Abstract
Background
Although ACDF has been widely used in treating cervical spondylosis and related diseases, the complications along with this anterior surgical technique have hindered its application and affected the postoperative outcome of the patients. Here, we investigated the clinical and radiological outcomes of a new integrated low-profile anterior plate and cage system for anterior cervical discectomy and fusion (ACDF) in treating cervical spondylosis.
Methods
A total of 96 cervical spondylosis patients who underwent single-level ACDF between 2018 to 2020 in our institute were enrolled. There were 28 patients using the new implants and 68 patients using the zero-profile (Zero-P) implants. The Japanese Orthopedic Association (JOA) score and the visual analog scale (VAS) were used to evaluate the clinical outcomes. The cervical and segmental Cobb angle and range of motion (ROM) were used to assessed the radiological outcomes. Incidence of complications were also recorded. All data were recorded at pre-operation, 6-month and 12-month post-operation.
Results
All patients were followed-up for at least 1-year, the mean follow-up time was over one year. The fusion rate was similar in the two groups. There was no significant difference in the postoperative JOA score recovery rate, postoperative VAS score of neck and arm pain, postoperative ROM, and incidence of complications between two groups (P > 0.05). However, postoperative cervical and segmental Cobb angle were better maintained in the new low-profile implant group compared to Zero-P group.
Conclusions
The clinical outcomes of the new low-profile implant were satisfactory and comparable to that of zero-profile system. It may have advantages in improving and maintaining the cervical lordosis, and can be an alternative device for single-level cervical spondylosis treated with ACDF.
Keywords: Cervical spondylosis, Alignment, ACDF, Carmen
Background
Anterior Cervical Discectomy and Fusion (ACDF) is one of the most common and effective surgical approach to treat cervical spondylosis. Since first introduced by Smith Robinson [1] and Cloward [2] in 1958, the ACDF procedure has become widely used till nowadays and is still proved as a standard procedure for cervical spondylosis. Although the surgical approach has not been changed for many years, the implants on the other hand have kept involving to minimizing the side effects and complications along with this surgical method.
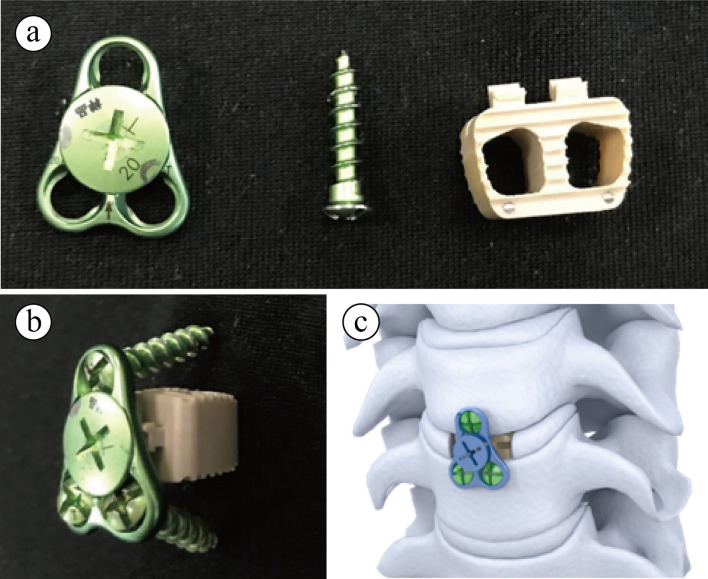
Varies implants were designed to promote segmental fusion and achieve better clinical outcomes. Although traditional bone grafting is reliable, It is then replaced by plate and cage system for its stability and does not need to prepare grafting materials from iliac bone of the patients. However, despite its advantages at restoring cervical alignment and maintain cervical height, it may also lead to complications like dysphagia, esophageal perforation and adjacent segment degeneration [3–5]. Recently, the zero-profile implant (Zero-P) has been invented and widely used for one or two segmental ACDF surgeries [6], and found that Zero-P implant could attain similar clinical results and significantly lowered the incidence of dysphagia and adjacent segment degeneration when compared to plate and cage system [7–11]. The reason of which may be due to its integrated design that does not protrudes the front rim of the cervical vertebrate. It is not until recent years that studies have reported that postoperative loss of cervical alignment has been observed in ACDF with Zero-P implant [12, 13], and further caused recurrent symptoms or revisions. Compared to titanium plate and cage system, Zero-P implant may cause postoperative lordosis loss and bone absorption, which is more significant on longer terms [13]. Considering the drawbacks of both types of implants, we here present a new integrated low-profile anterior plate and cage system (Carmen, Shanghai Sanyou Medical Co., Ltd, Shanghai, China) which is approved by the United States Food and Drug Administration in 2018. In this system, a titanium triangular thin plate with 3 screw trajectories can be attached to polyetheretherketone (PEEK) made disc spacer (Fig. 1a–c), since it mimics the zero-profile system and retain small plate design for screw fixation, we name it a low-profile anterior plate and cage system. The system is designed to combine both the advantages of traditional plate and cage system and zero-profile implants to avoid the complications in either system. Thus, the purpose of this study is to give the initial outcome of this new system and compare the clinical and radiological outcomes with the zero-profile implant.
