Abstract
Purpose of Review.
An increasing body of evidence indicates that persons living with HIV (PLWH) display dysfunctional immunometabolism. Here we provide an updated review of this topic and its relationship to HIV-associated immune stimuli and age-related disease.
Recent Findings.
HIV infection alters immunometabolism by increasing reliance on aerobic glycolysis for energy and productive infection and repurposing oxidative phosphorylation machinery for immune cell proliferation and survival. Recent studies in PLWH with diabetes mellitus and cardiovascular disease have identified an association with elevated T cell and monocyte glucose metabolism, respectively. Immunometabolic dysfunction has also been observed in PLWH in frailty and additional studies suggest a role for immunometabolism in non-AIDS defining cancers and neurocognitive disease. There is a plethora of HIV-associated immune stimuli that could drive immunometabolic dysfunction and age-related disease in PLWH but studies directly examining their relationship are lacking.
Summary.
Immunometabolic dysfunction is characteristic of HIV infection and is a potential link between HIV-associated stimuli and age-related comorbidities.
Keywords: HIV, Antiretroviral Therapy, Immune Activation, Immunometabolism, Glycolysis, Oxidative Phosphorylation
Introduction
Immune activation and inflammation are fundamental components in the pathogenesis of HIV infection that persists in antiretroviral therapy (ART)-treated people living with HIV (PLWH), even those receiving ART treatment during acute infection [1–4]. Non-AIDS comorbidities that typically manifest with advancing age have become increasingly common in the ART era [5,6], with many of these comorbidities showing associations with immune activation [7,8]. The drivers of immune activation are likely multifactorial and even with the advent of a sterilizing or functional cure could persist, as exemplified by elite controllers that display elevated immune activation compared to healthy controls [9].
Unlike most other cells within the body, many types of immune cells demonstrate the ability to switch their metabolic program when activated to generate energy and synthesize the machinery needed to achieve efficient immune function [10]. Key metabolic pathways implicated include glycolysis, glutaminolysis, fatty acid oxidation, and oxidative phosphorylation; with various fuel sources utilized to produce the intermediates necessary for each pathway. Alteration of immune cell metabolic programming that affects these pathways can result in alteration of immune function. These findings have led to the burgeoning field of immunometabolism that has only recently emerged as a major area of research in the context of HIV infection. Here we review the immunometabolic dysfunction associated with HIV infection and how this relates to drivers of immune activation and major age-related comorbidities.
Immunometabolism in PLWH
Gene expression and metabolites of carbohydrate metabolism, amino acid metabolism, oxidative phosphorylation (OXPHOS) and the tricarboxylic acid (TCA) cycle are associated with immune activation and disease progression in PLWH [11,12,13••], highlighting the important role of immunometabolism during HIV infection. In the last decade, an increasing number of studies have examined the immunometabolic dysfunction characteristic of HIV infection. These studies are discussed below and summarized in Table 1.
Table 1.
Summary of dysfunctional immunometabolism in HIV infection
| Metabolic Modulation | Cell Type | Implications for PLWH | References |
|---|---|---|---|
| Increased glucose uptake and expression of GLUT1 and HK1 | CD4+ T cells, CD14+CD16+ Monocytes, Macrophages |
Productive infection and susceptibility to infection | Palmer, 2013; Palmer, 2014; Hegedus, 2014; Loisel Meyer, 2012; Barrero, 2013; Masson, 2017 |
| Activation | |||
| Secretion of inflammatory cytokines | |||
| Decline in CD4 count | |||
| Increased lactate secretion and expression of LDHA | CD4+ T cells, CD14+CD16+ Monocytes |
Activation | Liao, 2012; Palmer, 2013 |
| Secretion of inflammatory cytokines | |||
| Increased intracellular glutamine | CD4+ T cells, Macrophages | Productive infection | Hegedus, 2017; Datta, 2016 |
| Survival of chronically infected cells | |||
| Increased intracellular glutamic acid and α-ketoglutarate | Macrophages | Survival of chronically infected cells | Datta, 2016 |
| Increased ROS production | CD4+ and CD8+ T cells, Macrophages | Survival of chronically infected cells | Castellano, 2019; Datta, 2016; Kalinowska, 2013; Masson, 2017 |
| Unresponsiveness to IL-7 | |||
| Increased fatty acid metabolism | Macrophages | Survival of chronically infected cells | Castellano, 2019; Datta, 2016 |
| Increased mitochondrial density and hyperpolarized mitochondria | CD4+ and CD8+ T cells | Increased sensitivity to apoptosis | Kalinowska, 2013; Masson, 2017 |
| Unresponsiveness to IL-7 |
Abbreviations: GLUT1 – Glucose transporter-1; HK1 – hexokinase-1; LDHA – Lactate dehydrogenase A; ROS – reactive oxygen species.
In Vitro Effects of HIV on Monocyte, Macrophage, and T cell Immunometabolism
The susceptibility of CD4+ T cells to HIV infection is primarily governed by the metabolic activity of the cell and, once infected, CD4+ T cell metabolism becomes altered. Glucose is an integral fuel source for HIV-infected CD4+ T cells and is utilized primarily for glycolysis despite the presence of oxygen that can be used for OXPHOS (i.e., aerobic glycolysis) [14•]. Compared to uninfected CD4+ T cells, HIV-infected CD4+ T cells display increased glucose transporter-1 (GLUT1) expression, increased glucose uptake, increased lactate production, and upregulation of the glycolysis enzymes lactate dehydrogenase A (LDHA) and hexokinase-1 [15,16•,17]. The increased reliance on aerobic glycolysis is required for reverse transcription, integration, and virion production [16•,17], identifying the metabolic program of the CD4+ T cell as essential for productive HIV infection. Along these lines, the metabolically active effector memory CD4+ T cell subset is associated with productive infection, whereas naïve and central memory CD4+ T cell subsets are associated with latent infection [16•].
In addition to increased aerobic glycolysis, HIV-infected CD4+ T cells repurpose their metabolic machinery using substrates of the TCA cycle [16•,18•]. The amino acid glutamine is used as a fuel source to repurpose the mitochondrial machinery and has been shown to be required for productive HIV infection [16•,18•]. Fatty acid oxidation was also identified as an energy source available to HIV-infected CD4+ T cells; however, glucose and glutamine are preferred [16•]. The concentrations of TCA cycle metabolites can also be affected by HIV factors. For example, treatment of Jurkat T cells with Tat alters mitochondrial machinery and increases production of succinate and malate in the TCA cycle [19]. A recent study in mice showed that increased CD4+ TH1 cell succinate promotes IFN-γ production and that the mitochondrial malate-aspartate shuttle is essential for gene regulation and proliferation of CD4+ TH1 cells [20].
Monocytes and macrophages can also be permissive to HIV infection. Similar to CD4+ T cells, the metabolic program of macrophages is affected by HIV infection [21•]. U937 monocyte-derived macrophages treated with the HIV viral protein Vpr increase their metabolic activity with increases in the following glycolytic enzymes: the hexokinase 1 (HK1), hexokinase 2 (HK2), glucose-6-phosphate dehydrogenase (G6PD) and pyruvate kinase M2 (PKM2) [22]. However, examination of primary human monocyte-derived macrophages latently infected with HIV did not show alterations in glycolysis, rather, they displayed mitochondrial dysfunction as evidenced by enlarged mitochondria and decreased OXPHOS [21•]. These latently infected macrophages also utilize glutamine as a major energy source [21•]. The use of glutaminolysis has been shown to maintain ROS homeostasis that may promote the survival of HIV infected macrophages [23].
Ex Vivo and In Vivo Effects of HIV on Monocyte, Macrophage, and T cell Immunometabolism
Both T cell and monocyte/macrophage immunometabolism has been assessed in PLWH. Compared to CD4+ T cells from people without HIV, CD4+ T cells and monocytes from treated PLWH have increased markers of activation and increase their reliance on aerobic glycolysis as evidenced by increased expression of GLUT1 and increased lactate production [24,25]. Assessment of monocyte subsets in treated PLWH show that the highest increase in the rate of glycolysis is seen in intermediate monocytes (CD14+CD16+) which have been shown to be pro-inflammatory and are expanded in PLWH [4,25]. These data suggest that the increased aerobic glycolysis in monocytes and T cells may contribute to the low-level chronic inflammation experienced by PLWH on ART. The increased proportion of CD4+ T cells expressing GLUT1 is negatively correlated with total CD4+ T cell percent in treated PLWH but not in people without HIV, providing a potential link between immunometabolism and decline of CD4+ T cells [26,27]. A study examining metabolite levels in plasma from elite controllers that spontaneously lose virological control identified increased lactate levels, indicative of increased aerobic glycolysis during viral rebound and immune dysfunction [13••].
Mitochondria have also been implicated in the dysfunctional immunometabolism in PLWH. GLUT1 expression on CD4+ T cells is associated with increased mitochondrial density and membrane potential in treated PLWH [24], but there is a decreased oxygen consumption rate (OCR), indicating a repurposing of the mitochondria in CD4+ T cells from solely oxidative phosphorylation during chronic HIV infection [26,28••]. A possible explanation is the utilization of alternate fuel sources in the TCA cycle as it was observed that the TCA cycle intermediate alpha-ketoglutarate increases along with a decrease in the amino acid fuel source glutamate in the plasma of elite controllers that lose virological control [13••]. Dysfunctional mitochondria can result in increased reactive oxygen species (ROS) production and oxidative stress. HIV-specific CD8+ T cells from PLWH have increased mitochondrial mass and ROS production compared to CD8+ T cells from people without HIV [29]. In CD4+ T cells and CD8+ T cells, oxidative stress is associated with IL-7 unresponsiveness, a lower CD4 count and increased production of cytokines [30].
