Abstract
Pediatric burn injuries can alter the trajectory of the survivor’s entire life. Patient-centered outcome measures are helpful to assess unique physical and psychosocial needs and long-term recovery. This study aimed to develop a conceptual framework to measure pediatric burn outcomes in survivors aged 5 to 12 years as a part of the School-Aged Life Impact Burn Recovery Evaluation Computer Adaptive Test (SA-LIBRE5–12 CAT) development. This study conducted a systematic literature review guided by the WHO International Classification of Functioning—Child and Youth and domains in the American Burn Association/Shriners Hospitals for Children Burn Outcomes Questionnaire5–18. Interviews with eight parents and seven clinicians were conducted to identify important domains in child recovery. One clinician focus group with four clinicians was completed to identify gaps in the preliminary framework, and semiweekly expert consensus meetings were conducted with three experts to solidify the framework. Qualitative data were analyzed by grounded theory methodology. Three major thematic outcome domains emerged: 1) Physical Functioning: fine motor and upper extremity, gross motor and lower extremity, pain, skin symptoms, sleep and fatigue, and physical resilience; 2) Psychological Functioning: cognitive, behavioral, emotional, resilience, and body image; and 3) Family and Social Functioning: family relationships, and parental satisfaction, school, peer relations, and community participation. The framework will be used to develop item banks for a CAT-based assessment of school-aged children’s health and developmental outcomes, which will be designed for clinical and research use to optimize interventions, personalize care, and improve long-term health outcomes for burned children.
Children continue to experience a disproportionate burden from burn injuries, with an estimated one third of burn injuries occurring in children younger than age 15.1 Burn injuries can affect the survivor’s entire life, especially when the burn was sustained during childhood.1,2 The health impacts of childhood burns often persist into adolescence or adulthood.3,4 The Centers for Disease Control and Prevention outlines significant social, emotional, and cognitive milestones that occur in this period.4–10 For school-aged children, 5 to 12 years, this period is defined by learning self-care, navigating changes in body image, cognitive development, beginning to form thoughts about the future, developing friendships, and experiencing peer pressure5,6; all of which can be significantly affected by a burn injury.3,8–14 Outcome measurement tools are essential to capture and assess the dynamic needs of this age group, monitor burn recovery, inform interventions, and evaluate healthcare efficacy and effectiveness.
Measures of pediatric outcomes after a burn injury include the Burn Outcomes Questionnaire (BOQ)5–18, for children and adolescents, and the BOQ11–18, for teenagers—both legacy measures and their limitations are discussed in the work of Brady et al.15,16 For example, although the BOQs are widely used among the burn community,15,17 the length of legacy measures may not always be practical for clinical use and the content covered does not address the wide range of formative development in this age group. A more granular instrument may be better suited to assess outcomes over such a dynamic period of growth. Tailored to each respondent in real time based on the level of ability, computer adaptive test (CAT) instruments based on item response theory psychometric models can help address these limitations.
To inform precise item pool selection, accurately measure recovery, and ultimately develop the CAT, there is a need for a specific conceptual framework for school-aged burn survivors. Previously established conceptual models, such as the BOQ5–18 and the World Health Organization’s International Classification for Functioning for Children and Youth (ICF-CY),15,18 provide essential frameworks for the development of a conceptual model for the proposed school-aged CAT. These two frameworks incorporate biological, psychological, and social aspects of a child’s recovery using a dynamic biopsychosocial approach. Both the ICF-CY and the BOQ5–18 are well-known and offer conceptual underpinnings for documenting health in youth, including body functioning, activity limitations, and environmental factors necessary for recovery.15,18 Although the ICF-CY is expansive and comprehensive, it has not yet been selectively applied to burn patients.19
This study aimed to develop a conceptual framework to understand the areas of physical, psychological, family, and social life most important to pediatric burn survivors aged 5 to 12 years as a part of the School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5–12). While a LIBRE framework has been developed for children aged 1 to 5 years,16 and adults aged 18 and older,20 this study aims to fill the gap for school-aged children 5 to 12 years of age. All three of the domains in the framework are based on the BOQ5–18 and the ICF-CY, mostly concentrating on activities and participation, body functions, and environmental factors.15,18 Clinical and research use of the SA-LIBRE5–12 CAT is needed to optimize interventions and personalize care for children with burn injuries. Once developed, this new computer-adaptive survey instrument will be used to measure, via parent proxy, the health-related quality of life outcomes of children with burns over time and to improve the quality of care.
METHODS
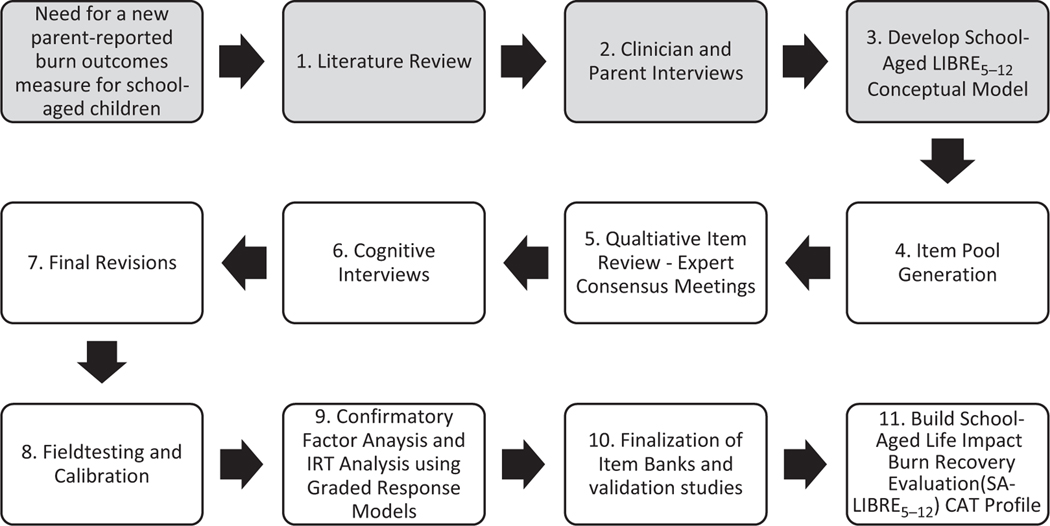
The development of the SA-LIBRE5–12 conceptual framework was grounded in the BOQ5–18 & 11–18 and the World Health Organization’s ICF-CY.15,18 The ICF-CY framework was designed to assess development, health, and disability in children and youth.21 Expanding beyond these frameworks, this study used a comprehensive literature review, individual interviews with parents and clinicians, one clinician focus group, and expert consensus meetings to guide the creation of the conceptual model framework. These methods represent the first three steps in the SA-LIBRE5–12 CAT development (Figure 1). During development, we focused on ensuring the domains both reflect the rapid developmental changes of school-aged children and reliably assess each domain through parent reports.