Fig. 1.
The design of a new integrated low-profile mini plate and cage system. a The new integrated low-profile mini plate and cage system can be divided into a triangular plate piece, the locking screw and self-drilling screw, and a polyetheretherketone (PEEK) cage with hook to attach to the plate (b). When used in cervical ACDF surgery, only the thin triangular titanium plate protrudes the vertebrate (c)
Methods
Patient population
All study procedures were approved by the institute chancellor’s Human Research Committee in accordance with institute’s protocol. Patients who underwent single-level anterior cervical diskectomy and fusion (ACDF) for diagnosed cervical radiculopathy or myelopathy between January 2018 and January 2020 in our institute were reviewed. The exclusion criteria included as follows: (1) ossification of the posterior longitudinal ligament; (2) acute spinal cord injuries; (3) severe cervical kyphosis; (4) history of cervical surgery; (5) thoracic or lumbar diseases; (6) history of rheumatoid, cerebral palsy, or tumors. Altogether 28 patients who underwent single-level ACDF with the new low-profile anterior plate and cage system (Carmen, Shanghai Sanyou Medical Co., Ltd, Shanghai, China) is included in this study, and 68 patients with Zero-P (DePuy Synthes, USA) for single-level ACDF symptomatic cervical spondylosis were retrospectively enrolled in this study. All patients were followed up regularly, with the mean follow-up time of 15.19 months (from 12 to 24).
Surgical technique
Under general anesthesia, the patients were placed in supine position. Then, a standard Smith-Robinson method was used. The surgical level was confirmed by intraoperative radiography. A thorough decompression was performed by removing the disc, part of posterior longitudinal ligament, and osteophytes. After scraping off the cartilaginous endplate, a suitable Carmen implant (Carmen group, Fig. 1a–c) or Zero-P implant (Zero-P group) was inserted in the disc space. And correct position of implants was reconfirmed by using intraoperative X-ray. All the ACDF surgeries were performed by the same surgeon. Patients were allowed to sit up and walk on the second day after surgery with a protection of Philadelphia collars. The collars were maintained in 2–3 weeks for all patients.
Clinical outcomes
Intraoperative measurements, including operative time and blood loss, were recorded. The clinical outcomes were assessed by using the Japanese Orthopedic Association (JOA) score and visual analog scale (VAS) of neck and arm pain. The recovery rate of JOA score was calculated by the following formula: Recovery rate (%) = (postoperative JOA score − preoperative JOA score)/(17 − preoperative JOA score) × 100%. Besides, incidence of dysphagia was also recorded.
Radiographical outcomes
All the patients were performed anteroposterior, lateral, and maximal flexion–extension lateral radiographic images before and after surgery. All the radiological measurements were analyzed by the Image J software (National Institutes of Health, Bethesda, Maryland).
The cervical alignment assessed by Cobb angle was measured between the upper endplate of C2 and the lower endplate of C7. Similarly, the segmental lordosis of the surgical level was measured by using Cobb method between the upper endplate of the upper vertebrate body and the lower endplate of the lower vertebrate body. Range of motion (ROM) of cervical spine was also measured by calculating the difference in the alignment at flexion and extension [14]. Proportion of ROM preserved (ROM preservation) was calculated by the following formula: ROM preservation = (postoperative ROM)/(preoperative ROM) × 100%.
