Abstract
Introduction
Studies have shown that rumination plays a significant mediating role between dispositional mindfulness (DM) and psychopathological symptoms in both clinical and non-clinical populations. However, no studies have examined this pathway in people with schizophrenia spectrum disorders (SSDs).
Methods
A cross-sectional, clinician-administered survey was conducted among people with SSDs (n = 52) in a community setting. Participants completed the Chinese versions of the Depression Anxiety Stress Scale, Five Facet Mindfulness Questionnaire-Short Form, Psychotic Symptom Rating Scale and Scale for the Assessment of Negative Symptoms. Structural equation modelling was performed to examine the pathways of mindfulness facets, rumination, negative emotions and psychotic symptoms.
Results
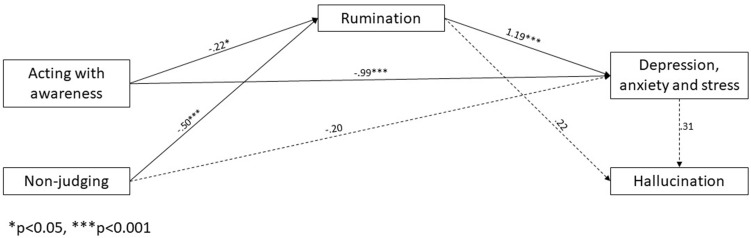
Two facets of mindfulness (nonjudging and acting with awareness) reduced rumination and negative emotional status. Rumination fully mediated the relationship between nonjudging and negative emotions and partially mediated the relationship between acting with awareness and negative emotions. Furthermore, rumination and negative emotions sequentially mediated the relationship between acting with awareness and hallucination (B = −0.44, 95% confidence interval [CI] = −0.338 to −0.045, p = 0.01) and between nonjudging and hallucination (B = −0.356, 95% CI = −0.255 to −0.008, p = 0.034). The model fit the data well (χ2(2) = 1.318, p = 0.517, Tucker–Lewis index = 1.075, comparative fit index = 1, standardised root mean residual = 0.0251, root mean square error of approximation = 0.0001).
Conclusion
Rumination and negative emotions serially mediated the relationship between DM and hallucination. The findings support the contribution of changes across transdiagnostic mediators underlying the therapeutic effects of mindfulness training. Further research examining the transdiagnostic processes of DM in influencing clinical outcomes in SSDs is warranted.
Keywords: schizophrenia spectrum disorders, psychosis, negative emotions, depression, anxiety, stress, rumination, psychotic symptoms, mindfulness
Introduction
Schizophrenia spectrum disorders (SSDs) are complex neurobehavioral disorders with a heterogeneous combination of symptoms that have a significant impact on both the individual and society.1 In addition to positive symptoms (such as delusion and hallucination) and negative symptoms (such as diminished emotional expression, avolition, alogia, asociality and anhedonia), epidemiology studies have found that depression and anxiety commonly co-occur in patients with SSDs, with over 75% of patients experiencing depression and 65% experiencing anxiety symptoms.2–9 Depression and anxiety are strongly associated with positive symptoms,2,3,5–7,9 negative symptoms,2,8 psychotic relapses3,9 and impaired social function,3,5,9 and are among the best symptom predictors of quality of life outcomes in people with SSDs.2–9 High levels of co-existing mental disorders have aroused interest in identifying the transdiagnostic factors underlying psychiatric symptoms that contribute to SSDs. Recently, researchers have suggested that rumination is an important transdiagnostic factor associated with the comorbidities of SSDs. Rumination, which is characterised by repetitive thoughts about negative personal experiences, has been suggested as an underlying mechanism for triggering and maintaining depression, anxiety and psychotic symptoms.10,11 Several studies have supported the correlation and predictive relationship between rumination and depressive symptoms,12,13 anxiety,13 positive symptoms13–16 and negative symptoms.17 A controlled trial also found that an intervention targeting rumination in patients with psychosis significantly reduced paranoid delusions relative to standard care over 8 weeks.18
Mindfulness, which refers to awareness that arises through consciously paying attention to one’s moment-to-moment experiences with nonjudgemental and acceptance stances,19 has emerged as a key domain for the understanding and treatment of mental health problems. Mindfulness has been conceptualised as both a state and a trait. State mindfulness refers to an intentional mindfulness meditation that temporarily brings one’s attention to one’s present experience and mental activity.20 Trait mindfulness, also called dispositional mindfulness (DM), is a dispositional characteristic involving a person’s tendency to abide in mindful states.20 DM has consistently been associated with fewer depressive symptoms and anxiety in clinical populations, such as people with depressive disorders,21–23 general anxiety disorders,21,22 bipolar affective disorder23–25 and post-traumatic stress disorder.21,22,26,27
Emerging evidence suggests that DM may protect against the development of psychiatric symptoms by buffering against rumination. Higher levels of DM have been frequently associated with lower levels of rumination28,29 and lower levels of depression and anxiety.30 Several mediation analyses and longitudinal studies have revealed that rumination significantly mediates associations between DM and symptoms of anxiety and depression in both community populations29,31–34 and patients with depression,22,35 anxiety disorders22,35 and substance use disorders.36 Recent randomised controlled trials investigating the effects of mindfulness training in people with major depressive disorder suggested that increased DM following mindfulness training was associated with decreased rumination, which in turn decreased negative emotions.37,38 DM theoretically directs one’s attention to the present moment nonjudgementally. This works in the opposite direction of rumination, which involves the repetitive judging of personal past experiences. The shift of attention disengages an individual from negative rumination and other psychopathological processes.20,38,39 Drawing from this framework, rumination might serve as an important mechanism underpinning the association between DM and negative emotions.29,32,40
Current evidence suggests that mindfulness practice, which cultivates both state and dispositional mindfulness in people with SSDs, could improve emotional and psychotic symptoms.41–44 Recent randomised control studies and meta-analyses showed that mindfulness-based interventions significantly improved DM, negative emotions, positive symptoms and negative symptoms compared with control groups.43–49 A 2-year longitudinal follow-up study of the relationships between changes in the five facets of mindfulness (observing, describing, acting with awareness, nonjudging and nonreactivity) and the clinical outcomes of psychotic patients who received mindfulness training revealed that all facets of mindfulness significantly increased over time and that two facets (observing and acting with awareness) were significantly associated with improvements in positive and negative symptoms.50 A recent mediation analysis also suggested that negative emotion might mediate the relationship between DM and clinical outcomes, such as quality of life, in people with SSDs.51 These results showed that increased DM was associated with improved emotions and psychotic symptoms in people with SSDs. Rumination is highly associated with negative emotions and psychotic symptoms and has been supported as a buffer between DM and psychiatric symptoms in clinical populations and SSDs. The mediating role of rumination between DM and psychiatric symptoms in SSDs deserves further investigation. To the best of our knowledge, this is the first study to investigate the causal relationship between DM and psychiatric symptoms in SSDs and to construct a conceptual model to explain how the former influences the latter. The study hypothesised that DM would predict the reduction of rumination, negative emotional status (in terms of depression, anxiety and stress levels) and psychotic symptoms (in terms of positive and negative symptoms) (H1) and that rumination would mediate the effect of DM on negative emotional status and psychotic symptoms (H2). In addition, a proposed sequential mediation model was hypothesised in which rumination and negative emotional status would serially mediate the relationship between DM and psychotic symptoms (H3).
