Abstract
Background
Dilated cardiomyopathy (DCMP) is characterized by ventricular chamber enlargement and systolic dysfunction which may cause heart failure. Patients with DCMP have overactivation of the renin-angiotensin-aldosterone systems, which can also adversely affect myocardial metabolism in heart failure. The impairment of myocardial metabolism can contribute to the progression of left ventricular remodeling and contractile dysfunction in heart failure. Although angiotensin II receptor blockers (ARBs) have been used to treat patients with DCMP, there has been no direct comparison of the efficacy of these agents. The objective of this study is to compare the effects of olmesartan and valsartan on myocardial metabolism in patients with DCMP.
Methods/design
The OVOID study (a comparison study of Olmesartan and Valsartan On myocardial metabolism In patients with Dilated cardiomyopathy) is designed as a non-blinded, open-label, parallel-group, prospective, randomized, controlled, multicenter clinical trial. A total of 40 DCMP patients aged between 20 and 85 years will be randomly allocated into the olmesartan or the valsartan group. 18F-fluoro-2-deoxyglucose (FDG) cardiac positron emission tomography (PET) will be performed at baseline and six months after receiving the study agent. The primary endpoint is myocardial glucose consumption per square meter, measured using 18F-FDG PET 6 months after receiving the study agent.
Discussion
The purpose of this trial is to compare the efficacy between olmesartan and valsartan in improving myocardial metabolism in DCMP patients. This will be the first randomized comparative study investigating the differential effects of ARBs on heart failure.
Trial registration
ClinicalTrials.govNCT04174456. Registered on 18 November 2019
Supplementary Information
The online version contains supplementary material available at 10.1186/s13063-021-05970-7.
Keywords: Olmesartan, Valsartan, Myocardial metabolism, Positron emission tomography
Background
Dilated cardiomyopathy (DCMP) is characterized by ventricular chamber enlargement and systolic dysfunction which may cause heart failure (HF) [1]. Increased wall stress and oxygen demand result in increased myocardial oxygen consumption in DCMP [2]. At the same time, myocardial energy efficiency is reduced with wasteful cycling of free fatty acids through lipolysis, re-esterification, and suppression of the more energy-efficient glucose metabolism [3, 4]. Thus, patients with DCMP may exhibit alterations in myocardial metabolism. Recent studies have suggested that the suppression of the renin-angiotensin-aldosterone systems (RAAS) might have potential myocardial metabolism benefits in DCMP patients [5, 6]; overactivation of the RAAS is one of the key detrimental mechanisms of DCMP progression and is associated with poor prognosis [7, 8]. The increased adrenergic tone in HF (1) not only exerts a direct toxic effect on myocytes (2) but also causes unfavorable changes in myocardial energy use [9, 10]. Therefore, suppression of RAAS could positively affect cardiac energy metabolism and is a potential therapeutic strategy in patients with DCMP. Angiotensin II receptor blockers (ARBs) have been shown to be effective in RAAS suppression [11], and currently, several ARBs have been approved for clinical use. However, there has been no direct comparison of the efficacy of different ARBs in HF patients. A previous study demonstrated that treatment with olmesartan significantly improved left ventricular (LV) function and ameliorated the progression of cardiac remodeling in rats with DCMP [12]. It has been reported that the antihypertensive action and duration of olmesartan may be greater than those of other ARBs because it is a more potent and selective angiotensin II receptor antagonist with no agonist activity [13–17].
The purpose of this study was to noninvasively compare the effects of olmesartan vs. valsartan on myocardial metabolism in nonischemic myocardial segments of patients with DCMP.
Objectives
Primary objective
The primary objective is to compare the effects of 6-month olmesartan and valsartan treatment on myocardial metabolism in DCMP patients.
Secondary objectives
The secondary objectives are to compare the effects of 6-month olmesartan and valsartan treatment in DCMP patients on the following variables: (1) change in myocardial glucose consumption, (2) change in N-terminal pro-B-type natriuretic peptide (NT-proBNP) level, (3) change in left ventricular ejection fraction (LVEF), (4) change in New York Heart Association (NYHA) functional class, and (5) the occurrence of clinical events.
Methods/design
Participants
Patients are eligible for this study if they are diagnosed with DCMP with an LV ejection fraction of < 40% and an LV end-diastolic diameter of > 117% of the predicted value corrected to body surface area and age with NYHA functional classes of III and IV (Table 1). A diagnosis of DCMP is determined using the currently accepted criteria [18].
