Abstract
Objective
Among adolescents and young adults (AYAs) with chronic illness, effective provider communication is essential for patient-centered care during a sensitive developmental period. However, communication in chronic illness care for AYAs is not well studied. Our objectives were to describe the provider communication skills in pediatric chronic kidney disease (CKD) care visits; and determine if communication skills differ by AYA characteristics.
Methods
We adapted a global consultation rating system for pediatric subspecialty care using audiotaped clinic encounters of 18 pediatric nephrologists with 99 AYAs (age M(SD)=14.9(2.6)) with CKD stages 1–5 and 96 caregivers. We hypothesized that provider communication skills would differ by AYA characteristics (age, gender, and race).
Results
The strongest provider skills included initiating the session and developing rapport; lowest rated skills were asking patient’s perspective and checking understanding. Communication scores did not consistently differ by AYA age or race, but were rated higher with female AYAs in several domains (ps<0.05).
Conclusions
Pediatric providers generally had adequate or good communication scores with AYAs, but improvement in certain skills, particularly with male AYAs, may further support patient-centered care.
Practice Implications
To achieve consistent, patient-centered communication with AYAs, an observation-based global assessment may identify areas for provider improvement.
1. INTRODUCTION
There is broad consensus among medical education institutions (including the Institute of Medicine,1 the Association of American Medical Colleges,2 the Medical Council of Canada,3 and the American Academy of Pediatrics4) that good communication skills (e.g., clear verbal content and good interpersonal skills) are crucial for delivering high-quality medical care. Further, the Accreditation Council for Graduate Medical Education (ACGME) has highlighted interpersonal and communication skills as a core area of competency in the education and certification of physicians.4 These organizations focus on both content of what is discussed and the process through which the interview unfolds,5,6 yet there is currently no gold standard on how best to measure or define communication skills.7 Not surprisingly then, provider communication is inconsistently defined and measured in research.8
The internationally-adopted Calgary-Cambridge Guides are used in medical education curricula in the United States, Canada, and Europe and the United Kingdom.5,9,10 The guides assert that effective provider communication should combine pertinent informative content with positive relational components, encompassing core principles that are applicable and important in both pediatric and adult visits.5,9,10 Specifically, it has been recommende d that providers demonstrate communication skills by using shared decision-making, active listening, and open-ended questions.11 Despite its strong theoretical foundation and prioritization in training of healthcare professionals,12,13 surprisingly little research has examined patient-provider communication skills with adolescents and young adults (AYAs). There is a need for development of a pediatric setting coding system to enable assessment of the core communication skills outlined by the Calgary-Cambridge guides. Further, it is crucial to identify any communication skills that may differ by AYA characteristics, which could signal potential risk factors or disparities in the quality of clinical care.
Pediatric chronic kidney disease (CKD) is a lifelong condition with myriad underlying etiologies, requiring daily maintenance regimens, constant monitoring, and frequent appointments. Pediatric CKD is also associated with adverse effects on physical growth and neurocognitive development,14,15 quality of life,16 and psychosocial experiences during transition.15,17 Prior work has shown that providers contribute the most talk (63.7%) during nephrology clinic visits with AYAs, most commonly in the form of biomedical information-giving,18 indicating that they are the predominant “driver” of communication during visits. Therefore, an understanding of communication skills, beyond quantity of communication, is needed in order to evaluate the extent to which communication skills align with those recommended for effective healthcare communication.5 Across the AYA developmental period, AYAs whose providers prioritize building a shared model of health have higher empowerment and self-care self-efficacy in following treatment regimens.19,20 Thus, identifying specific areas of strength and weakness in provider communication skills is needed in order to ensure effective quality of care across the transition period for AYAs with chronic conditions.
It is also important to consider the influence of AYA characteristics (e.g., age, gender, and race) on patient-provider communication skills. In a recent study of AYA nephrology care, the quantity of talk by AYAs increased with higher age in exchange for a decrease in caregiver talk, yet the quantity of provider talk did not differ with AYA age.18 Additionally, in a report by the World Health Organization,21 a number of gender inequalities in health and health behavior were identified, with gender differences increasing with AYA age in the United States and worldwide. Finally, minority parents often report that providers rarely understand their children’s needs and tended to engage in “overdiscussion” of topics that may reflect stereotyping (e.g., community violence and substance use).22 Thus, it is crucial to identify potential groups at higher risk for poorer communication during this crucial stage of transition.
This study was designed to evaluate provider communication during medical visits for AYAs with CKD and their parents using an adapted measure that evaluates communication skills recommended by the Calgary-Cambridge Guides. Specifically, we aimed to: 1) describe provider communication skills in pediatric subspecialty visits where AYAs receive chronic illness care; and 2) determine if communication skills differ by AYA characteristics (age, gender, race).
