Abstract
Background
Polycystic ovary syndrome (PCOS) is a complex polygenic disease and is one of the most common endocrinological and reproductive disorders. The purpose of this study was to evaluate the efficacy of acupuncture combined with herbal medicine among infertile females with polycystic ovary syndrome (PCOS).
Method
A total of 86 women with PCOS, experiencing infertility, were recruited and randomly assigned to receive either manual acupuncture (MA) or sham acupuncture (SA) twice per week for three menstrual cycles. Both groups received herbal medication. The evaluations were conducted after three menstrual cycles and 24 weeks’ follow-up.
Results
The trial was completed by 79 (91.86%) of the 86 randomly selected patients. During this study, the pregnancy rate in the MA group (46.34%) was significantly higher than the SA group (18.42%), with a P-value of 0.008. Moreover, the ovulation rate of the MA group (58.14%) was higher than that of the SA group (45.74%), with a P-value of 0.046. The improvement rate of PCOS score and testosterone level showed a statistical difference between the two groups (P-values were <0.05). There were no other differences between the two groups. Sex hormones level, including E2, T, P, LH, and LH/FSH were significantly lower after intervention in the MA group (P-values were <0.05) compared with baseline, while only the progesterone level was reduced in the SA group (P-value = 0.008).
Conclusion
Manual acupuncture combined with herbal medicine may be clinically useful for infertile women with PCOS in improving pregnancy and ovulation rate.
Trial Registration
Chinese Clinical Trial Registry: ChiCTR1800014997.
Keywords: Polycystic ovary syndrome, Manual acupuncture, Chinese Herbal Medicine, Infertility
1. Introduction
Polycystic ovary syndrome (PCOS) is a complex polygenic disease and is one of the most common endocrinological and reproductive disorders,1, 2 threatening 10% of women of child-bearing age.3 It is characterized by biochemical hyperandrogenism, chronic anovulation, and the presence of polycystic ovaries,4 which cause more than 75% of ovulatory infertility.5 PCOS syndromes are linked with obesity, impaired glucose tolerance, excessive body hair, acne, menstrual cycle disturbances, infertility, and imbalance of hormones.6 PCOS is complicated by depression, anxiety, and various other complications. Furthermore, PCOS poses a health hazard to women of childbearing age.7, 8
Clomiphene citrate (CC) is the first-line treatment for ovulatory infertility in women with PCOS; metformin and letrozole are also used as commonly prescribed drugs.9, 10 Cumulative ovulation rates of CC are as high as 90%, with a pregnancy rate of about 50–70%.11 However, up to 40% of women who received clomiphene treatment revealed less clinical improvement,12 a relatively high multiple-pregnancy rate (about 3–8%), and side effects such as mood changes, hot flushes,13 dizziness, nausea, gastrointestinal symptoms, and symptoms associated with ovarian enlargement and ovulation,14 as well as birth defects.15 Acupuncture and traditional Chinese medicine (TCM) has a long history of using for gynecological diseases and fertility issues such as those associated with PCOS, a multitude of studies have revealed that a wide spectrum of herbs could be used in the treatment of clinical and laboratory symptoms of PCOS, however, review of previous studies showed their effectiveness was not certain.16, 17 While in China, Chinese herbal remedies are widely accepted. Infertility patients have an urgent desire for treatment. Given these facts, herbal medicine is administered to all groups as basic treatment. The present study aimed to assess the efficacy of acupuncture combined with herbal medicine on ovulation and pregnancy rates, and the levels of hormones associated with infertility in women with PCOS.
2. Methods
2.1. Study design
A randomized, sham-controlled study was conducted in the outpatient clinics of Shuguang Hospital in Shanghai, China, between March 2018 and December 2019. The protocol was published and is available in the Supplement.18 This study was registered on February 27, 2018, in the Chinese Clinical Trial Registry (ChiCTR1800014997). https://www.chictr.org.cn/showproj.aspx?proj=25583.
2.2. Patients
The Rotterdam criteria, proposed in 2003, define the diagnostic criteria for both infertility and PCOS. Eligible women were between the ages of 20 and 40.4 In addition, the husband's semen examination results had to be normal.
Women with any of the following conditions were excluded: hyperprolactinemia, adrenal or ovarian tumors, thyroid disease, Cushing syndrome, and other heart and kidney diseases; oral contraceptives and hormonal drugs during the first month and other types of infertility; history of receiving acupuncture/moxibustion treatment within 2 months; use of other drugs that could affect the reproductive function or metabolism; participation in another clinical study in the past two months.