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | |
|
1) Patients with a diagnosis of heart failure NYHA functional class III or IV 2) Left ventricular end-diastolic diameter greater than 117% of the predicted value corrected for body surface area and age 3) Left ventricular ejection fraction ≤ 40% 4) Not planned for revascularization 5) Absence of severe intractable arrhythmias | |
| Exclusion criteria | |
|
1) Less than 20 years or more than 85 years old 2) The presence of hemodynamic instability 3) Known intolerance to olmesartan and valsartan 4) Coronary artery disease 5) Acute or subacute stage of myocarditis 6) Primary valve disease 7) Excessive use of alcohol 8) Expected or performed cardiac resynchronization therapy and heart transplantation 9) Stress-provoked Takotsubo cardiomyopathy 10) Tachycardia-induced cardiomyopathy 11) Peripartum cardiomyopathy 12) Cor pulmonale 13) Impaired renal function 14) A life expectancy < 1 year 15) An inability to give informed consent. |
NYHA New York Heart Association
The exclusion criteria are as follows: (1) less than 20 years and more than 85 years old, (2) the presence of hemodynamic instability, (3) known intolerance to olmesartan and valsartan, (4) coronary artery disease based on coronary angiography (≥ 50% stenosis in ≥ 1 of the major coronary arteries) and/or a history of myocardial infarction or angina pectoris, (5) acute or subacute stage of myocarditis, (6) primary valve disease, (7) excessive use of alcohol, (8) expected or performed cardiac resynchronization therapy and heart transplantation, (9) stress-provoked Takotsubo cardiomyopathy, (10) tachycardia-induced cardiomyopathy, (11) peripartum cardiomyopathy, (12) Cor pulmonale, (13) impaired renal function (estimated glomerular filtration rate of < 60 ml/min/1.73m2, (14) a life expectancy of less than 1 year, and (15) inability to provide informed consent. The complete lists of inclusion and exclusion criteria are provided in Table 1. Patients will not be excluded from the analysis after randomization. The participants will be dropped out of the study if (1) the subjects choose to withdraw from the study, (2) there is poor treatment compliance, (3) they experience serious adverse events or present a serious laboratory abnormality that constitutes an unacceptable risk with continued participation in the study, and (4) they are pregnant.
Study design
OVOID study (a comparison study of Olmesartan and Valsartan effects on myocardial metabolism in patients with Dilated cardiomyopathy) is a prospective, multicenter, randomized, open-label, active-controlled study with two parallel study groups. The study is being conducted in five tertiary hospitals in South Korea. The participants are randomly allocated into the olmesartan group and the valsartan group and followed-up for 6 months after discharge. The overall study algorithm is depicted in Fig. 1. A diagnostic coronary angiogram is performed on all patients to exclude coronary artery disease. If not contraindicated, the patients receive evidence-based pharmacological therapy (at the maximum tolerated dosages), except angiotensin-converting enzyme (ACE) inhibitor and ARB [19]. A baseline echocardiographic examination and 18F-fluoro-2-deoxyglucose (FDG) PET scan are performed before discharge. During the study period, study visits are scheduled at 1, 3, and 6 months. At each visit, the patients undergo a complete physical examination, medical history collection, and assessment of drug compliance. At each study visit, a sample of blood is sent to a central laboratory for the measurement of plasma NT-proBNP. The investigators evaluate all clinical and laboratory adverse events at each visit. To monitor safety, serum creatinine and blood urea nitrogen concentrations are determined at every study visit. The patient’s NYHA functional class and predefined clinical events are recorded at each clinical visit. 18F-FDG PET and echocardiography will be performed 6 months after randomization [18] by a core laboratory staff blinded to random assignment. Table 2 summarizes the study enrollment, interventions, and assessments details.
Fig. 1.
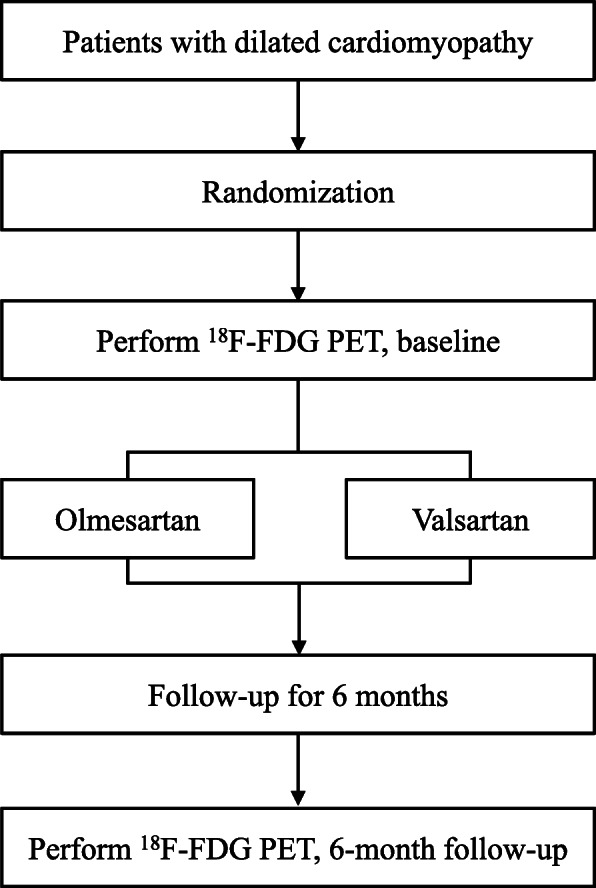
Study design. FDG, fluoro-2-deoxyglucose; PET, positron emission tomography
Table 2.
