Abstract
The congenital anomaly of the ovary is classified as a supernumerary, accessory, and lobulated ovary (LO). Although the former two entities are anomalies of abnormal location, LO is a category of morphological abnormality of the ovary. There are several case reports of this entity; however, most of them were diagnosed during surgery or histopathologically. One case report included ultrasound findings, with the diagnosis confirmed during surgery. We report a young-adult case with LO diagnosed and followed up with MR. Although LO is a rare congenital anomaly, it might be misdiagnosed as malignant tumors, as in our case. Therefore, radiologists and gynecologists should look out for this entity in MR findings, which can prove to be crucial in preventing unnecessary surgery.
Keywords: lobulated ovary, ovary, congenital anomaly, polycystic ovary syndrome, MRI
Introduction
Congenital anomaly of the ovary includes absence, lobulated, accessory, and supernumerary ovaries [1]. Among them, the lobulated ovary is the only entity of the morphological abnormality of the nomotopic ovarian tissue, and only 15 cases with lobulated ovary have been previously reported [2, 3]. Most patients were diagnosed during laparotomy [2], and another case was suspected with ultrasound and confirmed by open biopsy [3]. We diagnosed a case with lobulated ovary with MR, who were supposed malignant ovarian tumors. We could choose the observation option and confirmed the diagnosis after follow-up MR six months after the initial presentation. This is the first case report with MR of this rare congenital anomaly mimicking a malignant ovarian tumor.
Case Description
A 22-year-old woman with suspicion of malignant ovarian tumor visited our hospital. She had seen a gynecologic clinic to fill a prescription for oral contraceptives (OCs). She had been using OCs past four years; however, any ovarian abnormality had not been pointed out. Her other past medical history was unremarkable. Alfa fetoprotein (AFP), carcinoembryonic antigen (CEA), and serum level of estradiol showed a normal range. The gynecologist found her ovaries were swollen bilaterally with transvaginal ultrasound (TVUS) and suspected ovarian tumors. She was transferred to another hospital, and her MR imaging demonstrated bilateral lobulated ovarian masses. She was also supposed to have bilateral malignant ovarian tumors and scheduled exploratory laparoscopy. After that, she visited our hospital for a second opinion. Although her ovaries had been swollen and lobulated, the ovarian masses were composed of several lobules with hypointense rim and many tiny cysts on T2-weighted images (T2WI, Fig. 1A). It showed a lower signal at the periphery of each lobule on T1-weighted images (T1WI, Fig. 1B), and diffusion-weighted images (DWI) did not reveal abnormally restricted diffusion (Fig. 1C). The maximum diameter of both ovaries was 8.4 cm in the right and 4.9 cm in the left. They were abnormally larger than the average population as the standard maximum ovarian diameter had been reported as about 2.6 cm in their twenties [4]. Normal-shaped ovaries were not found anywhere in the scanned area, each lobule of the mass was very similar to the normal ovary including many developing follicles, and both ovarian masses showed the same morphological characteristics, we suspected congenital anomaly of the ovary. We scheduled follow-up MR examination six months after the initial visit. The 6 months follow-up period was uneventful, and the repeated MRI revealed the same findings and did not demonstrate any peritoneal implants or other ancillary findings of ovarian malignancy (Fig. 2). Therefore, we concluded the masses were lobulated ovaries as a rare congenital anomaly.
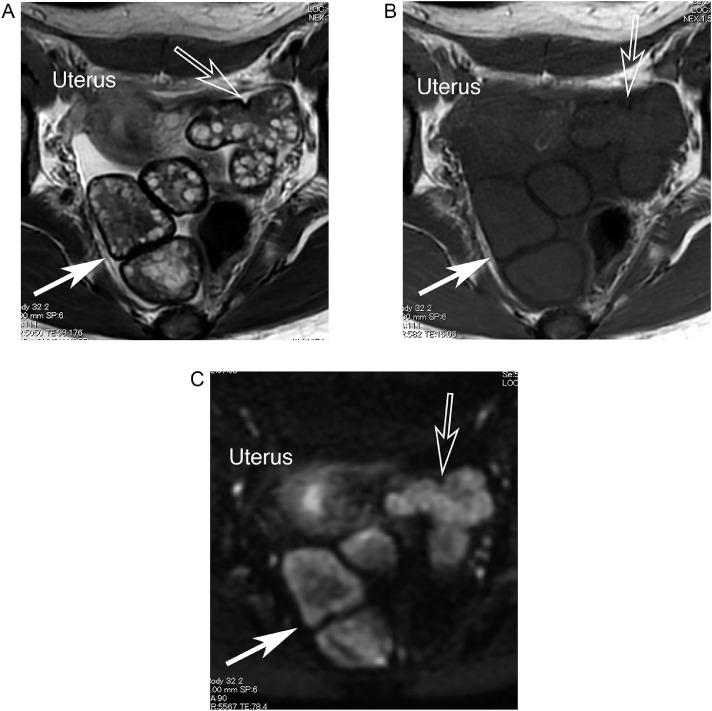
Fig. 1.
