Highlights
-
•
Loofah sponges are used for skin cleaning, but can become contaminated with bacterial pathogens
-
•
The abrasive nature of loofah sponges can allow for bacteria to enter the skin and cause infection
-
•
Patients should be aware of the risks with loofah sponge use and how to minimize risk of infection
Keywords: Streptococcus pyogenes, Loofah sponge, Impetigo
Abstract
Loofah sponges have been implicated in skin and soft tissue infections due to their ability to harbor bacteria and cause microtrauma to the skin. In this case report, we describe a case of impetigo and cellulitis due to Streptococcus pyogenes complicated by secondary spread through loofah sponge use. The same organism was cultured from the infected body sites and loofah sponge, and a comparative genomic analysis confirmed that the isolates were identical.
Introduction
Loofah sponges are a common shower accessory used for skin cleaning and exfoliation. Their abrasive nature can cause microtrauma to the skin and create a portal of entry for bacteria. Common bacterial species associated with these sponges often include Pseudomonas species and the Enterobacteriales. We describe a case of Streptococcus pyogenes secondary impetigo due to loofah sponge use.
Case
A 45 year-old male presented to the Emergency Department with a five-day history of right leg erythema and edema and a two-day history of fever, chills and night sweats. He also reported a 3-week history of linear group of pustular lesions on his right leg, which subsequently spread to his arms and contralateral leg (Fig. 1).
Fig. 1.
A linear group of pustular lesions on right leg three weeks prior to hospital admission (left) and ruptured pustular lesions on right forearm one week prior to admission (right).
His medical history was significant for hypertension and HIV infection, which was diagnosed 15 years ago, for which he was treated with emtricitabine-tenofovir, darunavir and ritonavir. There was no history of chronic skin disease, opportunistic infections, or injection drug use. On examination, it was noted that his right leg was tender, swollen and erythematous with a ruptured bulla overlying the anterior tibia region (Fig. 2). There were also scattered ulcerative lesions distributed on his legs, arms and neck. Furthermore, initial investigations were significant for a predominantly neutrophilic leukocytosis (23.8 × 109 cells/L) and an elevated C-reactive protein (345 mg/L). His CD4 count was 0.62 × 109 cells/L and HIV viral load was less than 40 copies per milliliter.
Fig. 2.

Scattered healing pustular lesions on the lower extremities after 48 h of intravenous cefazolin therapy.
Given that there was concern for cellulitis, the patient was treated empirically with intravenous cefazolin 2 g every 8 h. A wound swab of a right leg pustule and a punch biopsy of a left arm pustule were sent for bacterial, mycobacterial and fungal culture. Bacterial cultures from both specimens grew Streptococcus pyogenes (susceptible to penicillin, clindamycin and erythromycin). Fungal and mycobacterial cultures did not yield any growth. Histopathologic examination of the left arm biopsy showed non-specific inflammatory changes with no evidence of neoplasia or vasculitis.
With treatment, the patient’s fever resolved, and all skin lesions noted on admission began to improve. On further history, the patient reported that with the development of the pustular lesions on his right leg, he began to use a loofah sponge to aggressively clean the right leg, and other parts of his body. Soon after doing this, he began to develop the lesions elsewhere on his body. He lived at home alone and did not share the loofah sponge with anyone.
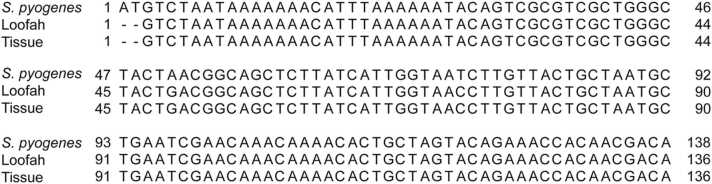
To determine whether the spreading of the lesions resulted from the loofah sponge, a sample of the patient’s sponge was submitted for bacterial culture. Indeed, the culture displayed moderate growth of S. pyogenes amongst a background of commensal skin microbiota. Whole genome sequencing was performed using the Illumina MiSeq platform following extraction of bacterial DNA from two isolates, one from the bath sponge and one from skin biopsy tissue culture. The sequencing reads were then assembled de novo using Unicycler and aligned to the genome of S. pyogenes str. MGAS10786 (NCBI: NZ_CP010450.1) as a reference [1]. Analysis of the emm gene, used for Streptococcus typing, indicated both isolates were emm type 28. Whole genome alignment further confirmed the isolates were identical and a representative alignment of the slo gene (encoding streptolysin O) is shown in Fig. 3.
Fig. 3.