Methods
Participants
The study was a cross-sectional, clinician-administered survey. Fifty-two participants were recruited from two Integrated Community Centres for Mental Wellness (ICCMWs) and two Long Stay Care Homes (LSCHs) covering Hong Kong’s largest geographical regions (New Territories and Kowloon, comprising 80% of Hong Kong’s area). ICCMWs are district-based community mental health centres that provide multidisciplinary assessment, continued care and rehabilitation services to psychiatric outpatients. LSCHs provide long-term residential care and active maintenance services to discharged chronic psychiatric patients. The study included patients who were aged 18 to 65 years, diagnosed with SSDs according to the criteria of the Diagnostic and Statistical Manual for Mental Disorders DSM-IV-TR (and DSM-V) or International Classification of Diseases (ICD-10) – Classification of Mental Disorders, and able to communicate in Cantonese and give informed consent. Individuals with comorbid organic brain disorders or substance abuse were excluded from this study.
Procedure
A convenience sample of patients with psychotic disorders was recruited from four study venues (two ICCMWs and two LSCHs) between May 2018 and September 2018. The participants were recruited through posters mounted at the research sites and referrals from their case managers. The study objectives and use of data were explained, and the participants were assured of confidentiality. The participants signed an informed consent form in accordance with the Declaration of Helsinki and then proceeded with clinical interviews. The clinical interviews were conducted by a psychiatric nurse who was experienced in the care and assessment of people with psychotic disorders. The study was approved by the Human Subjects Research Ethics Committees of the University of Hong Kong and Hospital Authority Hong Kong West Cluster (UW18-004) and the Hong Kong Polytechnic University (HSEARS2018531001).
Measures
Short Ruminative Response Scale
The 10-item Short Ruminative Response Scale (SRRS) is symptom- and self-focused, assessing possible causes and consequences of depressive mood.52 The SRRS comprises two distinct factors, namely, brooding (a passive comparison of one’s situation with unachievable positive standards) and reflection (purposefully engaging in inward cognitive problem-solving to relieve one’s distress).52 The items were rated on a 4-point Likert scale ranging from strongly disagree to strongly agree. The possible range of scores was between 10 and 40, with a higher score indicating a higher level of rumination. The SRRS has been frequently used to assess rumination in severe mental illnesses such as major depressive disorder and SSDs with auditory hallucination.15,53 The Chinese version of the SRRS showed satisfactory criterion-related validity, construct validity (goodness of fit index [GFI] = 0.95, incremental fit index [IFI] = 0.90, comparative fit index [CFI] = 0.92, root mean square error of approximation [RMSEA] = 0.077) and internal consistency (Cronbach’s α = 0.715 to 0.767) in Chinese undergraduate students.54
Depression Anxiety Stress Scale
The Depression Anxiety Stress Scale (DASS-21) comprises three subscales, namely, depression, anxiety and stress.55 Each subscale consists of seven items. The severity ratings are scored on a series of 4-point scales ranging from 0 (does not apply to me at all) to 3 (applies to me very much, or most of the time). Higher total or subscale scores indicate more severe symptoms. The Chinese version of DASS-21 demonstrated satisfactory convergent and discriminant validity (r = 0.41 to 0.51), internal consistency (Cronbach’s α = 0.86, 0.78 and 0.87 for the depression, anxiety and stress subscales, respectively, and 0.94 for the total scale score) in SSDs.56
Five Facet Mindfulness Questionnaire-Short Form
The Five Facet Mindfulness Questionnaire-Short Form (FFMQ-SF) consists of 20 items to measure five facets of mindfulness, namely, observing, describing, acting with awareness, nonjudging and nonreacting.57 Items are scored on a 5-point scale ranging from 1 (never/very rarely true) to 5 (very often/always true). Higher scores indicate greater levels of mindfulness. The FFMQ-SF significantly correlated with the Chinese version of the scale (FFMQ-C: r = 0.96), and the FFMQ-SF explained 91.3% of the variance of FFMQ-C.58 It exhibited good structural validity and good model fit (non-normed fit index = 0.91, CFI = 0.93, standardised root mean residual [SRMR] = 0.080 and RMSEA = 0.071) in the correlated five-factor model.58 The FFMQ-SF is reliable and valid to measure mindfulness levels in healthy Chinese people and those with significant psychological distress.
