Abstract
Introduction and importance
Ano-genital warts are rare presentation in children. The main route of transmission is by sexual intercourse however horizontal transmission, self-inoculation and vertical transmission are also documented. Establishing the route of transmission when there is no evidence of sexual abuse may be difficult in pediatric and female virgins such as in our case report. Surgical excision remains one of the best options for treatment of large warts in pediatrics. To the best of our knowledge, this is the first report of novel case of large genital warts in pediatrics in Tanzania.
Case presentation
We present a case of female child of one year and 10 months old with large ano-genital cauli-flower masses admitted at Kilimanjaro Christian Medical Centre. The child's hymen was intact and with no evidence of sexual abuse identified. The masses were excised under general anesthesia and histology confirmed Condyloma acuminata.
Clinical discussion
Ano-genital warts are rare presentation in pediatrics and female virgins. Sexual abuse should be ruled out in pediatrics patients. Self-inoculation is described as a possible route of transmission in pediatrics and in female virgins. Horizontal and vertical transmissions are also possible route of transmission of HPV. It might be difficult to establish the route of transmission as in our case report. The warts were successful treated by surgical excision and cauterization.
Conclusion
Condyloma acuminata are rare in pediatrics and establishing the route of transmission may be difficult. Sexual abuse should be ruled out in pediatrics.
Keywords: Anogenital warts, Human papilloma virus, Children, Tanzania
Highlights
-
•
Large genital warts are uncommon to the pediatric population.
-
•
If encountered in children, sexual assault/abuse should be ruled out.
-
•
The exact route of transmission in pediatrics without sexual abuse and female virgins may be difficult to establish.
-
•
HPV can be transmitted through horizontal and self-inoculation.
-
•
Surgical excision and electro-cauterization are effective treatment for pediatric genital warts
1. Introduction and importance
Ano-genital warts also known as Condyloma acuminata are caused by human papilloma virus (HPV) infection, typically 6 and 11 genotypes [1]. The disease is highly contagious and is considered to be sexually transmitted in adults, but this may not be the case in pediatrics where horizontal, vertical and self-inoculation routes of transmission have been reported [1]. This is a rare condition in pediatrics globally including Tanzania; however, the prevalence is on the rise due to the increase in HPV infection in adults [1].
Here, we report a case of one-year and ten-month old female child who presented with ano-genital warts. The child had intact hymen with no evidence of sexual abuse as observed from examination under anesthesia. The mother was also examined in order to determine the route of transmission, but no warts were found. Hence the exact route of transmission could not be established however horizontal or self- inoculation transmissions are suspected in our case report. The warts were treated successfully by surgical excision.
This work has been reported in line with the SCARE 2020 criteria [2].
2. Case presentation
A one-year and ten-month female child was brought to our Centre accompanied by her mother and channeled to urology department. The mother reported that she noticed abnormal “flesh-like” skin lesions on her child's vulva for past two-months which was gradually progressing in size. However, the color was normal, not discharging, not painful, passing urine well and not causing any sort of discomfort to the child. The child was seen at nearby health facility where topical silver nitrate was applied with no relief for about 1 month.
The child was delivered at a local health centre by spontaneous vaginal delivery (SVD) at term, weighing 3.6 kg. Antenatal, the mother booked at four months of gestation and visited antenatal clinic five times. She received all supplements as per protocol. She tested negative for HIV and VDRL was non-reactive. She was normotensive throughout her antenatal clinic visits with no skin or vulva lesions during delivery. The child also received all vaccines according to the Tanzanian guidelines. The child is the third borne in a family of 3 children. The mother is a housewife and the farther is a mechanic. All siblings are well with no similar conditions reported. However, we could not access other family members for physical examination to identify possible source of infection.
On general examination, the child was alert and clinically stable afebrile with no obvious skin lesions, not pale and not jaundiced. On local examination of her vulva, there was a large pink cauliflower-like interlabial mass, nontender with finger-like projections and two other small lesions, one on the mons pubis and the other one on the perianal area (Fig. 1). Laboratory works up were normal including VDRL and HIV test which were non-reactive and negative respectively.
Fig. 1.