2. METHODS
2.1. Study Design, Participants, and Data Collection
The data for this study was collected as part of the CKD: Hypertension Adherence in Teens (CHAT) study. Adolescents with CKD and their caregivers were recruited from three academic medical centers in the Mid-Atlantic region of the United States. Participants included AYAs 11–19 years old at time of consent with CKD stages 1–5, as well as post-kidney transplant, who had been prescribed an antihypertensive medication for at least 6 months. Patients in the larger study were excluded if they could not comprehend spoken English, had significant developmental delays, had a sibling already enrolled in the study, had undergone kidney transplant within the previous 6 months, were pregnant, or were not willing to use electronic medication monitors. Follow-up medical management visits with pediatric nephrology care providers (“provider”; nephrology physician or nurse practitioner) were audiotaped. All patient visits were audio-recorded with the written informed consent of the provider and the AYA and/or caregiver (AYAs provided consent if 18 years or older; if under 18, AYAs provided assent and their caregiver provided consent). Additional details regarding the CHAT study have been previously published.18
2.2. Adapting a Global Coding System for Provider Communication in Pediatric Subspecialty Care
To address our first aim, we adapted the Global Consultation Rating Scale (GCRS) for audiotaped pediatric nephrology care visits under the guidance of the original developers.23 The GCRS was created to reflect the Calgary-Cambridge Guides, a prominently used training system for medical education. 5,9,10 The scale, originally developed for evaluating provider communication during outpatient consultations with adults, encompasses 12 domains (initiating the session (greeting and setting the agenda), gathering information/problem identification, problem exploration, patient’s perspective (impact on life), non-verbal communication, developing rapport, providing structure, correct amount and type of information, aiding accurate recall and understanding, incorporating the patient’s perspective (illness framework), planning and shared decision making, closure) following the flow and structure of the visit and is rated on a three point scale where 0 is “not present/ poor”, 1 is “adequate”, and 2 is “good”.23
Adaptations to the GCRS included adjustments for pediatric subspecialty encounters, removal of a non-verbal communication code due to audio-only data, and the addition of two new codes to (1) assess the medication adherence and medication management conversations separately from problem exploration, and (2) evaluate a final check of understanding and agreement at the end of the visit, separate from closure of the visit. The additional code to evaluate a final check was added to reflect the growing body of literature that assessing understanding and agreement is associated with patient outcomes, including knowledge, self-efficacy and illness-management.24,25 We incorporated an assessment of the developmental appropriateness of conversation into evaluations of each domain of interaction. For each domain, we assessed whether providers acknowledged both the AYA as well as caregiver(s) using language that was relatively appropriate for each of their communication and knowledge capacity (for instance, speaking solely with a caregiver and not the AYA cannot earn a score of 2/“good”). Our final adaptation with illustrative examples of each is shown in Table 1.
Table 1:
Global Codes and Examples for Pediatric Subspecialty Care
| DOMAIN | DESCRIPTION | EXAMPLES | |
|---|---|---|---|
| 1 | Initiating the Session | Greets caregiver and child, engages in social niceties. Attends to patient comfort | 0: Disorganized or dismissive; explicitly ignores the child 1: “Hi. How are y u?” 2: “Good to see you, [patient] and [parent]. Come have a seat. How have you been?” |
| 2 | Gathering Information/ Problem Identification | Reviews prior plan/ issues; screens for new concerns. Listens attentively, leaves space for patients to talk | 0: Does not sufficiently allow time/ space for patient to tell his/her story; interrupts patient 1: “Any headaches recently?... Vomiting?... Blood in your urine?” 2: “What concerns or new problems are you having? Tell me more about that.” |
| 3A | Problem Exploration and Med Reconciliation | Appropriately uses open and closed questions- fa.qitates patienťs responses e.g., silence, repetition (includes med reconciliation) | 0: Not present OR mostly closed-ended questions; no space for patient; uses jargon 1: “Okay, but you’re better now?” “How many milligrams are you taking?” 2: “You felt dizzy all day...Tell me what else happened...”. “Let’s go through your medications. Tell me what you can think of’. |
| 3B | Adherence/ Med Management Conversation | Discussion about adherence is permissive and open; may also explore how m 'dication is, onitored/ managed | 0: No conversation OR negative/judgmental (“You really can’t miss a dose”) 1: “You haven’t missed any doses, right?”; “Are you taking them all?” 2: “About how many doses do you miss in a week?” “Who helps you remember?” |
| 4 | Patient’s Perspective | Perspective specif.allj about impact on life/functioning. Actively determines patienťs perspective ideas, concerns, expectations, feelings, effects on life. | 0: No conversation, does not elicit from patient, patient does not share perspective 1: “Okay”. 2: “What are your thoughts about your CKD?”, matches the patient’s interest, health literacy, and developmental/cognitive capacity. |
| 5 | (Non-Verbal Communication) | Not coded for audio data | Not coded for audio data |
| 6 | Developing/ Maint ining Rapport | Engages adolescent appropriately. Sensitive to patient’s feelings/ views. Empathic, non-judgmental | 0: Does not acknowledge patient’s views/feelings or is judgmental/dismissive 1: “Yeah that can hurt sometimes” 2: “I’m sorry to hear you’re going through this. Let’s find some ways to make it better.” |
| 7 | Providing Structure | Uses signposting, includes rationale for next section; Structures interview in logical sequence, attends to timing (but not rushed), keeps interview on task. | 0: Disorganized flow or structure is ineffective (rushed, distracted) 1: There is a general flow but may be passively created or inconsistent 2: “First let’s talk about how you’re feeling, and then I’ll examine you.” |