Statistical analysis
The data in this study were collected and analyzed by using the SPSS 18.0 (SPSS, Inc., USA). Continuous variables were shown in means and standard deviations (SD), and categorical variables in frequencies and percentages. Continuous variables were first tested for normality using the Shapiro–Wilk test, and statistically significant differences between the different subgroups were tested with Pearson’s Chi-square tests for categorical and Mann–Whitney U tests for continuous data that did not passed the normality test, otherwise were tested with Student’s t-test. P value less than 0.05 was considered statistically significant.
Results
Patients’ demographic analysis
Demographic data were summarized in Table 1. The new integrated low-profile implant Carmen was first used in 2018 in our institute, and was used in 28 patients until January 2020 (all patients were diagnosed as single-level cervical spondylosis, and were defined as Carmen group in the following study). 68 patients who received single-level ACDF with Zero-P device were defined as Zero-P group. The surgical segments ranged from C3 to C7, and the distribution of lesion segment showed no significant difference between two groups (P = 0.208). There were also no statistic differences in the gender, age, smoking status, BMI and duration of symptoms between two groups (P > 0.05, Table 1).
Table 1.
Demographic data of study groups
| Carmen group | Zero-P group | P value | |
|---|---|---|---|
| Patients (n) | 28 | 68 | |
| Gender | 0.400 | ||
| Male | 15 | 36 | |
| Female | 13 | 32 | |
| Age (years) | 47.2 ± 6.7 | 48.7 ± 7.3 | 0.339 |
| Smoking status | 0.957 | ||
| Smoking | 12 | 30 | |
| Non-smoking | 16 | 38 | |
| BMI | 22.5 ± 1.8 | 22.8 ± 2.2 | 0.488 |
| Duration of symptoms (months) | 14.4 ± 7.6 | 15.4 ± 5.9 | 0.492 |
| Lesion segment | 0.208 | ||
| C3/4 | 5 | 6 | |
| C4/5 | 8 | 21 | |
| C5/6 | 15 | 32 | |
| C6/7 | 9 | 9 | |
| Follow-up time | 15.1 ± 5.2 | 15.3 ± 5.2 | 0.859 |
BMI, body mass index. A P value of less than 0.05 was considered to indicate a statistically significant difference
Neurological outcome
The mean operative time, blood loss, and fusion rate were similar between two groups (Table 2). The mean JOA score was 9.76 ± 0.76 preoperatively and 13.58 ± 1.59 (6 months), 15.28 ± 1.17 (12 months) postoperatively, with the mean recovery rate of 76.24 ± 7.24 in the Carmen group at 12-month follow-up. And similar result was found in Zero-P group, with the mean JOA score was 9.52 ± 0.81 preoperatively and 13.12 ± 1.67 (6 months), 14.52 ± 1.23 (12 months) postoperatively, and the mean recovery rate was 66.84 ± 7.96 at 12-month follow-up. With regard to neck and arm VAS outcome, we also found that no significant differences exist between the two groups (P > 0.05, Table 2).
Table 2.