A 22-year-old woman with a lobulated ovary at the time of presentation.
Axial T2-weighted image demonstrates lobulated masses composed of several hypointense lobules with hypointense rim and many tiny cysts corresponding to follicles on (Fig. 1A, arrow: right ovary, open arrow: left ovary). They show hypointense lobulated masses circulated by the rim with a lower signal on axial T1-weighted image (Fig. 1B, arrow: right ovary, open arrow: left ovary). Slightly higher signals are shown at the periphery of each mass on DWI; that signal intensity was lower than normal endometrium (Fig. 1C, arrow: right ovary, open arrow: left ovary).
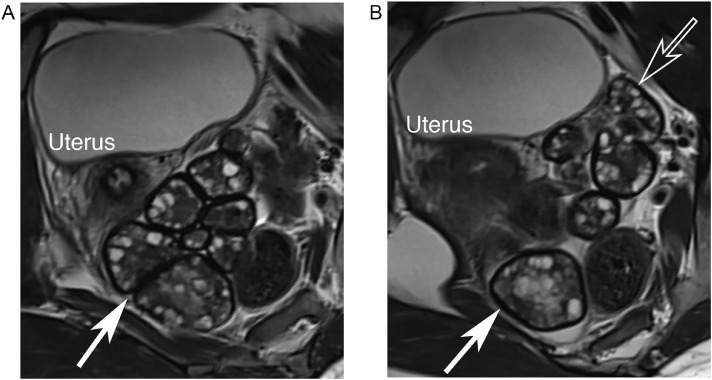
Fig. 2.
A 22-year-old woman with lobulated ovary after 6 months follow-up. Repeated oblique axial (Fig.2A, arrow: right ovary) and coronal (Fig.2B, arrow: right ovary, open arrow: left ovary) perpendicular to the uterine axis revealed the same findings as Figure 1.
Discussion
Wharton et al. reported three cases with congenital anomaly and advocated the entity of lobulated ovary separated from supernumerary and accessor ovary after an extensive analysis of previously reported cases [5]. According to Wharton, a supernumerary ovary is defined as a third ovary independent of and at some distance from ovaries, and the accessory ovary must be situated very close to the normally placed ovary [5]. On the other hand, a lobulated ovary is defined as an ovary divided by one or more fissures into two or more lobules. Bands of connective tissue sometimes connect the lobules. The classification mentioned above of congenital anomalies of the ovary seems widely accepted; accessory, supernumerary and lobulated ovaries [1]. However, sometimes the distinction among these three categories is unclear-cut, especially lobulated and accessory ovaries are similar. The former results from lobulation of the ovarian anlage, whereas the latter develops from embryonically separated parts of the eutopic ovarian anlage.
Only 15 cases with lobulated ovaries have been published to the best of our knowledge [2, 3]. Most of them were incidentally found at laparotomy [2], and a case was suspected with ultrasound and confirmed by open biopsy [3]. Our patient was suspected of ovarian neoplasm even malignancy and scheduled exploratory laparotomy, as ovaries had been swollen and showed lobulated shape. However, each lobule was very similar to a normal ovary or polycystic ovary. Therefore, we could suspect the possibility of a congenital anomaly and prevent unnecessary surgery. The differential diagnosis of this entity may include sex-cord stromal tumors of the ovary as it shows low signal intensity on T2WI and is well-demarcated. Fibrothecoma, a relatively common sex-cord stromal tumor, may show such MR findings [6] and may show cystic degeneration [7]. However, numerous tiny cysts arranged at the periphery of the mass as in the present case may be unusual in fibrothecoma. Bilateral well-demarcated hypointense masses on T2WI can also be considered metastatic ovarian tumors [3, 8, 9] that usually show strong enhancement [9] and restricted diffusion. Although contrast enhancement was not performed, none of the DWI revealed restricted diffusion in our present case. Therefore, MR findings of the lobulated ovary could be differentiated from ovarian neoplasms. The most important key finding is ovarian follicles at the periphery of each lobule of the lobulated masses. Both radiologists and gynecologists should know the morphological characteristics of the lobulated ovary as a rare congenital anomaly for correct diagnosis and carefully search for this structure during interpreting MR and ultrasound is most important for accurate diagnosis.
Each lobule in our present case was morphologically similar to polycystic ovary syndrome (PCOS) rather than a normal ovary. Kim DS et al. also reported not only morphological similarity but also elevated luteinized hormone (LH) and/or follicle-stimulating hormone (FSH) ratio, suggesting PCOS, in their case with lobulated ovary [2]. Although LH and/or FSH ratio was not measured in the present case, she did not show hirsutism or obesity, which are characteristic clinical findings of PCOS. Amenorrhea is also a typical clinical manifestation of PCOS; we could not evaluate she had menstrual abnormality or not, as she usually used oral contraceptives. As she did not get married, the obstetrical outcome is unknown, and close observation should be required. PCOS-like morphological abnormality has been reported neither in the supernumerary nor accessory ovary, especially since the latter is usually smaller than 1cm [10]. Dabirashrafi H. et al. reported that the maldescent ovary was always larger than usual. Their appearance resembled PCOS in their manuscript reporting increased incidence of malposition of the ovaries in uterine anomalies, such as Mullerian duct anomaly or Mayer-Rokitansky-Kuster-Hauser syndrome [11]. It seems interesting, although malposition is another kind of congenital anomaly.