| 8 | Correct Amount/ Type of Info | Chunks information; Seeks and addresses patienťs info needs; Tailors explanation to patient level; Uses clear language, avoids jargon | 0: Provides too much/too little/inappropriate information for patient’s needs; uses jargon 1: Info is somewhat tailored for level of understanding/needs, but is not consisted. 2: “There are a few things that might be going on. Would you like to hear m—e a, out?” |
| 9 | Aiding Accurate Recall & Understanding | Checks patienťs understanding (good if asks patient to restate information given) | 0: Does not assess understanding and/or seems insensitive to signs of patient confusion 1: “Ok?”...”Right?” 2: “So what should you do to clean the catheter again?...Any questions?” |
| 10 | Incorporating the Patient’s Perspective | Relates explanations to patienťs illness framework; Encourages patient to contribute reactions, feelings, and own ideas; Picks up and responds to patienťs covert verbal cues | 0: Does not ask for patient’s perspective or does not incorporate it into planning 1: “I know you don’t like that medicine but you really need to take it”. 2: “We should think about getting on the transplant list as an option in the future. You look surprised about this. What are your concerns?” |
| 11 | Planning and Shared Decision-Making | Explores management options with patient; Involves patient in decision making; Appropriately negotiates mutually acceptable plan | 0: “That’s my plan and I’m sticking to it” 1: “Can you agree to do what I am recommending?” 2: “Here is what I am proposing and I’d like to hear your thoughts”. |
| 12A | Closure | Contracts with patient re next steps; Summarizes session briefly and clarifies plan f care | 0: “The front desk will check you out and get you scheduled” 1: “So you’ll increase your dose and come back in 6 months” 2: “I think you’re doing really well. We have decided to increase your dose and see how that goes for 6 months. But let me know if you have any concerns before then, okay?” |
| 12B | Check understanding/ Agreement of final plan | Final check of patient’s understanding or agreement about the plan discussed with an opportunity for the patient to respond. | 0: No final check of patient’s understanding or agreement OR no opportunity to respond 1: “Okay?”, “Make sense?” “Any questions?” 2: “So tell me what we’re planning to do moving forward. What questions can I answer?” |
| 13 | Overall Rating of Consultation | Considering only communication skills: Does the provider appear qualified to be a clinician? | 0: definitely not; 1: probably not; 2: yes, but only barely, 3: well qualified, 4: exceptionally well-qualified/nearly perfect (optimal according to criteria- not norm-based) |
Note. “Patient” refers to adolescent and young adults (AYA) and/or caregiver. Provider must engage with both AYA and caregiver at a developmentally appropriate level to earn a score of 2 on any given code.
Two researchers (SS and WC) used the audio from the original GCRS training videos to achieve reliability with each other and with the master codes provided by the GCRS developers. We discussed our scores and adapted the GCRS manual to better reflect communication occurring in the pediatric visits.
2.3. Communication Coding
Once the adapted coding manual was finalized and reliability was achieved (average inter-coder agreement of at least r =.70), all tapes were coded using the finalized adapted global coding system. Twenty percent of the tapes were double-coded, discussed, and mutually agreed upon. For each visit, an average rating score was computed for all domains coded. Average inter-coder agreement for categories coded (r M(SD)=0.74 (0.16), range 0.44 (patient’s perspective) −1.00 (problem exploration)) and percent agreement of individual visits (M(SD)=75.24 (11.53), range 57.10–100%) were good. Coders also noted examples of communication dialogue they felt were representative of the coding system to provide qualitative contextual detail, which are presented in Table 1.
2.4. Data Analysis
All analyses were conducted using SPSS v24 (SPSS Inc, Chicago, IL). Distribution and spread of scores were examined for each communication domain using descriptive statistics. To address our second aim, we evaluated categorical differences in the distribution of GCRS scores based on AYA age, race, and gender (“characteristics”) using chi-square analyses. Additional linear mixed models were conducted to account for nesting of patients within provider, to control for provider gender, and to test for differences in the average communication score, a continuous measure. For each communication domain, a linear mixed model was computed using the “MIXED” command, the communication domain entered as a continuous dependent variable, AYA characteristics and provider gender entered as fixed effects, and provider study identifier entered as a random effect. Estimated marginal means were computed for each AYA characteristic.
3. RESULTS
3.1. Provider and AYA Characteristics
AYA characteristics are shown in Table 2 and provider characteristics are shown in Table 3. Of 102 audiotaped visits, 3 had less than 50% of the visit recorded and were deemed incomplete, resulting in a final sample size of 99. Visits lasted an average of 32 (SD=18) minutes. Participants included 18 providers, 99 AYAs and 96 caregivers. The mother was the caregiver present at the majority of appointments (n=80, 81%). Three AYAs attended clinic alone, without a caregiver. Mean AYA age at the visit was 14.9 years, half of AYAs were African American, and slightly more than half were male. Of the 18 providers, the majority were female (n=13, 72%) and Caucasian (n=10, 56%), and similarly, the majority of visits were completed by female and Caucasian providers (73% and 69%, respectively). Providers completed up to 14 individual visits, whereas some saw as few as a single visit. The over-representation of female, Caucasian, and attending nephrologist providers precluded explicit investigation of communication differences based on provider characteristics because the subgroups to be compared would yield insufficient power to reliably detect differences.
