Abstract
While urothelial carcinoma is the most common histologic type of bladder cancer in the United States, leiomyosarcoma is a rare and aggressive variant. The rarity of bladder leiomyosarcoma results in uncertainty regarding the optimal treatment pathway. We report on a patient with a giant non-metastatic bladder leiomyosarcoma effectively managed with primary surgical intervention without chemoradiation.
Keywords: Urology, Oncology, Leiomyosarcoma, Cystoprostoprostatectomy, Radical cystectomy
1. Introduction
Bladder malignancy is among the top ten most common cancers in the United States with urothelial carcinoma being the most common histologic type. Leiomyosarcoma is a relatively common histology of uterine cancer but rarely arises primarily in the bladder. While some prior studies have associated this cancer with cyclophosphamide therapy, it can also occur in the absence of this treatment. Due to the low incidence of this bladder leiomyosarcoma, current management guidelines are limited. In particular, there is scarce published literature on insights for optimal treatment in the setting of extremely large tumors.
In this case report we discuss management of giant leiomyosarcoma of the bladder utilizing surgical resection without concomitant perioperative chemoradiation.
2. Case presentation
A 56-year-old male presented to his primary care provider with new onset gross hematuria. He was initially treated with antibiotics, and ultimately underwent a CT of the abdomen and pelvis which revealed at large bladder mass invading into the prostate and causing bilateral hydroureteronephrosis, prompting referral to urology.
In our clinic, he endorsed persistent gross hematuria, dysuria, urinary frequency, and nocturia. He denied additional constitutional symptoms, and physical exam was unremarkable. He denied past medical history of malignancy and had a maternal history of breast cancer. On laboratory analysis, serum creatinine was normal and there was a mild normocytic anemia. A CT of the chest showed no evidence of metastatic disease. Interventional radiology was consulted and placed bilateral percutaneous nephrostomy tubes.
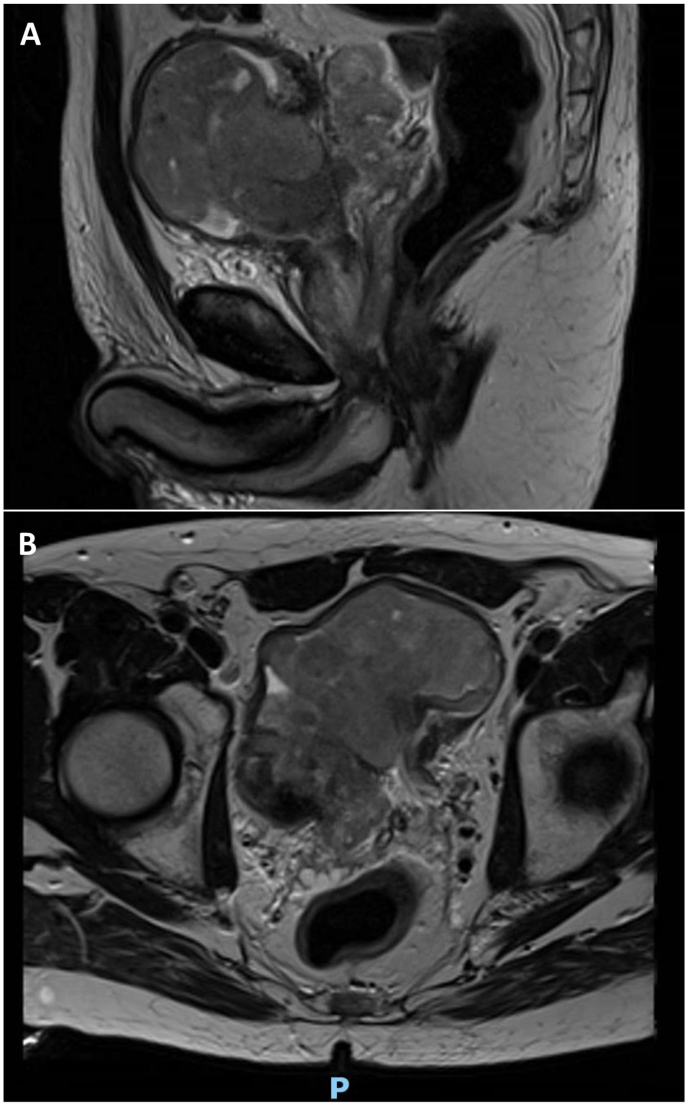
We performed a transurethral resection of bladder tumor to obtain pathologic diagnosis. During the resection, a small biopsy was performed instead of attempting complete resection because of concern for non-urothelial histology and the massive size of the polypoid submucosal tumor with significant parasitic appearing vasculature. The biopsy pathology confirmed high grade leiomyosarcoma. An MRI of the pelvis with and without contrast demonstrated a 9 cm bladder tumor with potential invasion of the prostate and abutment of the rectum with no evidence of lymphadenopathy (Fig. 1). A multidisciplinary sarcoma tumor board team reviewed the case and agreed to pursue upfront radical cystoprostatectomy with pelvic lymph node dissection. Our team also discussed the possible rectal involvement with our colorectal surgery colleagues to plan for a simultaneous colostomy if needed intraoperatively.