Figure 1.
Life cycle of the School-Aged LIBRE5–12 CAT (Computer Adaptive Test) development.
Literature Review and Preliminary Framework Development
The first step in developing an initial conceptual model framework was to review the ICF-CY and BOQ5–18.15,18 Second, we conducted a structured literature review using the PubMed/MEDLINE database based on the domains identified in the BOQ5–1815 and the ICF-CY.18 This review was a part of a broader systematic review aimed to identify the literature that exists on burn survivors aged 5 to 18 years. The search focused on identifying instruments that assess health and development outcomes in children aged 5 to 12. Third, to refine the initial framework grounded in the ICF-CY18 and BOQ5–18,15 a manual check was performed for conceptual frameworks based on references found in the identified articles (ie, Pediatric Symptom Checklist), well-known validated assessments and pediatric checklists (ie, Neuro-Quality of Life Item Bank), and other assessments suggested by content experts (ie, Social Emotional Assets and Resilience Scale). We excluded articles from our analysis if they were not accessible, not in English, or were not relevant to children aged 5 to 12 years with burn injuries. We reviewed each article for the content domains and assessed each during framework development. Based on the results of this process, we developed an initial conceptual framework.
Conceptual Model Refinement
This study conducted individual semistructured interviews with caregivers of burn survivors and clinicians, a clinician focus group, and expert consensus meetings to refine the preliminary conceptual model and fill any gaps in each of the domain contents.
Parent and Clinician Interviews.
The full research team created the interview guides for both the parent and clinician interviews with the goal of identifying outcomes most relevant when assessing burn recovery in this age group. Interviewees were asked to identify areas of life most difficult for burn survivors to return to, as well as how the burn injury directly or indirectly affected the typical health and/or development of the child. Further probing aimed to describe examples of that content. Interviewees were also asked about each domain from the literature review as well as which areas were missing from the framework. Clinicians were asked how best to frame questions that get at sensitive yet critically important topics such as bullying, anxiety, and aggression.
Interviews were conducted in English by one research assistant along with a note-taker and lasted between 45 and 90 minutes. Informed consent was obtained prior to the interview, and all interviewees were given a chance to ask questions about the research. The final sample size was based on thematic saturation determined by concurrent coding and data collection. Saturation was defined as recurring common themes coming up over and over. All participants were older than age 18, fluent in English, and were excluded if unable to give informed consent. Participants were reimbursed for their time and transportation.
Content expert clinicians were recruited through convenience sampling between January and March 2020. Clinician inclusion criteria were prior and current experience working with pediatric burn survivors. Parents were recruited with purposive sampling, either by phone or in person at the outpatient clinic. Beginning in March 2020, study procedures were compliant with COVID-19 pandemic safety protocols and restrictions. Parent inclusion criteria were being the guardian of a child aged 5 to 12 years who had experienced a burn injury.
Data Analysis
Qualitative Data Analysis.
All interviews were audiotaped and transcribed verbatim. After transcription, all identifiable information was removed. Four team members established a final codebook using grounded theory methodology and an iterative process of revision.21–24 Grounded theory methodology used a constant comparative analysis process moving in and out of data collection and analysis.25–27 Transcript analysis and management were conducted using NVivo12 software (QSR International Pty Ltd., Version 12, 2018).28 Two team members coded each transcript. Areas of disagreement were discussed among the dyad for reconciliation. Four research team members applied the coding schema to the data, following a structured, hierarchical coding process. Expert consensus meetings with pediatric burn clinicians and those who are experts in child and adolescent development made final analytical decisions, including thematic analysis, data interpretation, and selection of final constructs for the conceptual framework.
Quantitative Descriptive Data Analysis.
All descriptive statistics are presented using the median and interquartile range, and frequencies and proportions for continuous and categorical variables, respectively.
Ethical Approval
The Western Institutional Review Board approved this study (BOS1911 and BOS1912) for the Shriners Hospitals.
RESULTS
Literature Review
Our results showed that the outcome areas for pediatric patients with burn injuries aged 5 to 12 years most often described as impacted include physical functioning, psychological functioning, and family and social functioning. Based on 128 assessments identified in our literature review, 82 (64%) patient-reported outcome assessments, including proxy- and self-reported, met our inclusion criteria. Of those, 24 (29%)15,29–47 included items covering physical outcomes, 25 (30%)15,30,33–35,37,41,45–55 family and social outcomes, and 49 (60%)15,29,30,32,33,35–37,39,47–49,53,55–71 psychological outcomes, with a number of instruments covering more than one domain.