2.3. Randomization and blinding
A total of 86 eligible participants were recruited and randomly assigned to receive either MA or SA therapy in a 1:1 ratio. We generated the randomized sequence using Excel. The concealment of the allocation was secured by the use of an envelope. The assignment records were kept hidden until the completion of the study, and the envelopes were sealed. We registered the participants, and randomly assigned them to the different therapies. After being assigned to interventions, the patients were blinded. Acupuncturists could not be blinded to the treatment assignments given the nature of the interventions. Communication among participants was discouraged and avoided as they were treated separately in a separate room. Therefore, in this trial, participants, outcome assessors, data collectors, and statisticians were blinded to the treatment allocation.
2.4. Interventions
Both groups were treated with real herbal medicine twice a day. Patients were given the Taohong Siwu decoction orally during their menstrual period. Treatment for non-menstrual periods was based on syndrome differentiation; for spleen-kidney yang deficiency, Bushen Tiaojing decoction was used, and for liver-kidney deficiency, Guishao Dihuang decoction was used. Following training, two acupuncturists with more than three years of clinical experience were in charge of manipulating MA and SA. Sterile, disposable acupuncture needles (0.25×40 mm, Wuxi Jiajian Medical Instrument Co. Ltd., China), blunt-tip needles (0.25×25 mm, Wuxi Jiajian Medical Instrument Co., Ltd., China), and simple adhesive pads (for fixation) were used. Three menstrual cycles of acupuncture treatment (twice weekly) and Chinese herbal medicine were administered to participants (twice a day). The treatments in both groups started from the third day of menstruation to the third day after ovulation for three menstrual cycles. Treatments were stopped once the patient was pregnant.18 They received acupuncture on obligatory points, including RN4 (Guanyuan), bilateral EX-CA1 (Zigong), ST29 (Guilai), ST36 (Zusanli), and SP6 (Sanyinjiao). The remaining points were selected based on the syndrome differentiation and the menstrual cycle. The potential acupoints include RN6 (Qihai), RN12 (Zhongwan), DU20 (Baihui), and bilateral ST25 (Tianshu), KI3 (Taixi), KI6 (Zhaohai), LR3 (Taichong), SP10 (Xuehai), and PC6 (Neiguan). Each patient was selected for no more than 13 points. It was prohibited to use acupoints other than those prescribed. The semistandard prescriptions were based on clinical experience and the textbook "Acupuncture and Moxibustion".19 The participant was not treated further after pregnancy.
After sterilizing, adhesive pads adhered to acupoints during acupuncture therapy. Needles were inserted into the acupoints via the pad and 10 to 30 mm into the skin (depending on location) and then manipulated manually using techniques such as twisting, lifting, and thrusting to produce the " deqi " sensation (a sensation of soreness, numbness, distention, or sense of radiation, etc.) or needling sensation once every ten minutes for half-hour.20 The treatment procedure (selected acupoints and time of therapy) was identical in the SA group and the MA group except that they did not achieve deqi sensation.18
2.5. Outcome measures
Participants were assessed at baseline, each menstrual cycle, after three menstrual cycles of treatment, and at 24-week follow-up after the completion of the treatment. The primary outcome was the pregnancy rate during the trial. B-ultrasound confirmed the patient's pregnancy or HCG positivity in their blood or urine. The secondary outcomes included the ovulation rate observed through basal body temperature (BBT) or B ultrasound every menstrual cycle; change from baseline in PCOS and TCM syndrome scores (scoring was additive with higher values indicating increased severity); and change from baseline of the serum sex hormone levels included estradiol (E2), testosterone (T), progesterone (P), luteinizing hormone (LH), and follicle-stimulating hormone (FSH). In addition, the insulin resistance index (HOMA-IR = fasting blood glucose × fasting insulin/22.5) was assessed at baseline and after treatment of three menstrual cycles. A telephone follow-up was conducted 24 weeks following the completion of the treatment to see if the participants were pregnant. At each treatment session, acupuncture-related adverse events were recorded and reported to the study coordinators.
2.6. Ethical considerations
The ethics committee has been approved by the Institutional Review Board of Shuguang Hospital affiliated with Shanghai University of TCM (22 Dec 2017, Approval Number: 2017-569-52-01). Because of receiving a thorough explanation of the trial's protocols and the possibility of their clinical results being published, each participant willingly signed an informed consent form. The protocol was approved by the Shuguang Hospital's institutional ethics review board and was carried out in compliance with the Declaration of Helsinki.
2.7. Sample size calculation
The purpose of the study was to see whether there was a difference in the pregnancy rate between the MA and the SA groups.21, 22 We hypothesized that the pregnancy rate would be 76% in the MA group and 40% in the SA group. Assuming a two-sided alpha of 0.05, power of 90%, and a 20% drop-out rate, a sample size of 36 would be needed for each group to detect a difference between them. To increase the reliability of the study, we expanded the sample size to 86 cases (43 cases per group).