Effects of HIV on Immunometabolism of Other Immune Cells
In addition to monocytes, macrophages and T cells; NK cells and B cells also play a pivotal role in controlling an HIV infection but there is a paucity of immunometabolism data for these cells in PLWH. When compared to T cells, peripheral NK cells and B cells from ART naïve PLWH are less bioenergetic, however, both are able to undergo metabolic reprogramming to achieve efficient function [28••,31,32]. A recent report shows that NK cells from untreated PLWH have decreased oxidative phosphorylation and glycolysis compared to people without HIV but there was no difference between treated PLWH and people without HIV [28••]. However, it has been shown that NK cells require prolonged stimulation in the presence of IL-15 to observe any metabolic differences with the method used [32]. Similar to NK cells, peripheral B cells showed no difference in either oxidative phosphorylation or glycolysis when comparing either treated or untreated PLWH with people without HIV, but B cell metabolic reprogramming has been shown to be influenced by the microenvironment and the immunogenic stimulant which can be very different in vivo [28••]. These data highlight the need for more studies to further classify the metabolic program of NK cells and B cells in PLWH.
Factors Contributing to Dysfunctional Immunometabolism in PLWH
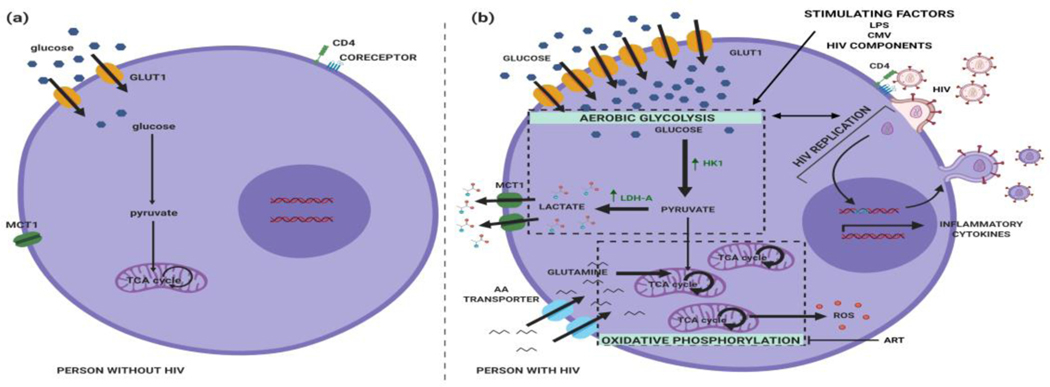
Treatment of PLWH does not completely normalize immunometabolism to levels of healthy people without HIV [24,25]. This is likely due to a combination of different immune stimulating factors that may include microbial translocation of immunogenic products from the gut into circulation, chronic co-infection with cytomegalovirus (CMV), residual HIV production, gut microbial dysbiosis, and antiretroviral drugs. Each of these factors could potentially affect the metabolic state of immune cells but most have not been investigated as factors driving immunometabolic dysfunction in PLWH. These factors are described below and a model depicting their effect on the immunometabolism of CD4+ T cells is shown in Figure 1.
Figure 1. Model of CD4+ T cell immunometabolism during HIV infection.
(a) Representation of a resting CD4+ T cell from a person without HIV. In the absence of stimulating factors, glucose is metabolized into pyruvate and is then further metabolized by entering the TCA cycle. Aerobic glycolysis, lactate production, amino acid utilization and production of inflammatory cytokines are absent. (b) Representation of a CD4+ T cell from a PLWH. Aerobic glycolysis may be initiated after stimulation of CD4+ T cells with lipopolysaccharide, cytomegalovirus, HIV components (e.g. Tat and Vpr) and/or replication of HIV. Initiation of aerobic glycolysis is accompanied by increases in glucose consumption, glucose transporter-1 surface expression, hexokinase-1 expression, and lactate dehydrogenase-A expression. HIV infection also augments mitochondrial respiration as CD4+ T cells utilize alternative fuel sources such as glutamine for oxidative phosphorylation and antiretroviral therapy impairs the electron transport chain and increases reactive oxygen species production. These changes in glycolysis and oxidative phosphorylation in CD4+ T cells from PLWH are associated with increased expression of inflammatory cytokines and increased reactive oxygen species. (Abbreviations: AA transporter – amino acid transporter, ART – antiretroviral therapy, CMV – cytomegalovirus, GLUT1 – glucose transporter-1, HK1 – hexokinase-1, LDH-A – lactate dehydrogenase-A, LPS – lipopolysaccharide, MCT1 – monocarboxylate transporter 1/2, ROS – reactive oxygen species, TCA cycle – tricarboxylic acid cycle)
Microbial Translocation
During HIV infection the gastrointestinal mucosa undergoes irreversible damage [33–35]. The damaged mucosal barrier allows low levels of microbial components and microbes themselves to traverse the mucosa in a process referred to as microbial translocation (reviewed [36]). As microbes and some components of microbes are recognized by pattern recognition receptors (e.g., toll-like receptors) that stimulate immune cells, they could potentially serve as a chronic source of low-level immune stimulation. Both LPS and markers of immune activation are elevated in PLWH, and although reduced with antiretroviral therapy, both remain elevated compared to people without HIV [37]. Studies in acutely SIV-infected pig-tailed macaques show that treatment with sevelamer, a drug that reduces systemic LPS levels, decreases immune activation [38]. In contrast to these studies, microbial translocation is similar between Ugandan children with and without HIV and is not associated with markers of immune activation, indicating that microbial translocation may not be a major cause of immune activation in all settings [39]. In addition, human studies that reduced systemic LPS levels pharmacologically with sevelamer or rifaximin had minimal to no effect on immune activation [7,40]. It remains to be determined whether microbial translocation is linked to immunometabolic perturbations in PLWH.
Microbial Metabolites
In addition to the structural damage that occurs in the gut mucosa, HIV infection also causes microbial dysbiosis in the gut [41–43]. The gut microbiome is less diverse in PLWH and is associated with increased monocyte activation [44]. This microbial dysbiosis is associated with decreased levels of bacteria that produce butyrate [45•], a short chain fatty acid (SCFA) that induces differentiation of regulatory T cells [46,47], and dampens monocyte, macrophage and dendritic cell inflammatory responses [47–49]. Many immune cells express SCFA receptors that, when stimulated, can impact cell function [50]. Administering prebiotics to PLWH can increase butyrate producing bacteria and dampen markers of immune activation [51]. Recently, incubation of human macrophages with butyrate was shown to decrease glycolytic metabolism [52].
Gut microbes can catabolize tryptophan into a number of metabolites that can interact with immune cells. Microbial dysbiosis in the gut of PLWH has been linked to increased microbial tryptophan metabolism and immune activation [41,53]. PLWH have evidence of increased tryptophan catabolism via the kynurenine pathway [54], with a resulting increase in the kynurenine to tryptophan ratio that is associated with atherosclerotic cardiovascular disease (CVD) and type 2 diabetes mellitus (DM) [53,55•]. These tryptophan metabolites have been shown to be active on human T cells, causing decreased differentiation of Th17 cells and increased differentiation of Treg cells [54]. However, a recent study did not identify microbial tryptophan catabolizing enzymes (e.g., IDO-1) in the metatranscriptome of PLWH [56]. These differing results may be due to different study population characteristics. Host cells are also capable of metabolizing tryptophan via the kynurenine pathway, making it less clear if the increased kynurenine to tryptophan ratio observed in PLWH arises from tryptophan catabolism by microbial cells, host cells, or a combination of both.
Trimethylamine-N-oxide (TMAO) is a metabolite produced by select gut bacteria that metabolize choline and L-carnitine. Although most studies show no difference in TMAO levels in PLWH and people without HIV [57,58], TMAO levels in PLWH have been linked to atherosclerotic CVD and immune activation [59–61]. However, not all studies have demonstrated this linkage [57,62,63] and it remains unknown if and how TMAO can affect immune cells.
Cytomegalovirus
CMV infection is nearly universal in PLWH but does not usually cause any overt signs of disease in non-immunosuppressed PLWH [64,65]. A substantial proportion of CD4+ and CD8+ T cells are CMV-specific in PLWH, and although ART treatment alleviates CMV viremia, CMV-specific T cells either remain elevated or even increase [64,66]. In addition to the high level of CMV-specific T cells in treated PLWH, markers of inflammation and immunosenescence are elevated compared to treated PLWH without CMV infection [67,68]. CD8+ T cell markers of immunosenescence are also increased in CMV-infected ART-treated PLWH compared to ART-untreated PLWH, however, they are at levels lower than CMV-infected, people without HIV, raising questions as to the role of CMV-associated immunosenescence in the context of HIV infection [69].
Detection of CMV DNA, but not EBV DNA, in ART-treated PLWH is associated with CD4+ T cell activation [70,71••], indicating that not all herpesviruses are associated with immune activation. Further supporting the role of CMV as a cause of immune activation, valganciclovir treatment of CMV-infected ART-treated PLWH with CD4+ T cell counts <350 cells/mm3 results in a reduction of CD8+ T cell markers of activation [72]. In the same study, valganciclovir had little impact on DNA detection of EBV, HHV-6 and HHV-8, providing further evidence as to the specificity of CMV, and not other herpesviruses, driving T cell activation [72]. How CMV influences immunometabolism in the context of HIV infection has not been examined.
Viral Reservoir
Adherence to contemporary antiretroviral therapy can reduce HIV viral loads to undetectable levels by traditional quantitative assays. However, ultra-sensitive assays that can detect a single viral copy per milliliter show that low levels of virus are detectable for most PLWH [73]. Whether this residual low-level viremia represents production or replication of HIV is not universally agreed upon [74,75]. Regardless, low level viremia detected by ultrasensitive assays is associated with soluble immune activation markers [76], and in poor immunologic responders, associated with cellular immune activation markers [77]. Interestingly, one study showed that CMV- and EBV-specific CD4+ T cells are preferentially infected with latent HIV [78•], linking herpesvirus co-infection with immune activation and potentially virus production. A study that examined virologically suppressed treated PLWH showed a correlation between residual viremia, using an ultra-sensitive assay, and microbial translocation [79]. These studies demonstrate the interrelatedness of factors that may contribute to immune activation and dysfunctional immunometabolism in the context of HIV infection.