Clinical outcomes between two implant groups
| Carmen group | Zero-P group | P value | |
|---|---|---|---|
| Operative time (min) | 53.16 ± 5.29 | 55.24 ± 5.17 | 0.082 |
| Blood loss (mL) | 32.46 ± 8.31 | 34.52 ± 6.42 | 0.218 |
| Fusion rate (%) | 100 | 98.5 | 0.921 |
| JOA score | |||
| Preoperation | 9.76 ± 0.76 | 9.52 ± 0.81 | 0.442 |
| Postoperation (6 m) | 13.58 ± 1.59 | 13.12 ± 1.67 | 0.298 |
| Postoperation (12 m) | 15.28 ± 1.17 | 14.52 ± 1.23 | 0.213 |
| Recovery rate (6 m) | 52.76 ± 7.81 | 48.13 ± 8.02 | 0.141 |
| Recovery rate (12 m) | 76.24 ± 7.24 | 66.84 ± 7.96 | 0.064 |
| Neck VAS | |||
| Preoperation | 4.16 ± 0.80 | 4.43 ± 0.88 | 0.452 |
| Postoperation (6 m) | 0.86 ± 0.75 | 1.02 ± 0.78 | 0.137 |
| Postoperation (12 m) | 0.52 ± 0.43 | 0.89 ± 0.51 | 0.052 |
| Arm VAS | |||
| Preoperation | 6.70 ± 0.87 | 6.81 ± 0.89 | 0.573 |
| Postoperation (6 m) | 0.68 ± 0.71 | 0.81 ± 0.81 | 0.223 |
| Postoperation (12 m) | 0.55 ± 0.40 | 0.77 ± 0.52 | 0.134 |
JOA, the Japanese Orthopedic Association score; VAS, the visual analog scale. A P value of less than 0.05 was considered to indicate a statistically significant difference
Radiological outcome
Cervical alignment and the segmental Cobb angle of the surgery level were assessed and compared between the two groups. Although no significant difference was found in pre-operative cervical Cobb angle and segmental Cobb angle between two groups (P > 0.05), and initial post-operative (3 days P.O.) cervical Cobb angle and segmental Cobb angle between two groups (P > 0.05), both the cervical Cobb angle and segmental Cobb angle showed significant differences at one-year follow-up (Table 3), with the cervical Cobb angle and segmental Cobb angle significantly higher in the Carmen group than that in the Zero-P group (P < 0.01, Fig. 2a–f). Besides, there was no statistic difference in preoperative ROM, postoperative ROM, and its preservation between two groups (P > 0.05). Figure 2 shown the representative cervical X-ray images of typical case from the Carmen group and the Zero-P group, respectively.
Table 3.
Radiological features between two implant groups
| Carmen group | Zero-P group | P value | |