The Chinese Version of the Psychotic Symptom Rating Scale
The Chinese version of the Psychotic Symptom Rating Scale (C-PSYRATS) consists of 17 items assessing specific dimensions of hallucinations and delusions rated on a 5-point scale ranging from 0 (absent) to 4 (severe/often/extreme).59 It contains two subscales, namely, the auditory hallucinations subscale (AHS) with 11 items and the delusions subscale (DS) with six items. The scale measures the subjective characteristics of auditory hallucinations and delusions, including their nature, persistence, amount, distress, disruption and controllability.59 The C-PSYRATS showed good internal consistency (Cronbach’s α = 0.86 and 0.90 for the AHS and DS, respectively, and 0.89 for the overall scale). It also demonstrated satisfactory concurrent (Pearson’s r = 0.48 to 0.75, p = 0.003), construct (GFI = 0.097, Tucker–Lewis index [TLI] = 1.04, p = 0.02) and content validity, as well as satisfactory test–retest reliability (intraclass correlation coefficient [ICC] = 0.81 to 0.85), in Chinese people with psychosis.60
Scale for the Assessment of Negative Symptoms
The clinician-rated 25-item Scale for the Assessment of Negative Symptoms (SANS) evaluates affective flattening, anhedonia–asociality, attention, alogia and avolition–apathy.61 The symptoms feature a general description, and each domain is divided into observable behaviour (eg, lack of vocal inflexions, physical anergia). Items are rated on a 6-point scale ranging from 0 (none) to 5 (severe). Each subscale consists of several items addressing specific symptoms such as unchanging facial expression and poor eye contact. The tool demonstrated satisfactory internal consistency (Cronbach’s α = 0.74 to 0.84) and test–retest reliability (ICC = 0.70 to 0.92).61
Data Analysis
Statistical analyses were performed using SPSS (version 23.0) in Windows in conjunction with Analysis of Moment Structures (AMOS 26.0). Frequencies and/or means and standard deviations were used to describe the categorical and continuous variables. Correlations among variables were indicated by Pearson correlation coefficients.
Path analysis was performed in AMOS to examine the relationship between mindfulness facets, rumination and clinical symptoms (emotional status, positive and negative symptoms). Path analysis was adopted to confirm the mediating effect of rumination and negative emotional status and provide estimates of the relative importance of direct and indirect effects.
Parameter estimation was based on the maximum likelihood method (non-robust) and covariance matrix from the data. Alternative models were compared to test the model’s robustness and the hypothesised interpretation of the direction of the identified paths.62 Goodness of fit was assessed using the standard fit indices of chi square (χ2), CFI, TLI, SRMR and RMSEA.63,64 The chi-square/df-ratio should be less than 5 when the sample size is small and should not be significant.65 A TLI and CFI larger than 0.95 represent a perfect fit. The SRMR is a popular absolute fit indicator and should be smaller than 0.08. The RMSEA estimates lack of fit in a model compared with a perfect model and should therefore be smaller than 0.05.
Unstandardised direct, indirect and total effects were estimated with bootstrapping (size 5000). All significant tests were two-sided with a 5% level of significance. Specific indirect effects were tested using an “indirect effects” plugin developed by Gaskin and Lim (2018).66
Results
Fifty-two patients with psychotic disorders participated in the study. Thirty-eight of the participants (73.1%) were female. The average age was 51.44 (standard deviation [SD] = 9.15), and the average duration of illness was 24.49 (SD = 9.7) years. Majorities of the 52 participants were married (n = 38, 73.1%), lived in LSCHs (n = 27, 51.9%) and had a secondary school education or above (n = 34, 65.3%). Twenty-eight were unemployed (53.8%). Details of the socio-demographic and clinical characteristics are summarised in Table 1.
Table 1.
Participants’ Sociodemographic and Clinical Characteristics. (N = 52)
| Characteristics | Mean (SD)/Percentage (n) |
|---|---|
| Age (mean) | 51.44 SD 9.15 |
| Duration of Illness (DOI) (mean) | 24.49 (9.7) |
| Sex | |
| - Male | 26.9 (14) |
| - Female | 73.1 (38) |
| Marital status | |
| - Married | 73.1 (38) |
| - Single | 11.5 (6) |
| - Divorce | 15.4 (8) |
| Residence | |
| - Community | 48.1 (25) |
| - Long stay care home | 51.9 (27) |
| Education | |
| - Primary school | 17.3 (9) |
| - Secondary school | 53.8 (28) |
| - University/College | 11.5 (6) |
| - Others | 17.3 (9) |
| Employment | |
| - Full time | 11.5 (6) |
| - Part time | 5.8 (3) |
| - Unemployment | 53.8 (28) |
| - Others | 28.8 (15) |
The mean (SD) scores of the outcome measures are shown in Table 2. There were significant negative associations between mindfulness and negative emotional status (r = −0.422, p = 0.002), mindful nonjudging and rumination (r = −0.563, p < 0.0001), acting with awareness and rumination (r = −0.406, p = 0.003), nonjudging and negative emotional status (r = −0.416, p = 0.002) and acting with awareness and negative emotional status (r = −0.582, p < 0.0001). In addition, there were significant positive associations between rumination and negative emotional status (r = 0.621, p < 0.0001), rumination and hallucination (r = 0.293, p = 0.035) and negative emotional status and hallucination (r = 0.355, p = 0.010).
Table 2.
Correlations Between FFMQ, Its Facets, Rumination, and Clinical Symptoms (n=52)
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. FFMQ | 56.93 | 8.89 | 1 | ||||||||||
| 2. Nonreact | 10.48 | 3.17 | 0.452** | 1 | |||||||||
| 3. Nonjudge | 13.28 | 3.99 | 0.211 | −0.395** | 1 | ||||||||
| 4. Actaware | 13.60 | 4.72 | 0.624** | −0.083 | 0.278* | 1 | |||||||
| 5. Describe | 9.98 | 3.77 | 0.628** | 0.403** | −0.24 | 0.081 | 1 | ||||||
| 6. Observe | 9.60 | 3.14 | 0.415** | 0.413** | −0.406** | −0.101 | 0.355** | 1 | |||||
| 7. SRRS | 17.48 | 4.10 | −0.153 | 0.334* | −0.563** | −0.406** | 0.221 | 0.290* | 1 | ||||
| 8. DASS | 18.64 | 11.04 | −0.422** | 0.119 | −0.416** | −0.582** | −0.039 | 0.136 | 0.621** | 1 | |||
| 9. PSYRAT_AHS | 7.42 | 11.55 | −0.121 | −0.057 | −0.17 | −0.128 | −0.065 | 0.2 | 0.293* | 0.355** | 1 | ||
| 10. PSYRAT_DS | 2.16 | 5.01 | −0.130 | 0.149 | −0.228 | −0.225 | −0.124 | 0.257 | 0.102 | 0.124 | 0.322* | 1 | |
| 11. SANS | 55.27 | 21.92 | −0.013 | −0.095 | 0.120 | 0.254 | −0.272 | −0.150 | −0.035 | −0.102 | 0.142 | 0.126 | 1 |
Notes: *p<0.05, **p<0.01.