Fig. 1.
MRI Pelvis demonstrating leiomyosarcoma. (A) Sagittal image. (B) Axial image.
Surgical resection with radical cystoprostoprostatectomy, en bloc resection of the leiomyosarcoma, pelvic lymphadenectomy, and creation of ileal conduit was performed (Fig. 2). Final pathology demonstrated a 9.2 cm grade 3 leiomyosarcoma (25 mitoses per 10 high power fields, with lymphovascular invasion, and 10% necrosis present) with negative margins (Fig. 3). Additionally, sixteen pelvic nodes were negative for metastases. The patient recovered from surgery uneventfully and was discharged on post-operative day 4. At 9-month follow-up he was found to have no evidence of disease on imaging.
Fig. 2.
Radical Cystoprostatectomy Specimens. (A) Prior to sectioning. (B) Sagittal section demonstrating tan-white fleshy cut surfaces with foci of hemorrhage.
Fig. 3.
H&E-stained section of the tumor. (A) Low-magnification view demonstrating a hypercellular mass with necrosis (star), infiltrating the perivesicle adipose tissue (arrow). (B) Higher magnification view showing spindled tumor cells with eosinophilic cytoplasm arranged in intersecting fascicles. Marked nuclear atypia is present. Mitotic figures, including atypical ones (star) are abundant.
3. Discussion
Bladder leiomyosarcoma is a rare malignancy that accounts for only 0.1% of bladder lesions.1 Given the rarity of this tumor, there has not been a consensus on standard treatment pathways, and there is limited data to guide clinical decision making. Our case is notable due to the massive size of tumor and lack of neoadjuvant treatment. Prior literature has explored the role of neoadjuvant cyclophosphamide therapy, although these reports are limited.2,3 A systematic review and meta-analysis by Zieschang et al. reviewed 210 cases between 1970 and 2018, finding that only 26% of patients received neoadjuvant chemotherapy and that surgical resection with negative margins was critical for optimal oncologic outcomes.4 While the role of lymphadenectomy is unclear, a Surveillance, Epidemiology, and End Results database (SEER) study of 183 patients demonstrated a 38% rate of locoregional disease, supporting consideration of lymph node dissection at time of surgery.5 Our case demonstrates the feasibility of surgical resection for a very large leiomyosarcoma of the bladder without utilization of neoadjuvant systemic therapy. Further research is needed to determine the optimal utilization of perioperative chemoradiation and their necessity and impact on long term patient outcomes.
4. Conclusion
Leiomyosarcoma is a rare histology for bladder malignancy, with limited reports discussing massive tumors. This case report provides an example of a patient with a large primary tumor occurring in the absence of prior chemotherapy, without evidence of nodal involvement or metastatic disease, and confirms that primary surgical intervention can sometimes be effective without perioperative chemoradiation.
Consent
Consent for this article was obtained from the patient.
Credit author statement
Alexander Hart: Conceptualization, methodology, Investigation, Writing-Original Draft, Writing- Review & editing. Charles Schlaepfer: Writing- Review & editing, visualization. Neha Dhungana: Writing-Review & editing, visualization Mohammed Milhem: Writing- Review & editing, Supervision, Visualization, Investigation. Vignesh Packiam: Conceptualization, methodology, writing- review & editing, visualization, supervision, project administration.
Declaration of competing interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
References
- 1.Hamadalla N.Y., Rifat U.N., Safi K.C., Mohammed M., Abu-Farsakh H. Leiomyosarcoma of the urinary bladder: a review and a report of two further cases. Arab J Urol. Jun 2013;11(2):159–164. doi: 10.1016/j.aju.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parekh D.J., Jung C., O'Conner J., Dutta S., Smith E.R., Jr. Leiomyosarcoma in urinary bladder after cyclophosphamide therapy for retinoblastoma and review of bladder sarcomas. Urology. Jul 2002;60(1):164. doi: 10.1016/s0090-4295(02)01701-6. [DOI] [PubMed] [Google Scholar]
- 3.Svajdler M., Jr., Andrašina I., Ilenčíková D., Rychlý B., Piačková B. Recurring multifocal leiomyosarcoma of the urinary bladder 22 years after therapy for bilateral (hereditary) retinoblastoma: a case report and review of the literature. Cesk Patol. Jan 2012;48(1):44–48. [PubMed] [Google Scholar]
- 4.Zieschang H., Koch R., Wirth M.P., Froehner M. Leiomyosarcoma of the urinary bladder in adult patients: a systematic review of the literature and meta-analysis. Urol Int. 2019;102(1):96–101. doi: 10.1159/000494357. [DOI] [PubMed] [Google Scholar]
- 5.Rodríguez D., Preston M.A., Barrisford G.W., Olumi A.F., Feldman A.S. Clinical features of leiomyosarcoma of the urinary bladder: analysis of 183 cases. Urol Oncol. Oct 2014;32(7):958–965. doi: 10.1016/j.urolonc.2014.01.025. [DOI] [PubMed] [Google Scholar]