2.8. Statistical analysis
SPSS software (version 21.0, International Business Machines Corporation, China) was used for statistical evaluations. An intention-to-treat population, which includes participants who received at least one treatment and one primary outcome measure, was used for statistical analysis (n = 79). Continuous data were shown as mean and standard deviation (x ®±s) if normally distributed, or median (interquartile range, IQR) if abnormally distributed. Categorical variables were expressed as numbers and percentages. Continuous data were compared using Wilcoxon rank-sum tests or 2 sample t-tests, while categorical variables were compared using chi-square testing. A variance analysis was performed to evaluate the variations between the two groups and within each group. P-value = 0.05 (two-sided) was considered statistically significant.
3. Results
3.1. Participants and baseline characteristics
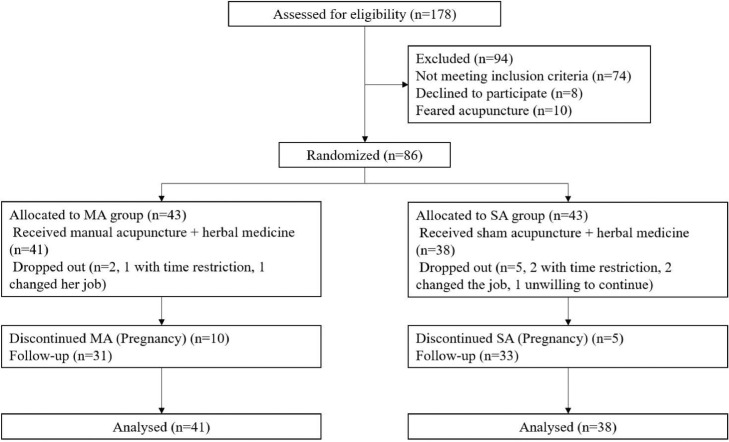
A total of 178 people were contacted to participate in the study, with 92 being excluded and 86 being eligible and randomly assigned to either the MA or SA group. Among those excluded, 74 did not match the inclusion criteria, 8 expressed a strong desire to conceive and declined to participate in the research, and 10 expressed fear of acupuncture therapy. In the MA group, two members left (1 case changed her job and 1 case had time inconvenience). In the SA group, five members left (2 cases changed jobs, 2 cases had time inconvenience, and 1 case unwilling to follow up). The study was completed by 79 individuals (91.86%), as represented in Fig. 1.
Fig. 1.
Baseline and clinical characteristics of the study paticipants.
Baseline characteristics were similar between the groups (Table 1). No significant difference was found between the two groups in age, duration of illness, body mass index (BMI), PCOS score, TCM score, and serum sex hormone. Randomization ensured that patient characteristics were properly balanced.
Table 1.
Baseline and clinical characteristics of the study paticipants.
| Characteristic | MA group (n = 41) | SA group (n = 38) | p-value |
|---|---|---|---|
| Age, year† | 30.8 ± 3.5 | 29.7 ± 3.2 | 0.918 |
| Duration of illness, month† | 23.5 ± 12.2 | 22.0 ± 8.5 | 0.34 |
| BMI† | 18.8 ± 2.3 | 17.9 ± 2.1 | 0.611 |
| PCOS Scores† | 3.6 ± 1.6 | 3.7 ± 1.9 | 0.371 |
| TCM Scores† | 4.9 ± 2.4 | 4.7 ± 2.3 | 0.954 |
| Serum sex hormones level‡ | |||
| E2, pmol/L | 125.0 (103.5,169.5) | 163.3 (104.5,201.5) | 0.285 |
| T, nmol/L | 1.6 (1.2,2.0) | 1.4 (1.0,2.1) | 0.283 |
| P, nmol/L | 0.8 (0.5,1.0) | 0.9 (0.6,1.4) | 0.325 |
| FSH, IU/L | 5.4 (4.3,6.0) | 5.0 (4.3,6.1) | 0.765 |
| LH, IU/L | 6.1 (3.1,9.6) | 4.2 (2.5,7.0) | 0.116 |
MA group, manual acupuncture group; SA group, sham acupuncture group; BMI, body mass index, is the weight in kilograms divided by the square of the height in meters; PCOS, polycystic ovary syndrome; TCM, traditional Chinese medicine; E2, estradiol; T, total testosterone; P, progesterone; FSH, follicle-stimulating hormone; LH, luteinizing hormone;.
Mean (SD);.
Median (IQR).