Abbreviations: FFMQ, Five Facet Mindfulness Questionnaire; Observe, FFMQ facet – Observing; Describe, FFMQ facet – Describing; Actaware, FFMQ facet - Acting with awareness; Nonjudge, FFMQ facet – Nonjudging; Nonreact, FFMQ facet – Nonreacting; SRRS, Short rumination response scale; DASS, Depression Anxiety Stress Scales; PSYRAT_AHS, Psychotic Symptoms Rating Scale-Auditory hallucination scale; PSYRAT_DS, Psychotic Symptoms Rating Scale-Delusion scale; SANS, The Scale for the Assessment of Negative Symptoms.
An initial structural equation model was designed in which rumination was considered as a mediator of the relationship between the total mindfulness score and negative emotional status, and psychotic symptoms were predicted by negative emotional status. Meanwhile, only two mindfulness facets (nonjudging and acting with awareness) showed statistically significant relationships with rumination and negative emotional status. In addition, negative symptoms and delusion showed no correlation with overall mindfulness, the five facets of mindfulness, emotional status or rumination. Therefore, only two mindfulness facets (nonjudging and acting with awareness) were included in the mediation analysis, while negative symptoms and delusion were excluded from the model.
This initial model revealed no association between the suggested demographic variables and endogenous variables, except education level and DASS-21 (B = 1.78, SE = 0.89, p = 0.045). Education level was therefore controlled in the structural equation model while other demographic variables were removed. Unstandardised regression estimates of the tested model are illustrated in Figure 1, with lines indicating the significant paths and dashed lines indicating the non-significant paths. For visual clarity, the correlations among error terms and the control variable included in the model are not presented. The model provided a good fit to the data (χ2(2) = 1.318, p = 0.517, TLI = 1.075, CFI = 1, SRMR = 0.0251, RMSEA = 0.0001). The statistical details of the path coefficients are presented in Tables 3 and 4. Because hypothesis H1 suggested that DM would predict psychotic symptoms, the model including the path between these two mindfulness facets and hallucination was also run. However, the model indexes failed to show a good fit (χ2(1) = 4.47, p < 0.05, TLI = 0.235, CFI = 0.949, RMSEA = 0.261).
H1: DM would predict the reduction of rumination, negative emotional status and psychotic symptoms.
Figure 1.
Unstandardized parameter estimates for the proposed model.
Table 3.
Summary of the Total and Direct Effects for the Proposed Model (Unstandardized Coefficient)
| Pathways | Direct Effect | Total Effect | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | S.E. | Lower | Upper | p | B | S.E. | Lower | Upper | p | |||
| Actaaware | ➔ | SRRS | −0.218 | 0.099 | −0.374 | −0.051 | 0.035* | |||||
| Nonjudge | ➔ | SRRS | −0.495 | 0.103 | −0.662 | −0.328 | 0.001** | |||||
| Actaaware | ➔ | DASS | −0.994 | 0.3 | −1.455 | −0.489 | 0.002** | −1.254 | 0.31 | −1.745 | −0.703 | 0.002** |
| Nonjudge | ➔ | DASS | −0.198 | 0.335 | −0.742 | 0.355 | 0.61 | −0.788 | 0.279 | −1.261 | −0.348 | 0.007** |
| Actaaware | ➔ | PSYRAT_AHS | −0.44 | 0.184 | −0.771 | −0.17 | 0.010* | |||||
| Nonjudge | ➔ | PSYRAT_AHS | −0.356 | 0.182 | −0.693 | −0.077 | 0.035* | |||||
Notes: *p < 0.050; **p < 0.010.
Abbreviations: FFMQ – Actaaware, Five Facet Mindfulness Questionnaire – Acting with Awareness; FFMQ – Nonjudge, Five Facet Mindfulness Questionnaire – Nonjudge; SRRS, Short rumination response scale; DASS, Depression Anxiety Stress Scales; PSYRAT_AHS, Psychotic Symptoms Rating Scale-Auditory hallucination scale.
Table 4.
Summary of the Indirect Effects for the Proposed Model (Unstandardized Coefficient)
| Pathways | B | S.E. | Lower | Upper | p |
|---|---|---|---|---|---|
| Indirect effect of Acting with Awareness on Depression, anxiety and stress | |||||
| Through Rumination | −0.26 | 0.139 | −0.263 | −0.019 | 0.019* |
| Indirect effect of Nonjudgement on Depression, anxiety and stress | |||||
| Through Rumination | −0.591 | 0.206 | −0.402 | −0.081 | 0.001** |
| Indirect effect of Acting with Awareness on Hallucination | |||||
| Total | −0.44 | 0.184 | −0.338 | −0.045 | 0.01* |
| Through Rumination | −0.048 | 0.114 | −0.274 | 0.088 | 0.433 |
| Through Depression, anxiety and stress | −0.310 | 0.19 | −0.651 | −0.022 | 0.076 |
| Through Rumination and then Depression, anxiety and stress | −0.081 | 0.073 | −0.324 | −0.016 | 0.032* |
| Indirect effect of Nonjudgement on Hallucination | |||||
| Total | −0.356 | 0.182 | −0.255 | −0.008 | 0.034* |
| Through Rumination | −0.110 | 0.231 | −0.499 | 0.262 | 0.597 |
| Through Depression, anxiety and stress | −0.062 | 0.123 | −0.339 | 0.072 | 0.401 |
| Through Rumination and then Depression, anxiety and stress | −0.184 | 0.14 | −0.541 | −0.31 | 0.039* |
Notes: *p < 0.050; **p < 0.010.