Bacterial isolates from the loofah sponge and skin biopsies are both S. pyogenes. Nucleotide sequences assembled from the bacterial isolates and the slo gene encoding for streptolysin O from S. pyogenes str. MGAS10786 share 99% pairwise identity. Only the first ~100 bp of the alignment is shown.
After 4 days of intravenous cefazolin, the patient was transitioned to oral cephalexin 500 mg four times daily to complete a 10-day course of treatment. Cephalexin was chosen over penicillin due to greater oral bioavailability. At the 1-month follow-up with the patient, the right leg had significantly improved with minimal residual post-inflammatory changes, and all other skin lesions had resolved.
Discussion
Streptococcus pyogenes (also known as Group A Streptococcus) is the most common cause of skin and soft tissue infections, which can range from impetigo, erysipelas, and cellulitis to necrotizing fasciitis. Primary impetigo occurs because of direct bacterial invasion of healthy skin and manifests as maculopapular or vesicular lesions which often become covered with yellow-colored crusts. Secondary impetigo can occur when bacteria gain entry through a disrupted skin barrier resulting from trauma, an insect bite, or chronic skin diseases.
As we observed with this patient’s initial symptoms, S. pyogenes skin infections can also manifest as a sporotrichoid lymphocutaneous infection, where superficial cutaneous lesions develop along the lymphatic system. Other notable pathogens which can also produce this syndrome include: Nocardia species, non-tuberculous mycobacteria (such as Mycobacterium marinum), Leishmania species, Francisella tularensis, and Sporothrix schenckii. Thus, obtaining skin biopsies of the affected lesions for culture is crucial in determining the causative agent.
In this case report, the use of a loofah sponge is the most likely reservoir and risk factor for developing secondary Group A Streptococcus impetigo. This is supported by a history of aggressive sponge use preceding the development of skin lesions on other parts of the body, isolation of identical strains of Group A Streptococcus from the bath sponge and skin biopsies, and response to anti-streptococcal antibiotic therapy.
Loofah sponges are often used for their exfoliative properties, but their ability to cause microtrauma of the skin can allow bacteria to invade the skin and cause infection. Due to frequent contact with human skin and water, loofah sponges can become contaminated and colonized with human pathogens [2]. Cases of Pseudomonas folliculitis associated with contaminated loofah sponges have been well described in the literature [3], [4].
To our knowledge, this is the first case report of S. pyogenes secondary impetigo due to the use of a loofah sponge. Patients who present with skin and soft tissue infections with no clear predisposing factors should be asked about the use of loofah sponges as a potential risk factor. Patients who use them should be counseled on strategies to minimize the risk of contamination and infection, such as replacing them on a periodic basis, allowing the sponge to dry completely in between use, not sharing them with other family members, or forgoing their use altogether.
Ethical approval
Not applicable
Consent
Written and signed consent has been obtained from the patient.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Philip W. Lam: Conceptualization, Writing – original draft preparation, Writing – reviewing and editing. Adrienne K. Chan: Conceptualization, Writing – reviewing and editing. N. Y. Elizabeth Chau: Formal analysis, Investigation, Writing – reviewing and editing. Shawn T. Clark: Formal analysis, Investigation, Writing – reviewing and editing. Robert A. Kozak: Conceptualization, Formal analysis, Investigation, Writing – original draft preparation, Writing – reviewing and editing.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
PWL, AKC and RK conceived of the work. STC and NYEC provided laboratory technical support. STC, NYEC and RK carried out the whole genome sequencing and interpretation of results. PWL and RK drafted the manuscript. PWL, AKC, STC and RK revised and proofread the manuscript. Bacterial genomes were sequenced at the Center for the Analysis of Genome Evolution and Function (University of Toronto, Canada). The authors thank Herbert Liu for his technical assistance.
References
- 1.Wick R.R., Judd L.M., Gorrie C.L., Holt K.E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol. 2017;13 doi: 10.1371/journal.pcbi.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottone E.J., Perez A.A., 2nd, Oeser J.L. Loofah sponges as reservoirs and vehicles in the transmission of potentially pathogenic bacterial species to human skin. J Clin Microbiol. 1994;32:469–472. doi: 10.1128/jcm.32.2.469-472.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frenkel L.M. Pseudomonas folliculitis from sponges promoted as beauty aids. J Clin Microbiol. 1993;31:2838. doi: 10.1128/jcm.31.10.2838-.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bottone E.J., Perez A.A., 2nd Pseudomonas aeruginosa folliculitis acquired through use of a contaminated loofah sponge: an unrecognized potential public health problem. J Clin Microbiol. 1993;31:480–483. doi: 10.1128/jcm.31.3.480-483.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]