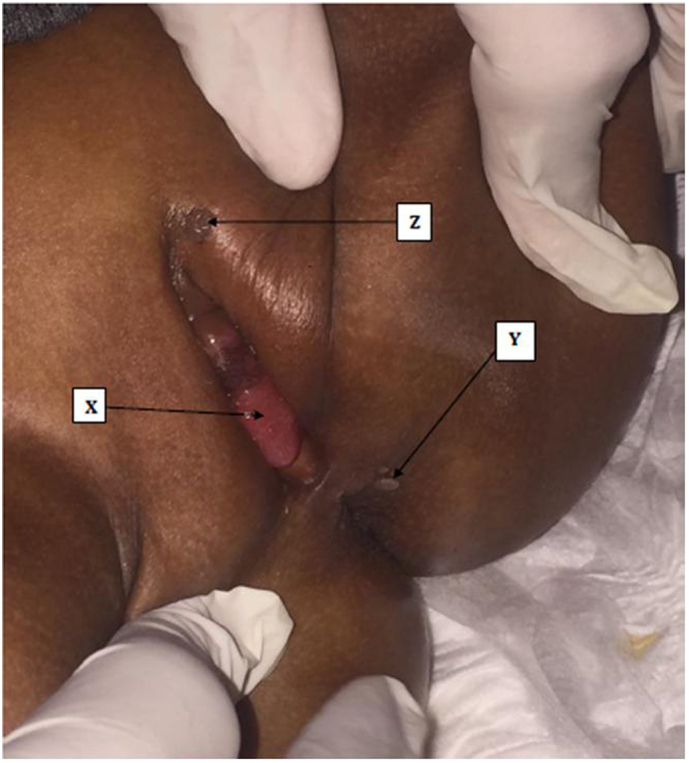
X, Y and Z shows warts on interlabial, perianal and Mons's pubis area respectively.
The mother was counseled to have the child's warts surgically removed, and the child was sent to the urology theatre for the procedure. Upon examination under general anesthesia (EUA), she was noted to have large 4 by 4-centimeter Condylomatous mass between the labia, the mass was occupying almost the whole introitus (Fig. 2). The external urethral meatus could not be located. However, the labial major and minor were spared and the hymen was intact and no signs of sexual abuse such as pain, discoloration, bleeding or abnormal discharge per vagina, perineum or anal region (Fig. 3). There were also other two small lesions one on the perianal and the other one on the mons pubis area. The large interlabial mass was excised completely and submitted for histology analysis. The external urethral meatus was located after removal of the mass as it was attached on it and hence, meatoplasty was done. The other two small lesions were cauterized by diathermy. Urethrocystoscopy revealed the urethra and urinary bladder to be normal. Size 8 Fr Foley catheter was left in situ for three days, thereafter she was allowed home after having uneventful recovery (Figure3). She was reviewed as an outpatient two-months post operatively where she was noted to have good prognosis with no features of recurrence. Histopathology results confirmed ano-genital warts with positive P16 immunohistochemistry (IHC) (Fig. 4).
Fig. 2.
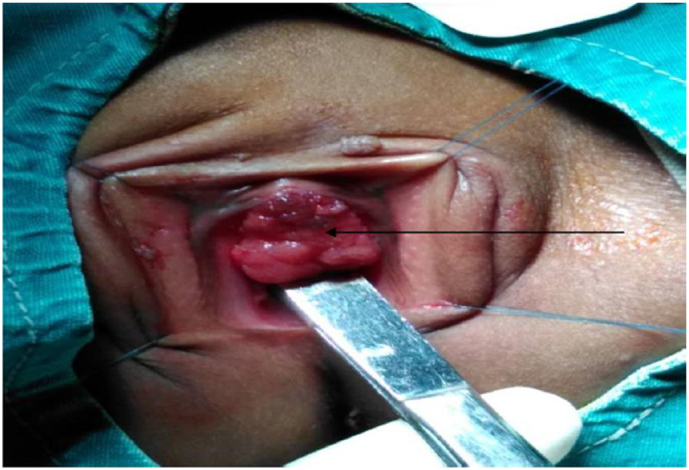
The arrow showing the large interlabial mass with nonvisualized external urethral meatus.
Fig. 3.