Antiretroviral Therapy
ART can have a direct effect on the mitochondrial function of immune cells [28••,80–82,83•]. Nucleoside reverse transcriptase inhibitors (NRTI) are a major cause of T cell mitochondrial dysfunction because they directly inhibit DNA polymerase-γ which is integral for mtDNA replication [84]. The NRTI tenofovir decreases mitochondrial respiration which may be caused by a decrease in expression levels of pyruvate dehydrogenase A (PDHA) and succinate dehydrogenase B (SDHB) [82]. Recent reports show that the effect of ART on mitochondria is not limited to the NRTI class, as integrase strand inhibitors (INSTI) and protease inhibitors (PI) reduce mitochondrial respiration in CD4+ T cells and increase ROS production [28••,85]. CD4+ T cells treated with NRTI, non-nucleoside reverse transcriptase inhibitors (NNRTI), INSTI and PI showed no differences in the expression of HIF1α, GLUT1 or PGK1, suggesting that ART effects on immunometabolism do not involve the glycolysis machinery [28••]. These studies highlight that ART may contribute to dysfunctional immunometabolism through altering mitochondrial function.
Implications of Dysfunctional Immunometabolism to Age-related Diseases
PLWH display an aged immune cell phenotype earlier than age-matched individuals without HIV [86]. In addition, as PLWH live longer due to ART, aging exacerbates chronic immune activation and exhaustion, microbial translocation and dysbiosis, CMV reactivation and immune response [87–91]. Immunometabolism is likely an important mediator of this aging process and associated age-related disease.
Cardiovascular Disease
In the ART era, CVD is a leading cause of morbidity and mortality in PLWH [92]. PLWH, both men and women, are at an increased risk of coronary artery disease and myocardial infarction (MI) [93,94]. Although coronary artery disease is the most frequent form of cardiovascular disease in PLWH, there is also increased risk for other types of cardiovascular diseases, including stroke [94], ventricular dysfunction and heart failure [95], myocardial steatosis and fibrosis [96,97], atrial fibrillation [98], and pulmonary arterial hypertension [99].
Inflammation plays an integral role in the development of atherosclerosis and subsequent cardiovascular events [100]. The association of increased inflammation and the increased risk of CVD has been identified in both individuals without HIV and PLWH, but may be heightened in PLWH [101,102•]. Increased inflammation in PLWH, as measured by plasma levels of sTNFR-I and sTNFR-II, is associated with increased incidence of MI and stroke [7]. Additionally, IL-6, sIL-2R and D-dimer are associated with increased carotid artery intima-media thickness (CIMT) in treated women with HIV [103]. Immune activation is mediated by monocytes/macrophages and T cells as activation of these cell types is associated with the presence of carotid artery lesions and coronary plaques in PLWH [104,105]. Monocytes from PLWH are activated and have elevated prothrombotic tissue factor expression, which exacerbates the development of the atherosclerotic plaque [106,107••]. It is unclear as to the HIV-specific drivers of increased CVD risk, but both LPS and CMV have been directly implicated. LPS was shown to drive immune activation of monocytes and subsequent coagulopathy in an SIV model, thereby linking the microbial translocation product LPS to immune activation and CVD [107••]; and the immune response to CMV is associated with atherosclerotic CVD for PLWH [108–110]. Additionally, TMAO concentration is associated with the number and severity of plaques in PLWH as well as immune activation and inflammation [59,61]. In a population of mostly ART-treated women with suppressed HIV infection, inflammatory monocyte GLUT1 expression was identified to be associated with cardiovascular disease markers and subclinical atherosclerotic cardiovascular disease [111••,112••], linking immune activation, immunometabolism and co-morbid cardiovascular disease.
Diabetes Mellitus
DM is more prevalent in PLWH compared to individuals without HIV, including a higher prevalence for younger non-obese PLWH [113••]. In the United States, DM prevalence for PLWH has increased from ≈ 0% in the pre-ART era to 6.8% ‒11.8% in the modern ART era, highlighting the increasing importance of DM in PLWH [6,113••,114]. Increasing prevalence of type 2 DM in PLWH has also been shown in African countries, with higher prevalence of type 2 DM in PLWH compared to persons without HIV,and an even higher prevalence for untreated PLWH [115]. The increased prevalence of DM in PLWH occurs in the absence of traditional risk factors, indicating the presence of HIV-specific factors in DM development [113••].
DM is now considered an inflammatory disease [116], and in PLWH DM is associated with activation of T cells and monocytes [53,117]. ART-treated PLWH with DM have increased inflammation, expression of CD4+ T cell GLUT1, and increased CD4+ T cell metabolic activity compared to those without DM [118]. Additionally, CD8+ T cells and monocytes from PLWH with DM compared to those without DM have increased expression of GLUT1 (Butterfield TR, unpublished data). In a pathogenic SIV model, increased peripheral CD8+ T cells and increased inflammatory cytokine production was associated with a 2.6-fold decrease in GLUT4 (GLUT most responsive to insulin) expression on adipocytes [119•]. An analysis of insulin resistance in PLWH identified a negative correlation between HOMA-IR and expression of the monocyte electron transport chain (ETC) gene NDUFS7, inflammatory signaling pathway gene MAPK11, and adipokine signaling pathway gene CMKLR1 [120]. These findings provide evidence for immunometabolic perturbations in PLWH with DM and a potential linkage of systemic insulin resistance and the metabolic and activation state of monocytes.
Adipose tissue is an environment of adipocytes closely associated with macrophages and T cells, which communicate via cytokines to either maintain metabolic homeostasis or contribute to metabolic disorders [121,122]. Adipose tissue has been identified to play a key role in the development of insulin resistance, DM and other inflammatory conditions, as well as serving an additional role in PLWH as a possible reservoir for memory CD4+ T cells that harbor HIV [123]. The proportion of activated CD4+ T cells from adipose tissue of PLWH increases with increasing glucose intolerance [124•]. Most of these CD4+ T cells are of the effector memory phenotype which are more responsive to stimulation, suggesting that adipose tissue may provide a setting for chronic stimulation of CD4+ T cells in PLWH [124•]. These memory CD4+ T cells rely heavily on fatty acid oxidation (FAO) for proliferation and survival [10] and the byproducts of FAO, the acylcarnitines, are associated with DM and IR in PLWH [125,126]. Taken together, these findings suggest a role for the interaction between adipocytes and memory CD4+ T cells in the increased risk of DM in PLWH.
The availability and metabolism of amino acids in immune cells has also been shown to be associated with DM in PLWH. The plasma level of tryptophan is decreased, while the Kyr/Trp ratio is increased in PLWH with DM, indicating increased catabolism of tryptophan, though the cell type(s) responsible for the catabolism of tryptophan is unknown [53,127]. Tryptophan catabolism in PLWH with DM is associated with increased inflammation [53,125,127]. CMV-specific antibodies in PLWH have also been linked to inflammation and are associated with insulin resistance, supporting increased inflammation and immune activation with the development of DM in PLWH [128].
Cancer
Mortality from non-AIDS defining cancers (NADC) is increased in PLWH compared to people without HIV, with more severe forms at diagnosis [129,130]. During 2006–2009 in the United States, 10% of mortality in PLWH was attributable to NADC, which increased each year over the study period of 1995–2009 [131]. The incidence of NADC increased from 31.4% in the pre-ART era of 1991 – 1995 to 58% in the early-ART era of 1996 – 2002 [132]. The risk factors for cancers in PLWH include traditional risk factors such as smoking for lung cancer and age for all cancers [131,133,134]. However, when calculated risk is adjusted based on traditional risk factors, PLWH continue to have a higher risk for cancer compared to people without HIV [133,134]. These studies highlight the burden of cancers in PLWH on ART and that there are HIV-specific risk factors for cancer.
Immunometabolic dysfunction and inflammation experienced in PLWH may create an environment that promotes tumor growth. Increased IL-6 plasma concentration is associated with increased risk of developing cancer in PLWH, implicating inflammation in oncogenesis in PLWH [135]. It is believed that pulmonary inflammation and repeated infections result in the increased risk for lung cancer and that the immune dysfunction experienced even on ART plays a role in increased NADC risk [136,137]. In people without HIV an increased Kyr/Trp ratio is also implicated in the immunosuppressive environment that promotes tumor growth but has not been investigated in the context of HIV infection [138]. Furthermore, studies in people without HIV have shown that increasing lactate concentrations suppress the anti-tumor response [139,140], a process that could be exacerbated in PLWH considering the increased aerobic glycolysis [24,25] and plasma concentrations of lactate [13••].
Other Diseases
The age-related diseases discussed above are some of the most common and researched for PLWH, but others such as frailty and HIV-associated neurocognitive disorders (HAND) have also been investigated in the context of immunometabolism. Frailty, a condition characterized by physical slowness, fatigue, low activity, weakness and physical shrinking in the elderly, occurs at a younger age in PLWH [4,141] and is associated with increased measures of inflammation in PLWH [142,143]. Monocyte glycolytic metabolism and activation may be important for the development of frailty in PLWH, as increased expression of GLUT1 on monocytes is associated with frailty in treated PLWH [143,144•]. HIV-associated neurocognitive disorder (HAND) is also a major co-morbid condition in PLWH as more than half of PLWH are affected HAND [145]. Inflammation and viral replication in viral reservoirs appear to be the most integral factors leading to the burden of HAND in PLWH [146,147]. Markers of inflammation, T cell activation, monocyte activation and viral replication are associated with the presence of HIV-associated dementia (HAD) in PLWH [146,147] and CMV antibody response is associated with decreased neurocognitive performance in PLWH [148]. These age-related conditions are important risk factors for each other as it has been shown that neurocognitive decline in PLWH is a risk factor for frailty [149] and CVD and DM are independent risk factors for HAND [150]. This is further underscored by the fact that a number of PLWH present with more than one co-morbid condition [151,152].
Conclusion
HIV immunometabolism studies have increased dramatically in recent times, yet many important questions remain. The relationship between HIV-specific immune stimuli and immunometabolism is unknown and only a very small number of studies have investigated immunometabolism in the context of age-related diseases. Drug targeting of immunometabolism has become a major area of investigation that could have therapeutic potential in the context of age-related disease in PLWH but remains unexplored. Future investigation of these topics will be important to more completely understand the role of immunometabolism in PLWH.