Expert Consensus Meetings
The conceptual framework was developed iteratively in tandem with parent and clinician interviews and expert consensus meetings. Three experts, including a burn surgeon, pediatric psychiatrist, and health services researcher with experience in psychometrics, and all four research coordinators met semiweekly for 6 months to solidify the conceptual model framework based on a prior knowledge, literature review results, and results of the parent and clinician interviews. The framework was then presented to a larger team including three additional content experts. We paid special attention to identifying domains and content that can adequately capture the dynamic developmental nature of children’s health during the 5 to 12 age range and can be reliably assessed through parent-reports. Special consideration for each domain was also given to ensure culture and gender sensitivity. Each domain and focus within a domain were individually reviewed by two research assistants to mitigate any cultural, socioeconomic, or gender bias.
Interviews
This study interviewed 19 stakeholders including 8 parents and 11 clinicians. The eight parents, seven females and one male, participated in individual semistructured interviews (Table 1). Their children, four males and four females, had an average age of 9.2 years. All eight children had a burn to a critical area (face, hand, genitals, or hand), and a majority had a TBSA under 20% (62.5%; Table 2). Seven clinicians participated in individual interviews and four participated in one focus group. A majority were female (n = 10), with a median age of 48 years and a median time of 13 years of experience in burn care (Table 3). Clinicians included surgeons, an elementary school teacher, child life specialists, occupational therapists, physical therapists, social workers, burn nurses, pediatricians, and burn professionals associated with burn camps. Select quotations from these interviews are presented in Supplementary Appendix 2.
Table 1.
Caregiver demographics table (n = 8)
| Median (IQR) or Frequency (%) | |
|---|---|
|
| |
| Age, years | 46.5 (42.8–50.0) |
| Sex | |
| Female | 7 (87.5%) |
| Male | 1 (12.5%) |
| Number of children at home | 2.5 (2–3) |
| Education level | |
| High school degree | 1 (12.5%) |
| Associate’s degree | 1 (12.5%) |
| Bachelor’s degree | 2 (25.0%) |
| Master’s degree | 4 (50.0%) |
| Partner at home | |
| Yes | 6 (75.0%) |
| No | 2 (25.0%) |
| Race | |
| White | 5 (62.5%) |
| Hispanic | 1 (12.5%) |
| White, Hispanic | 1 (12.5%) |
| Other | 1 (12.5%) |
IQR, interquartile range.
Table 2.
Child demographics table (n = 8)
| Median (IQR) or Frequency (%) | |
|---|---|
|
| |
| Age, years | 9.2 (7.2–10.0) |
| Sex | |
| Female | 4 (50.0%) |
| Male | 4 (50.0%) |
| Time since burn, years | 1.1 (0.3–7.4) |
| TBSA | |
| <20% | 5 (62.5%) |
| ≥20% | 3 (37.5%) |
| Burn to critical area | |
| Yes | 8 (100.0%) |
| No | 0 (0.0%) |
| Burn location* | |
| Hand | 6 |
| Feet | 2 |
| Genitals | 1 |
| Face | 4 |
Number does not equal sample size as some children had burns to multiple locations.
Table 3.
Clinician demographics table (n = 11)
| Clinicians | Median (IQR) or Frequency (%) |
|---|---|
|
| |
| Job titles* | Burn surgeon (acute/ reconstructive) Child life specialist Occupational therapist Pediatrician Physical therapist Psychologist Registered nurse Social worker Elementary school teacher |
| Sex | |
| Male | 1 (9.1%) |
| Female | 10 (90.9%) |
| Age, years | 48 (43–52) |
| Race | |
| White | 9 (81.2%) |
| Other | 1 (9.1%) |
| Missing | 1 (9.1%) |
| Years of burn care experience | 13 (5.5–25) |
Number does not equal sample size as some clinicians have the same job title.
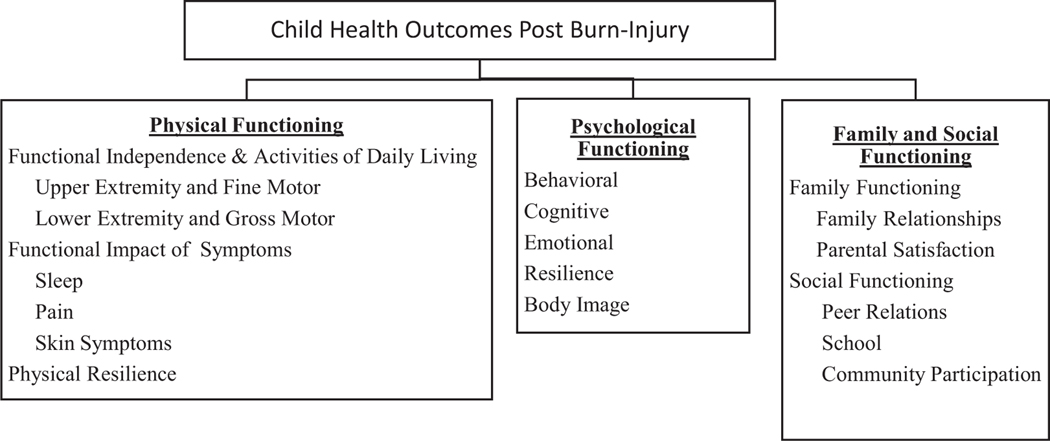
Resulting Conceptual Framework
The ICF-CY18 and the American Burn Association/Shriners Hospitals for Children BOQ5–1815 were chosen as the guiding construct for the conceptual model framework (Table 1; Figure 2; Supplementary Appendix 1).
Figure 2.
School-aged LIBRE5–12 conceptual framework. LIBRE, Life Impact Burn Recovery Evaluation.