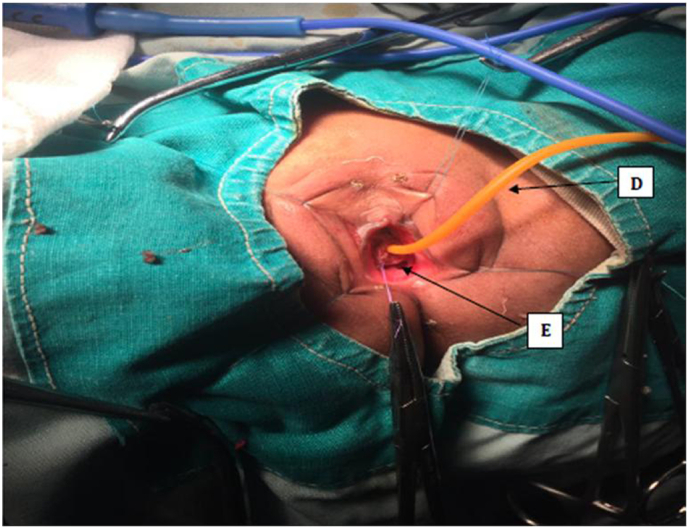
D shows the Foley catheter in situ and E shows the intact hymen.
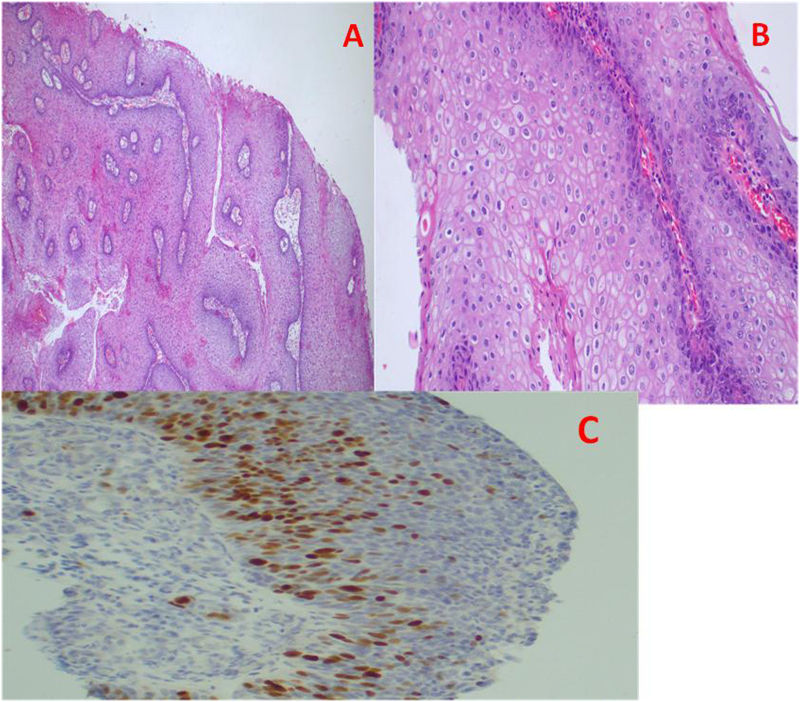
Fig. 4.
Histopathology of a genital warts demonstrating bulbous papillomatous acanthosis with exo-endophytic growth pattern; H & E-stained section, 4× original magnification (A); presence of gross HPV koilocytic cytopathic effects, H&E-stained sections 20× (B) and positive immunoreactivity with p16, IHC 20× original magnification (C).
3. Discussion
Condylomata acuminata are anogenital warts caused by HPV and there are over 200 genotypes of HPV, of which 30–40 specifically affect the genital tract [1]. They account for a number of diseases in the pediatric group, ranging from common warts, condylomata acuminata to the life-threatening respiratory papillomatosis [3]. Most commonly young adults who are sexually active are at higher risk. On the contrary, pediatric population is vertically transmitted from infected genital tract or through caretakers with hand warts [1]. However sexual abuse is a rather common cause of anogenital warts in children and should be ruled out with detailed history and physical examination for signs of abuse [1], [4]. In the index case, the mother denied history of warts during her pregnancy and there was no evidence of sexual abuse on clinical examination. Other mode of transmission can be horizontal which includes fomites, fingers, and mouth, skin contact (other than sexual). Self-inoculation is described as a potential mode of transmission in pediatrics and female virgins without history of sexual abuse [5]. It was difficult to establish the exact route of infection in our case report, however horizontal transmission or self -inoculation are suspected as possible route of transmission.