|---|---|---|---|
| Cervical Cobb angle (°) | |||
| Preoperation | 8.72 ± 5.82 | 9.35 ± 4.82 | 0.453 |
| Postoperation (3 days) | 16.19 ± 4.95 | 15.33 ± 4.42 | 0.405 |
| Postoperation (12 m) | 15.98 ± 5.25 | 12.53 ± 4.42 | 0.012* |
| Segmental Cobb angle (°) | |||
| Preoperation | 3.01 ± 1.33 | 3.42 ± 1.25 | 0.174 |
| Postoperation (3 days) | 5.59 ± 1.76 | 5.73 ± 1.57 | 0.702 |
| Postoperation (12 m) | 5.69 ± 1.71 | 4.19 ± 1.18 | 0.024* |
| Total ROM (°) | |||
| Preoperation | 38.31 ± 7.49 | 37.22 ± 6.79 | 0.538 |
| Postoperation (12 m) | 33.25 ± 7.43 | 31.48 ± 6.91 | 0.242 |
| Preservation rate (%) | 87.53 ± 15.89 | 85.07 ± 14.92 | 0.321 |
ROM, range of motion. A P value of less than 0.05 was considered to indicate a statistically significant difference
Fig. 2.
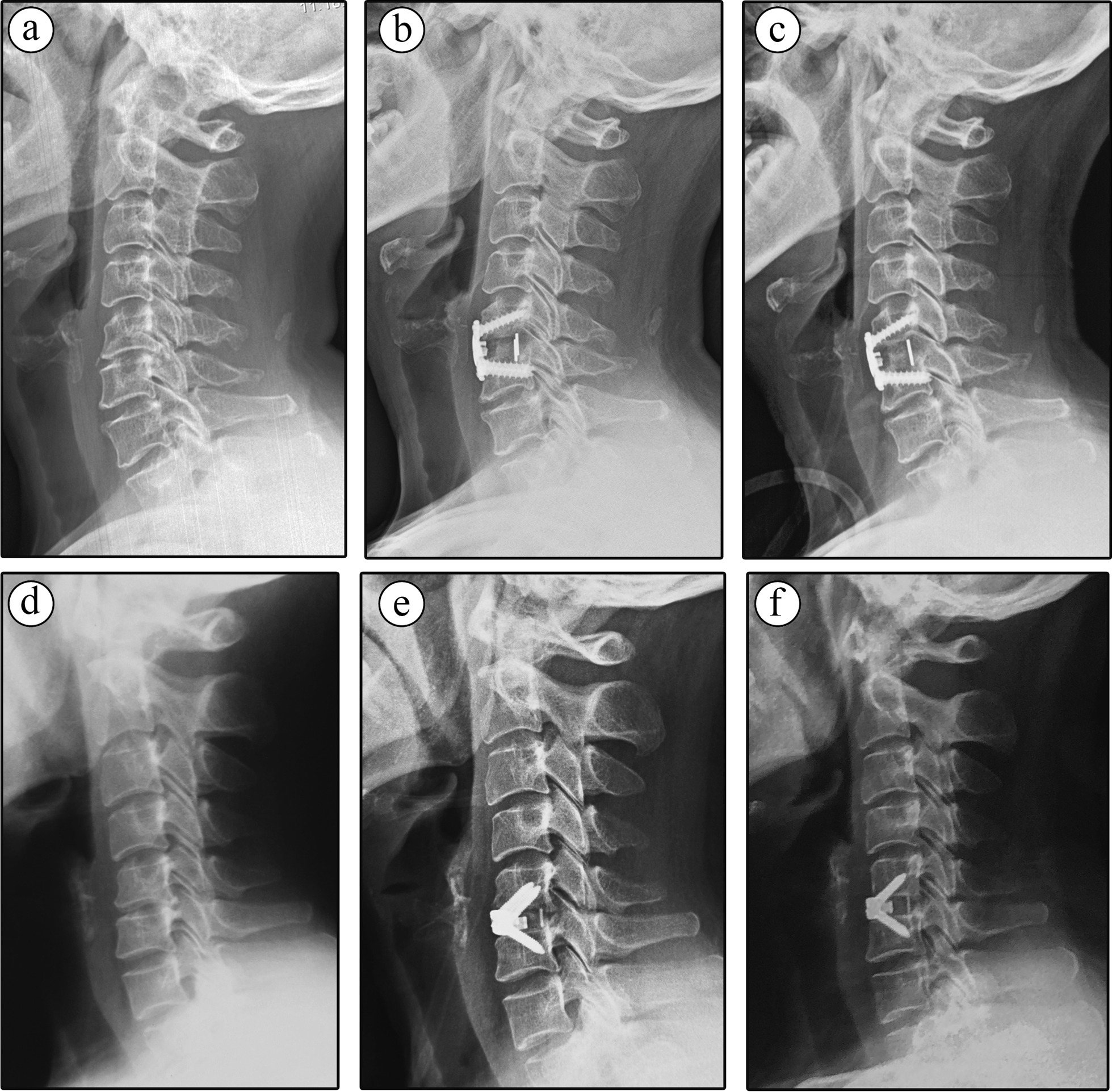
Representative cervical X-ray images of Carmen and Zero-P implant treated patient. a–c Single-level male patient treated with Carmen device, the segmental Cobb angle of C5–C6 changed from 11-degree lordosis to 18-degree lordosis after the surgery, and reached 20-degree at one-year follow-up, as well as the C2–C7 Cobb angle. d, e Single-level male patient treated with Zero-P device, the segmental Cobb angle of C5–C6 changed from 7-degree lordosis to 9-degree lordosis after the surgery, and decreased to 4-degree at one-year follow-up, as well as the C2–C7 Cobb angle (15-degree preoperative, 20-degree postoperative and 15-degree at one-year follow-up)
Complications
The incidence of postoperative dysphagia occurred in 1 patient in Carmen group and 2 in Zero-P group, all these patients had no symptom at 6-month follow-up, and no patient suffered severe dysphagia (Table 4). For adjacent segment degeneration, 2 patients in Carmen group and 5 patients in Zero-P group had adjacent disc degeneration during follow-up, but no significant compression and neurological symptoms occurred (Table 4). 2 patients in Zero-P group suffered postoperative axial pain after the surgery, and recovered within 6-month (Table 4). 1 patient had pseudoarthrosis in Zero-P group and did not achieve fusion until 12-month post-operation (Table 4).
Table 4.