Physical Functioning
The physical functioning domain encompasses the following subdomains: 1) the functional independence and activities of daily living, 2) functional impact of physical symptoms, and 3) physical resilience.
Functional Independence and Activities of Daily Living.
This subdomain is further divided into two subdomain foci: 1) upper extremity and fine motor and 2) lower extremity and gross motor. Based on the ICF-CY, the upper extremity and fine motor subdomain focus includes upper body mobility (eg, lifting and carrying objects, fine hand use, hand and arm use) and self-care (eg, dressing, eating, and drinking). During interviews, parents confirmed the difficulties their children had with fine motor skills (Supplementary Appendix 1). Clinicians provided insight into the ways they approach this topic. “Most of our development assessments at this point are task based. Can you cut on a line? Can you draw a circle? Can you tie your shoes? Can you string a bead? We’re looking at pinch-grasp fine motor, manipulation in context of an activity.”
Based on the ICF-CY, lower extremity and gross motor subdomain focus includes gross motor functions (eg, changing basic body positions, maintaining body positions, transferring oneself, walking, and moving around), self-care (eg, washing oneself and toileting), as well as exercise tolerance functions. As noted in the interviews, children may face adversities in a number of areas. One parent noted that because of the burn, their child “can’t move, she can’t use the bathroom like everybody else.”
Functional Impact of Symptoms.
This subdomain is defined as the physical discomfort and impairments children might experience as a result of the burn injury. This subdomain encompasses the 1) sleep and fatigue, 2) pain, and 3) skin symptoms subdomain foci. This domain is represented in the physical health of the BOQ5–18 and the ICF-CY body functions and activities and participation domains15,18 (Table 1; Supplementary Appendix 1). The pain subdomain focus is defined in accordance with the ICF-CY by generalized pain, pain in a body part, and pain in multiple body parts. The sleep and fatigue subdomain focus is defined in accordance with the ICF-CY by the amount, onset, and maintenance of sleep, as well as energy and drive functions, continuity of consciousness, and exercise tolerance functions. The skin symptoms subdomain focus is defined in accordance with the ICF-CY by sensitivity to temperature and pressure as well as sensations related to the skin (eg, itching, burning sensation, and tingling).
Physical Resilience.
The physical resilience subdomain focus is defined as the resilience and stamina children exhibit when confronting physical challenges postburn injury.
Psychological Functioning
The psychological functioning domain includes the following subdomains: 1) behavioral, 2) cognitive, 3) emotional, 4) resiliency, and 5) body image.
Behavioral.
The behavioral subdomain focuses on personality functions (eg, agreeableness and temperament), self-care (eg, looking after one’s mental health), and interpersonal relationships (eg, appropriately relating to peers and figures of authority). Additionally, the domain is defined by externalizing behaviors such as those related to aggression, conduct, and withdrawal. Clinician experts described the types of questions they ask to understand pediatric behavioral changes, including “is your child throwing temper tantrums? Are they angry a lot of the time? Are they much quieter than they were before they were injured?”
Cognitive.
In accordance with the ICF-CY, the cognitive subdomain is primarily focused on mental functions (eg, consciousness and intellectual functions) and being able to learn and apply knowledge (eg, focusing attention, thinking, reading, writing, and decision making) (Supplementary Appendix 1). For children with larger burns, clinicians and parents discussed the difficulties some children face in returning to a preburn cognitive ability. One parent commented that, “He has disabilities that stem from his injury that make it cognitively difficult for him. He is behind in school” (Supplementary Appendix 2).
Emotional.
The emotional subdomain covers topics including emotional functioning (eg, appropriateness of emotions), and temperament and personality regulation (eg, range and regulation of emotion). The qualitative results highlighted the range of emotions children experience postburn, including anger, separation anxiety, and fear. For example, one clinician reported that “anger is prominent in this age group.”
Resilience.
The resilience subdomain focuses primarily on the child’s ability to cope, adapt to new circumstances, and community integration after the burn injury. Although this domain is not clearly defined in the BOQ5–18 or the ICF-CY, the core foundation of the domain’s content aligns with a number of topics covered in the aforementioned frameworks.15,18 The ICF-CY describes the importance of the ability to handle stress and care for oneself amid trauma. During interviews, clinicians highlighted the importance of capturing resiliency in this population. One noted that “resiliency—if there is a way to assess this it would be so important. This separates those that do well and those that do not.” According to one clinician, some children “have a sense of like pride, almost badge of honor.”
Body Image.
The body image subdomain is primarily an expansion on the BOQ5–18’s appearance domain, integrating aspects of the ICY-CY experience of self-functions. Qualitative results highlighted the role body image plays in this age group in particular. One parent reflected on her child’s comments, saying that his friends “take a really immature response to feeling and call him a name … it is heart breaking. He will say things, like, for his birthday, he probably won’t have a party because ‘well no one is going to want to come to party mom’ and he pointed to his face.”
Family and Social Functioning
The family and social functioning domain is defined by children’s observable interest and ability to connect with others, while also addressing the indirect negative or positive effects of the child’s burn injury on the daily activities of the individual’s family and family cohesiveness. This domain is further broken down into two subdomains followed by specific foci. The two subdomains are 1) family functioning and 2) social functioning. The family functioning subdomain contains both 1) family relationships and 2) parental satisfaction to address ways in which a burn injury affects the child’s family, specifically their immediate caregivers. The social functioning subdomain foci are 1) peer relations, 2) school, and 3) community participation as these various categories each contribute significantly to the child’s overall social integration postburn injury. The conceptualization for both of these subdomains was widely influenced by the ICF-CY and the BOQ5–18 (Table 1; Supplementary Appendix 1).15,18
Family Functioning.