Although we could not find any urogenital anomaly demonstrated in her MR, an increased frequency of associated congenital urogenital malformation has been reported in cases with ovarian anomalies. Cruikshank SH estimated 36% of the supernumerary ovary might have associated anomaly [12]. Kim DS et al. described two cases with Mullerian duct anomaly in 15 cases with lobulated ovary [2]. Although the exact incidence of the associated anomaly is unclear, we should also pay attention to the uterine morphology and renal or ureteral malformation in diagnosing ovarian anomaly.
In conclusion, radiologists should know of the morphological anomaly of the ovarian anomaly and should raise the possibility of lobulated ovaries when the bilateral ovaries had been swollen with lobulation and peripherally arranged numerous small follicles.
Footnotes
Acknowledgments: The authors would like to thank Enago (www.enago.jp) for the English language review.
Competing Interests: None of the authors have any financial/personal interest or belief that could affect our objectivity.
References
- 1.Irving JA, Clement PB. In: Blaustein's Pathology of the Female Genital Tract. editors. Kurman R, Hedrick Ellenson L, Ronnett B, editors. Switzerland: Springer, Cham; 2019. Nonneoplastic Lesions of the Ovary; pp. 715–770. [Google Scholar]
- 2.Kim DS, Monn H, Kim MS, Kim SW. Lobulated polycystic ovary with huge parovarian cyst. Asia Oceania J Obstet Gynaecol. 1985;11:75–79. doi: 10.1111/j.1447-0756.1985.tb00050.x. doi: [DOI] [PubMed] [Google Scholar]
- 3.Chen T, Li J, Yang X, Huang H, Cai S. Ultrasound manifestations of lobulated ovaries: Case report. Medicine (Baltimore) 2018;97:e0550. doi: 10.1097/MD.0000000000010550. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hauth EA, Jaeger HJ, Libera H, Lange S, Forsting M. Magnetic resonance imaging of the ovaries of healthy women: determination of normal values. Acta Radiol. 2006;47:986–992. doi: 10.1080/02841850600885419. doi: [DOI] [PubMed] [Google Scholar]
- 5.Wharton LR. Two cases of supernumerary ovary and one of accessory ovary, with an analysis of previously reported cases. Am J Obstet Gynecol. 1959;78:1101–1119. doi: 10.1016/s0002-9378(16)36660-1. doi: [DOI] [PubMed] [Google Scholar]
- 6.Troiano RN, Lazzarini KM, Scoutt LM, Lange RC, Flynn SD, McCarthy S. Fibroma and fibrothecoma of the ovary: MR imaging findings. Radiology. 1997;204:795–798. doi: 10.1148/radiology.204.3.9280262. doi: [DOI] [PubMed] [Google Scholar]
- 7.Takeshita T, Shima H, Oishi S, Machida N, Yamazaki K, Imamura T, et al. Ovarian fibroma (fibrothecoma) with extensive cystic degeneration: unusual MR imaging findings in two cases. Radiat Med. 2005;23:70–74. [PubMed] [Google Scholar]
- 8.Ha HK, Baek SY, Kim SH, Kim HH, Chung EC, Yeon KM. Krukenberg's tumor of the ovary: MR imaging features. AJR Am J Roentgenol. 1995;164:1435–1439. doi: 10.2214/ajr.164.6.7754887. doi: [DOI] [PubMed] [Google Scholar]
- 9.Tanaka YO, Saida TS, Minami R, Yagi T, Tsunoda H, Yoshikawa H, et al. MR findings of ovarian tumors with hormonal activity, with emphasis on tumors other than sex cord-stromal tumors. Eur J Radiol. 2007;62:317–327. doi: 10.1016/j.ejrad.2007.02.027. doi: [DOI] [PubMed] [Google Scholar]
- 10.Tantitamit T, Lee CL, Kuo HH. Inevitable Removal of Left Accessory Ovary. Gynecol Minim Invasive Ther. 2020;9:106–107. doi: 10.4103/GMIT.GMIT_44_18. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dabirashrafi H, Mohammad K, Moghadami-Tabrizi N. Ovarian malposition in women with uterine anomalies. Obstet Gynecol. 1994;83:293–294. [PubMed] [Google Scholar]
- 12.Cruikshank SH, Van Drie DM. Supernumerary ovaries: update and review. Obstet Gynecol. 1982;60:126–129. [PubMed] [Google Scholar]