3.2. Primary outcome
During treatment, 15 participants successfully conceived, including ten in the MA group and five in the SA group, as represented in Table 2. The pregnancy rate was 24.39% (10/41) in patients who received manual acupuncture combined with herbal medicine and 13.16% (5/38) in the sham acupuncture combined with herbal medicine group.
Table 2.
Comparison of pregnancy rates between the two groups.
| Groups | N | After treatment, n(%) | During follow-up, n (%) | Total, n (%) |
|---|---|---|---|---|
| MA group | 41 | 10 (24.39) | 9 (29.03) | 19 (46.34) |
| SA group | 38 | 5 (13.16) | 2 (6.06) | 7 (18.42) |
| p-value | – | 0.203 | 0.015 | 0.008 |
MA group, manual acupuncture group; SA group, sham acupuncture group.
A total of 11 individuals reported pregnancy during the 6-month follow-up period. There were 9 participants in the MA group with a pregnancy rate of 29.03% (9/31) and 2 in the sham acupuncture group with a pregnancy rate of 6.06% (2/33) (P-value = 0.015). The obtained results revealed that the MA group had a pregnancy rate of 46.34% (19/41), which was significantly higher than the SA group's rate of 18.42% (7/38) (P-value = 0.008).
3.3. Secondary outcomes
After three menstrual cycles of treatment, the MA group's ovulation rate was 58.14%, significantly higher than the SA group's ovulation rate i.e., 45.74%, as represented in Table 3 (P-value = 0.046). PCOS score and testosterone levels in the MA group had statistically greater improvements compared to the SA group (Table 4).
Table 3.
Comparison of ovulation rate between the two groups (number of times).
| Groups | Ovulation | No ovulation | Ovulation rate | p-value |
|---|---|---|---|---|
| MA group | 75 | 54 | 58.14% | 0.046 |
| SA group | 59 | 70 | 45.74% |
MA group, manual acupuncture group; SA group, sham acupuncture group.
Table 4.
Comparison of other secondary outcomes before and after treatment in the two groups (□x ± s) / [M (Q25, Q75)].
| Items | Groups | N | Baseline | After treatment | p-value (intra-group) | Index value reduction changeb (%) | p-value (between groups) |
|---|---|---|---|---|---|---|---|
| PCOS Score | MA group | 31 | 3.71±1.75 | 2 (0,3) | <0.001 | 60 (33.33,100) | 0.003 |
| SA group | 33 | 3.64±1.85 | 2 (1.5,3) | <0.001 | 33.33 (0,100) | ||
| TCM Score | MA group | 31 | 5.0±2.61 | 2 (1,3) | <0.001 | 60 (50,71.43) | 0.317 |
| SA group | 33 | 4.67±2.33 | 2 (1,3) | <0.001 | 60 (46.43,66.67) | ||
| E2(pmol/L) | MA group | 31 | 131 (107,167) | 119.33±52.31 | 0.009 | 18.29 (-2.9,42.8) | 0.131 |
| SA group | 33 | 161.48 (90.5,203) | 132 (77.5,187.5) | 0.513 | -6.9 (-18.44,34.48) | ||
| T(nmol/L) | MA group | 31 | 1.59 (1.32,2.03) | 1.15 (0.95,1.57) | <0.001 | 23.77±22.99 | 0.037 |
| SA group | 33 | 1.15 (0.95,2.08) | 1.14 (0.87,1.68) | 0.131 | 2.13 (-14.58,35.29) | ||
| P(nmol/L) | MA group | 31 | 0.8 (0.5,1.0) | 0.6 (0.4,0.79) | 0.023 | 20 (0,40) | 0.824 |
| SA group | 33 | 0.8 (0.59,1.33) | 0.6 (0.4,0.9) | 0.008 | 14.26±50.344 | ||
| FSH(IU/L) | MA group | 31 | 5.26±1.08 | 5.08±1.26 | 0.368 | 1.80±21.42 | 0.92 |
| SA group | 33 | 5.04 (4.27,6.23) | 5.02 (4.19,5.81) | 0.561 | 1.98 (-16.66,16.61) | ||
| LH(IU/L) | MA group | 31 | 6.89±4.01 | 3.94 (2.48,6.58) | 0.043 | 13.99 (-13.7,55.33) | 0.108 |
| SA group | 33 | 4.17 (2.50,6.83) | 4 (2.59,6.84) | 0.888 | 0 (-69,35.4) | ||
| LH/FSH | MA group | 31 | 1.35±0.75 | 0.82 (0.55,1.3) | 0.038 | 20.88(-17.02,39.78) | 0.149 |
| SA group | 33 | 0.84 (0.56,1.34) | 0.83 (0.62,1.30) | 0.728 | -0.17 (-47.18,33.42) | ||
| HOMA-IR | MA group | 31 | 2.06 (1.32,2.56) | 1.7 (1.18,2.7) | 0.753 | -2.62±40.53 | 0.736 |
| SA group | 33 | 1.69 (1.15,2.71) | 1.86 (1.22,3) | 0.845 | 0 (0,8.15) |
Index value reduction change = (After treatment–Baseline)/ Baseline ⅹ 100%.