HPV is a non-enveloped, double-stranded DNA-virus that infects basal keratinocytes and mucosal epithelium, typically via small breaks in the skin. Most HPV infections are cleared by the host immune system within 7–9 months but can persist longer. HPV carries two oncogenes, E6 and E7, which aid in tumor growth and carcinogenesis [3]. These proteins bind and inactivate the tumor suppressor gene, p53 that prevents unregulated cell growth [3]. The first vaccine created to target HPV, the major cause of cervical cancer, was developed in the early 2000s that targeted four strains HPV-6, 11, 16 and 18. Recently in 2015, another vaccine was developed and covered strains HPV-31, 33, 45, 52 and 58 including the previously covered [3]. The vaccine cannot prevent this current age group of the infection but “eradication” can extinguish in this age group.
Diagnosis is usually clinical and confirmed by biopsy as reported by Elfaitoiki et al. in their case report and also done in our case [5]. The management is usually difficult in children due to the age and size of the lesions [5]. Treatment modalities include cryotherapy, laser therapy, electro-cauterization and surgical excision, of which all need local or general anesthesia [5]. The case reported here, was successfully treated by surgical excision and electro-cauterization under general anesthesia. Topical agent like podophylline can also be used on its own or in conjunction with surgical excision as reported by Hajaratu et al. [6]. The authors also state that lesions of Chondylomata acuminata are rare in children, and when they occur their management is usually surgery [6].
4. Conclusion
Condyloma acuminata are not only transmitted sexually but through non-sexual way. Vulval lesions are uncommon in children hence examinations should be thorough. Surgical management is associated with good outcome.
Condyloma acuminata is not only sexually transmitted but can also be transmitted non-sexually. For the reason that vulval lesions in children are less common, examinations should be comprehensive. Surgical treatment and electro-cauterization are linked to a positive outcome.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical standards were reviewed and approved by the Urology Department.
Consent
Written informed consent was obtained from the patient's mother for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors' contributions
-
▪
Jay Lodhia – conceptualization and writing of the script
-
▪
Alex Mremi – processing and reading of histology slides
-
▪
Oregeness Mbwambo – reviewed medical records and final editing of script
-
▪
Seif Mshangama – reviewed medical records
-
▪
Frank Bright – Supervising surgeon and review of medical records
-
▪
Bartholomeo Ngowi – Lead surgeon and writing of manuscript
Research registration
N/A.
Guarantor
Jay Lodhia – Corresponding author.
Declaration of competing interest
The authors declare they have no competing interests.
Acknowledgments
Acknowledgement
The authors would like to thank the child's mother for permission to share her child's medical history including clinical photographs for educational purposes and publication.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Me J., Ea D., N D, Ok Y., Na F. Condyloma acuminata in an infant: case report in a resource limited setting. Ann. Clin. Med. Case Rep. 2020;05(05) doi: 10.47829/acmcr.2020.5502. [DOI] [Google Scholar]
- 2.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAseREport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 3.Fuller C., Hudgins E., Finelt N. Human-papillomavirus-related disease in pediatrics. Curr. Opin. Pediatr. 2018;30(1):169–174. doi: 10.1097/mop.0000000000000561. [DOI] [PubMed] [Google Scholar]
- 4.Petekkaya S., Erkol Z., Hosukler E., Samurcu H., Gundogdu V., Buken B. Evaluation of genital condyloma accuminata seen during pediatric age as for sexual abuse: case report. Pediatr. Urol. Case Rep. 2018;5(2):47–51. doi: 10.14534/j-pucr.2018236888. [DOI] [Google Scholar]
- 5.Elfatoiki F., Hali F., Baghad B., Marnissi F., Chiheb S. Giant perianal condyloma acuminatum in an infant without sexual abuse. Arch. Pediatr. 2019;26(8):473–474. doi: 10.1016/j.arcped.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Sulayman H., Berde A., Ahmed S. Vulval warts in the paediatric age group: a report of three cases. J. Obstet. Gynaecol. India. 2015;66(1):57–59. doi: 10.1007/s13224-015-0676-y. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]