The impact of a child’s burn injury is not limited to the child’s personal experiences but extends to the family unit, indicated by the family relationships subdomain focus. One clinician stressed the importance of family during the recovery process, “Family is everything. Family is so important.” This subdomain focus addressed a family’s ability to carry on a routine daily functioning postburn injury. Physical and emotional support is a critically important environmental factor to analyze when evaluating a child’s burn injury recovery (eg, immediate family, extended family, neighbors, acquaintances, and community members).
The parental satisfaction subdomain focus describes attitudes of caregivers toward their child’s burn injury recovery, which can affect a child’s ability to recover. Children often regress following trauma, and during an interview, a clinician said that, “The ability to make up that regression is very much dependent on how the parent or caregiver responds to the regression.” According to the ICF-CY, this identifies general or specific opinions from caregivers that may greatly influence the child’s behavior and actions.
Social Functioning.
The peer relations subdomain focus within the social functioning subdomain reflects a child’s ability to relate with strangers and create formal and informal relationships with friends, teachers, classmates, and fellow service providers. The guiding principle is mental functioning, allowing each child to exemplify temperament and personality functions with the aim of identifying oneself as unique through the establishment of a set of personality traits.
The school subdomain focus describes an ICF-CY-defined major life area for school-aged children. Engaging in education is a key requirement for school-aged children postburn injury. This domain covers topics including learning course material, attending classes, and working cooperatively with peers and teachers. School can be a difficult experience to navigate for burn survivors, as one clinician pointed out, “Sometimes you think it’s only the ones with the severe burn and disfigurements. It could be a tiny little scar and they are still made fun of for that.”
The community participation subdomain focus encompasses various activities required in organized social life outside of family, friends, and school. Particularly important to school-aged children, participation in recreation and leisure is described here (eg, games, sports, arts, hobbies, and socializing). Engaging in religious organizations may be applicable for children within their specific community (eg, attending church, temple, mosque or synagogue, and spiritual contemplation).
DISCUSSION
This study aimed to develop a conceptual model framework grounded in the ICF-CY18 to understand which aspects of physical, psychological, family, and social life are most important to assess recovery in school-aged burn survivors aged 5 to 12 years. We used qualitative methods and a literature review to identify the most important outcomes for this age group. The conceptual framework is comprised of three major domains and their respective subdomains: 1) physical functioning: upper extremity and fine motor, lower extremity and gross motor, sleep, pain, skin symptoms and fatigue, and physical resilience; 2) psychological functioning: behavioral, cognitive, emotional, resilience, and body image; 3) family and social functioning: family relationships, parental satisfaction, peer relations, school, and community participation. This conceptual model will function as a foundation for developing an item pool to build a CAT assessing children’s physical and psychosocial recovery from burns, as well as the impact of family relationships on their healing process.
Traditional legacy measures require a large number of items to be administered to the participant. Legacy measures, such as the BOQ5–18,15 although specific to burn injuries, lack granularity in domains critical to recovery for school-aged children, including body structure, peer relations, and environmental factors.72 Our conceptual framework is a synthesis of existing frameworks explicitly tailored for parents of school-aged burn survivors. In addition to expanding on the content in extant frameworks, integrating coproduction that combined the synergies of clinicians and parents of burn survivors73,74 was a critical component of the development process to meet the target population’s needs. Consequently, the SA-LIBRE5–12 CAT will provide a thorough and more customized and personalized burn outcome assessment for school-aged children.
While our framework is rooted in the ICF-CY18 and the BOQ5–18,15 it differs in several respects. First is the addition of resiliency and physical resiliency subdomains. Resiliency emerged as a significant theme during discussions with parents and clinicians, and our expert consultants corroborated its relevance. As such, two novel subdomains emerged. Conceptualization of the subdomains relates to several areas within the ICF-CY, such as the global mental functions (ie, dispositions and intrapersonal functions and adaptability) and general tasks and demands (ie, handling stress and other psychological needs). Second is the formation of a cognitive subdomain. Parents of children with severe burns spoke about the noticeable changes in their child’s cognitive functioning related to social interactions and the ability to complete schoolwork. We created the subdomain based on the ICF-CY mental functions (ie, consciousness functions and intellectual functions) and learning and applying knowledge (ie, learning to read, learning to write, and acquiring skills). Last, our family domain was created by synthesizing relevant areas of the BOQ5–1815 (family disruption and parental concern) and the ICF-CY18 (support and relationships and interpersonal relationships—family). While existing frameworks do not account for parents’ relationships, parents often discussed the strain that their child’s burn injury placed on their relationship with their partner and the indirect impact this had on their child’s healing process. To address this vital aspect of a child’s environmental influence on their recovery, we included parent-to-parent relationships within the parental satisfaction subdomain focus.
Another notable study finding is the expansion of existing domains from the BOQ5–18.15 For example, we expanded on the BOQ5–1815 school reentry domain by distinguishing the underlying principles into three subdomain foci: school, peer relations, and community participation. Social relationships, both in and out of school, emerged as a significant theme in clinician and parent interviews. The peer relations subdomain focus includes concepts from the ICF-CY18 body functions (ie, personality functions), activities and participation (ie, interpersonal interactions), and environmental factors (ie, support and relationships). Community participation was included to assess engagement in activities prominent in school-aged children’s life, such as sports and spiritual events, tying into the ICF-CY18 domain on community, social, and civic life.