Acknowledgements
This work was supported in part by a UM1 AI106701 award (Alan Landay) and the Office of the Principal of the University of the West Indies, Mona (Joshua Anzinger).
As a Global Infectious Diseases Scholar, Tiffany Butterfield received mentored research training in the development of this manuscript. This training was supported in part by the University at Buffalo Clinical and Translational Science Institute award UL1TR001412 and the Global Infectious Diseases Research Training Program award D43TW010919. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Clinical and Translational Science Institute or the National Institutes of Health.
Footnotes
Compliance with Ethical Standards
Human and Animal Rights and Informed Consent All reported studies/experiments with human subjects performed by the authors have been previously published and complied with all applicable ethical standards.
Conflict of Interest Tiffany R. Butterfield, Alan L. Landay and Joshua J. Anzinger declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
This article is part of the Topical Collection on HIV Pathogenesis and Treatment
REFERENCES
Papers of particular interest, published recently, have been highlighted as:
•Of importance
••Of major importance
- 1.Hunt PW, Martin JN, Sinclair E, Bredt B, Hagos E, Lampiris H, et al. T Cell Activation Is Associated with Lower CD4 + T Cell Gains in Human Immunodeficiency Virus – Infected Patients with Sustained Viral Suppression during Antiretroviral Therapy. J Infect Dis. 2003;187:1534–43. [DOI] [PubMed] [Google Scholar]
- 2.Vinikoor MJ, Cope A, Gay CL, Ferrari G, McGee KS, Kuruc JD, et al. Antiretroviral therapy initiated during acute HIV infection fails to prevent persistent T-cell activation. J Acquir Immune Defic Syndr. 2013;62:505–8. DOI: 10.1097/QAI.0b013e318285cd33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sereti I, Krebs SJ, Phanuphak N, Fletcher JL, Slike B, Pinyakorn S, et al. Persistent, albeit reduced, chronic inflammation in persons starting antiretroviral therapy in acute HIV infection. Clin Infect Dis. 2017;64:124–31. DOI: 10.1093/cid/ciw683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hearps AC, Maisa A, Cheng W-J, Angelovich T a, Lichtfuss GF, Palmer CS, et al. HIV infection induces age-related changes to monocytes and innate immune activation in young men that persist despite combination antiretroviral therapy. AIDS. 2012;26:843–53. DOI: 10.1097/QAD.0b013e328351f756 [DOI] [PubMed] [Google Scholar]
- 5.Guaraldi G, Orlando G, Zona S, Menozzi M, Carli F, Garlassi E, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis. 2011;53:1120–6. DOI: 10.1093/cid/cir627 [DOI] [PubMed] [Google Scholar]
- 6.The Antiretroviral Therapy Cohort Collaboration Study Group. Causes of Death in HIV1–Infected Patients Treated with Antiretroviral Therapy, 1996–2006: Collaborative Analysis of 13 HIV Cohort Studies. Clin Infect Dis. 2010;50:1387–96. DOI: 10.1086/652283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tenorio AR, Zheng Y, Bosch RJ, Krishnan S, Rodriguez B, Hunt PW, et al. Soluble Markers of Inflammation and Coagulation but Not T-Cell Activation Predict Non – AIDS-Defining Morbid Events During Suppressive Antiretroviral Treatment. J Infect Dis. 2014;210:1248–59. DOI: 10.1093/infdis/jiu254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duffau P, Wittkop L, Lazaro E, Le Marec F, Cognet C, Blanco P, et al. Association of immune-activation and senescence markers with non-AIDS-defining comorbidities in HIV-suppressed patients. AIDS. 2015;29:2099–108. DOI: 10.1097/QAD.0000000000000807 [DOI] [PubMed] [Google Scholar]
- 9.Krishnan S, Wilson EMP, Sheikh V, Rupert A, Mendoza D, Yang J, et al. Evidence for innate immune system activation in HIV type 1-infected elite controllers. J Infect Dis. 2014;209:931–9. DOI: 10.1093/infdis/jit581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearce EL, Pearce EJ. Metabolic pathways in immune cell activation and quiescence. Immunity. 2013;38:633–43. DOI: 10.1016/j.immuni.2013.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L Le Zhang ZN, Wu X Jiang YJ, Fu YJ, Shang H. Transcriptomic meta-analysis identifies gene expression characteristics in various samples of HIV-infected patients with nonprogressive disease. J Transl Med. 2017;15. DOI: 10.1186/s12967-017-1294-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu JQ, Dwyer DE, Dyer WB, Yang YH, Wang B, Saksena NK. Genome-wide analysis of primary CD4+ and CD8+ T cell transcriptomes shows evidence for a network of enriched pathways associated with HIV disease. Retrovirology. 2011;8:18. DOI: 10.1186/1742-4690-8-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tarancon-Diez L, Rodríguez-Gallego E, Rull A, Peraire J, Viladés C, Portilla I, et al. Immunometabolism is a key factor for the persistent spontaneous elite control of HIV-1 infection. EBioMedicine. 2019;42:86–96. DOI:10.1016/j.ebiom.2019.03.004.30879922 •• This study describes the metabolomic profile of PLWH who lose virological control, which is characterized by aerobic glycolysis, dysfunctional mitochondria and oxidative stress. Importantly, decreased functionality of CD8+ T cells was found to be associated with dysfunctional mitochondria and oxidative stress.
- 14. Kavanagh Williamson M, Coombes N, Juszczak F, Athanasopoulos M, Khan M, Eykyn T, et al. Upregulation of Glucose Uptake and Hexokinase Activity of Primary Human CD4+ T Cells in Response to Infection with HIV-1. Viruses. 2018;10:114. DOI:10.3390/v10030114. • This study provides a comprehensive assessment of glucose transporter mRNA and protein expression in resting CD4+ T cells and CD3/CD28stimulated uninfected and HIV-infected CD4+ T cells.
- 15.Loisel-Meyer S, Swainson L, Craveiro M, Oburoglu L, Mongellaz C, Costa C, et al. Glut1-mediated glucose transport regulates HIV infection. Proc Natl Acad Sci U S A. 2012;109:2549–54. DOI: 10.1073/pnas.1121427109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valle-Casuso JC, Angin M, Volant S, Passaes C, Monceaux V, Mikhailova A, et al. Cellular Metabolism Is a Major Determinant of HIV-1 Reservoir Seeding in CD4+ T Cells and Offers an Opportunity to Tackle Infection. Cell Metab. 2019;29:611–626.e5. DOI:10.1016/j.cmet.2018.11.015.30581119 • This study demonstrates that HIV preferentially targets the most metabolically active CD4+ T cells, the effector memory subset, and that the metabolic program of the cell dictates the outcome of HIV infection in vitro.
- 17.Hegedus A, Kavanagh Williamson M, Huthoff H. HIV-1 pathogenicity and virion production are dependent on the metabolic phenotype of activated CD4+ T cells. Retrovirology. 2014;11:98. DOI: 10.1186/s12977-014-0098-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hegedus A, Kavanagh Williamson M, Khan MB, Dias Zeidler J, Da Poian AT, El-Bacha T, et al. Evidence for Altered Glutamine Metabolism in Human Immunodeficiency Virus Type 1 Infected Primary Human CD4+ T Cells. AIDS Res Hum Retroviruses. 2017;33:1236–47. DOI:10.1089/aid.2017.0165.28844150 • This work describes altered glutamine metabolism in CD4+ T cells infected with HIV in vitro.
- 19.Liao W, Tan G, Zhu Z, Chen Q, Lou Z, Dong X, et al. Combined Metabonomic and Quantitative Real-Time PCR Analyses Reveal Systems Metabolic Changes in Jurkat T-Cells Treated with HIV-1 Tat Protein. J Proteome Res. 2012;11:5109–23. DOI: 10.1021/pr300173c [DOI] [PubMed] [Google Scholar]
- 20.Bailis W, Shyer JA, Zhao J, Canaveras JCG, Al Khazal FJ, Qu R, et al. Distinct modes of mitochondrial metabolism uncouple T cell differentiation and function. Nature. Nature Publishing Group; 2019. DOI: 10.1038/s41586-019-1311-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Castellano P, Prevedel L, Valdebenito S, Eugenin EA. HIV infection and latency induce a unique metabolic signature in human macrophages. Sci Rep. 2019;9:3941. DOI:10.1038/s41598-019-39898-5.30850623 • This study shows that HIV infection of macrophages in vitro results in enlarged mitochondria with reduced function without any change in glycolysis.
- 22.Barrero CA, Datta PK, Sen S, Deshmane S, Amini S, Khalili K, et al. HIV-1 Vpr Modulates Macrophage Metabolic Pathways : A SILAC-Based Quantitative Analysis. Zhao RY, editor. PLoS One. 2013;8:e68376. DOI: 10.1371/journal.pone.0068376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Datta PK, Deshmane S, Khalili K, Merali S, Gordon JC, Fecchio C, et al. Glutamate metabolism in HIV-1 infected macrophages: Role of HIV-1 Vpr. Cell Cycle. 2016;15:2288–98. DOI: 10.1080/15384101.2016.1190054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmer CS, Ostrowski M, Gouillou M, Tsai L, Yu D, Zhou J, et al. Increased glucose metabolic activity is associated with CD4+ T-cell activation and depletion during chronic HIV infection. AIDS. 2013;28:297–309. DOI: 10.1097/QAD.0000000000000128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmer CS, Anzinger JJ, Zhou J, Gouillou M, Landay A, Jaworowski A, et al. Glucose Transporter 1 − Expressing Proinflammatory Monocytes Are Elevated in Combination Antiretroviral Therapy − Treated and Untreated HIV + Subjects. J Immunol. 2014;193:5595–603. DOI: 10.4049/jimmunol.1303092 [DOI] [PubMed] [Google Scholar]
- 26.Masson JJR, Murphy AJ, Lee MKS, Ostrowski M, Crowe SM, Palmer CS. Assessment of metabolic and mitochondrial dynamics in CD4+ and CD8+ T cells in virologically suppressed HIV-positive individuals on combination antiretroviral therapy. Ndhlovu LC, editor. PLoS One. 2017;12:e0183931. DOI: 10.1371/journal.pone.0183931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Masson JJR, Cherry CL, Murphy NM, Sada-Ovalle I, Hussain T, Palchaudhuri R, et al. Polymorphism rs1385129 Within Glut1 Gene SLC2A1 Is Linked to Poor CD4+ T Cell Recovery in Antiretroviral-Treated HIV+ Individuals. Front Immunol. 2018;9:900. DOI: 10.3389/fimmu.2018.00900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Korencak M, Byrne M, Richter E, Schultz BT, Juszczak P, Ake JA, et al. Effect of HIV infection and antiretroviral therapy on immune cellular functions. JCI Insight. 2019;4. DOI:10.1172/JCI.INSIGHT.126675. •• This work utilized Seahorse extracellular flux analysis to assess the metabolism of multiple immune cell types from PLWH and showed that incubation of CD4+ T cells with integrase strand inhibitors decreased oxidative phosphorylation.