Table 2:
Patient Demographics (N=99)
| M (SD) | N | % | |
|---|---|---|---|
| AYA Age | 14.9 (2.6) | ||
| AYA Race | |||
| African American | 51 | 52% | |
| Caucasian | 39 | 40% | |
| Asian | 4 | 4% | |
| Native Hawaiian/Pacific Islander | 1 | 1% | |
| Other | 4 | 4% | |
| AYA Gender | |||
| Male | 54 | 55% | |
| Female | 45 | 46% | |
| AYA Health Status | |||
| Post-transplant | 23 | 23% | |
| ESRD | 24 | 24% | |
| Hypertension diagnosis | 38 | 38% | |
| Obese (BMI > 95th %ile) | 32 | 32% | |
| Household Income | |||
| <$50,000 | 34 | 34% | |
| $50,000–100,000 | 29 | 29% | |
| ≥$100,000 | 32 | 32% | |
| Not reported | 4 | 4% | |
| Health Insurance | |||
| Public | 41 | 41% | |
| Private | 41 | 41% | |
| Both (Public and Private) | 5 | 5% | |
| Military | 6 | 6% | |
| Unknown/Other | 6 | 6% | |
| Caregiver Relationship to AYA | |||
| Mother | 80 | 81% | |
| Father | 10 | 10% | |
| Other | 6 | 6% | |
| No caregiver present | 3 | 3% | |
Note. AYA = adolescents and young adults; BMI = body mass index.
Table 3:
Provider Characteristics
| Individual Providers (Total N=18) | # Visits (Total N=99) | |||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Gender | ||||
| Male | 4 | 22% | 25 | 25% |
| Female | 14 | 78% | 74 | 75% |
| Race | ||||
| Caucasian | 11 | 62% | 70 | 71% |
| Asian | 6 | 33% | 26 | 26% |
| African American | 1 | 6% | 3 | 3% |
| Role | ||||
| Attending Nephrologist | 14 | 78% | 95 | 96% |
| Nephrology Postdoctoral Fellow | 3 | 17% | 3 | 3% |
| Nurse Practitioner | 1 | 6% | 1 | 1% |
3.2. Communication Characteristics
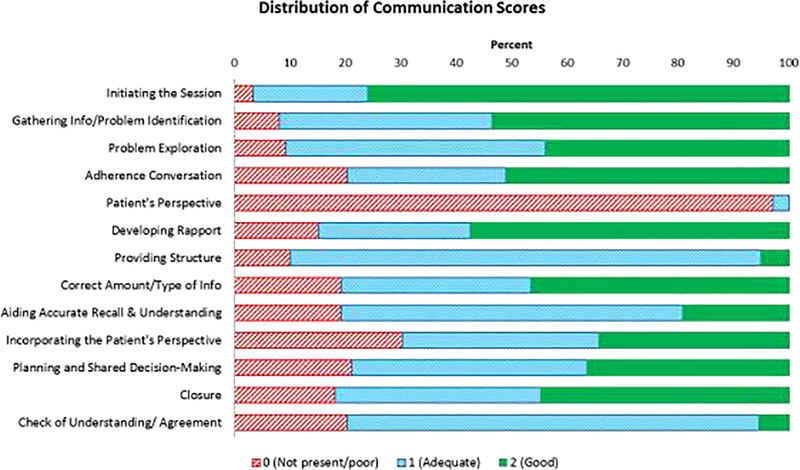
Providers, on average, were scored highest on initiating the session, gathering information, and developing rapport, and scored lowest on patient’s perspective, checking understanding/agreement, and providing structure. Figure 1 shows the distribution of scores for each proficiency. Specifically, providers tended to earn high scores of 2 on initiating the session (76%) and developing rapport (58%). Additionally, providers were most likely to receive a score of zero (not present or poor, referred to from this point as “poor”) on asking for the patient’s perspective, with providers in 97% of visits failing to ask for either the parent or patient’s opinion about his or her CKD. Related, providers in 30% of visits received poor scores for incorporating the patient’s perspective into treatment planning. Other skills with high frequencies of missing or poor scores included planning and shared decision-making (21%) and checking understanding/ agreement (20%). In fact, providers in only 5% of visits explicitly checked understanding and agreement with the treatment plan at the end of the visit (e.g. using teach-back26) while the remaining simply asked “Okay?” or “Sound good?”.
Figure 1.
Overall Distribution of Communication Scores
The structure of the visit was predominantly scored as adequate (n=85%). Providers who received a “good” score (5%) provided explicit structuring and “signposting” (using statements to introduce and orient the patient to the next topic: e.g. “Let’s talk about options now”). In fifty-one percent of visits, providers assessed adherence in a permissive way that normalized missed doses (e.g. “Have you missed any doses?”)27 and often asked about how caregivers monitored medication use. Of the remaining visits, 29% only briefly assessed adherence, often by using leading questions (e.g., “you’re taking all of your medicine, right?”), and 20% did not ask about adherence at all despite the fact that all participants were prescribed at least an antihypertensive medication.