Participant timeline
| Time point | Study period | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Enrolment | Olmesartan group | Valsartan group | |||||||
| Time | Week 0 | Week 1 | Week 4 | Week 12 | Week 24 | Week 1 | Week 4 | Week 12 | Week 24 |
| Enrolment | |||||||||
| Eligibility screen | ○ | ||||||||
| Informed consent | ○ | ||||||||
| Interventions | |||||||||
| OVOID 24 weeks program | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |
| Assessments | |||||||||
| Demographic data | ○ | ||||||||
| Baseline PET | ○ | ||||||||
| 6-month PET | ○ | ○ | |||||||
| Secondary outcomes | ○ | ○ | |||||||
| Clinical examination | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Adverse events | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |
PET Positron emission tomography
The study protocol (version # 2.3, 6 November, 2019), which follows the SPRIT guidelines (see the additional file, appendix A), was approved by the Institutional Review Board. The recruitment of participants started in December 2019 and was completed in December 2021. This study follows the principles of the Declaration of Helsinki, whereby all patients sign a written informed consent stating that participation is voluntary and could be withdrawn at any time without any negative consequences concerning their current or future medical treatment. Written informed consent is obtained from each participant before 18F-FDG PET and randomization. The trial is overseen by an independent data monitoring committee and registered at www.clinicaltrials.gov: NCT04174456.
Study endpoints
The primary hypothesis to be tested is the efficacy of olmesartan in significantly improving myocardial metabolism in DCMP patients compared to valsartan with a 6-month follow-up period. Myocardial metabolism is visualized using PET with metabolic tracers; this study uses PET and 18F-FDG to assess myocardial glucose use. The primary endpoint is myocardial glucose consumption measured by PET 6 months after randomization. The secondary endpoints include changes in myocardial glucose consumption, NT-proBNP levels, LVEF, NYHA functional class from baseline to the last available observation after treatment, and the occurrence of predefined clinical events after receiving the study agent.
In this study, clinical events are all causes of death, cardiovascular death, left ventricular assist device implantation, listing for cardiac transplantation, hospitalization for worsening HF, and intensification of therapy defined by an increase in the diuretic dose of > 50% in the outpatient setting during the 6 months of follow-up. The adverse events will be reported from in-hospital observation and follow-ups. The study population will be instructed to contact the research staff via mobile phone at any time if adverse events occurred during the study period.
Intervention and comparator descriptions
The eligible patients are randomly assigned to either the olmesartan or valsartan group in a 1:1 fashion. Study patients assigned to the olmesartan group take olmesartan 20 mg once daily. The control arm will receive valsartan because it is widely used to treat heart failure with reduced LVEF; valsartan 40 mg twice a day is administered, and then titrated to a target of 160 mg twice daily as tolerated throughout the study period [20]. If up-titration is not clinically feasible, either because of hypotension or deepening azotemia, the previous dose is subsequently administered as the maximal tolerable dose. Any patient who is found to take less than 80% or more than 120% of the assigned study drug as assessed by tablet counts is considered non-compliant [21].
Assignment of interventions: allocation
Sequence generation
Participants are randomly assigned to either the olmesartan or valsartan group in a 1:1 fashion. Randomization will take place following coronary angiography, which is conducted after stabilization by conservative treatment. Random assignments are generated using Excel spreadsheet software (Microsoft Corporation, Redmond, CA, USA).
Concealment mechanism
Randomization is performed by a person that is not involved in this study and kept concealed. The connection will require a login, password, and study number which will be provided by the data manager from Dong-A University Hospital.
Implementation
The assigned treatment will be administered for 6 months. We will take measures to minimize drop out and any potential biases attributable to dropout will be explored statistically. If a participant wishes to withdraw from the study, the reason for withdrawal will be documented in the participant records for the subsequent analysis in the interpretation of the results.
18F-FDG PET acquisition protocol and image interpretation
18F-FDG PET imaging is performed at the core lab (Dong-A University Hospital, Busan, South Korea). All studies are performed with a Biograph mCT flow scanner (Siemens Healthcare, Knoxville, TN, USA) consisting of a PET scanner coupled with a multi-detector CT scanner, allowing the acquisition of co-registered CT and PET images at the same time. After fasting for at least 6 h, different doses of insulin (1U-5U) are injected after 40–60 min of oral administration of 25–50 g of a 50% glucose load according to different blood glucose levels, for the patients to reach an optimal blood glucose concentration of 5.55–7.77 mmol/L [22]. After confirming that the proper blood sugar level is reached, low-dose CT is acquired, first with 100 kV, 30 mAs, 0.5 s each rotation, and 3.75 mm of slice thickness, without oral or intravenous contrast media before PET acquisition. Simultaneously with the initiation of the PET acquisition, 185 MBq of 18F-FDG is rapidly injected intravenously and the PET scan is acquired for 50 min in the list-mode. Standard static, 8-bin ECG-gated, and dynamic PET images are generated from the list-mode PET data, and the first two PET images (i.e., static and gated images) are reconstructed using the last 10 min of the entire data acquisition. Dynamic PET images are also reconstructed with 33-time frames (12 × 10 s, 3 × 20 s, 6 × 20 s, 4 × 60 s, and 8 × 5 min). These frames are generated with a 200 × 200 matrix, 2-mm slice thickness, a Gaussian filter of 4 mm in full width at half maximum, three iterations, and 21 subsets.
First, myocardial FDG uptake and functional status are evaluated visually and quantitatively using the QPS and QGS programs (Cedar-Sinai Medical Center, Los Angeles, CA, USA). To produce polar maps of the LV, reorientation and segmentation are performed in the dedicated program. Two experienced nuclear medicine physicians categorize the myocardial glucose uptake into four grades based on visual evaluation: grade 0 = minimal uptake, grade 1 = mostly minimal or mild uptake, grade 2 = mostly intense or moderate uptake, and grade 3 = homogeneously intense uptake [23]. When the grading is inconsistent between the two physicians, the grade is determined by mutual consultation.