MA group, manual acupuncture group; SA group, sham acupuncture group; PCOS, Polycystic Ovary Syndrome; TCM, Traditional Chinese Medicine; E2, estradiol; T, total testosterone; P, progesterone; FSH, follicle-stimulating hormone; LH, luteinizing hormone; HOMA-IR = fasting blood glucose x fasting insulin/22.
After completion of treatment, compared with baseline, patients in the MA group had statistically significant improvement in PCOS score, TCM score, E2, T, P, LH levels, and the ratio of luteinizing hormone to follicle-stimulating hormone, but no significant improvement in FSH level or HOMA-IR. Details are listed in Table 4. When compared to baseline, patients in the SA group demonstrated statistically significant improvements in PCOS, TCM, and progesterone levels. However, no significant variations were observed in the levels of other hormones (P-value >0.05).
3.4. Adverse events
Adverse events were recorded in the study, while neither group experienced any noticeable side effects (local hematoma, dizziness, or gastrointestinal pain due to acupuncture reactions). The needles used in the manual acupuncture group were relatively thin (0.25×40 mm), moreover, in the sham group the blunt tip needles were used with no skin penetration. Most of the acupuncture points were located on the abdomen where fat was abundant, and with even and gentle twirling, lifting, and thrusting to achieve the “DeQi” sensation.
4. Discussion
The current randomized sham-controlled trial revealed that in comparison with sham acupuncture (in combination with herbal medicine), manual acupuncture (in combination with herbal medicine) significantly improved pregnancy rate, ovulation rate, and quality of life in infertile women with PCOS. In addition, manual acupuncture provided some more benefits than sham acupuncture. The obtained data support acupuncture combined with herbal medicine as an effective infertility treatment in patients with PCOS.
Pregnancy is the ultimate evaluation indicator of infertility treatment. Herein, we found that manual acupuncture combined with Chinese herbal medicine (MA group) for three menstrual cycles improved pregnancy and ovulation rates more than the SA group, and had a long-lasting effect. Our findings showed consistency with the previously reported studies23, 24, 25 in which acupuncture has been demonstrated to improve menstrual frequency in women with PCOS, however, such RCTs are too limited to determine effectiveness of acupuncture for PCOS. A systematic review reported a promising effect of Bushen Huoxue herbal medicine on increasing pregnancy rates, although the quality of evidence was relatively low.26 Complementary and alternative medicine therapies, including TCM and acupuncture, are commonly used.27 In this trial, we selected the acupuncture points according to the literature.28, 29, 30 Furthermore, TCM places considerable emphasis on the differentiation and treatment of various syndromes as a key therapeutic principle. Treatment according to the phase of the menstrual cycle is also common in gynecological diseases. Acupuncture therapy is widely used as it is a non-invasive TCM therapy and has fewer side effects. Therefore, this trial also followed the therapeutic principle of syndrome differentiation to enhance the therapeutic effects of acupuncture combined with herbal medicine.
Systematic literature reviews indicate that authentic acupuncture may improve ovulation and menstruation rates when compared to no acupuncture.31, 32 The efficacy of acupuncture for PCOS is inconclusive due to insufficient overall evidence.33 A randomized controlled trial demonstrated that acupuncture failed to treat women with PCOS,34 which attracted wide attention and controversy.35, 36 In their study, clomiphene was used as basic treatment, whereas herbal medicine was used in this study, acupuncture treatment in both studies were similar. Patients received acupuncture treatment from the third day of menstruation to the third day of ovulation may avoid the risk of treatment during pregnancy.34 Acupuncture is an alternative traditional therapy in which specific points on the body are stimulated by inserting thin needles through the skin.37 Treatment efficacy may vary according to the treatment regimen, acupoint selection, manipulation, treatment duration, frequency, and acupuncturist qualification.38 Therefore, the underlined factors have been considered in the design of this trial study. The compliance of the participants in the trial was high (91.86%), maybe since these patients had a strong desire to get pregnant. No serious side effects were observed during the trial.