3.3. Communication Differences by Patient Characteristics
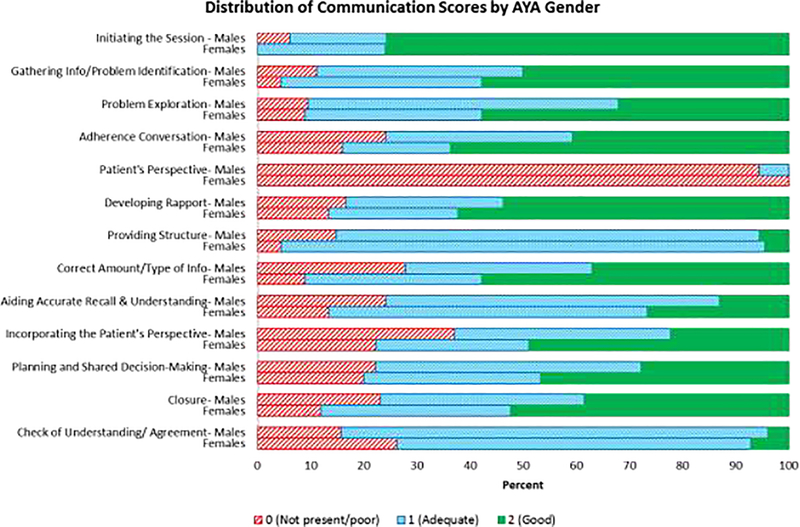
There were no significant differences in communication skills by AYA age or race (data not shown). However, gender differences were present on five out of 12 communication domains. Providers scored significantly higher with female AYAs than male AYAs on: problem exploration (M = 1.49 vs 1.23 respectively, p = 0.03), correct amount/ type of info M = 1.49 vs. 1.09, p = 0.03), and incorporating patient’s perspective (M = 1.27 vs. 0.85, p=0.02) The overall rating was similarly higher for female vs. male AYAs at 2.25 and 1.87 respectively (p = 0.01). In addition, the average rating across all 12 domains was higher in visits with female AYAs than male AYAs with means of 1.19 vs. 0.97 (p<0.01). These differences were maintained in linear mixed models accounting for provider gender and nesting of visits within provider. As shown in Figure 2, interactions with male AYAs tended to have more domains rated “not present/poor” (0) as well as fewer visits rated “good” (2), reflecting a downward shift in scores compared to visits with female AYAs.
Figure 2.
Distribution of Communication Scores Stratified by AYA Gender. AYA=Adolescent and Young Adult
4. DISCUSSION AND CONCLUSION
4.1. Discussion
We observed several areas of high proficiency in provider communication such as initiating the session, gathering information, and developing rapport, whereas skills central to patient-centered care26 as well as adherence assessment were not consistently demonstrated. Although communication did not differ by AYA age or race, providers earned higher communication scores during visits with female AYAs compared to males. This study provides novel observations about provider communication skills with AYAs and raises questions about the delivery of patient-centered care to males in pediatric subspecialty clinics.
Visits tended to be natural, without clear disorganization but also few instances of overt imposition of structure. They often used a friendly and warm communication style that appeared to put their patients at ease. Although less frequently rated as “good”, providers were nearly always scored as at least “adequate” in exploring the presenting problem and providing structure. This may indicate that providers used more overt means to explore a problem only when concerns were voiced by patients.
In contrast to strengths observed in some areas, more than half of visits were scored below the “good” rating for shared decision-making and incorporating the patient perspective. Shared decision-making that earned “good” scores welcomed and/or explicitly asked for feedback (e.g., “The question is whether this is the right dose for you…I’m going to need your input on that”). Providers rated as “poor” in shared decision-making and/or checking understanding did not ask for input from the AYA or caregiver. As all visits were follow-up appointments, it is likely that there were no recommended changes to the treatment regimen and therefore providers did not see a need to solicit feedback or understanding. Indeed, previous studies show that parents and providers conceptualize shared decision-making differently: parents see it as partnership between two equal parties, while providers view it as a way of convincing parents to agree with the providers’ plan.28 However, the creators of the GCRS have emphasized the importance of continuous shared decision-making at every visit. Failure to ensure understanding and agreement of the plan at each visit could interfere with patient-centered care,12 especially patient education, active participation, and adherence.8,29 Related, there is growing evidence that using “teach back” to assess understand is associated with higher patient knowledge and self-efficacy, and better adherence and health outcomes.24,25 Notably many providers think they are using “teach back” when they are not.30 Fortunately, it is a skill that can be taught in a brief training30 and is therefore a practical intervention that can improve provider communication.