Second, the dynamic PET data are analyzed using PMOD software (v3.6, Zürich, Switzerland) to assess myocardial glucose consumption. The PET image is automatically loaded using the PMOD Cardiac PET modeling (PCARDP) module to align the directions, and the volume of interest (VOI) is set by manually adjusting the detailed direction. To generate a time-activity-curve (TAC), VOIs of the LV, right ventricle (RV), and myocardium of the heart are generated. The selected PET image is smoothed with an FWHM 4 mm 3-dimensional Gaussian filter. It is confirmed that the RV TAC appears first, the LV TAC shows the next distinct peak, and finally, the myocardial TAC appears static. To perform the simulation, we select the 18F-FDG tracer and Patlak model from the PCARDP module. For the analysis of FDG data, the patient’s lumped constant (LC) and plasma glucose level (PG) are entered. Finally, the metabolic rate of glucose (MRGlu = slopexPG / LC) is obtained from the regression slope. For cardiac PET imaging, PCARDP uses the standard American Heart Association (AHA) 17-segment model. The final results are calculated in a table form and expressed in polar coordinates.
Echocardiography
Echocardiographic examinations are performed at the participating centers and sent to the echocardiographic core lab (Dong-A University Hospital, Busan, South Korea). The analyses are performed by one experienced investigator. The biventricular dimensions and systolic and diastolic functions are assessed according to the international guidelines [24]. The left ventricular end-systolic diameter (LVESD) and left ventricular end-diastolic diameters (LVEDD) are measured by M-mode echocardiography. The LV volume and LVEF are calculated using a modified Simpson’s method. All volumes are indexed according to body surface area. All measurements are obtained from the mean of three beats (patients in sinus rhythm) or five beats (patients with atrial fibrillation).
Cardiac 123I-metaiodobenzylguanidine scans and image analysis
The condition of cardiac sympathetic nerves is assessed using 123I-metaiodobenzylguanidine (MIBG), which is a norepinephrine analog and therefore is used as a tracer for sympathetic neuron integrity and function [25, 26], at baseline and 6 months after receiving the study agent. Early and delayed cardiac MIBG scans are performed at 30 min and 3 h after the intravenous injection of 111 MBq of 123I-MIBG, respectively. A planar image is obtained with a dual-head gamma camera equipped with a low-energy high-resolution parallel-hole collimator (eCAM, Siemens Healthcare, Knoxville, TN, USA). We also obtain a cardiac single-photon emission computed tomography (SPECT) image after acquiring the delayed planar image. Medications that could affect the MIBG uptake are withheld for 24 h prior to the administration of 123I- MIBG. Relative cardiac uptake is determined by setting the region-of-interest (ROI) on the anterior view. The entire left ventricular ROI is drawn manually, and a rectangular ROI is also set on the upper mediastinal area. The heart-to-mediastinum ratio (HMR) of the early (eHMR) and delayed (dHMR) images are calculated by dividing the average count density per pixel of the left ventricular ROI by that of the mediastinal ROI, respectively. A normal HMR is defined as greater than 1.8 in the delayed image, a number based on a previous study [27]. The wash-out rate (WR), which is an index of the rate at which MIBG is washed out between the early and the delayed images, is calculated using the following formula:
A factor of 1.21 is multiplied by the delayed value to correct for the decay of 123I at 3 h [28].
Adverse events
The analysis of safety-related data is performed with respect to the frequency of serious adverse events, stratified by the causality and intensity of the morbidity in both treatment groups. At each visit, the patients are interviewed about the occurrence of any adverse events, including the time of onset, duration, and severity, and all the information is recorded on a case report form.
Withdrawals
The patients are free to withdraw from the trial upon request at any time and without providing reasons for their decision. Moreover, the primary investigator can withdraw study patients if continuation of the trial would be detrimental to the patient’s well-being. Withdrawals are documented on a case report form and in the patient’s medical records, and all ongoing severe adverse events are followed-up.
Sample size
The sample size calculation was based on the primary endpoint and primary analysis for the intention-to-treat population. The sample size was calculated using the study’s primary objective- to confirm a 20% relative difference in myocardial glucose consumption uptake between olmesartan and valsartan treatment with a power of 90%. Based on previous reports, we assumed the myocardial glucose consumption value to be approximately 50 μl/g/min in DCMP patients [29, 30]. We expected that the relative difference in glucose uptake measurement would be at least 20% in DCMP patients. We adjusted the sample size, considering an estimated follow-up loss rate of 20% with a two-sided level of significance α = 5% and a power of 1-β = 90%, resulting in 20 patients in each group to show a difference with a two-sided Student’s t-test. The sample size was increased to up to 22 patients in each group with an expected drop-outs rate of 10% at the end of the study. Therefore, a total of 44 patients will be randomized and included in this study.
Statistical analysis
Statistical analyses are performed on an intention-to-treat basis. The continuous variables are presented as mean ± SD or median and interquartile range and compared by Student’s t-test or Mann-Whitney U test, respectively, depending on the normality of the variables. The chi-squared test is used to analyze the categorical variables. Repeated measures between baseline and follow-up are evaluated using the paired t-test for continuous Gaussian-distributed parameters or the Wilcoxon test, as appropriate. Receiver operating curve analysis is used to assess the efficacy of using myocardial glucose consumption to predict clinical events. Spearman’s correlation analysis is used to analyze the correlations between myocardial glucose consumption and possible influencing factors. The independent influencing factors of myocardial glucose consumption are analyzed by multivariate logistic regression, and the regression coefficients, odds ratio, and 95% confidence intervals are calculated.