While the ICF-CY18 and the BOQ5–1815 were our primary guiding frameworks, our results also include several similarities to the Preschool1–5 LIBRE framework.16 First, in line with the Preschool1–5 LIBRE framework,16 we did not have a domain specific to satisfaction with the current state. Our framework is primarily concerned with pediatric health outcomes rather than the process of care outcomes. Second, self-care is not a designated subdomain but rather incorporated within physical functioning. While the ICF-CY18 includes a self-care subdomain (ie, washing oneself and toileting), we conceptualized children’s ability to perform self-care activities as indicators of their physical abilities and thus included these topics within the physical functioning domain. Third, our qualitative results corroborated those of the Preschool1–5 LIBRE framework16 study and found body image to be a significant aspect of school-aged children’s mental health. We created the body image subdomain in response to both parents’ and clinicians’ remarks of changed appearance resulting from the burn affecting children’s health. We based it on the BOQ5–18 appearance domain and the ICF-CY’s specific mental functions (experience of self and time functions; body image).15,18
While the School-Aged5–12 and Preschool1–5 LIBRE frameworks16 share many similarities, our results produced one key distinction. Despite communication and language functioning appearing as a subdomain within the Preschool1–5 LIBRE conceptual model,16 communication skills did not emerge as a concept requiring an individual domain but rather one incorporated into a number of different areas in the school-aged child’s life. Consequently, this domain is distributed throughout the SA-LIBRE5–12 framework into subdomains such as family and peer relations to assess communication functioning within these specific contexts.
Our study has several limitations. First, our findings may have limited generalizability due to recall and selection bias among the parents. We attempted to mitigate these biases by asking about the burn’s impact on specific areas of their child’s health and development. Additionally, the majority of the parents were female and white. Although we aimed to recruit a diverse population, parent demographics may limit the generalizability of our data. Second, although we included 128 instruments, some instruments, such as those not published in English, may have been missed in the literature review. Lastly, the aim of this study was to create the initial conceptual model, and as such, future work quantitative work is warranted to confirm this model empirically. Despite these limitations, this study develops a comprehensive conceptual model encompassing significant areas in the lives of children that are affected by a burn injury.
CONCLUSIONS
Through a comprehensive literature review, clinician and parent interviews, and expert consensus meetings, this article presents the development of a conceptual framework for a parent-reported health outcome metric after a burn injury in school-aged children aged 5 to 12 years. The three major framework domains were 1) physical functioning, 2) psychological functioning, and 3) family and social functioning. This framework will help develop a comprehensive assessment tool for this age group by guiding both the item pool selection for the SA-LIBRE5–12 and ultimately the CAT. In addition, the conceptual framework can help inform effective rehabilitation or intervention strategies aimed at improving biopsychosocial outcomes for burn survivors in this age group. The goal of this work is to ensure the care provided to children with burn injuries is tailored to individual targeted needs throughout the recovery process to improve long-term health outcomes.
Supplementary Material
Acknowledgments
Funding: This study was funded by Shriners Hospitals for Children (79145-BOS-20) and the National Institute on Disability, Independent Living, and Rehabilitation Research (90DPBU0001).
Footnotes
SUPPLEMENTARY DATA
Supplementary data are available at Journal of Burn Care & Research online.
Conflict of interest statement. The authors have no conflicts of interest to declare.
REFERENCES
- 1.American Burn Association. National burn awareness week fact sheet. Published February 2017; accessed 4 May 2020; available from http://ameriburn.org/wp-content/uploads/2017/04/nbaw-fact-sheet-rev.pdf
- 2.World Health Organization. Burns. Published 6 March 2018; accessed 4 May 2020; available from https://www.who.int/news-room/fact-sheets/detail/burns
- 3.Duke JM, Boyd JH, Randall SM, Rea S, Wood FM. Childhood burn injury-impacts beyond discharge. Transl Pediatr 2015;4:249–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Disseldorp LM, Niemeijer AS, Van Baar ME, Reinders-Messelink HA, Mouton LJ, Nieuwenhuis MK. How disabling are pediatric burns? Functional independence in Dutch pediatric patients with burns. Res Dev Disabil 2013;34:29–39. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Middle childhood (6–8 years old). Published 6 March 2020; accessed 4 May 2020; available from https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html
- 6.Centers for Disease Control and Prevention. Middle childhood (9–11 years old). Published 6 March 2020; accessed 4 May 2020; available from https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle2.html
- 7.Hubbuck C. Treatment of children with severe burns. Lancet 2003;362:s44–5. [DOI] [PubMed] [Google Scholar]
- 8.van Baar ME, Polinder S, Essink-Bot ML et al. Quality of life after burns in childhood (5–15 years): children experience substantial problems. Burns 2011;37:930–8. [DOI] [PubMed] [Google Scholar]
- 9.Rivlin E, Faragher EB. The psychological sequelae of thermal injury on children and adolescents: Part 1. Dev Neurorehabil 2007;10:161–72. [DOI] [PubMed] [Google Scholar]
- 10.McGarry S, Elliott C, McDonald A, Valentine J, Wood F, Girdler S. Paediatric burns: from the voice of the child. Burns 2014;40:606–15. [DOI] [PubMed] [Google Scholar]
- 11.De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am 2014;23:185–222, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rimmer RB, Foster KN, Bay CR et al. The reported effects of bullying on burn-surviving children. J Burn Care Res 2007;28:484–9. [DOI] [PubMed] [Google Scholar]