Increased acting with awareness and nonjudging significantly reduced rumination (acting with awareness: B = −0.218, 95% confidence interval [CI] = −0.374 to −0.051, p = 0.035; nonjudging: B = −0.495, 95% CI = −0.662 to −0.328, p = 0.001). Increased acting with awareness and nonjudging significantly reduced negative emotional status (acting with awareness: B = −1.254, 95% CI = −1.745 to −0.703, p = 0.002; nonjudging: B = −0.788, 95% CI = −1.261 to −0.348, p = 0.007) (see Table 3).
H2: Rumination would mediate the effect of DM on negative emotional status and psychotic symptoms.
Two mindfulness facets (nonjudging and acting with awareness) affected negative emotional status both directly and indirectly. Acting with awareness reduced depression, anxiety and stress levels both directly (B = −0.994, 95% CI = −1.455 to −0.489, p = 0.002) and indirectly, mediated by rumination (B = −0.26, 95% CI = −0.263 to −0.019, p = 0.019). Nonjudging reduced depression, anxiety and stress levels indirectly (B = −0.591, 95% CI = −0.402 to −0.081, p = 0.001), but the direct effect was not significant (B = −0.198, 95% CI = −0.742 to 0.355, p = 0.61), suggesting that rumination fully mediated the effect of nonjudging on negative emotional status. The model including the path between two mindfulness facets (nonjudging and acting with awareness) and hallucination was run to explore the mediating effect of rumination between DM and hallucination. However, as mentioned, the model indexes showed a poor fit. The direct and indirect effects are shown in Tables 3 and 4.
H3: Rumination and negative emotional status would serially mediate the relationship between DM and psychotic symptoms.
There was no correlation between acting with awareness and hallucination (r = −0.128, p > 0.05) or between nonjudging and hallucination (r = −0.17, p > 0.05). However, there were significant indirect effects between acting with awareness and hallucination (B = −0.44, 95% CI = −0.338 to −0.045, p = 0.01) and between nonjudging and hallucination (B = −0.356, 95% CI = −0.255 to −0.008, p = 0.034). There were three specific indirect pathways between acting with awareness and hallucination and between nonjudging and hallucination. The pathway through rumination and then negative emotional status was significant in both relationships (acting with awareness: B = −0.081, CI = −0.324 to −0.016, p = 0.032; nonjudging: B = −0.184, 95% CI = −0.541 to −0.31, p = 0.039), but the pathways through either rumination or emotional status were not significant. The results showed that rumination and negative emotional status sequentially mediated the relationship between acting with awareness and hallucination and between nonjudging and hallucination. The indirect effects of the proposed model are summarised in Table 4.
Discussion
This was the first study to explore the mechanisms underpinning the relationship between DM and clinical symptomatology in SSDs. The results supported the hypothesis that increased DM was associated with reduced rumination and reduced negative emotional status; and the hypothesis that rumination might directly and indirectly mediate the effects of acting with awareness and nonjudging on negative emotional status. The results suggested that rumination and negative emotional status might mediate the influence of acting with awareness and nonjudging on hallucination. The findings were in line with recent systematic reviews that found rumination to be a significant mediator of the effects of DM on global psychopathological symptoms in clinical populations.67,68 The findings also provided exploratory information on the underlying mechanism of mindfulness training that might improve clinical outcomes by modifying transdiagnostic factors like rumination or negative emotions associated with psychotic symptoms.44,50,69
Our findings suggested that rumination might act as an independent mediator of the relationship between DM and the negative emotional status among patients with SSDs. Laboratory and experimental studies have discovered that people with SSDs have intact emotional experiences and even stronger emotional intensity than healthy populations despite reduced emotional expressivity.70–72 Studies have shown that people with SSDs make greater use of rumination, which is strongly linked to depressive symptoms.15,17,71,73,74 Patients struggle with ruminative thinking focused on mental illness, symptoms, social disability and social difficulties in work and relationships.12,75 This ruminative tendency induces deleterious effects such as increasing recall of negative memories and greater attention to personal deficits, which increases the risk of psychotic symptoms.12,69 Our findings supported the theoretical model of mindfulness for psychosis suggested by Chadwick (2015), which proposed that DM serves as an alternative way for patients to become clearly aware of their illness experience and respond to their experience nonjudgementally.50,75 However, it is important to note that our results did not fully examine the effect of all mediating factors listed in the theoretical model, such as experience avoidance and acceptance, on the relationship between DM and psychopathological symptoms in SSDs. Further longitudinal studies are needed to elucidate the utility of mindfulness theory.
Our results also suggested that two mindfulness facets (acting with awareness and nonjudging) might be significant predictors of rumination and subsequent change in levels of depression, anxiety and stress. The findings were consistent with previous studies and a recent mediation analysis that found acting with awareness and nonjudging to be significant predictors of depression and anxiety, while describing and observing were found to be unable to predict depression and anxiety in the general population and people with SSDs.51,76,77 Acting with awareness and nonjudging were suggested to have a substantial role in the prediction of rumination and mental health outcomes, particularly depressive symptoms and quality of life.51,76,77 Individuals who were judgemental and lacked awareness were found to have higher levels of depression and anxiety and were more inclined to self-criticise and ruminate on negative feelings rather than responding with awareness and self-acceptance, potentially exacerbating and maintaining psychopathological symptoms.77–79
The study results showed that the influence of DM on hallucination was completely mediated by rumination and negative emotions and significantly mediated by the specific pathway from rumination to negative emotional status. The results contradicted our hypothesis that increased DM would reduce psychotic symptoms both directly and indirectly through the mediation of rumination and negative emotions. We ran an alternative model by adding direct paths between two mindfulness facets (acting with awareness and nonjudging) and hallucination, but the model showed a poor fit. The poor model fit might be explained by the small sample size in this study, which was insufficient to test all possible regression paths.9 However, the findings still provided preliminary evidence about the mediating effects of transdiagnostic factors between DM and hallucination. DM and mindfulness practice are conceptualised as cognitive processes that may influence the underlying transdiagnostic mediators associated with psychopathology. Transdiagnostic mediators such as rumination and negative emotion are suggested to amplify or buffer the psychopathological process.51 DM and mindfulness practice may help to uncouple these transdiagnostic processes implicated in the comorbidities of SSDs.51,80 Our findings shed light on the contribution of changes in transdiagnostic mediators underlying the therapeutic effects of mindfulness training. However, further research is needed to confirm the mediating role of rumination, negative emotions and other transdiagnostic factors in the relationship between DM and psychotic symptoms in SSDs.