Despite all AYAs being prescribed medication, one-fifth of visits did not address adherence at all and over one-quarter of visits had brief conversations that precluded discussion about barriers to adherence. In nearly half of visits, providers assessed adherence in a manner that was not permissive for patients to admit nonadherence (e.g., “You’re taking all your medicine, right? You’re not missing any doses?”), if it was asked at all. Providers may have relied on nursing staff to conduct medication reconciliation, which eliminates opportunity to discuss medication issues or assess adherence. Although physicians tend to acknowledge the importance of discussing medication adherence with patients, in practice this aspect of conversation is commonly neglected31 and as a result, they may not attain a reliable estimate of adherence.32
We did not observe any communication differences based on AYA age or race, controlling for provider gender, suggesting consistency across the developmental period of adolescence and young adulthood and no evidence of racial bias. The lack of age differences is not surprising because coders accounted for the developmental appropriateness of provider communication strategies. Additionally, African American adult males with CKD are at elevated risk for faster progression of their disease and poorer hypertension control compared to Caucasians and women.33 Therefore, male AYAs may be in a particularly sensitive period for laying the foundation for long-term CKD self-management. In this study, providers treating female AYAs, regardless of race, were more likely to engage in thorough exploration of presenting problems and medication regimens, openly discuss adherence in a nonjudgmental manner, provide tailored medical information, explicitly evaluate and aid understanding of information, incorporate the patient’s perspective in treatment planning, and provide a comprehensive closure that includes a summary of the plan and next steps. The current coding system uses a “0” rating regardless of whether proficiency was absent (e.g., not assessing patient preferences) or whether it was executed inadequately (e.g., ignoring patient preferences). Therefore, although we detected more highly rated communication with female AYAs, further work will need to build upon these findings to identify whether communication skills were weak or less likely to be exhibited altogether.
There are several possible explanations for gender differences in provider communication. Female AYAs may elicit a more open communication style from providers.34 Adolescents also report a preference towards gender congruent providers;35 therefore, males may be less comfortable discussing their health with female providers. Further, in adults, females tend to score more highly on measures of narrative autobiographical memory.36 Thus, perhaps male AYAs are less likely to provide details regarding their medical history and may elicit narrower communication from providers. Regardless, missing or insufficient provider communication skills could have substantial negative ramifications on the quality of care received by males. According to the WHO,21 gender differences in AYA health are likely indicative of unique issues of concern for males compared to females, rather than one gender being at risk for poorer overall health. Male AYAs may have fewer health complaints to report to providers, or are reluctant to discuss them.21 Additional study is needed to more thoroughly understand the nature of gender differences in communication within pediatric subspecialty settings and the extent to which it may be associated with health consequences and inequalities.
As with all studies, several limitations should be considered in interpreting our results. First, observing providers who were aware of being audiotaped for research may have altered their behavior due to the Hawthorne Effect. Anecdotally, providers reported they were surprised how little they noticed the recorder. If behavior was altered, our results may simply be a conservative estimate of relative weaknesses in provider communication; they may in fact perform more poorly in daily practice when not recorded. Second, communication scoring was completed by two female coders who may have had implicit gender biases affecting scoring. A carefully crafted scoring manual was used to minimize any potential biases. Future studies should use a combination of male and female coders and may benefit from assessing implicit coder gender bias. Third, we could not thoroughly evaluate provider gender differences or gender concordance due to insufficient power to detect differences between subgroups. Only four (22%) providers were males, comprising only 25 (25%) of all visits. However, in our linear mixed models, we did control for nesting of visits within provider as well as provider gender to mitigate potential effects from individual provider differences. Fourth, availability of audio data precluded observation of nonverbal behavior, which may have limited our evaluations of interactions during visits. Fifth, as noted above, communication skills outlined by the GCRS have not yet been tested for associations with health outcomes. Finally, as this was a study of AYA subspecialty care, the communication skills observed may not generalize to primary care or care for other age groups.
Current measures and definitions of “good communication” are rooted in theory rather than being research-derived.37 For example, while theory suggests using open-ended questions indicates good communication, we do not know if open-ended questions lead to greater patient satisfaction or better outcomes. Indeed, the Calgary-Cambridge guides operate under the assumptions that (1) there are key elements of good provider communication that should be present in all medical consultations, (2) providers should actively engage in executing those communication elements, and (3) that trained coders have the ability to reliably assess these skills. While there is growing theoretical and research supporting the Calgary Cambridge Guides and related assessment tools,5,38,39, the assumptions inherent in the Calgary Cambridge Guides have been questioned by others40,41 As the evidence for which communication skills are linked with positive health behaviors and outcomes grows, the GCRS will need to be adapted.
4.2. Conclusion
In this study of provider communication skills in AYA nephrology care using an adapted GCRS coding system based on the Calgary-Cambridge Guides, 5,9,10,23 coders detected variability in provider communication skills. Few providers explicitly checked for patient agreement or understanding of the plan, which has been identified as a key factor of patient-centered care11,26. In addition, there is significant room for increased incorporation of the patient and family’s perspective and engagement in shared decision-making. Most current definitions of communication skills are theoretically derived (including the Calgary-Cambridge Guides) and future research is needed to elucidate the elements of communication that practically impact patient satisfaction, adherence, and health outcomes. Further, although no age or race differences were observed, providers were more likely to use higher rated communication skills with female AYAs compared to males across several domains. Future work should longitudinally investigate the health implications of these gender differences in communication with the goal of developing targeted interventions42 to minimize disparities and promote optimal care for AYAs with chronic conditions.