Incidence of complications between two groups
| Carmen group | Zero-P group | P value | |
|---|---|---|---|
| Dysphagia | 1 (3.6) | 2 (3.0) | 0.872 |
| ASD (n, %) | 2 (7.1) | 5 (7.4) | 0.971 |
| Axial pain (n, %) | 0 (0) | 2 (3.0) | 0.359 |
| Pseudoarthrosis | 0 (0) | 1 (1.5) | 0.519 |
| Implant failure | 0 (0) | 0 (0) | – |
| Revisions | 0 (0) | 0 (0) | – |
ASD, adjacent segment degeneration. A P value of less than 0.05 was considered to indicate a statistically significant difference
Discussion
Since ACDF was first introduced by Smith Robinson and Cloward in 1958, this surgical technique has been widely used for the treatment of cervical degenerative disc diseases [1]. Initially, autologous bone graft was used to achieve intervertebral fusion. However, the use of bone graft could lead to the donor-site complications including hematoma formation, neurological injury, infection, and pain [15]. Later on, various types of implants and devices have been developed to assist intervertebral fusion. Of all devices, the plate and cage system can provide solid stability and improve cervical sagittal alignment [16], and is widely used till now due to such advantages. However, this system has been reported to have higher risks of having complications like dysphagia and adjacent segment degeneration (ASD), which were not negligible. Thus, recently developed zero-profile implant system (Zero-P for example) was designed to decreased the incidence of dysphagia and ASDs [17].
Although Zero-P system has been proved to have advantages over traditional plate and cage system in postoperative complications, and has comparable clinical outcomes to traditional plate and cage system as provided by previous researches [7–9, 11, 18], it is less efficient in dealing with cervical alignment anomalies. Recent reports have demonstrated that compared with titanium plate and cage system, zero profile system failed to maintain C2-7 Cobb angle, segmental Cobb angle and adjacent vertebral height in longer follow-ups [16]. While other reports showed that multiple Zero-P fixation failed to maintain cervical lordosis when compared to plate and cage system [13]. And recent meta-analysis found that traditional plate and cage system can restore the cervical alignment better than Zero-P implants [10, 12, 19, 20]. Thus, how to achieve best clinical outcomes and prevent loss of lordosis and other complications like ASDs after ACDF is still controversial.
Here, we retrospectively studied the a newly designed low-profile mini plate system, the Carmen system, and compared the initial clinical outcome and radiological results after one-year follow-up in single level cervical spondylosis. The findings showed that, both the Carmen system and Zero-P system could achieve similar neurological outcome and maintain functional recovery till one-year follow-up, which confirmed that the Carmen design is eligible for ACDF surgeries. Cervical lordosis plays an important role in maintaining the sagittal alignment and spinal balance. Loss of cervical lordosis is related to pain, disability, and undesirable loading shift of the thoracic and lumbar spine, and could result in adjacent segment degeneration or other issues [7]. For Carmen is mainly aimed to achieve better lordosis maintenance than the zero-profile system. The plate of which is designed with low profile triangle shape, which automatically affixes the bone surface and accords with the direction of vertical stress conduction. The triangular frame can effectively control the transverse shear force caused by fretting, ensure fusion, and avoid postoperative complications. Here we found that both the C2–C7 cervical Cobb and segmental Cobb angle were initially restored after the surgery, and were maintained during follow-ups in the Carmen group than those in the Zero-P group. The possible reason for these results may be due to the trilateral mini plate designed to restrict cage subsidence and maintain segmental curvature. Another possible reason may be attributed to the screw placement differences in two devices, which they go through the cortical bone in a more parallel angle in Carmen implant, while the screws go through the cage first and then go through the endplate to the cancellous bone in zero profile device, as mentioned in previous studies [16, 21].
Dysphagia is a well-known postoperative complication after ACDF. The incidence of dysphagia varies widely, with the rate of 50.2%, 32.2%, 17.8%, and 12.5% at 1, 2, 6, and 12 months, respectively [22]. The exact reason for dysphagia is still unclear. Female gender, multiple surgical level, esophageal injury, postoperative soft tissue edema, adhesive formations around implanted cervical plates, and postoperative hematoma may be the risk factors for dysphagia. Previous studies reported that the incidence of dysphagia was significantly higher in traditional plate and cage than that in the Zero-P implant [20, 23]. In this study, we found that the use of the Carmen implant and the Zero-P implant both led to the similar incidence of dysphagia after the operation, and none had severe dysphagia more than 6 months. Lee et al. [24] reported that the use of a smaller and smoother plate indeed reduced the incidence of dysphagia as compared with a slightly larger and less smooth plate. In our new design, the trilateral plate used in Carmen implant is smaller and smoother than traditional plate. So, this is the possible reason for similar incidence of dysphagia in the Carmen implant compared with the Zero-P implant. For other complications like ASDs, axial pain and pseudoarthrosis, both implants showed no differences when compared, and it may be due to the sample size that needs further studies.