Limitations
The study had several limitations. First, the sample size was small, which would affect the accuracy of parameter estimates in the path analysis. Second, although this was a multi-site study, convenience sampling was adopted for subject recruitment, which led to self-selection bias. Third, majorities of the participants in this study were female, aged over 45 and married, with a long duration of illness, which might limit the generalisation of the findings. Fourth, the study adopted a cross-sectional study design. Further research should include longitudinal mediation analyses with objective psychophysiological measurements to examine how DM operates through mediators to impact emotion regulation and psychotic symptoms in SSDs.
Implications
The study provided evidence that DM might predict clinical outcomes through the influence of rumination and symptoms of depression, anxiety and stress. Other transdiagnostic processes should be further explored to elicit more potential ways to remediate the transdiagnostic process that underlies psychopathological problems in people with SSDs. Further longitudinal studies using psychophysiological measurements (such as neuroimaging) should be conducted to elicit the underexplored mechanism of DM and its influence on the transdiagnostic process underpinning psychopathological problems. In a paradigmatic shift away from conventional, symptom-specific treatment, the current findings highlighted the importance of targeting rumination and DM in transdiagnostic treatment approaches to SSDs. Further prospective and experimental studies should explore the potential utility of transdiagnostic interventions targeting DM and rumination in this population.
Acknowledgments
The abstract of this paper, “Mindfulness and mood symptomatology in schizophrenia: the mediating roles of rumination”, was presented at the 11th Asian Conference on Psychology and the Behavioral Sciences (ACP2021) as a conference presentation with interim findings. The abstract was published in the ACP2021 programme abstract book: https://iafor.org/archives/conference-programmes/acp/acp-programme-2021.pdf
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Maggini C, Raballo A. Exploring depression in schizophrenia. Eur Psychiatry. 2006;21(4):227–232. doi: 10.1016/j.eurpsy.2005.07.001 [DOI] [PubMed] [Google Scholar]
- 3.Hartley S, Barrowclough C, Haddock G. Anxiety and depression in psychosis: a systematic review of associations with positive psychotic symptoms. Acta Psychiatr Scand. 2013;128(5):327–346. doi: 10.1111/acps.12080 [DOI] [PubMed] [Google Scholar]
- 4.Muller JE, Koen L, Seedat S, et al. Anxiety disorders and schizophrenia. Curr Psychiatry Rep. 2004;6(4):255–261. [DOI] [PubMed] [Google Scholar]
- 5.Baynes D, Mulholland C, Cooper SJ, et al. Depressive symptoms in stable chronic schizophrenia: prevalence and relationship to psychopathology and treatment. Schizophr Res. 2000;45(1–2):47–56. doi: 10.1016/S0920-9964(99)00205-4 [DOI] [PubMed] [Google Scholar]
- 6.Huppert JD, Smith TE. Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS Spectr. 2005;10(9):721–731. doi: 10.1017/S1092852900019714 [DOI] [PubMed] [Google Scholar]
- 7.Moritz S, Göritz AS, McLean B, et al. Do depressive symptoms predict paranoia or vice versa? J Behav Ther Exp Psychiatry. 2017;56:113–121. doi: 10.1016/j.jbtep.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 8.Edwards CJ, Garety P, Hardy A. The relationship between depressive symptoms and negative symptoms in people with non-affective psychosis: a meta-analysis. Psychol Med. 2019;49(15):2486–2498. doi: 10.1017/S0033291719002381 [DOI] [PubMed] [Google Scholar]
- 9.Temmingh H, Stein DJ. Anxiety in patients with schizophrenia: epidemiology and management. CNS Drugs. 2015;29(10):819–832. doi: 10.1007/s40263-015-0282-7 [DOI] [PubMed] [Google Scholar]
- 10.Sellers R, Wells A, Morrison AP. Are experiences of psychosis associated with unhelpful metacognitive coping strategies? A systematic review of the evidence. Clin Psychol Psychother. 2018;25(1):31–49. doi: 10.1002/cpp.2132 [DOI] [PubMed] [Google Scholar]
- 11.Cui Y, Kim SW, Lee BJ, et al. Negative schema and rumination as mediators of the relationship between childhood trauma and recent suicidal ideation in patients with early psychosis. J Clin Psychiatry. 2019;80(3):17m12088. [DOI] [PubMed] [Google Scholar]
- 12.Thomas N, Ribaux D, Phillips LJ. Rumination, depressive symptoms and awareness of illness in schizophrenia. Behav Cogn Psychother. 2014;42(2):143–155. doi: 10.1017/S1352465812000884 [DOI] [PubMed] [Google Scholar]
- 13.Bassett M, Sperlinger D, Freeman D. Fear of madness and persecutory delusions: preliminary investigation of a new scale. Psychosis. 2009;1(1):39–50. doi: 10.1080/17522430802535031 [DOI] [Google Scholar]
- 14.Hartley S, Haddock G, Vasconcelos e Sa D, et al. An experience sampling study of worry and rumination in psychosis. Psychol Med. 2014;44(8):1605–1614. doi: 10.1017/S0033291713002080 [DOI] [PubMed] [Google Scholar]
- 15.Badcock JC, Paulik G, Maybery MT. The role of emotion regulation in auditory hallucinations. Psychiatry Res. 2011;185(3):303–308. doi: 10.1016/j.psychres.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 16.Vorontsova N, Garety P, Freeman D. Cognitive factors maintaining persecutory delusions in psychosis: the contribution of depression. J Abnorm Psychol. 2013;122(4):1121–1131. doi: 10.1037/a0034952 [DOI] [PubMed] [Google Scholar]
- 17.Halari R, Premkumar P, Farquharson L, et al. Rumination and negative symptoms in schizophrenia. J Nerv Ment Dis. 2009;197(9):703–706. doi: 10.1097/NMD.0b013e3181b3af20 [DOI] [PubMed] [Google Scholar]
- 18.Freeman D, Dunn G, Startup H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry. 2015;2(4):305–313. doi: 10.1016/S2215-0366(15)00039-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kabat-Zinn J. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936–943. [DOI] [PubMed] [Google Scholar]