- 29.Petrovas C, Mueller YM, Dimitriou ID, Altork SR, Banerjee A, Sklar P, et al. Increased mitochondrial mass characterizes the survival defect of HIV-specific CD8+ T cells. Blood. 2007;109:2505–13. DOI: 10.1182/blood-2006-05-021626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalinowska M, Bazdar DA, Lederman MM, Funderburg N, Sieg SF. Decreased IL-7 Responsiveness Is Related to Oxidative Stress in HIV Disease. PLoS One. 2013;8. DOI: 10.1371/journal.pone.0058764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franchina DG, Grusdat M, Brenner D. B-Cell Metabolic Remodeling and Cancer. Vol. 4, Trends in Cancer. Cell Press; 2018. p. 138–50. DOI: 10.1016/j.trecan.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 32.Mah AY, Cooper MA. Metabolic regulation of natural killer cell IFN-γ production. Crit Rev Immunol. 2016;36:131–47. DOI: 10.1615/CritRevImmunol.2016017387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Batman PA, Miller ARO, Forster SM, Harris JRW, Pinching AJ, Griffin GE. Jejunal enteropathy associated with human immunodeficiency virus infection: Quantitative histology. J Clin Pathol. 1989;42:275–81. DOI: 10.1136/jcp.42.3.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim SG, Menzies IS, Lee CA, Johnson MA, Pounder RE. Intestinal permeability and function in patients infected with human immunodeficiency virus: A comparison with coeliac disease. Scand J Gastroenterol. 1993;28:573–80. DOI: 10.3109/00365529309096090 [DOI] [PubMed] [Google Scholar]
- 35.Chung CY, Alden SL, Funderburg NT, Fu P, Levine AD. Progressive Proximal-to-Distal Reduction in Expression of the Tight Junction Complex in Colonic Epithelium of Virally-Suppressed HIV+ Individuals. PLoS Pathog. 2014;10. DOI: 10.1371/journal.ppat.1004198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marchetti G, Tincati C, Silvestri G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin Microbiol Rev. 2013;26:2–18. DOI: 10.1128/CMR.00050-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brenchley JM, Price D a, Schacker TW, Asher TE, Silvestri G, Rao S, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–71. DOI: 10.1038/nm1511 [DOI] [PubMed] [Google Scholar]
- 38.Kristoff J, Haret-Richter G, Ma D, Ribeiro RM, Xu C, Cornell E, et al. Early microbial translocation blockade reduces SIV-mediated inflammation and viral replication. J Clin Invest. 2014;124:2802–6. DOI: 10.1172/JCI75090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fitzgerald FC, Lhomme E, Harris K, Kenny J, Doyle R, Kityo C, et al. Microbial translocation does not drive immune activation in ugandan children infected with HIV. J Infect Dis. 2019;219:89–100. DOI: 10.1093/infdis/jiy495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sandler NG, Zhang X, Bosch RJ, Funderburg NT, Choi AI, Robinson JK, et al. Sevelamer does not decrease lipopolysaccharide or soluble cd14 levels but decreases soluble tissue factor, low-density lipoprotein (ldl) cholesterol, and oxidized ldl cholesterol levels in individuals with untreated hiv infection. J Infect Dis. 2014;210:1549–54. DOI: 10.1093/infdis/jiu305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vujkovic-Cvijin I, Dunham RM, Iwai S, Maher MC, Albright RG, Broadhurst MJ, et al. Dysbiosis of the gut microbiota is associated with hiv disease progression and tryptophan catabolism. Sci Transl Med. 2013;5:193ra91. DOI: 10.1126/scitranslmed.3006438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mutlu EA, Keshavarzian A, Losurdo J, Swanson G, Siewe B, Forsyth C, et al. A Compositional Look at the Human Gastrointestinal Microbiome and Immune Activation Parameters in HIV Infected Subjects. PLoS Pathog. 2014;10. DOI: 10.1371/journal.ppat.1003829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vázquez-Castellanos JF, Serrano-Villar S, Latorre A, Artacho A, Ferrús ML, Madrid N, et al. Altered metabolism of gut microbiota contributes to chronic immune activation in HIV-infected individuals. Mucosal Immunol. 2015;8:760–72. DOI: 10.1038/mi.2014.107 [DOI] [PubMed] [Google Scholar]
- 44.Nowak P, Troseid M, Avershina E, Barqasho B, Neogi U, Holm K, et al. Gut microbiota diversity predicts immune status in HIV-1 infection. AIDS. 2015;29:2409–18. DOI: 10.1097/QAD.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 45. Dillon SM, Kibbie J, Lee EJ, Guo K, Santiago ML, Austin GL, et al. Low abundance of colonic butyrate-producing bacteria in HIV infection is associated with microbial translocation and immune activation. AIDS. 2017;31:511–21. DOI:10.1097/QAD.0000000000001366.28002063 • This study shows an inverse relationship between the abundance of butyrate producing bacteria in the colonic mucosae and immune activation in PLWH. In vitro addition of butyrate decreased immune activation of T cells.
- 46.Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446–50. DOI: 10.1038/nature12721 [DOI] [PubMed] [Google Scholar]
- 47.Singh N, Gurav A, Sivaprakasam S, Brady E, Padia R, Shi H, et al. Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis. Immunity. 2014;40:128–39. DOI: 10.1016/j.immuni.2013.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.SÄEMANN MD, BÖHMIG GA, ÖSTERREICHER CH, BURTSCHER H, PAROLINI O, DIAKOS C, et al. Anti-inflammatory effects of sodium butyrate on human monocytes: potent inhibition of IL-12 and up-regulation of IL-10 production. FASEB J. 2000;14:2380–2. DOI: 10.1096/fj.00-0359fje [DOI] [PubMed] [Google Scholar]
- 49.Chang P V, Hao L, Offermanns S, Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci U S A. 2014;111:2247–52. DOI: 10.1073/pnas.1322269111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corrêa-Oliveira R, Fachi JL, Vieira A, Sato FT, Vinolo MAR. Regulation of immune cell function by short-chain fatty acids. Vol. 5, Clinical and Translational Immunology. John Wiley and Sons Inc.; 2016. DOI: 10.1038/cti.2016.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Serrano-Villar S, Vázquez-Castellanos JF, Vallejo A, Latorre A, Sainz T, Ferrando-Martínez S, et al. The effects of prebiotics on microbial dysbiosis, butyrate production and immunity in HIV-infected subjects. Mucosal Immunol. 2017;10:1279–93. DOI: 10.1038/mi.2016.122 [DOI] [PubMed] [Google Scholar]
- 52.Schulthess J, Pandey S, Capitani M, Rue-Albrecht KC, Arnold I, Franchini F, et al. The Short Chain Fatty Acid Butyrate Imprints an Antimicrobial Program in Macrophages. Immunity. 2019;50:432–445.e7. DOI: 10.1016/j.immuni.2018.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoel H, Hove-Skovsgaard M, Hov JR, Gaardbo JC, Holm K, Kummen M, et al. Impact of HIV and Type 2 diabetes on Gut Microbiota Diversity, Tryptophan Catabolism and Endothelial Dysfunction. Sci Rep. 2018;8. DOI: 10.1038/s41598-018-25168-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Favre D, Mold J, Hunt PW, Kanwar B, Loke P, Seu L, et al. Tryptophan catabolism by indoleamine 2, 3-dioxygenase 1 alters the balance of TH17 to regulatory T cells in HIV disease. Sci Transl Med. 2010;2. DOI: 10.1126/scitranslmed.3000632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Qi Q, Hua S, Clish CB, Scott JM, Hanna DB, Wang T, et al. Plasma tryptophan-kynurenine metabolites are altered in human immunodeficiency virus infection and associated with progression of carotid artery atherosclerosis. Clin Infect Dis. 2018;67:235–42. DOI:10.1093/cid/ciy053.29415228 • This study provides evidence for a linkage between tryptophan catabolism, immune activation and the presence of carotid plaques in PLWH.