The present study also had several limitations. Firstly, the nature of this study was retrospective, the observed results should be further studied using cohort to rule out the bias. Secondly, the patient population was relatively small in the Carmen implant group, for initial data is needed to further expand its usage, which will be done in the future. Thirdly, the follow-up duration was relatively short. Despite these limitations, this study was the first clinical evaluation study of the newly designed Carmen implant for ACDF treated cervical spondylosis patients.
Conclusions
When compared to the zero-profile implant, the primary clinical outcomes of the integrated low-profile mini plate implant used in ACDF was satisfactory and was comparable to that of zero-profile system. Besides, this implant may have advantages in improving and maintaining the cervical and segmental lordosis compared to zero-profile system. The new integrated low-profile mini plate (Carmen) system can be a better alternative in single-level cervical spondylosis treated with ACDF.
Acknowledgements
Not applicable
Abbreviations
- ACDF
Anterior cervical discectomy and fusion
- ASD
Adjacent segment degeneration
- Zero-P
Zero-profile
- JOA
Japanese Orthopedic Association score
- VAS
Visual analog scale
- ROM
Range of motion
Authors' contributions
LW and CX drafted the work and the original paper. CX, MD, LW and YD made the substantial contributions to the conception WY, YT, PC and XS provided resource. HQ, HC, XW and XW revised the work and validated the contents. WY, PC and XS designed the work and was the project administration. All authors read and approved the final manuscript.
Funding
This research was supported by Grants from Shanghai Rising-Star Program (20QA1409200), National Natural Science Foundation of China (82172470, 82072471, 81871802, 81902234, 82002335, 81972090), Shanghai "Rising Stars of Medical Talent" Youth Development Program.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethical approval of this study was given by the Naval Medical University ethics committee review board. This research was conducted in regard of the Declaration of Helsinki.
Consent for publication
Written informed consent for publication was obtained from the patient.
Competing interests
The authors declare no conflict of interest concerning the study or the findings specified in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Leixin Wei, Chen Xu, Minjie Dong and Yibo Dou have contributed equally to this work.
Contributor Information
Xiaolong Shen, Email: spine_shen@163.com.
Peng Cao, Email: mdpinocao@163.com.
Wen Yuan, Email: yuanwenspine@smmu.edu.cn.
References
- 1.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-a(3):607–624. doi: 10.2106/00004623-195840030-00009. [DOI] [PubMed] [Google Scholar]
- 2.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 3.Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine. 2009;34(26):2886–2892. doi: 10.1097/BRS.0b013e3181b64f2c. [DOI] [PubMed] [Google Scholar]
- 4.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32(21):2310–2317. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 5.Fisahn C, Schmidt C, Rustagi T, Moisi M, Iwanaga J, Norvell DC, et al. Comparison of chronic dysphagia in standalone versus conventional plate and cage fusion. World Neurosurg. 2018;109:e382–e388. doi: 10.1016/j.wneu.2017.09.188. [DOI] [PubMed] [Google Scholar]
- 6.Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F. A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res. 2011;469(3):666–673. doi: 10.1007/s11999-010-1597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y, Liu Y, Chen H, Cao P, Yuan W. Comparison of curvature between the zero-p spacer and traditional cage and plate after 3-level anterior cervical discectomy and fusion: mid-term results. Clin Spine Surg. 2017;30(8):E1111–E1116. doi: 10.1097/BSD.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 8.Chen Y, Chen H, Cao P, Yuan W. Anterior cervical interbody fusion with the Zero-P spacer: mid-term results of two-level fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2015;24(8):1666–1672. doi: 10.1007/s00586-015-3919-9. [DOI] [PubMed] [Google Scholar]