Peripheral blood examination showed that the manual acupuncture group could significantly reduce E2, T, P, LH levels, and LH/FSH ratio in infertile patients with PCOS. However, only a statistically significant decrease in P lever was observed in the SA group. Acupuncture may help patients with PCOS to overcome their hyperandrogenic state, resulting in increased ovulation and pregnancy rates. According to the reported studies, acupuncture can decrease the ratio of LH/FSH, T, LH, and BMI levels. Furthermore, it improves ovarian function, local microcirculation, and uterine wall environment in patients with PCOS, which is conducive to the implantation of fertile eggs, similar to Diane-35.39, 40 The reported studies have been revealed that oral contraceptives can effectively reduce the LH/FSH ratio and androgen levels, improve symptoms, and restore ovulation to some extent, and reduce endometrial hyperplasia.41
Infertile PCOS patients showed a tendency for the insulin resistance index improvement after acupuncture but with no significant difference compared with the sham group. Both groups have similar effects in improving TCM symptoms, which may be due to the role of Chinese herbal decoction. The improvement of clinical symptoms of manual acupuncture combined with herbal medicine is significantly better than that of the sham group. All participants reported pregnant in this study were naturally conceived, most of them received herbal medicine treatment during the 6-month follow-up period. As a result, we provide evidence that acupuncture is effective in the treatment of infertile PCOS patients.
The limitations of this study include its relatively small sample size, the lack of an assessment of the blinding efficacy, and a record of how many patients in the MA and SA groups reported achieving deqi. After treatment, participants who were confirmed to be pregnant refused to have their blood drawn again, so the sample size of blood indicators was relatively small. In this study, 79 participants (91.86%) completed the trial, the dropout rate was less than 10%, so the withdrawn participants who had failed to complete the whole treatment course were not included in statistics, it might affect the outcomes. Further, the single-center trial was likely to overestimate treatment effect.
In conclusion according to the obtained data, manual acupuncture of three menstrual cycles combined with herbal medicine increased the pregnancy rate and ovulation rate compared with sham acupuncture combined with herbal medicine among infertile women with PCOS. A larger sample of clinical trials is necessary to extensively explore the long-term efficacy and the underlying therapeutic mechanism of acupuncture.
Acknowledgments
We would like to thank all the patients, nurses, and professionals in Shuguang Hospital for their help and support.
CRediT authorship contribution statement
Wen Pan: Formal analysis, Data curation, Writing – original draft. Feng-xing Li: Data curation. Qiao Wang: Formal analysis, Data curation, Writing – original draft. Zou-qin Huang: Funding acquisition. Yu-ming Yan: Data curation. Ling Zhao: Conceptualization, Methodology, Writing – review & editing. Xue-yong Shen: Conceptualization, Methodology, Writing – review & editing.
Acknowledgments
Conflict of interest
The authors have no competing interests to declare.
Funding
This work was funded by the Pudong New Area Health Commission, Shanghai, China (Grant Code PDZY-2018–0610).
Ethical statement
This trial has been approved by the Institutional Review Board of Shuguang Hospital affiliated with Shanghai University of TCM (22 Dec 2017, Approval Number: 2017-569-52-01). All participants have signed written informed consent.
Data availability
The obtained data in the current study are available upon reasonable request from the corresponding authors.
Contributor Information
Ling Zhao, Email: zl2@shutcm.edu.cn.
Xue-yong Shen, Email: sxy1@shutcm.edu.cn.
References
- 1.Dumesic D.A., Oberfield S.E., Stener-Victorin E., Marshall J.C., Laven J.S., Legro R.S. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. 2015;36(5):487–525. doi: 10.1210/er.2015-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Norman R.J., Dewailly D., Legro R.S., Hickey T.E. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–697. doi: 10.1016/S0140-6736(07)61345-2. [DOI] [PubMed] [Google Scholar]
- 3.Yildiz B.O., Bozdag G., Yapici Z., Esinler I., Yarali H. Prevalence, phenotype and cardiometabolic risk of polycystic ovary syndrome under different diagnostic criteria. Hum Reprod. 2012;27(10):3067–3073. doi: 10.1093/humrep/des232. [DOI] [PubMed] [Google Scholar]
- 4.Rotterdam EA-SPcwg. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS) Hum Reprod. 2004;19(1):41–47. doi: 10.1093/humrep/deh098. [DOI] [PubMed] [Google Scholar]
- 5.Gorry A., White D.M., Franks S. Infertility in polycystic ovary syndrome: focus on low-dose gonadotropin treatment. Endocrine. 2006;30(1):27–33. doi: 10.1385/ENDO:30:1:27. [DOI] [PubMed] [Google Scholar]
- 6.Pasquali R., Gambineri A., Pagotto U. The impact of obesity on reproduction in women with polycystic ovary syndrome. BJOG. 2006;113(10):1148–1159. doi: 10.1111/j.1471-0528.2006.00990.x. [DOI] [PubMed] [Google Scholar]
- 7.Azizi Kutenaee M., Amirjani S., Asemi Z., et al. The impact of depression, self-esteem, and body image on sleep quality in patients with PCOS: a cross-sectional study. Sleep Breath. 2019 doi: 10.1007/s11325-019-01946-9. [DOI] [PubMed] [Google Scholar]