The safety analysis will include the calculation of frequencies and rates of adverse events reported in the two groups. This analysis will be performed on the full analysis set, which consists of patients who receive at least one dose of the study medication. Graphical methods, including scatter plots and boxplots, will be used to visualize the findings of the trial. Given that dropouts are expected, multiple imputations, based on regression methods, will be performed to complete the data analysis. A fully specified statistical analysis plan will be written before unmasking of the data. All statistical analyses will be performed using SPSS Version 16.0 or higher. Statistical significance is considered for p-values of < 0.05.
The report presenting the primary findings of this study will follow the Consolidated Standards of Reporting Trials 2010 guidelines. Study results will be disseminated to researchers and clinicians via publications and conference presentations. Authorship of published papers will follow established guidelines for defining the level of contribution that warrants authorship.
Data management
This study will be coordinated by Dong-A University Hospital, which is responsible for the data processing and quality control. Completed electronic case report forms will be entered by trained site personnel and will be transmitted to a central data repository at Dong-A University Hospital. At regular intervals, all data will be transferred from electronic case report form to SPSS for statistical summarization, data description, and data analysis. Further cross-checking of the data will be performed in SPSS. Site qualification will be issued by Dong-A University Hospital for each modality before subject enrollment. Before beginning enrollment, eligible sites will be qualified by the imaging Core Laboratories based on-site surveys and on the successful transfer of one or more complete datasets with sufficient image quality and completeness for each modality. During the study, technical quality assessment of image and test acquisition will be accomplished on all studies by central repository research technicians trained by the imaging Core Laboratories. This ongoing review will ensure adequate quality and completeness of datasets. The collected data will be stored for 5 years after the end of the study and will be destroyed after that.
Data monitoring
Data monitoring will be done semiannually to ensure that the electronic case report form is completed accurately. Data quality control will be regularly undertaken at each investigating site to ensure that the electronic case report form is accurately completed.
Frequency and plans for auditing trial conduct
Auditing will be conducted by the Dong-A University Hospital auditing department.
Protocol amendments
Any protocol modifications must be approved by the IRB prior to the implementation in this trial. Substantial changes will be added on ClinicalTrials.gov if there are protocol amendments from the original approved version.
Plan for data assessment
All paper files are to be stored in locked file cabinets, and electronic files are to be stored in password-protected, encrypted files. Both paper and electronic files will be accessed by members of the research team only. The final dataset will reside with the principal investigator.
Ancillary and post-trial care
Ancillary study is not planned. After the study, patients will receive a standard therapy.
Discussion
Renin-angiotensin-aldosterone system in DCMP
Overactivity of the RAAS is associated with poor patient prognosis in DCMP [7, 8]. Angiotensin II binds the angiotensin II receptor in targeted tissues and stimulates vasoconstriction and secretion of aldosterone, a steroid hormone, which mediates sodium reabsorption and water retention [31]. Aldosterone has an avid, renal sodium-water retaining effect and is considered a key hormone in the development of HF through its pleiotropic actions mediated by mineralocorticoid receptors [31]. Previous studies showed that chronic angiotensin II receptor stimulation-induced cardiac systolic dysfunction and electrical remodeling in the absence of hypertension [32, 33]. Further, a recent animal study reported that angiotensin II overstimulation led to an increased susceptibility to DCMP [34].
Myocardial metabolism in DCMP
Patients with DCMP exhibit myocardial metabolism dysfunction characterized by decreased fatty acid metabolism and increased myocardial glucose metabolism [21, 22]. Recent studies suggested that RAAS might adversely affect cardiac energy metabolism in heart failure [5, 6]. Cardiac energy metabolic changes in heart failure can manifest as both a deficit in energy production by the heart, as well as a decrease in cardiac efficiency [35, 36]. Several investigators have shown a link between myocardial metabolism and impaired heart function. Myocardial energy efficiency in HF declines to as low as 15%, whereas in healthy volunteers or patients with coronary artery disease without HF, it is as high as 40% [37]. Alterations in myocardial substrate metabolism have been implicated in the pathogenesis of contractile dysfunction and HF [38]. Therefore, a further understanding of the relationship between the RAAS and myocardial metabolism could improve the control of HF and may lead to the development of new HF therapies.
