] | 35/F | Frontal bone | Right frontal mass, 3.0×2.0cm. | CT showed the right frontal bone lesions from the plate was flat outward expansion of the defect, the edge clear, the density decreased, the inner plate is not continuous | Excision | NO | 12 |
M = male, F = female, MRI=magnetic resonance imaging, CT=computer tomography.
Pathologically, spindle cell hemangioma is characterized by cavernous vessels and fusiform areas [8]. The cells are dark pink in HE staining, with plump nuclei and clear nucleoli. Immunohistochemical CD31 (and factor VIII or CD34) were positive.
Surgical treatment is the first choice and effective treatment for SCH. Although SCH is considered to be a benign disease, it has been reported that there may be recurrence after operation, and it may also involve the whole limb. However, no recurrence or other progression was found in this case after follow-up for 5 years. In the retrospective literature, 4 cases were followed up, the follow-up period ranged from 9 months to 18 months, and no signs of recurrence or progression were found during the follow-up period.
Conclusion
we have described a rare case of intraosseous SCH of the frontal bone, despite its rarity, this lesion should be included in the differential diagnosis of primary bone tumor or imaging, especially if it is an osteolytic lesion with a loculated soap bubble appearance, and have an obvious enhancement on postcontrast. The diagnosis still needs to be combined with a pathological examination.
Patient consent
Written informed consent was obtained from his guardian for publication of this report.
Competing Interests
The authors report no conflict of interest concerning the materials or methods used in this study, or related to the findings specified in this paper.
References
- 1.Weiss SW, Enzinger FM. Spindle cell hemangioendothelioma: A low grade angiosarcoma resembling a cavernous hemangioma and Kaposi's sarcoma. Am J Surg Pathol. 1986;10:521–530. [PubMed] [Google Scholar]
- 2.Hakozaki M, Tajino T, Watanabe K, et al. Intraosseous spindle cell hemangioma of the calcaneus: a case report and review of the literature. Ann Diagn Pathol. 2012;16:369–373. doi: 10.1016/j.anndiagpath.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Tsukamoto S, Honoki K, Shimada K, et al. Periosteal spindle cell hemangioma of the fibula: a case report. Skeletal Radiol. 2013;42:1165–1168. doi: 10.1007/s00256-013-1603-x. [DOI] [PubMed] [Google Scholar]
- 4.Winter A, Siu A, Jamshidi A, Malawer M, et al. Spindle cell hemangioendothelioma of the sacrum: case report. J Neurosurg Spine. 2014;21:275–278. doi: 10.3171/2014.3.SPINE13651. [DOI] [PubMed] [Google Scholar]
- 5.Jun Wu, You Zhou, Jun Fan, et al. Skull spindle cell hemangioma: case report. Chin J Neurosurg Dis Res. 2011;10:280–281. [Google Scholar]
- 6.Ding J, Hashimoto H, Imayama S, Tsuneyashi M, Enjoje M. Spindle cell hemangioendothelioma: probably a benign vascular lesion, not a low grade angiosarcoma. A clinicopathological, ultrastructural and immunohistochemical study. Virchows Arch A Pathol Anat Histopathol. 1992;420:77–88. doi: 10.1007/BF01605988. [DOI] [PubMed] [Google Scholar]
- 7.Chung DH, Keum JS, Lee GK, et al. Spindle cell hemangioendothelioma. J Korean Med Sci. 1995;10 doi: 10.3346/jkms.1995.10.3.211. 211S–215S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiss SW, Goldblum JR. In: Enzinger and Weiss's soft tissue tumors. 5th ed. Weiss SW, Goldblum JR, editors. Mosby/Elsevier; Philadelphia, PA: 2008. Spindle cell hemangioma; pp. 655–658. [Google Scholar]