- 8.Bazarganipour F., Ziaei S., Montazeri A., Foroozanfard F., Kazemnejad A., Faghihzadeh S. Psychological investigation in patients with polycystic ovary syndrome. Health Qual Life Outcomes. 2013;11:141. doi: 10.1186/1477-7525-11-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Legro R.S., Chen G., Kunselman A.R., et al. Smoking in infertile women with polycystic ovary syndrome: baseline validation of self-report and effects on phenotype. Hum Reprod. 2014;29(12):2680–2686. doi: 10.1093/humrep/deu239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amer S.A., Smith J., Mahran A., Fox P., Fakis A. Double-blind randomized controlled trial of letrozole versus clomiphene citrate in subfertile women with polycystic ovarian syndrome. Hum Reprod. 2017;32(8):1631–1638. doi: 10.1093/humrep/dex227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thessaloniki EA-SPCWG. Consensus on infertility treatment related to polycystic ovary syndrome. Hum Reprod. 2008;23(3):462–477. doi: 10.1093/humrep/dem426. [DOI] [PubMed] [Google Scholar]
- 12.Brown J., Farquhar C., Beck J., Boothroyd C., Hughes E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Syst Rev. 2009;(4) doi: 10.1002/14651858.CD002249.pub4. [DOI] [PubMed] [Google Scholar]
- 13.Legro R.S., Brzyski R.G., Diamond M.P., et al. Letrozole versus clomiphene for infertility in the polycystic ovary syndrome. N Engl J Med. 2014;371(2):119–129. doi: 10.1056/NEJMoa1313517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J., Si Q., Li J. Therapeutic effects of metformin and clomiphene in combination with lifestyle intervention on infertility in women with obese polycystic ovary syndrome. Pak J Med Sci. 2017;33(1):8–12. doi: 10.12669/pjms.331.11764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reefhuis J., Honein M.A., Schieve L.A., Rasmussen S.A. Use of clomiphene citrate and birth defects, national birth defects prevention study, 1997-2005. Hum Reprod. 2011;26(2):451–457. doi: 10.1093/humrep/deq313. [DOI] [PubMed] [Google Scholar]
- 16.Run-Ming Y. The origin and development of chinese acupuncture and moxibustion. Anc Sci Life. 1985;4(4):224–228. [PMC free article] [PubMed] [Google Scholar]
- 17.Moini Jazani A., Nasimi Doost Azgomi H., Nasimi Doost Azgomi A., Nasimi Doost Azgomi R. A comprehensive review of clinical studies with herbal medicine on polycystic ovary syndrome (PCOS) Daru. 2019;27(2):863–877. doi: 10.1007/s40199-019-00312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Q., Deng H., Cheng K., et al. Manual acupuncture for the infertile female with polycystic ovary syndrome (PCOS): study protocol for a randomized sham-controlled trial. Trials. 2019;20(1):564. doi: 10.1186/s13063-019-3667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Z J., Z. B-x, L L. Acupuncture and moxibustion. Beijing: people's Medical Publishing House; 2014.
- 20.Hui K.K., Nixon E.E., Vangel M.G., et al. Characterization of the "deqi" response in acupuncture. BMC Complem Altern Med. 2007;7:33. doi: 10.1186/1472-6882-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang J., Liu Y., Huang J., et al. Acupuncture and Chinese medicine of artificial cycle therapy for insulin resistance of polycystic ovary syndrome with phlegm damp type and its mechanism. Zhongguo Zhen Jiu. 2017;37(11):1163–1168. doi: 10.13703/j.0255-2930.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Min Z., Hong-Yan Y., Xiao-Yun W., Jing-Jing D., Jian L. Randomized controlled study of disease-syndrome combination therapy for anovulatory infertility. J Guangzhou Univ Tradit Chin Med. 2017;34(06):815–818. [Google Scholar]
- 23.Johansson J., Redman L., Veldhuis P.P., et al. Acupuncture for ovulation induction in polycystic ovary syndrome: a randomized controlled trial. Am J Physiol Endocrinol Metab. 2013;304(9):E934–E943. doi: 10.1152/ajpendo.00039.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu J., Zuo Y. Efficacy of acupuncture as adjunctive treatment on infertility patients with polycystic ovary syndrome. Zhongguo Zhen Jiu. 2018;38(4):358–361. doi: 10.13703/j.0255-2930.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Yin Y., Zhang Y., Zhang H., Jiang D., Guo G. Clinical therapeutic effects of acupuncture combined with Chinese herbal medicine on infertility of polycystic ovary syndrome in the patients with ovulation induction with letrozole. Zhongguo Zhen Jiu. 2018;38(1):27–32. doi: 10.13703/j.0255-2930.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Yuan B.C., Ma K., Zhang C.H., Yuan Y. Bushen Huoxue herbal medicine in subfertile women with polycystic ovary syndrome: a Meta-analysis. Zhongguo Zhong Yao Za Zhi. 2019;44(6):1080–1086. doi: 10.19540/j.cnki.cjcmm.2019.0021. [DOI] [PubMed] [Google Scholar]
- 27.Liao W.T., Chiang J.H., Li C.J., Lee M.T., Su C.C., HR Yen. Investigation on the use of traditional chinese medicine for polycystic ovary syndrome in a nationwide prescription database in Taiwan. J Clin Med. 2018;7(7) doi: 10.3390/jcm7070179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chao-chao Y., Li-hong K., Chao-yang M., et al. The rules of acupoint-selection of acupuncture for polycystic ovary syndrome based on data mining. World J Acupunct.-Moxibust. (WJAM) 2016;26(03):73–78. [Google Scholar]
- 29.Ge X., Yue-lai C. Regularities in application of acupoints in acupuncture treatment for ovulatory disorder infertility shanghai J Acu-mox 2017;36(5):620–5.