- 13.Landolt MA, Buehlmann C, Maag T, Schiestl C. Brief report: quality of life is impaired in pediatric burn survivors with posttraumatic stress disorder. J Pediatr Psychol 2009;34:14–21. [DOI] [PubMed] [Google Scholar]
- 14.Kazis LE, Lee AF, Hinson M et al. ; Multi-Center Benchmarking Study Working Group. Methods for assessment of health outcomes in children with burn injury: the Multi-Center Benchmarking Study. J Trauma Acute Care Surg 2012;73:S179–88. [DOI] [PubMed] [Google Scholar]
- 15.Daltroy LH, Liang MH, Phillips CB et al. American Burn Association/Shriners Hospitals for Children burn outcomes questionnaire: construction and psychometric properties. J Burn Care Rehabil 2000;21:29–39. [DOI] [PubMed] [Google Scholar]
- 16.Brady KJS, Grant GG, Stoddard FJ et al. Measuring the impact of burn injury on the parent-reported health outcomes of children 1 to 5 years: a conceptual framework for development of the preschool life impact burn recovery evaluation profile cat. J Burn Care Res. 2020;41:84–9. doi: 10.1093/jbcr/irz110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Baar ME, Essink-Bot ML, Oen IM et al. Reliability and validity of the Dutch version of the American Burn Association/Shriners Hospital for Children Burn Outcomes Questionnaire (5–18 years of age). J Burn Care Res 2006;27:790–802. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. 2007. International classification of functioning, disability and health: children and youth version: ICF-CY. World Health Organization. https://apps.who.int/iris/handle/10665/43737. [Google Scholar]
- 19.Wasiak J, McMahon M, Danilla S, Spinks A, Cleland H, Gabbe B. Measuring common outcome measures and their concepts using the International Classification of Functioning, Disability and Health (ICF) in adults with burn injury: a systematic review. Burns 2011;37:913–24. [DOI] [PubMed] [Google Scholar]
- 20.Marino M, Soley-Bori M, Jette AM et al. Development of a conceptual framework to measure the social impact of burns. J Burn Care Res 2016;37:e569–78. [DOI] [PubMed] [Google Scholar]
- 21.Babbie ER. The basics of social research. 7th ed. Belmont, CA: Cengage; 2017. [Google Scholar]
- 22.Tolley EE, Ulin PR, Mack N, Robinson ET, Succop SM. Qualitative methods in public health: a field guide for applied research. 2nd ed. San Francisco (CA): Wiley; 2016. [Google Scholar]
- 23.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res 2009;18:1263–78. [DOI] [PubMed] [Google Scholar]
- 25.Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol 1990;13:3–21. [Google Scholar]
- 26.Charmaz K. Constructionism and the grounded theory method. In: Holstein JA, Gubrium JF, editors. Handbook of constructionist research. New York: The Guilford Press; 2008. p. 397–412. [Google Scholar]
- 27.Ghezeljeh TN, Emami A. Grounded theory: methodology and philosophical perspective. Nurse Res 2009;17:15–23. [PubMed] [Google Scholar]
- 28.QSR International. Qualitative data analysis software | NVivo. Accessed 24 April 2020; available from https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 29.Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Can J Public Heal. 2013;104:e131–e135. doi: 10.1007/bf03405676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Achenbach T. Manual for the ASEBA school-age forms & profiles an integrated system of multi-informant assessment. Res Cent Child. Published online 2007. [Google Scholar]
- 31.Saxe G, Chawla N, Stoddard F et al. Child stress disorders checklist: a measure of ASD and PTSD in children. J Am Acad Child Adolesc Psychiatry 2003;42:972–8. [DOI] [PubMed] [Google Scholar]
- 32.March JS, Amaya-Jackson L, Terry R, Costanzo P. Posttraumatic symptomatology in children and adolescents after an industrial fire. J Am Acad Child Adolesc Psychiatry 1997;36:1080–8. [DOI] [PubMed] [Google Scholar]
- 33.Lai JS, Nowinski C, Victorson D et al. Quality-of-life measures in children with neurological conditions: pediatric Neuro-QOL. Neurorehabil Neural Repair 2012;26:36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paz SH, Slotkin J, McKean-Cowdin R et al. Development of a vision-targeted health-related quality of life item measure. Qual Life Res 2013;22:2477–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gershon RC, Wagster MV, Hendrie HC, Fox NA, Cook KF, Nowinski CJ. NIH toolbox for assessment of neurological and behavioral function. Neurology 2013;80:S2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the pediatric quality of life InventoryTM version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 37.Jellinek MS, Murphy JM, Robinson J, Feins A, Lamb S, Fenton T. Pediatric symptom checklist: screening school-age children for psychosocial dysfunction. J Pediatr. 1988;112:201–9. doi: 10.1016/S0022-3476(88)80056-8 [DOI] [PubMed] [Google Scholar]
- 38.Revicki DA, Chen WH, Harnam N et al. Development and psychometric analysis of the PROMIS pain behavior item bank. Pain 2009;146:158–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bevans KB, Gardner W, Pajer KA et al. Psychometric evaluation of the PROMIS® pediatric psychological and physical stress experiences measures. J Pediatr Psychol 2018;43:678–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tucker CA, Bevans KB, Teneralli RE, Smith AW, Bowles HR, Forrest CB. Self-reported pediatric measures of physical activity, sedentary behavior, and strength impact for PROMIS: item development. Pediatr Phys Ther 2014;26:385–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lai JS, Stucky BD, Thissen D et al. Development and psychometric properties of the PROMIS® pediatric fatigue item banks. Qual Life Res. 2013;22:2417–27. doi: 10.1007/s11136-013-0357-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kratz AL, Slavin MD, Mulcahey MJ, Jette AM, Tulsky DS, Haley SM. An examination of the PROMIS(®) pediatric instruments to assess mobility in children with cerebral palsy. Qual Life Res 2013;22:2865–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Varni JW, Stucky BD, Thissen D et al. PROMIS Pediatric Pain Interference Scale: an item response theory analysis of the pediatric pain item bank. J Pain 2010;11:1109–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hung M, Voss MW, Bounsanga J, Crum AB, Tyser AR. Examination of the PROMIS upper extremity item bank. J Hand Ther. 2017;30(4):485–90. doi: 10.1016/j.jht.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Forrest CB, Meltzer LJ, Marcus CL et al. Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep. 2018;41. doi: 10.1093/sleep/zsy054 [DOI] [PubMed] [Google Scholar]