- 56.Vázquez-Castellanos JF, Serrano-Villar S, Jiménez-Hernández N, Soto Del Rio MD, Gayo S, Rojo D, et al. Interplay between gut microbiota metabolism and inflammation in HIV infection. ISME J. 2018;12:1964–76. DOI: 10.1038/s41396-018-0151-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haissman JM, Knudsen A, Hoel H, Kjær A, Kristoffersen US, Berge RK, et al. Microbiota-Dependent Marker TMAO Is Elevated in Silent Ischemia but Is Not Associated with First-Time Myocardial Infarction in HIV Infection. J Acquir Immune Defic Syndr. 2016;71:130–6. DOI: 10.1097/QAI.0000000000000843 [DOI] [PubMed] [Google Scholar]
- 58.Haissman JM, Haugaard AK, Ostrowski SR, Berge RK, Hov JR, Trøseid M, et al. Microbiota-dependent metabolite and cardiovascular disease marker trimethylamine-N-oxide (TMAO) is associated with monocyte activation but not platelet function in untreated HIV infection. BMC Infect Dis. 2017;17. DOI: 10.1186/s12879-017-2547-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Srinivasa S, Fitch KV., Lo J, Kadar H, Knight R, Wong K, et al. Plaque burden in HIV-infected patients is associated with serum intestinal microbiota-generated trimethylamine. AIDS. 2015;29:443–52. DOI: 10.1097/QAD.0000000000000565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elliott Miller P, Haberlen SA, Brown TT, Margolick JB, DiDonato JA, Hazen SL, et al. Intestinal microbiota-produced trimethylamine-N-oxide and its association with coronary stenosis and HIV serostatus. J Acquir Immune Defic Syndr. 2016;72:114–8. DOI: 10.1097/QAI.0000000000000937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shan Z, Clish CB, Hua S, Scott JM, Hanna DB, Burk RD, et al. Gut microbial-related choline metabolite trimethylamine-N-oxide is associated with progression of carotid artery atherosclerosis in HIV infection. J Infect Dis. 2018;218:1474–9. DOI: 10.1093/infdis/jiy356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Knudsen A, Christensen TE, Thorsteinsson K, Ghotbi AA, Hasbak P, Lebech AM, et al. Microbiota-dependent marker TMAO is not associated with decreased myocardial perfusion in well-treated HIV-infected patients as assessed by 82 rubidium PET/CT. Vol. 72, Journal of Acquired Immune Deficiency Syndromes. Lippincott Williams and Wilkins; 2016. p. e83–5. DOI: 10.1097/QAI.0000000000001044 [DOI] [PubMed] [Google Scholar]
- 63.Missailidis C, Neogi U, Stenvinkel P, Trøseid M, Nowak P, Bergman P. The microbial metabolite trimethylamine-N-oxide in association with inflammation and microbial dysregulation in three HIV cohorts at various disease stages. AIDS. 2018;32:1589–98. DOI: 10.1097/QAD.0000000000001813 [DOI] [PubMed] [Google Scholar]
- 64.Naeger DM, Martin JN, Sinclair E, Hunt PW, Bangsberg DR, Hecht F, et al. Cytomegalovirus-Specific T Cells Persist at Very High Levels during Long-Term Antiretroviral Treatment of HIV Disease. Unutmaz D, editor. PLoS One. 2010;5:e8886. DOI: 10.1371/journal.pone.0008886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gianella S, Massanella M, Wertheim JO, Smith DM. The Sordid Affair Between Human Herpesvirus and HIV. Vol. 212, Journal of Infectious Diseases. Oxford University Press; 2015. p. 845–52. DOI: 10.1093/infdis/jiv148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deayton J, Mocroft A, Wilson P, Emery VC, Johnson MA, Griffiths PD. Loss of cytomegalovirus (CMV) viraemia following highly active antiretroviral therapy in the absence of specific anti-CMV therapy. AIDS. 1999;13:1203–6. DOI: 10.1097/00002030-199907090-00008 [DOI] [PubMed] [Google Scholar]
- 67.Freeman ML, Shive CL, Nguyen TP, Younes SA, Panigrahi S, Lederman MM. Cytokines and T-Cell Homeostasis in HIV Infection. J Infect Dis. 2016;214:S51–7. DOI: 10.1093/infdis/jiw287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barrett L, Stapleton SN, Fudge NJ, Grant MD. Immune resilience in HIV-infected individuals seronegative for cytomegalovirus. AIDS. 2014;28:2045–9. DOI: 10.1097/QAD.0000000000000405 [DOI] [PubMed] [Google Scholar]
- 69.Lee SA, Sinclair E, Hatano H, Hsue PY, Epling L, Hecht FM, et al. Impact of HIV on CD8+ T cell CD57 expression is distinct from that of CMV and aging. PLoS One. 2014;9. DOI: 10.1371/journal.pone.0089444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gianella S, Massanella M, Richman DD, Little SJ, Spina CA, Vargas MV., et al. Cytomegalovirus Replication in Semen Is Associated with Higher Levels of Proviral HIV DNA and CD4 + T Cell Activation during Antiretroviral Treatment. J Virol. 2014;88:7818–27. DOI: 10.1128/jvi.00831-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Christensen-Quick A, Massanella M, Frick A, Rawlings SA, Spina C, Vargas-Meneses M, et al. Subclinical Cytomegalovirus DNA Is Associated with CD4 T Cell Activation and Impaired CD8 T Cell CD107a Expression in People Living with HIV despite Early Antiretroviral Therapy. J Virol. 2019;93. DOI:10.1128/jvi.00179-19 •• This work shows that CMV replication, but not EBV replication, is associated with CD4+ T cell activation that persists even after early ART treatment.
- 72.Hunt PW, Martin JN, Sinclair E, Epling L, Teague J, Jacobson M a, et al. Valganciclovir reduces T cell activation in HIV-infected individuals with incomplete CD4+ T cell recovery on antiretroviral therapy. J Infect Dis. 2011;203:1474–83. DOI: 10.1093/infdis/jir060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Palmer S, Maldarelli F, Wiegand A, Bernstein B, Hanna GJ, Brun SC, et al. Low-level viremia persists for at least 7 years in patients on suppressive antiretroviral therapy. Proc Natl Acad Sci U S A. 2008;105:3879–84. DOI: 10.1073/pnas.0800050105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rosenbloom DIS, Hill AL, Laskey SB, Siliciano RF. Re-evaluating evolution in the HIV reservoir. Nature. 2017;551:E6–8. DOI: 10.1038/nature24634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lorenzo-Redondo R, Fryer HR, Bedford T, Kim EY, Archer J, Kosakovsky Pond SL, et al. Persistent HIV-1 replication maintains the tissue reservoir during therapy. Nature. 2016;530:51–6. DOI: 10.1038/nature16933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ostrowski SR, Katzenstein TL, Pedersen BK, Gerstoft J, Ullum H. Residual viraemia in HIV-1-infected patients with plasma viral load ≤20 copies/ml is associated with increased blood levels of soluble immune activation markers. Scand J Immunol. 2008;68:652–60. DOI: 10.1111/j.1365-3083.2008.02184.x [DOI] [PubMed] [Google Scholar]
- 77.Mavigenr M, Delobel P, Cazabat M, Dubois M, L’Faqihi-Olive FE, Raymond S, et al. HIV-1 residual viremia correlates with persistent T-cell activation in poor immunological responders to combination antiretroviral therapy. PLoS One. 2009;4. DOI: 10.1371/journal.pone.0007658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Henrich TJ, Hobbs KS, Hanhauser E, Scully E, Hogan LE, Robles YP, et al. Human immunodeficiency virus type 1 persistence following systemic chemotherapy for malignancy. J Infect Dis. 2017;216:254–62. DOI:10.1093/infdis/jix265.28838149 • This study demonstrates increased HIV DNA and RNA predominantly in CMV-specific and EBV-specific CD4+ T cells.
- 79.Baroncelli S, Galluzzo CM, Pirillo MF, Mancini MG, Weimer LE, Andreotti M, et al. Microbial translocation is associated with residual viral replication in HAART-treated HIV+ subjects with <50copies/ml HIV-1 RNA. J Clin Virol. 2009;46:367–70. DOI: 10.1016/j.jcv.2009.09.011 [DOI] [PubMed] [Google Scholar]
- 80.Maagaard A, Holberg-Petersen M, Løvgården G, Holm M, Olav Pettersen F, Kvale D. Distinct Mechanisms for Mitochondrial DNA Loss in T and B Lymphocytes from HIV-Infected Patients Exposed to Nucleoside Reverse-Transcriptase Inhibitors and Those Naive to Antiretroviral Treatment. J Infect Dis. 2008;198:1474–81. DOI: 10.1086/592713 [DOI] [PubMed] [Google Scholar]
- 81.Wallace ZR, Sanderson S, Simon AK, Dorrell L. Exposure to zidovudine adversely affects mitochondrial turnover in primary T cells. Antiviral Res. 2016;133:178–82. DOI: 10.1016/j.antiviral.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 82.Zhao X, Sun K, Lan Z, Song W, Cheng L, Chi W, et al. Tenofovir and adefovir down-regulate mitochondrial chaperone TRAP1 and succinate dehydrogenase subunit B to metabolically reprogram glucose metabolism and induce nephrotoxicity. Sci Rep. 2017;7. DOI: 10.1038/srep46344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Yu F, Hao Y, Zhao H, Xiao J, Han N, Zhang Y, et al. Distinct mitochondrial disturbance in CD4+T and CD8+T cells from HIV-infected patients. J Acquir Immune Defic Syndr. 2017;74:206–12. DOI:10.1097/QAI.0000000000001175.27608061 • This study compares mitochondrial function in CD4+ T cells and CD8+ T cells from people without HIV, ART-naïve and ART-experienced PLWH. The authors show an accumulation of reactive oxygen species in CD8+ T cells in ART-experienced PLWH.