4.3. Practice Implications
Our findings indicate that pediatric providers may not achieve optimal communication in a number of areas in chronic illness care for AYAs. Achieving better communication with AYAs is particularly important, as they are at a crucial developmental stage in their medical self-management. Specifically, providers should consider using more patient-centered communication to integrate the patient and family’s perceptions and experience into education and treatment recommendations. This may include asking AYAs about their perspective on their illness, assessing adherence in an open and nonjudgmental manner,27 employing shared decision-making techniques,43 and using the “teach-back” method.26 Finally, while there are no specific guidelines for effective communication with male patients, providers should be aware of the possible need to build rapport more deliberately and to facilitate autobiographical memory encoding and retrieval,36 such as by using repetition and checking of understanding. A sensitive communication style which assesses individual patient needs and adjusts elements of the visit as needed will ensure appropriate, personalized delivery of healthcare with AYAs.
Highlights.
Patient-centered communication is emphasized in medical training and care models.
Structured assessment of provider communication is needed for pediatric care.
Adolescents and young adults (AYAs) are in a developmentally sensitive period.
We evaluated provider communication with AYAs with chronic kidney disease.
Ratings were highest for initiating, gathering information, and developing rapport.
Ratings were lowest for several patient-centered communication skills.
Acknowledgments
This study was conducted using data from the CHAT study (Doctor-Teen Communication and Antihypertensive Adherence in Chronic Kidney Disease) with support from NIH R01 DK092919 (PI: K. Riekert). The funding source has no involvement in the conduct of this research or preparation of the manuscript. We would like to thank our adolescent and young adults, their caregivers, and medical care providers for their participation in this study. Thank you to Dr. Jenny Burt at the Cambridge Centre for Health Services Research, who provided training and mentorship in the adaptation of the coding system.
Funding Source: This study was conducted using data from the CHAT study (Doctor-Teen Communication and Antihypertensive Adherence in Chronic Kidney Disease) with support from NIH R01 DK092919 (PI: K. Riekert). The funding source has no involvement in the conduct of this research or preparation of the manuscript.
Abbreviations
- AYAs
Adolescents and young adults
- CKD
Chronic kidney disease
- CHAT
CKD: Hypertension Adherence in Teens
- GCRS
Global Consultation Rating Scale
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: None of the authors have any conflicts of interest, including financial interests or gains.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Institute of Medicine. Coverage Matters: Insurance and Health Care. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- [2].Brown RF, Bylund CL. Communication skills training: describing a new conceptual model. Acad Med J Assoc Am Med Coll. 2008;83(1):37–44. [DOI] [PubMed] [Google Scholar]
- [3].Makoul G Communication skills education in medical school and beyond. JAMA. 2003;289(1):93–93. [DOI] [PubMed] [Google Scholar]
- [4].Education Accreditation Council for Graduate Medical Education. Advancing education in interpersonal and communication skills: an educational resource from the ACGME Outcome Project. ACGME Outcome Proj Chic IL. 2005. [Google Scholar]
- [5].Kurtz S, Silverman J, Benson J, Draper J. Marrying content and process in clinical method teaching: enhancing the Calgary–Cambridge guides. Acad Med. 2003;78(8):802–809. [DOI] [PubMed] [Google Scholar]
- [6].Makoul G The SEGUE Framework for teaching and assessing communication skills. Patient Educ Couns. 2001;45(1):23–34. [DOI] [PubMed] [Google Scholar]
- [7].Tulsky JA, Beach MC, Butow PN, et al. A Research Agenda for Communication Between Health Care Professionals and Patients Living With Serious Illness. JAMA Intern Med. 2017;177(9):1361–1366. [DOI] [PubMed] [Google Scholar]
- [8].Haskard Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: A meta-analysis. Med Care. 2009;47(8):826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kurtz SM, Silverman JD. The Calgary—Cambridge Referenced Observation Guides: An aid to defining the curriculum and organizing the teaching in communication training programmes. Med Educ. 1996;30(2):83–89. [DOI] [PubMed] [Google Scholar]
- [10].Silverman J The Calgary Cambridge Guides: The ‘teenage years.’ Clin Teach. 2007;4(2):87–93. [Google Scholar]
- [11].Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: Theoretical and practical issues. Soc Sci Med 1982. 2005;61(7):1516–1528. [DOI] [PubMed] [Google Scholar]
- [12].Committee on Hospital Care, Institute for Patient and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404. [DOI] [PubMed] [Google Scholar]
- [13].American Medical Association. An Ethical Force Program Consensus Report: Improving Communication - Improving Care. Chicago, Illinois: 2006. [Google Scholar]
- [14].Mahan JD, Warady BA, Committee C. Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol. 2006;21(7):917–930. [DOI] [PubMed] [Google Scholar]