- 30.Jin X., Chun-chun J., Zhen-ru S., Jie S., You-bing X. Study on acupoint seleection rules of treating infertility in ancient literature. J Nanjing Univ Tradit Chin Med. 2019;35(6):719–723. [Google Scholar]
- 31.Jo J., Lee Y.J., Lee H. Acupuncture for polycystic ovarian syndrome: a systematic review and meta-analysis. Medicine (Baltimore) 2017;96(23):e7066. doi: 10.1097/MD.0000000000007066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yun L., Liqun W., Shuqi Y., Chunxiao W., Liming L., Wei Y. Acupuncture for infertile women without undergoing assisted reproductive techniques (ART): a systematic review and meta-analysis. Medicine (Baltimore) 2019;98(29):e16463. doi: 10.1097/MD.0000000000016463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim C.E.D., Ng R.W.C., Cheng N.C.L., Zhang G.S., Chen H. Acupuncture for polycystic ovarian syndrome. Cochrane Database Syst Rev. 2019;7 doi: 10.1002/14651858.CD007689.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu X.K., Stener-Victorin E., Kuang H.Y., et al. Effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome: a randomized clinical trial. JAMA. 2017;317(24):2502–2514. doi: 10.1001/jama.2017.7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Y., Zhao Y., Yu S., Hu Y. Some issues from effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome in JAMA. Zhongguo Zhen Jiu. 2017;37(12):1342–1346. doi: 10.13703/j.0255-2930.2017.12.023. [DOI] [PubMed] [Google Scholar]
- 36.Gang W.J., Jing X.H. Is acupuncture actually not effective for polycystic ovary syndrome? : analysis of the trial published in jama. Chin J Integr Med. 2017;23(12):883–886. doi: 10.1007/s11655-017-2831-z. [DOI] [PubMed] [Google Scholar]
- 37.Gang W.J., Meng X., Jing X.H. Assessing the adequacy of acupuncture in clinical trials: current status and suggestions. Zhongguo Zhen Jiu. 2019;39(3):229–233. doi: 10.13703/j.0255-2930.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 38.Shi G.X., Yang X.M., Liu C.Z., Wang L.P. Factors contributing to therapeutic effects evaluated in acupuncture clinical trials. Trials. 2012;13:42. doi: 10.1186/1745-6215-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cao Y., Zhang L., Zhao D., Liu Z. DONG's extraordinary acupoints for the ovarian function of polycystic ovary syndrome:a randomized controlled pilot trial. Zhongguo Zhen Jiu. 2017;37(7):710–714. doi: 10.13703/j.0255-2930.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Wang S.J., Zhang J.J., Qie L.L. Acupuncture relieves the excessive excitation of hypothalamic-pituitary-adrenal cortex axis function and correlates with the regulatory mechanism of GR, CRH, and ACTHR. Evidence-based complementary and alternative medicine. eCAM. 2014;2014 doi: 10.1155/2014/495379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adeniji A.A., Essah P.A., Nestler J.E., Cheang K.I. Metabolic effects of a commonly used combined hormonal oral contraceptive in women with and without polycystic ovary syndrome. J Womens Health (Larchmt) 2016;25(6):638–645. doi: 10.1089/jwh.2015.5418. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The obtained data in the current study are available upon reasonable request from the corresponding authors.