- 84.Setzer B, Schlesier M, Walker UA. Effects of Didanosine-Related Depletion of mtDNA in Human T Lymphocytes. J Infect Dis. 2005;191:848–55. DOI: 10.1086/427655 [DOI] [PubMed] [Google Scholar]
- 85.Selvaraj S, Ghebremichael M, Li M, Foli Y, Langs-Barlow A, Ogbuagu A, et al. Antiretroviral therapy-induced mitochondrial toxicity: Potential mechanisms beyond polymerase-γ inhibition. Clin Pharmacol Ther. 2014;96:110–20. DOI: 10.1038/clpt.2014.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Appay V, Sauce D. Assessing immune aging in HIV-infected patients. 2017; DOI: 10.1080/21505594.2016.1195536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Papagno L, Spina C a, Marchant A, Salio M, Rufer N, Little S, et al. Immune activation and CD8+ T-cell differentiation towards senescence in HIV-1 infection. PLoS Biol. 2004;2:E20. DOI: 10.1371/journal.pbio.0020020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dan JM, Massanella M, Smith DM, Spina CA, Schrier R, Daar ES, et al. Effect of CMV and HIV transcription on CD57 and PD-1 T-cell expression during suppressive ART. In: Journal of Acquired Immune Deficiency Syndromes. Lippincott Williams and Wilkins; 2016. p. 133–7. DOI: 10.1097/QAI.0000000000000936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Deeks SG. HIV Infection, Inflammation, Immunosenescence, and Aging. Annu Rev Med. 2011;62:141–55. DOI: 10.1146/annurev-med-042909-093756.HIV [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alcaide ML, Parmigiani A, Pallikkuth S, Roach M, Freguja R, Della Negra M, et al. Immune activation in HIV-infected aging women on antiretrovirals--implications for age-associated comorbidities: a cross-sectional pilot study. PLoS One. 2013;8:e63804. DOI: 10.1371/journal.pone.0063804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Desai S, Landay AL. Early Immune Senescence in HIV disease. Curr HIV/AIDS Rep. 2010;7:4–10. DOI: 10.1007/s11904-009-0038-4.Early [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miller CJ, Baker JV., Bormann AM, Erlandson KM, Hullsiek KH, Justice AC, et al. Adjudicated morbidity and mortality outcomes by age among individuals with HIV infection on suppressive antiretroviral therapy. PLoS One. 2014;9. DOI: 10.1371/journal.pone.0095061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pinto DSM, da Silva MJLV. Cardiovascular Disease in the Setting of Human Immunodeficiency Virus Infection. Curr Cardiol Rev. 2018;14:25–41. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gutierrez J, Albuquerque ALA, Falzon L. HIV infection as vascular risk: A systematic review of the literature and meta-analysis. Vol. 12, PLoS ONE. Public Library of Science; 2017. DOI: 10.1371/journal.pone.0176686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cerrato E, D’Ascenzo F, Biondi-Zoccai G, Calcagno A, Frea S, Grosso Marra W, et al. Cardiac dysfunction in pauci symptomatic human immunodeficiency virus patients: A meta-analysis in the highly active antiretroviral therapy era. Eur Heart J. 2013;34:1432–6. DOI: 10.1093/eurheartj/ehs471 [DOI] [PubMed] [Google Scholar]
- 96.Holloway CJ, Ntusi N, Suttie J, Mahmod M, Wainwright E, Clutton G, et al. Comprehensive cardiac magnetic resonance imaging and spectroscopy reveal a high burden of myocardial disease in HIV patients. Circulation. 2013;128:814–22. DOI: 10.1161/CIRCULATIONAHA.113.001719 [DOI] [PubMed] [Google Scholar]
- 97.Thiara DK, Liu CY, Raman F, Mangat S, Purdy JB, Duarte HA, et al. Abnormal myocardial function is related to myocardial steatosis and diffuse myocardial fibrosis in HIV-infected adults. J Infect Dis. 2015;212:1544–51. DOI: 10.1093/infdis/jiv274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hsu JC, Li Y, Marcus GM, Hsue PY, Scherzer R, Grunfeld C, et al. Atrial fibrillation and atrial flutter in human immunodeficiency virus-infected persons: Incidence, risk factors, and association with markers of HIV disease severity. J Am Coll Cardiol. 2013;61:2288–95. DOI: 10.1016/j.jacc.2013.03.022 [DOI] [PubMed] [Google Scholar]
- 99.Janda S, Quon BS, Swiston J. HIV and pulmonary arterial hypertension: A systematic review. Vol. 11, HIV Medicine. 2010. p. 620–34. DOI: 10.1111/j.1468-1293.2010.00829.x [DOI] [PubMed] [Google Scholar]
- 100.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–25. DOI: 10.1038/nature10146 [DOI] [PubMed] [Google Scholar]
- 101.Kuller LH, Tracy R, Belloso W, De Wit S, Drummond F, Lane HC, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203. DOI: 10.1371/journal.pmed.0050203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Siedner MJ, Kim JH, Nakku RS, Bibangambah P, Hemphill L, Triant VA, et al. Persistent immune activation and carotid atherosclerosis in HIV-infected ugandans receiving antiretroviral therapy. J Infect Dis. 2016;213:370–8. DOI:10.1093/infdis/jiv450.26347573 • This study highlights that the association of immune activation and CVD in PLWH also applies to the low- and middle-income country setting.
- 103.Kaplan RC, Landay AL, Hodis HN, Gange SJ, Norris PJ, Young M, et al. Potential cardiovascular disease risk markers among HIV-infected women initiating antiretroviral treatment. J Acquir Immune Defic Syndr. 2012;60:359–68. DOI: 10.1097/QAI.0b013e31825b03be.Potential [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kaplan RC, Sinclair E, Landay AL, Lurain N, Sharrett AR, Gange SJ, et al. T Cell Activation and Senescence Predict Subclinical Carotid Artery Disease in HIV-Infected Women. J Infect Dis. 2011;203:452–63. DOI: 10.1093/infdis/jiq071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Burdo TH, Lo J, Abbara S, Wei J, DeLelys ME, Preffer F, et al. Soluble CD163, a novel marker of activated macrophages, is elevated and associated with noncalcified coronary plaque in HIV-infected patients. J Infect Dis. 2011;204:1227–36. DOI: 10.1093/infdis/jir520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Funderburg NT, Mayne E, Sieg SF, Asaad R, Jiang W, Kalinowska M, et al. Increased tissue factor expression on circulating monocytes in chronic HIV infection: relationship to in vivo coagulation and immune activation. Blood. 2010;115:161–7. DOI: 10.1182/blood-2009-03-210179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Schechter ME, Andrade BB, He T, Richter GH, Tosh KW, Policicchio BB, et al. Inflammatory monocytes expressing tissue factor drive SIV and HIV coagulopathy. Sci Transl Med. 2017;9. DOI:10.1126/scitranslmed.aam5441. •• This study demonstrates a linkage between, microbial translocation, innate immune activation and coagulopathy in an SIV model.
- 108.Hsue PY, Hunt PW, Sinclair E, Bredt B, Franklin A, Killian M, et al. Increased carotid intima-media thickness in HIV patients is associated with increased cytomegalovirus-specific T-cell responses. AIDS. 2006;20:2275–83. DOI: 10.1097/QAD.0b013e3280108704 [DOI] [PubMed] [Google Scholar]
- 109.Parrinello CM, Sinclair E, Landay AL, Lurain N, Sharrett AR, Gange SJ, et al. Cytomegalovirus immunoglobulin G antibody is associated with subclinical carotid artery disease among HIV-infected women. J Infect Dis. 2012;205:1788–96. DOI: 10.1093/infdis/jis276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Knudsen A, Kristoffersen US, Panum I, Hansen YB, Skottrup PD, Hasbak P, et al. Coronary artery calcium and intima-media thickness are associated with level of cytomegalovirus immunoglobulin G in HIV-infected patients. HIV Med. 2019;20:60–2. DOI: 10.1111/hiv.12672 [DOI] [PubMed] [Google Scholar]
- 111. Anzinger JJ, Butterfield TR, Gouillou M, McCune JM, Crowe SM, Palmer CS. Glut1 Expression Level on Inflammatory Monocytes is Associated With Markers of Cardiovascular Disease Risk in HIV-Infected Individuals. J Acquir Immune Defic Syndr. 2018;77. DOI:10.1097/QAI.0000000000001559.29771793 •• This study provides a link between immunometabolism and cardiovascular disease in treated PLWH.
- 112. Butterfield TR, Hanna DB, Kaplan RC, Kizer JR, Durkin HG, Young MA, et al. Increased glucose transporter-1 expression on intermediate monocytes from HIV-infected women with subclinical cardiovascular disease. AIDS. 2017;31. DOI:10.1097/QAD.0000000000001320. •• This study demonstrates a specific association of inflammatory monocyte immunometabolism and subclinical cardiovascular disease in treated women with HIV.
- 113. Hernandez-Romieu AC, Garg S, Rosenberg ES, Thompson-Paul AM, Skarbinski J. Is diabetes prevalence higher among HIV-infected individuals compared with the general population? Evidence from MMP and NHANES 2009–2010. BMJ Open Diabetes Res Care. 2017;5. DOI:10.1136/bmjdrc-2016-000304. •• This study describes the increased prevalence of diabetes mellitus in a large cohort of PLWH compared to uninfected controls. The authors show that this increased prevalence in PLWH is present even without traditional risk factors of obesity and increased age.
- 114.Crum NF, Riffenburgh RH, Wegner S, Agan BK, Tasker SA, Spooner KM, et al. Comparisons of Causes of Death and Mortality Rates among HIV-infected persons : Analysis of the Pre-, early and late HAART (Highly active antiretroviral therapy) eras. J Acquir Immune Defic Syndr. 2006;41:194–200. [DOI] [PubMed] [Google Scholar]
- 115.Prioreschi A, Munthali RJ, Soepnel L, Goldstein JA, Micklesfield LK, Aronoff DM, et al. Incidence and prevalence of type 2 diabetes mellitus with HIV infection in Africa: A systematic review and meta-analysis. Vol. 7, BMJ Open. BMJ Publishing Group; 2017. DOI: 10.1136/bmjopen-2016-013953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Vol. 11, Nature Reviews Immunology. 2011. p. 98–107. DOI: 10.1038/nri2925 [DOI] [PubMed] [Google Scholar]
- 117.Shikuma CM, Chow DC, Gangcuangco LMA, Zhang G, Keating SM, Norris PJ, et al. Monocytes expand with immune dysregulation and is associated with insulin resistance in older individuals with chronic HIV. Unutmaz D, editor. PLoS One. 2014;9:e90330. DOI: 10.1371/journal.pone.0090330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Butterfield TR, Hanna DB, Kaplan RC, Kizer JR, Durkin HG, Young MA, et al. HIV+ women with diabetes mellitus exhibit CD4+ T lymphocyte immunometabolic dysfunction. In: International AIDS Society Conference on HIV Science. Mexico City, Mexico; 2019. [Google Scholar]
- 119. Couturier J, Agarwal N, Nehete PN, Baze WB, Barry MA, Jagannadha Sastry K, et al. Infectious SIV resides in adipose tissue and induces metabolic defects in chronically infected rhesus macaques. Retrovirology. 2016;13. DOI:10.1186/s12977-016-0260-2.26935098 • This SIV study describes the association of GLUT4 expression on adipocytes with increased percentage of peripheral CD8+ T cells and increased inflammatory cytokines. This provides a potential link between diabetes mellitus and inflammation.