- [15].Wong CJ, Moxey-Mims M, Jerry-Fluker J, Warady BA, Furth SL. CKiD (CKD in Children) Prospective Cohort Study: A Review of Current Findings. Am J Kidney Dis. 2012;60(6):1002–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fadrowski J, Cole SR, Hwang W, et al. Changes in physical and psychosocial functioning among adolescents with chronic kidney disease. Pediatr Nephrol. 2006;21(3):394–399. [DOI] [PubMed] [Google Scholar]
- [17].Duquette PJ, Hooper SR, Wetherington CE, Icard PF, Gipson DS. Brief Report: Intellectual and Academic Functioning in Pediatric Chronic Kidney Disease. J Pediatr Psychol. 2007;32(8):1011–1017. [DOI] [PubMed] [Google Scholar]
- [18].Coburn SS, Eakin MN, Roter D, et al. Patient-provider communication in nephrology care for adolescents and young adults. Patient Educ Couns. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Schouten BC, Meeuwesen L. Cultural differences in medical communication: A review of the literature. Patient Educ Couns. 2006;64(1–3):21–34. [DOI] [PubMed] [Google Scholar]
- [20].Tsay S-L, Hung L-O. Empowerment of patients with end-stage renal disease--a randomized controlled trial. Int J Nurs Stud. 2004;41(1):59–65. [DOI] [PubMed] [Google Scholar]
- [21].Inequalities in young people’s health. HBSC international report from the 2005/2006 survey. March 2017. [Google Scholar]
- [22].Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2):e183–e193. [DOI] [PubMed] [Google Scholar]
- [23].Burt J, Abel G, Elmore N, et al. Assessing communication quality of consultations in primary care: initial reliability of the Global Consultation Rating Scale, based on the Calgary-Cambridge Guide to the Medical Interview. BMJ Open. 2014;4(3):e004339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14(1):210–247. [DOI] [PubMed] [Google Scholar]
- [25].Hong Y-R, Cardel M, Suk R, et al. Teach-Back Experience and Hospitalization Risk Among Patients with Ambulatory Care Sensitive Conditions: a Matched Cohort Study. J Gen Intern Med. 2019;34(10):2176–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff Proj Hope. 2010;29(7):1310–1318. [DOI] [PubMed] [Google Scholar]
- [27].Callon W, Saha S, Korthuis PT, et al. Which Clinician Questions Elicit Accurate Disclosure of Antiretroviral Non-adherence When Talking to Patients? AIDS Behav. October 2015:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fiks AG, Hughes CC, Gafen A, Guevara JP, Barg FK. Contrasting parents’ and pediatricians’ perspectives on shared decision-making in ADHD. Pediatrics. 2011;127(1):e188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].DiMatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Couns. 2004;55(3):339–344. [DOI] [PubMed] [Google Scholar]
- [30].Feinberg I, Ogrodnick MM, Hendrick RC, Bates K, Johnson K, Wang B. Perception versus reality: The use of teach back by medical residents. Health Lit Res Pract. 2019;3(2):e117–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hines R, Stone NJ. Patients and physicians beliefs and practices regarding adherence to cardiovascular medication. JAMA Cardiol. 2016;1(4):470–473. [DOI] [PubMed] [Google Scholar]
- [32].Pruette CS, Coburn SS, Eaton CK, et al. Does a multimethod approach improve identification of medication nonadherence in adolescents with chronic kidney disease? Pediatr Nephrol. August 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Duru OK, Li S, Jurkovitz C, et al. Race and sex differences in hypertension control in CKD: results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis. 2008;51(2):192–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Roter D, Hall JA. Doctors Talking with Patients/Patients Talking with Doctors: Improving Communication in Medical Visits. Greenwood Publishing Group; 2006. [Google Scholar]
- [35].Bernzweig J, Takayama JI, Phibbs C, Lewis C, Pantell RH. Gender differences in physician-patient communication: evidence from pediatric visits. Arch Pediatr Adolesc Med. 1997;151(6):586–591. [DOI] [PubMed] [Google Scholar]
- [36].Grysman A Gender and gender typicality in autobiographical memory: A replication and extension. Mem Hove Engl. 2018;26(2):238–250. [DOI] [PubMed] [Google Scholar]
- [37].Tulsky JA, Beach MC, Butow PN, et al. A research agenda for communication between health care professionals and patients living with serious illness. JAMA Intern Med. 2017;177(9):1361–1366. [DOI] [PubMed] [Google Scholar]
- [38].Burt J, Abel G, Elliott MN, et al. The evaluation of physicians’ communication skills from multiple perspectives. Ann Fam Med. 2018;16(4):330–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Burt J, Abel G, Elmore N, et al. Rating communication in gp consultations: The association between ratings made by patients and trained clinical raters. Med Care Res Rev. 2018;75(2):201–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Street RL, De Haes HCJM. Designing a curriculum for communication skills training from a theory and evidence-based perspective. Patient Educ Couns. 2013;93(1):27–33. [DOI] [PubMed] [Google Scholar]
- [41].Salmon P, Young B. Creativity in clinical communication: from communication skills to skilled communication. Med Educ. 2011;45(3):217–226. [DOI] [PubMed] [Google Scholar]
- [42].Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a patient-centered communication intervention on oncologist-patient communication, quality of life, and health care utilization in advanced cancer: The VOICE randomized clinical trial. JAMA Oncol. 2017;3(1):92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lipstein EA, Dodds CM, Britto MT. Real life clinic visits do not match the ideals of shared decision making. J Pediatr. 2014;165(1):178–183.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]