- 9.Qi M, Chen H, Liu Y, Zhang Y, Liang L, Yuan W. The use of a zero-profile device compared with an anterior plate and cage in the treatment of patients with symptomatic cervical spondylosis: a preliminary clinical investigation. Bone Jt J. 2013;95(4):543–547. doi: 10.1302/0301-620X.95B4.30992. [DOI] [PubMed] [Google Scholar]
- 10.Dong J, Lu M, Lu T, Liang B, Xu J, Zhou J, et al. Meta-analysis comparing zero-profile spacer and anterior plate in anterior cervical fusion. PLoS ONE. 2015;10(6):e0130223. [DOI] [PMC free article] [PubMed]
- 11.Njoku I, Jr, Alimi M, Leng LZ, Shin BJ, James AR, Bhangoo S, et al. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: clinical article. J Neurosurg Spine. 2014;21(4):529–537. doi: 10.3171/2014.6.SPINE12951. [DOI] [PubMed] [Google Scholar]
- 12.Shi S, Liu ZD, Li XF, Qian L, Zhong GB, Chen FJ. Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: a preliminary clinical study. Spine J Off J N Am Spine Soc. 2015;15(9):1973–1980. doi: 10.1016/j.spinee.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 13.Sun B, Shi C, Wu H, Xu Z, Lin W, Shen X, et al. Application of zero-profile spacer in the treatment of three-level cervical spondylotic myelopathy: 5-year follow-up results. Spine (Phila Pa 1976). 2020;45(8):504–11. [DOI] [PubMed]
- 14.Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, et al. Cervical alignment and range of motion after laminoplasty: radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature. Spine. 2012;37(20):E1243–E1250. doi: 10.1097/BRS.0b013e3182659d3e. [DOI] [PubMed] [Google Scholar]
- 15.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003;28(2):134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 16.Li T, Yang JS, Wang XF, Meng CY, Wei JM, Wang YX, et al. Can zero-profile cage maintain the cervical curvature similar to plate-cage construct for single-level anterior cervical diskectomy and fusion? World Neurosurg. 2020;135:e300–e306. doi: 10.1016/j.wneu.2019.11.153. [DOI] [PubMed] [Google Scholar]
- 17.Yang Y, Ma L, Liu H, Xu M. A meta-analysis of the incidence of patient-reported dysphagia after anterior cervical decompression and fusion with the zero-profile implant system. Dysphagia. 2016;31(2):134–145. doi: 10.1007/s00455-015-9681-7. [DOI] [PubMed] [Google Scholar]
- 18.He S, Feng H, Lan Z, Lai J, Sun Z, Wang Y, et al. A randomized trial comparing clinical outcomes between zero-profile and traditional multilevel anterior cervical discectomy and fusion surgery for cervical myelopathy. Spine. 2018;43(5):E259–E266. doi: 10.1097/BRS.0000000000002323. [DOI] [PubMed] [Google Scholar]
- 19.Basu S, Rathinavelu S. A prospective study of clinical and radiological outcomes of zero-profile cage screw implants for single-level anterior cervical discectomy and fusion: is segmental lordosis maintained at 2 years? Asian Spine J. 2017;11(2):264–271. doi: 10.4184/asj.2017.11.2.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang Z, Zhao Y, Luo J. Incidence of dysphagia of zero-profile spacer versus cage-plate after anterior cervical discectomy and fusion: a meta-analysis. Medicine. 2019;98(25):e15767. [DOI] [PMC free article] [PubMed]
- 21.Panchal R, Gandhi A, Ferry C, Farmer S, Hansmann J, Wanebo J. A biomechanical evaluation of a next-generation integrated and modular ACDF device possessing full-plate, half-plate, and no-profile fixation iterations. Glob Spine J. 2019;9(8):826–833. doi: 10.1177/2192568219834252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine. 2002;27(22):2453–2458. doi: 10.1097/00007632-200211150-00007. [DOI] [PubMed] [Google Scholar]
- 23.Xiao S, Liang Z, Wei W, Ning J. Zero-profile anchored cage reduces risk of postoperative dysphagia compared with cage with plate fixation after anterior cervical discectomy and fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cervical Spine Res Soc. 2017;26(4):975–984. doi: 10.1007/s00586-016-4914-5. [DOI] [PubMed] [Google Scholar]
- 24.Lee MJ, Bazaz R, Furey CG, Yoo J. Influence of anterior cervical plate design on Dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech. 2005;18(5):406–409. doi: 10.1097/01.bsd.0000177211.44960.71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.