- 120.Dye CK, Corley MJ, Li D, Khadka VS, Mitchell BI, Sultana R, et al. Comparative DNA methylomic analyses reveal potential origins of novel epigenetic biomarkers of insulin resistance in monocytes from virally suppressed HIV-infected adults. Clin Epigenetics. 2019;11. DOI: 10.1186/s13148-019-0694-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang Q, Wu H. T Cells in Adipose Tissue: Critical Players in Immunometabolism. Front Immunol. 2018;9:2509. DOI: 10.3389/fimmu.2018.02509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Shikuma CM, Gangcuango LMA, Killebrew DA, LiButti DE, Chow DC, Nakamoto BK, et al. The Role of HIV and monocytes/macrophages in adipose tissue biology. J Acquir Immune Defic Syndr. 2015;65:151–9. DOI: 10.1097/01.qai.0000435599.27727.6c.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Couturier J, Suliburk JW, Brown JM, Luke DJ, Agarwal N, Yu X, et al. Human adipose tissue as a reservoir for memory CD4+ T cells and HIV. AIDS. 2015;29:667–74. DOI: 10.1097/QAD.0000000000000599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Wanjalla CN, McDonnell WJ, Barnett L, Simmons JD, Furch BD, Lima MC, et al. Adipose tissue in persons with HIV is enriched for CD4+ T effector memory and T effector memory RA+ cells, which show higher CD69 expression and CD57, CX3CR1, GPR56 co-expression with increasing glucose intolerance. Front Immunol. 2019;10. DOI:10.3389/fimmu.2019.00408.30723470 • This study of PLWH demonstrates increasing proportions of activated tissue resident CD4+ T cells in adipose tissue with increasing glucose intolerance, providing a link between immune activation and diabetes mellitus.
- 125.Moon JY, Zolnik CP, Wang Z, Qiu Y, Usyk M, Wang T, et al. Gut microbiota and plasma metabolites associated with diabetes in women with, or at high risk for, HIV infection. EBioMedicine. 2018;37:392–400. DOI: 10.1016/j.ebiom.2018.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bailin SS, Jenkins CA, Petucci C, Culver JA, Shepherd BE, Fessel JP, et al. Lower concentrations of circulating medium and long-chain acylcarnitines characterize insulin resistance in persons with HIV. AIDS Res Hum Retroviruses. 2018;34:536–43. DOI: 10.1089/aid.2017.0314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Harrison ML, Wolfe AS, Fordyce J, Rock J, García AA, Zuñiga JA. The additive effect of type 2 diabetes on fibrinogen, von Willebrand factor, tryptophan and threonine in people living with HIV. Amino Acids. 2019; DOI: 10.1007/s00726-019-02715-4 [DOI] [PubMed] [Google Scholar]
- 128.Brunt SJ, Cysique LA, Lee S, Burrows S, Brew BJ, Price P. Short communication: Do cytomegalovirus antibody levels associate with age-related syndromes in HIV patients stable on antiretroviral therapy? AIDS Res Hum Retroviruses. 2016;32:567–72. DOI: 10.1089/aid.2015.0328 [DOI] [PubMed] [Google Scholar]
- 129.Coghill AE, Shiels MS, Suneja G, Engels EA. Elevated cancer-specific mortality among HIV-infected patients in the United States. J Clin Oncol. 2015;33:2376–83. DOI: 10.1200/JCO.2014.59.5967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Coghill AE, Han X, Suneja G, Lin CC, Jemal A, Shiels MS. Advanced stage at diagnosis and elevated mortality among US patients with cancer infected with HIV in the National Cancer Data Base. Cancer. 2019; DOI: 10.1002/cncr.32158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Engels EA, Yanik EL, Wheeler W, Gill MJ, Shiels MS, Dubrow R, et al. Cancer-Attributable Mortality among People with Treated Human Immunodeficiency Virus Infection in North America. Clin Infect Dis. 2017;65:636–43. DOI: 10.1093/cid/cix392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mitsuyasu RT. Non-AIDS-defining cancers. Top Antivir Med. 2014;22:660–5. DOI: 10.1097/QCO.0b013e3283213080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kirk GD, Merlo C, O’Driscoll P, Mehta SH, Galai N, Vlahov D, et al. HIV Infection Is Associated with an Increased Risk for Lung Cancer, Independent of Smoking. Clin Infect Dis. 2007;45:103–10. DOI: 10.1086/518606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Engels EA, Brock MV., Chen J, Hooker CM, Gillison M, Moore RD. Elevated incidence of lung cancer among HIV-infected individuals. J Clin Oncol. 2006;24:1383–8. DOI: 10.1200/JCO.2005.03.4413 [DOI] [PubMed] [Google Scholar]
- 135.Borges ÁH, Silverberg MJ, Wentworth D, Grulich AE, Fätkenheuer G, Mitsuyasu R, et al. Predicting risk of cancer during HIV infection: The role of inflammatory and coagulation biomarkers. AIDS. 2013;27:1433–41. DOI: 10.1097/QAD.0b013e32835f6b0c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Engels EA. Non-AIDS-defining malignancies in HIV-infected persons: Etiologic puzzles, epidemiologic perils, prevention opportunities. AIDS. 2009;23:875–85. DOI: 10.1097/QAD.0b013e328329216a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sigel K, Wisnivesky J, Crothers K, Gordon K, Brown ST, Rimland D, et al. Immunological and infectious risk factors for lung cancer in US veterans with HIV: a longitudinal cohort study. Lancet HIV. 2017;4:e67–73. DOI: 10.1016/S2352-3018(16)30215-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hornyák L, Dobos N, Koncz G, Karányi Z, Páll D, Szabó Z, et al. The role of indoleamine-2,3-dioxygenase in cancer development, diagnostics, and therapy. Vol. 9, Frontiers in Immunology. Frontiers Media S.A.; 2018. DOI: 10.3389/fimmu.2018.00151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Comito G, Iscaro A, Bacci M, Morandi A, Ippolito L, Parri M, et al. Lactate modulates CD4 + T-cell polarization and induces an immunosuppressive environment, which sustains prostate carcinoma progression via TLR8/miR21 axis. Oncogene. 2019;38:3681–95. [DOI] [PubMed] [Google Scholar]
- 140.Raychaudhuri D, Bhattacharya R, Sinha BP, Liu CSC, Ghosh AR, Rahaman O, et al. Lactate Induces Pro-tumor Reprogramming in Intratumoral Plasmacytoid Dendritic Cells. Front Immunol. 2019;10. DOI: 10.3389/fimmu.2019.01878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Desquilbet L, Jacobson LP, Fried LP, Phair JP, Jamieson BD, Holloway M, et al. HIV-1 infection is associated with an earlier occurrence of a phenotype related to frailty. J Gerontol A Biol Sci Med Sci. 2007;62:1279–86. [DOI] [PubMed] [Google Scholar]
- 142.Erlandson KM, Ng DK, Jacobson LP, Margolick JB, Dobs AS, Palella FJ, et al. Inflammation, immune activation, immunosenescence, and hormonal biomarkers in the frailty-related phenotype of men with or at risk for HIV infection. J Infect Dis. 2017;215:228–37. DOI: 10.1093/infdis/jiw523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Margolick JB, Bream JH, Martínez-Maza O, Lopez J, Li X, Phair JP, et al. Frailty and circulating markers of inflammation in HIV+ and HIV2 men in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2017;74:407–17. DOI: 10.1097/QAI.0000000000001261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Yeoh HL, Cheng AC, Cherry CL, Weir JM, Meikle PJ, Hoy JF, et al. Immunometabolic and Lipidomic Markers Associated With the Frailty Index and Quality of Life in Aging HIV+ Men on Antiretroviral Therapy. EBioMedicine. 2017;22:112–21. DOI:10.1016/j.ebiom.2017.07.01528754302 • This study shows that frail men living with HIV have increased expression of GLUT1 on monocytes and increased markers of innate immune activation.
- 145.Heaton RK, Clifford DB, Franklin DR, Woods SP, Ake C, Vaida F, et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–96. DOI: 10.1212/WNL.0b013e318200d727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.McGuire JL, Gill AJ, Douglas SD, Kolson DL. Central and peripheral markers of neurodegeneration and monocyte activation in HIV-associated neurocognitive disorders. J Neurovirol. 2015;21:439–48. DOI: 10.1007/s13365-015-0333-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ancuta P, Kamat A, Kunstman KJ, Kim E-Y, Autissier P, Wurcel A, et al. Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS One. 2008;3:e2516. DOI: 10.1371/journal.pone.0002516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Letendre S, Bharti A, Perez-Valero I, Hanson B, Franklin D, Woods SP, et al. Higher Anti-Cytomegalovirus Immunoglobulin G Concentrations Are Associated with Worse Neurocognitive Performance during Suppressive Antiretroviral Therapy. Clin Infect Dis. 2018;67:770–7. DOI: 10.1093/cid/ciy170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zamudio-Rodríguez A, Belaunzarán-Zamudio PF, Sierra-Madero JG, Cuellar-Rodríguez J, Crabtree-Ramírez BE, Alcala-Zermeno JL, et al. Association between Frailty and HIV-Associated Neurodegenerative Disorders among Older Adults Living with HIV. AIDS Res Hum Retroviruses. 2018;34:449–55. DOI: 10.1089/aid.2017.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sacktor N. Changing clinical phenotypes of HIV-associated neurocognitive disorders. Vol. 24, Journal of NeuroVirology. Springer; 2018. p. 141–5. DOI: 10.1007/s13365-017-0556-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kim DJ, Westfall AO, Chamot E, Willig AL, Mugavero MJ, Ritchie C, et al. Multimorbidity patterns in HIV-infected patients: The role of obesity in chronic disease clustering. J Acquir Immune Defic Syndr. 2012;61:600–5. DOI: 10.1097/QAI.0b013e31827303d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Duffau P, Ozanne A, Bonnet F, Lazaro E, Cazanave C, Blanco P, et al. Multimorbidity, age-related comorbidities and mortality: Association of activation, senescence and inflammation markers in HIV adults. AIDS. 2018;32:1651–60. DOI: 10.1097/QAD.0000000000001875 [DOI] [PubMed] [Google Scholar]