- 20.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11(3):230–241. [Google Scholar]
- 21.Barnhofer T, Duggan DS, Griffith JW. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Pers Individ Dif. 2011;51(8):958–962. doi: 10.1016/j.paid.2011.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desrosiers A, Vine V, Klemanski DH, et al. Mindfulness and emotion regulation in depression and anxiety: common and distinct mechanisms of action. Depress Anxiety. 2013;30(7):654–661. doi: 10.1002/da.22124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilbert K, Gruber J. Emotion regulation of goals in bipolar disorder and major depression: a comparison of rumination and mindfulness. Cognit Ther Res. 2014;38(4):375–388. doi: 10.1007/s10608-014-9602-3 [DOI] [Google Scholar]
- 24.Carruthers SP, Rossell SL, Murray G, et al. Mindfulness, mood symptom tendencies and quality of life in bipolar disorder: an examination of the mediating influence of emotion regulation difficulties. J Affect Disord. 2021;298(Pt A):166–172. doi: 10.1016/j.jad.2021.10.107 [DOI] [PubMed] [Google Scholar]
- 25.Xuan R, Li X, Qiao Y, et al. Mindfulness-based cognitive therapy for bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. 2020;290:113116. doi: 10.1016/j.psychres.2020.113116 [DOI] [PubMed] [Google Scholar]
- 26.Carpenter JK, Conroy K, Gomez AF, et al. The relationship between trait mindfulness and affective symptoms: a meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clin Psychol Rev. 2019;74:101785. doi: 10.1016/j.cpr.2019.101785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garland EL, Roberts-Lewis A. Differential roles of thought suppression and dispositional mindfulness in posttraumatic stress symptoms and craving. Addict Behav. 2013;38(2):1555–1562. doi: 10.1016/j.addbeh.2012.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tomlinson ER, Yousaf O, Vittersø AD, et al. Dispositional mindfulness and psychological health: a systematic review. Mindfulness. 2018;9(1):23–43. doi: 10.1007/s12671-017-0762-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parmentier FBR, García-Toro M, García-Campayo J, et al. Mindfulness and symptoms of depression and anxiety in the general population: the mediating roles of worry, rumination, reappraisal and suppression. Front Psychol. 2019;10:506. doi: 10.3389/fpsyg.2019.00506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3(5):400–424. doi: 10.1111/j.1745-6924.2008.00088.x [DOI] [PubMed] [Google Scholar]
- 31.Coffey KA, Hartman M, Fredrickson BL. Deconstructing mindfulness and constructing mental health: understanding mindfulness and its mechanisms of action. Mindfulness. 2010;1(4):235–253. doi: 10.1007/s12671-010-0033-2 [DOI] [Google Scholar]
- 32.Petrocchi N, Ottaviani C. Mindfulness facets distinctively predict depressive symptoms after two years: the mediating role of rumination. Pers Individ Dif. 2016;93:92–96. doi: 10.1016/j.paid.2015.08.017 [DOI] [Google Scholar]
- 33.Alleva J, Roelofs J, Voncken M, et al. On the relation between mindfulness and depressive symptoms: rumination as a possible mediator. Mindfulness. 2012;5(1):72–79. doi: 10.1007/s12671-012-0153-y [DOI] [Google Scholar]
- 34.Ciesla JA, Reilly LC, Dickson KS, et al. Dispositional mindfulness moderates the effects of stress among adolescents: rumination as a mediator. J Clin Child Adolesc Psychol. 2012;41(6):760–770. doi: 10.1080/15374416.2012.698724 [DOI] [PubMed] [Google Scholar]
- 35.Desrosiers A, Vine V, Curtiss J, et al. Observing nonreactively: a conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. J Affect Disord. 2014;165:31–37. doi: 10.1016/j.jad.2014.04.024 [DOI] [PubMed] [Google Scholar]
- 36.Cao Q, Zhao H, Yao J, et al. Anxiety and sleep quality in Chinese persons with a substance use disorder: a moderated mediation model of rumination and mindfulness. Curr Psychol. 2019;40(6):2715–2724. doi: 10.1007/s12144-019-00200-5 [DOI] [Google Scholar]
- 37.Hawley LL, Schwartz D, Bieling PJ, et al. Mindfulness practice, rumination and clinical outcome in mindfulness-based treatment. Cognit Ther Res. 2013;38(1):1–9. doi: 10.1007/s10608-013-9586-4 [DOI] [Google Scholar]
- 38.Perestelo-Perez L, Barraca J, Peñate W, et al. Mindfulness-based interventions for the treatment of depressive rumination: systematic review and meta-analysis. Int J Clin Health Psychol. 2017;17(3):282–295. doi: 10.1016/j.ijchp.2017.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farb NAS, Anderson AK, Irving JA, Segal ZV. Mindfulness interventions and emotion regulation. In: Gross JJ, editor. Handbook of Emotion Regulation. The Guilford Press; 2014:548–567. [Google Scholar]
- 40.Svendsen JL, Kvernenes KV, Wiker AS, et al. Mechanisms of mindfulness: rumination and self-compassion. Nordic Psychol. 2016;69(2):71–82. doi: 10.1080/19012276.2016.1171730 [DOI] [Google Scholar]
- 41.Hofmann SG, Sawyer AT, Witt AA, et al. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Strauss C, Cavanagh K, Oliver A, et al. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS One. 2014;9(4):e96110. doi: 10.1371/journal.pone.0096110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tong AC, Lin JJ, Cheung VY, et al. A low-intensity mindfulness-based intervention for mood symptoms in people with early psychosis: development and pilot evaluation. Clin Psychol Psychother. 2015;23(6):550–560. [DOI] [PubMed] [Google Scholar]