- 46.Stewart AL, Hays RD, Ware JE Jr. The MOS short-form general health survey. Reliability and validity in a patient population. Med Care 1988;26:724–35. [DOI] [PubMed] [Google Scholar]
- 47.Pepperdine CR, McCrimmon AW. Test Review: Sparrow SS, Cicchetti DV, & Saulnier CA (2016), “Vineland Adaptive Behavior Scales, Third Edition” (“Vineland-3”). San Antonio, TX: Pearson. Can J Sch Psychol. Published online 2018. doi: 10.1177/0829573517733845 [DOI] [Google Scholar]
- 48.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social support: theory, research and applications. NATO ASI Series (D: Behavioural and Social Sciences). vol 24. Dordrecht: Springer; 1985. doi: 10.1007/978-94-009-5115-0_5 [DOI] [Google Scholar]
- 49.Salsman JM, Butt Z, Pilkonis PA, et al. Emotion assessment using the NIH Toolbox. Neurology 2013;80:S76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abidin RR. Parenting stress index. 3rd ed. Odessa, FL: Professional Manual; 1995. [Google Scholar]
- 51.Rigby K, Slee PT. Dimensions of interpersonal relation among Australian children and implications for psychological well-being. J Soc Psychol 1993;133:33–42. [DOI] [PubMed] [Google Scholar]
- 52.Bevans KB, Riley AW, Landgraf JM et al. Children’s family experiences: development of the PROMIS® pediatric family relationships measures. Qual Life Res 2017;26:3011–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Irwin DE, Stucky B, Langer MM et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res 2010;19:595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dewalt DA, Thissen D, Stucky BD et al. PROMIS Pediatric Peer Relationships Scale: development of a peer relationships item bank as part of social health measurement. Health Psychol 2013;32:1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morales LS, Edwards TC, Flores Y, Barr L, Patrick DL. Measurement properties of a multicultural weight-specific quality-of-life instrument for children and adolescents. Qual Life Res 2011;20:215–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mendelson BK, Mendelson MJ, White DR. Body-esteem scale for adolescents and adults. J Pers Assess 2001;76:90–106. [DOI] [PubMed] [Google Scholar]
- 57.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595–605. [PubMed] [Google Scholar]
- 58.Langley AK, Bergman RL, McCracken J, Piacentini JC. Impairment in childhood anxiety disorders: preliminary examination of the child anxiety impact scale-parent version. J Child Adolesc Psychopharmacol 2004;14:105–14. [DOI] [PubMed] [Google Scholar]
- 59.Bosquet Enlow M, Kassam-Adams N, Saxe G. The Child Stress Disorders Checklist-Short Form: a four-item scale of traumatic stress symptoms in children. Gen Hosp Psychiatry 2010;32:321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de la Vega R, Racine M, Sánchez-Rodríguez E et al. Psychometric properties of the short form of the Children’s Depression Inventory (CDI-S) in young people with physical disabilities. J Psychosom Res. 2016;90:57–61. doi: 10.1016/j.jpsychores.2016.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Putnam SP, Rothbart MK. Development of short and very short forms of the Children’s Behavior Questionnaire. J Pers Assess 2006;87:102–12. [DOI] [PubMed] [Google Scholar]
- 62.Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire: psychometric features and prospective relationships with depression and anxiety in adults. Eur J Psychol Assess. 2007;20:135–9. doi: 10.1027/1015-5759.23.3.141 [DOI] [Google Scholar]
- 63.Goleman D, Boyatzis R. Social intelligence and the biology of leadership. Harv Bus Rev 2008;86:74–81, 136. [PubMed] [Google Scholar]
- 64.Motlagh H. Impact of event scale-revised. J Physiother. 2010;56:203. doi: 10.1016/S1836-9553(10)70029-1 [DOI] [PubMed] [Google Scholar]
- 65.Forrest CB, Ravens-Sieberer U, Devine J et al. Development and evaluation of the PROMIS® pediatric positive affect item bank, child-report and parent-proxy editions. J Happiness Stud 2018;19:699–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Forrest CB, Bevans KB, Pratiwadi R et al. Development of the PROMIS ® pediatric global health (PGH-7) measure. Qual Life Res 2014;23:1221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at annual meeting of the Int Soc Trauma Stress Stud, San Antonio, TX, October 1993. Published online 1993. [Google Scholar]
- 68.Lawrence JW, Heinberg LJ, Roca R, Munster A, Spence R, Fauerbach JA. Development and validation of the satisfaction with appearance assessing body image among burn-injured patients. Psychol Assess. 1998;10:64–70. doi: 10.1037/1040-3590.10.1.64 [DOI] [Google Scholar]
- 69.Endrulat NR, Tom K, & Merrell KW (2009, August). Strength-based assessment: Applications and development of the Social-Emotional Assets and Resilience Scales, parent version. Presented at the meeting of the American Psychological Association, Toronto, Canada. [Google Scholar]
- 70.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6. [DOI] [PubMed] [Google Scholar]
- 71.Goodman WK, Price LH, Rasmussen SA et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006–11. [DOI] [PubMed] [Google Scholar]
- 72.Osborne CL, Petersson C, Graham JE et al. The multicenter benchmarking study of burn injury: a content analysis of the outcome measures using the international classification of functioning, disability and health. Burns. 2016;42:1396–1403. doi: 10.1016/j.burns.2016.07.023 [DOI] [PubMed] [Google Scholar]
- 73.Batalden M, Batalden P, Margolis P et al. Coproduction of healthcare service. BMJ Qual Saf 2016;25:509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hickey G. The potential for coproduction to add value to research. Heal Expect 2018;21:693–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.