OVOID study (a comparison study of Olmesartan and Valsartan On myocardial metabolism In patients with Dilated cardiomyopathy)
Angiotensin blockade is a major DCMP therapeutic strategy; it provides a balanced reduction in preload and afterload and inhibits cardiac hypertrophy and remodeling, therefore reducing mortality and morbidity [19, 39, 40]. This trial is conducted to test the hypothesis that olmesartan could improve myocardial metabolism more effectively than valsartan for DCMP patients during a 6-month follow-up period. This is a short-term clinical study. However, this is the first trial investigating the potential benefits of 6 months olmesartan treatment on myocardial metabolism in DCMP patients. There are some pharmacological differences between the different ARBs. Among them, individual studies have demonstrated differences between ARBs efficacy in lowering blood pressure [13, 14, 41, 42]. However, as of March 2020, there have been no registered randomized trials comparing ARBs in patients with DCMP. Olmesartan has a double-chained domain consisting of carboxyl and hydroxyl groups, which can strongly combine with the angiotensin II receptor [15, 16]. Recently, Ishiyama reported that olmesartan increased ACE2 expression in the remodeling heart after myocardial infarction, which theoretically could contribute to the beneficial effects of ARB by facilitating increased cardiac Ang-(1-7) formation [43]. Olmesartan can block the angiotensin II receptors more efficiently because angiotensin II does not increase and can also enhance the effect of bradykinin through the inhibition of kininase II. Moreover, the increased Ang-(1-7) may have vasodilatory and organ-protective effects, such as the inhibition of vascular remodeling and cardiac hypertrophy [44–46]. If the potential benefits of olmesartan on myocardial metabolism are proved, the results of the present study may demonstrate the differential effects of ARBs as metabolic therapy.
Supplementary Information
Additional file 1: Appendix A. SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents*. Appendix B. World Health Organization Trial Registration Data Set. Appendix C. Informed consent (only for Korean).
Acknowledgements
We would like to thank all members of the present study group for their ideas, suggestions, participation, and support. The authors are solely responsible for the study design and the conduct of the study, all data analyses, drafting, and editing of this and future manuscripts, trial reports, and their final contents.
Trial status
The OVOID study trial received ethical approval on 6 November, 2019 (Protocol version 2, 18-215). The trial is registered at www.clinicaltrials.gov (NCT04174456); 18 November 2019. The recruitment of participants started in December 2019 and was completed in December 2021.
Abbreviations
- ACE
Angiotensin-converting enzyme
- AHA
American Heart Association
- ARB
Angiotensin II receptor blocker
- DCMP
Dilated cardiomyopathy
- FDG
18F-fluoro-2-deoxyglucose
- HF
Heart failure
- HMR
Heart-to-mediastinum ratio
- NT-proBNP
N-terminal pro-B-type natriuretic peptide
- LC
Lumped constant
- LV
Left ventricle
- LVEDD
Left ventricular end-diastolic diameters
- LVEF
Left ventricular ejection fraction
- LVESD
Left ventricular end-systolic diameter
- MIBG
123I-metaiodobenzylguanidine
- NYHA
New York Heart Association
- OVOID
A comparison study of Olmesartan and Valsartan On myocardial metabolism In patients with Dilated cardiomyopathy
- PCARDP
PMOD Cardiac PET modeling
- PET
Positron emission tomography
- PG
Plasma glucose level
- RAAS
Renin-angiotensin-aldosterone systems
- ROI
Region-of-interest
- RV
Right ventricle
- SPECT
Single-photon emission computed tomography
- TAC
Time-activity-curve
- VOI
Volume of interest
- WR
Wash-out rate
Authors’ contributions
KP, the principle investigator for this study, contributed to the study design, drafting, and revising of the manuscript. SJ made significant contributions to drafting and revising the manuscript. All authors contributed to patient enrollment and treatment. All authors have approved the final manuscript.
Funding
This trial is an investigator-initiated trial supported by a grant from Daewoong. No source or funding was used to support the creation of this paper. The funding body does not interfere in the analysis and interpretation of the data.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
The study protocol was approved the Dong-A University Hospital Institutional Review Board (IRB 18-215). Written informed consent will be obtained and documented for all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sua Jo, Email: flysofina@gmail.com.
Kyungil Park, Email: cardiopark@gmail.com.
References
- 1.Japp AG, Gulati A, Cook SA, Cowie MR, Prasad SK. The diagnosis and evaluation of dilated cardiomyopathy. J Am Coll Cardiol. 2016;67(25):2996–3010. doi: 10.1016/j.jacc.2016.03.590. [DOI] [PubMed] [Google Scholar]
- 2.Katz AM. Mechanisms and abnormalities of contractility and relaxation in the failing heart. Cardiologia. 1993;38(12 Suppl 1):39–43. [PubMed] [Google Scholar]
- 3.Eichhorn EJ, Hesch CN, Barnett JH, et al. Effect of metoprolol on myocardial function and energetics in patients with nonischemic dilated cardiomyopathy: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol. 1994;24(5):1310–1320. doi: 10.1016/0735-1097(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 4.Kjekshus JK, Mjos OD. Effect of inhibition of lipolysis on myocardial oxygen consumption in the presence of isoproterenol. J Clin Invest. 1972;51(7):1767–1776. doi: 10.1172/JCI106978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mori J, Zhang L, Oudit GY, Lopaschuk GD. Impact of the renin-angiotensin system on cardiac energy metabolism in heart failure. J Mol Cell Cardiol. 2013;63:98–106. doi: 10.1016/j.yjmcc.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Mori J, Alrob OA, Wagg CS, Harris RA, Lopaschuk GD, Oudit GY. ANG II Causes insulin resistance and induces cardiac metabolic switch and inefficiency: a critical role of PDK4. Am J Physiol Heart Circ Physiol. 2013;304(8):H1103–H1113. doi: 10.1152/ajpheart.00636.2012. [DOI] [PubMed] [Google Scholar]
- 7.Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14(1):30–38. doi: 10.1038/nrcardio.2016.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tripathi R, Sullivan R, Fan TM, et al. Enhanced heart failure, mortality and renin activation in female mice with experimental dilated cardiomyopathy. PLoS One. 2017;12(12):e0189315. doi: 10.1371/journal.pone.0189315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burniston JG, Saini A, Tan LB, Goldspink DF. Angiotensin II induces apoptosis in vivo in skeletal, as well as cardiac, muscle of the rat. Exp Physiol. 2005;90(5):755–761. doi: 10.1113/expphysiol.2005.030908. [DOI] [PubMed] [Google Scholar]
- 10.Pellieux C, Aasum E, Larsen TS, Montessuit C, Papageorgiou I, Pedrazzini T, Lerch R. Overexpression of angiotensinogen in the myocardium induces downregulation of the fatty acid oxidation pathway. J Mol Cell Cardiol. 2006;41(3):459–466. doi: 10.1016/j.yjmcc.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Singh KD, Karnik SS. Angiotensin type 1 receptor blockers in heart failure. Current drug targets. 2020;21(2):125–131. doi: 10.2174/1389450120666190821152000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sukumaran V, Watanabe K, Veeraveedu PT, Thandavarayan RA, Gurusamy N, Ma M, Yamaguchi K', Suzuki K, Kodama M, Aizawa Y. Beneficial effects of olmesartan, an angiotensin II receptor type 1 antagonist, in rats with dilated cardiomyopathy. Exp Biol Med. 2010;235(11):1338–1346. doi: 10.1258/ebm.2010.010016. [DOI] [PubMed] [Google Scholar]
- 13.Oparil S, Williams D, Chrysant SG, Marbury TC, Neutel J. Comparative efficacy of olmesartan, losartan, valsartan, and irbesartan in the control of essential hypertension. J Clin Hypertens. 2001;3(5):283–291. doi: 10.1111/j.1524-6175.2001.01136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith DH, Dubiel R, Jones M. Use of 24-hour ambulatory blood pressure monitoring to assess antihypertensive efficacy: a comparison of olmesartan medoxomil, losartan potassium, valsartan, and irbesartan. Am J Cardiovasc Drugs. 2005;5(1):41–50. doi: 10.2165/00129784-200505010-00006. [DOI] [PubMed] [Google Scholar]
- 15.Laeis P, Püchler K, Kirch W. The pharmacokinetic and metabolic profile of olmesartan medoxomil limits the risk of clinically relevant drug interaction. J Hypertens Suppl. 2001;19(1):S21–S32. doi: 10.1097/00004872-200106001-00004. [DOI] [PubMed] [Google Scholar]
- 16.Scott LJ, McCormack PL. Olmesartan medoxomil: a review of its use in the management of hypertension. Drugs. 2008;68(9):1239–1272. doi: 10.2165/00003495-200868090-00005. [DOI] [PubMed] [Google Scholar]
- 17.Ono T, Sanai T, Miyahara Y, Noda R. Olmesartan is more effective than other angiotensin receptor antagonists in reducing proteinuria in patients with chronic kidney disease other than diabetic nephropathy. Curr Ther Res Clin Exp. 2013;74:62–67. doi: 10.1016/j.curtheres.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinto YM, Elliott PM, Arbustini E, Adler Y, Anastasakis A, Böhm M, Duboc D, Gimeno J, de Groote P, Imazio M, Heymans S, Klingel K, Komajda M, Limongelli G, Linhart A, Mogensen J, Moon J, Pieper PG, Seferovic PM, Schueler S, Zamorano JL, Caforio ALP, Charron P. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J. 2016;37(23):1850–1858. doi: 10.1093/eurheartj/ehv727. [DOI] [PubMed] [Google Scholar]
- 19.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 20.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey de Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride P, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776–803. doi: 10.1016/j.jacc.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 21.Demonceau J, Ruppar T, Kristanto P, et al. Identification and assessment of adherence-enhancing interventions in studies assessing medication adherence through electronically compiled drug dosing histories: a systematic literature review and meta-analysis. Drugs. 2013;73(6):545–562. doi: 10.1007/s40265-013-0041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dilsizian V, Bacharach SL, Beanlands RS, Bergmann SR, Delbeke D, Dorbala S, Gropler RJ, Knuuti J, Schelbert HR, Travin MI. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 2016;23(5):1187–1226. doi: 10.1007/s12350-016-0522-3. [DOI] [PubMed] [Google Scholar]
- 23.Williams G, Kolodny GM. Suppression of myocardial 18F-FDG uptake by preparing patients with a high-fat, low-carbohydrate diet. AJR Am J Roentgenol. 2008;190(2):W151–W156. doi: 10.2214/AJR.07.2409. [DOI] [PubMed] [Google Scholar]
- 24.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Dimitriu-Leen AC, Scholte AJ, Jacobson AF. 123I-MIBG SPECT for evaluation of patients with heart failure. J Nucl Med. 2015;56(Supplement 4):25S–30S. doi: 10.2967/jnumed.115.157503. [DOI] [PubMed] [Google Scholar]
- 26.Zelt JGE, deKemp RA, Rotstein BH, Nair GM, Narula J, Ahmadi A, Beanlands RS, Mielniczuk LM. Nuclear imaging of the cardiac sympathetic nervous system: a disease-specific interpretation in heart failure. JACC Cardiovasc Imaging. 2020;13(4):1036–1054. doi: 10.1016/j.jcmg.2019.01.042. [DOI] [PubMed] [Google Scholar]
- 27.Carrió I. Cardiac neurotransmission imaging. J Nucl Med. 2001;42(7):1062–1076. [PubMed] [Google Scholar]
- 28.Travin MI. Cardiac autonomic imaging with SPECT tracers. J Nucl Cardiol. 2013;20(1):128–143. doi: 10.1007/s12350-012-9655-1. [DOI] [PubMed] [Google Scholar]
- 29.Dávila-Román VG, Vedala G, Herrero P, de las Fuentes L, Rogers JG, Kelly DP, Gropler RJ. Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 2002;40(2):271–277. doi: 10.1016/s0735-1097(02)01967-8. [DOI] [PubMed] [Google Scholar]
- 30.van den Heuvel AF, van Veldhuisen DJ, van der Wall EE, et al. Regional myocardial blood flow reserve impairment and metabolic changes suggesting myocardial ischemia in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 2000;35(1):19–28. doi: 10.1016/s0735-1097(99)00499-4. [DOI] [PubMed] [Google Scholar]
- 31.Weber KT. Aldosterone in congestive heart failure. N Engl J Med. 2001;345(23):1689–1697. doi: 10.1056/NEJMra000050. [DOI] [PubMed] [Google Scholar]
- 32.Paradis P, Dali-Youcef N, Paradis F, et al. Overexpression of angiotensin II type 1 receptor in cardiomyocytes induces cardiac hypertrophy and remodeling. Proc Natl Acad Sci. 2000;97(2):931–936. doi: 10.1073/pnas.97.2.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rivard K, Paradis P, Nemer M, Fiset C. Cardiac-specific overexpression of the human type 1 angiotensin II receptor causes delayed repolarization. Cardiovasc Res. 2008;78(1):53–62. doi: 10.1093/cvr/cvn020. [DOI] [PubMed] [Google Scholar]
- 34.Mathieu S, El Khoury N, Rivard K, Paradis P, Nemer M, Fiset C. Angiotensin II overstimulation leads to an increased susceptibility to dilated cardiomyopathy and higher mortality in female mice. Sci Rep. 2018;8(1):952. doi: 10.1093/cvr/cvn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanley WC, Recchia FA, Lopaschuk GD. Myocardial substrate metabolism in the normal and failing heart. Physiol Rev. 2005;85(3):1093–1129. doi: 10.1152/physrev.00006.2004. [DOI] [PubMed] [Google Scholar]
- 36.Lopaschuk GD, Ussher JR, Folmes CD, et al. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90(1):207–258. doi: 10.1152/physrev.00015.2009. [DOI] [PubMed] [Google Scholar]
- 37.Takaoka H, Takeuchi MT, Odake M. Comparison of hemodynamic determinants for myocardial oxygen consumption under different contractile states in human ventricle. Circulation. 1993;87(1):59–69. doi: 10.1161/01.cir.87.1.59.. [DOI] [PubMed] [Google Scholar]
- 38.Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circ Res. 2013;113(6):709–724. doi: 10.1161/CIRCRESAHA.113.300376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohn JN, Tognoni G, Valsartan Heart Failure Trial Investigators A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345(23):1667–1675. doi: 10.1056/NEJMoa010713. [DOI] [PubMed] [Google Scholar]
- 40.Park K, Kim YD, Kim KS, Lee SH, Park TH, Lee SG, Kim BS, Hur SH, Yang TH, Oh JH, Hong TJ, Park JS, Hwang JY, Jeong B, Bae WH, VALID Investigators The impact of a dose of the angiotensin receptor blocker valsartan on post-myocardial infarction ventricular remodelling. ESC Heart Fail. 2018;5(2):354–363. doi: 10.1002/ehf2.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dézsi CA. The different therapeutic choices with ARBs. Which one to give? When? Why? Am J Cardiovasc Drugs. 2016;16(4):255–266. doi: 10.1007/s40256-016-0165-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abraham HMA, White CM, White WB. The comparative efficacy and safety of the angiotensin receptor blockers in the management of hypertension and other cardiovascular diseases. Drug Saf. 2015;38(1):33–54. doi: 10.1007/s40264-014-0239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension. 2004;43(5):970–976. doi: 10.1161/01.HYP.0000124667.34652.1a. [DOI] [PubMed] [Google Scholar]
- 44.Strawn WB, Ferrario CM, Tallant EA. Angiotensin-(1-7) reduces smooth muscle growth after vascular injury. Hypertension. 1999;33(1):207–211. doi: 10.1161/01.hyp.33.1.207. [DOI] [PubMed] [Google Scholar]
- 45.Ferreira AJ, Santos RAS, Almeida AP. Angiotensin-(1-7): cardioprotective effect in myocardial ischemia/reperfusion. Hypertension. 2001;38(3):665–668. doi: 10.1161/01.hyp.38.3.665. [DOI] [PubMed] [Google Scholar]
- 46.Averill DB, Ishiyama Y, Chappell MC, Ferrario CM. Cardiac angiotensin-(1-7) in ischemic cardiomyopathy. Circulation. 2003;108(17):2141–2146. doi: 10.1161/01.CIR.0000092888.63239.54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix A. SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents*. Appendix B. World Health Organization Trial Registration Data Set. Appendix C. Informed consent (only for Korean).
Data Availability Statement
Not applicable.