- 44.Lam AHY, Leung SF, Lin JJ, et al. The effectiveness of a mindfulness-based psychoeducation programme for emotional regulation in individuals with schizophrenia spectrum disorders: a pilot randomised controlled trial. Neuropsychiatr Dis Treat. 2020;16:729–747. doi: 10.2147/NDT.S231877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chadwick P, Strauss C, Jones A-M, et al. Group mindfulness-based intervention for distressing voices: a pragmatic randomised controlled trial. Schizophr Res. 2016;175(1–3):168–173. doi: 10.1016/j.schres.2016.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jansen JE, Gleeson J, Bendall S, et al. Acceptance- and mindfulness-based interventions for persons with psychosis: a systematic review and meta-analysis. Schizophr Res. 2020;215:25–37. doi: 10.1016/j.schres.2019.11.016 [DOI] [PubMed] [Google Scholar]
- 47.Chien WT, Bressington D, Yip A, et al. An international multi-site, randomized controlled trial of a mindfulness-based psychoeducation group programme for people with schizophrenia. Psychol Med. 2017;47:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hodann-Caudevilla RM, Díaz-Silveira C, Burgos-Julián FA, et al. Mindfulness-based interventions for people with schizophrenia: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(13):4690. doi: 10.3390/ijerph17134690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu YC, Li IL, Hsiao FH. Effectiveness of mindfulness-based intervention on psychotic symptoms for patients with schizophrenia: a meta-analysis of randomized controlled trials. J Adv Nurs. 2021;77(6):2565–2580. doi: 10.1111/jan.14750 [DOI] [PubMed] [Google Scholar]
- 50.Chien WT, Chow KM, Chong YY, et al. The role of five facets of mindfulness in a mindfulness-based psychoeducation intervention for people with recent-onset psychosis on mental and psychosocial health outcomes. Front Psychiatry. 2020;11:177. doi: 10.3389/fpsyt.2020.00177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bergmann N, Hahn E, Hahne I, et al. The relationship between mindfulness, depression, anxiety, and quality of life in individuals with schizophrenia spectrum disorders. Front Psychol. 2021;12:708808. doi: 10.3389/fpsyg.2021.708808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Treynor W. Rumination reconsidered: a psychometric analysis. Cognit Ther Res. 2003;27(3):247–259. doi: 10.1023/A:1023910315561 [DOI] [Google Scholar]
- 53.Parola N, Zendjidjian XY, Alessandrini M, et al. Psychometric properties of the ruminative response scale-short form in a clinical sample of patients with major depressive disorder. Patient Prefer Adherence. 2017;11:929–937. doi: 10.2147/PPA.S125730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang H, Xu Y. Reliability and validity of the Chinese Short Ruminative Responses Scale (SRRS) in Chinese undergraduates. Psychol Res. 2010;4:54. [Google Scholar]
- 55.Norton PJ. Depression Anxiety and Stress Scales (DASS-21): psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253–265. doi: 10.1080/10615800701309279 [DOI] [PubMed] [Google Scholar]
- 56.Wang K, Shi H-S, Geng F-L, et al. Cross-cultural validation of the depression anxiety stress scale-21 in China. Psychol Assess. 2016;28(5):e88–e100. doi: 10.1037/pas0000207 [DOI] [PubMed] [Google Scholar]
- 57.Baer RA, Smith GT, Hopkins J, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- 58.Hou J, Wong SY-S, Lo HH-M, et al. Validation of a Chinese version of the five facet mindfulness questionnaire in Hong Kong and development of a short form. Assessment. 2014;21(3):363–371. doi: 10.1177/1073191113485121 [DOI] [PubMed] [Google Scholar]
- 59.Haddock G, McCARRON J, Tarrier N, et al. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med. 1999;29(4):879–889. doi: 10.1017/S0033291799008661 [DOI] [PubMed] [Google Scholar]
- 60.Chien W-T, Lee IY-M, Wang L-Q. A Chinese version of the psychotic symptom rating scales: psychometric properties in recent-onset and chronic psychosis. Neuropsychiatr Dis Treat. 2017;13:745–753. doi: 10.2147/NDT.S131174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Andreasen NC. Negative symptoms in schizophrenia. Definition and reliability. Arch Gen Psychiatry. 1982;39(7):784–788. doi: 10.1001/archpsyc.1982.04290070020005 [DOI] [PubMed] [Google Scholar]
- 62.Kline RB. Principles and Practice of Structural Equation Modelling. New York: Guilford Press; 1998. [Google Scholar]
- 63.Byrne BM. Testing for multigroup invariance using AMOS graphics: a road less traveled. Struct Equ Model Multidiscip J. 2004;11(2):272–300. doi: 10.1207/s15328007sem1102_8 [DOI] [Google Scholar]
- 64.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 65.Wheaton B, Muthen B, Alwin DF, et al. Assessing reliability and stability in panel models. Sociol Methodol. 1977;8:84–136. doi: 10.2307/270754 [DOI] [Google Scholar]
- 66.Gaskin J, Lim J. “Indirect Effects”, AMOS Plugin. Gaskination’s StatWiki; 2018.
- 67.Gu J, Strauss C, Bond R, et al. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- 68.Alsubaie M, Abbott R, Dunn B, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev. 2017;55:74–91. doi: 10.1016/j.cpr.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 69.Ludwig L, Mehl S, Schlier B, et al. Awareness and rumination moderate the affective pathway to paranoia in daily life. Schizophr Res. 2020;216:161–167. doi: 10.1016/j.schres.2019.12.007 [DOI] [PubMed] [Google Scholar]
- 70.Horan WP, Hajcak G, Wynn JK, et al. Impaired emotion regulation in schizophrenia: evidence from event-related potentials. Psychol Med. 2013;43(11):2377–2391. doi: 10.1017/S0033291713000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van der Meer L, Wout M, Aleman A. Emotion regulation strategies in patients with schizophrenia. Psychiatry Res. 2009;170(2):108–113. doi: 10.1016/j.psychres.2009.07.010 [DOI] [PubMed] [Google Scholar]
- 72.Visser KF, Esfahlani FZ, Sayama H, et al. An ecological momentary assessment evaluation of emotion regulation abnormalities in schizophrenia. Psychol Med. 2018;48(14):2337–2345. doi: 10.1017/S0033291717003865 [DOI] [PubMed] [Google Scholar]
- 73.Ricarte JJ, Hernández JV, Latorre JM, et al. Rumination and autobiographical memory impairment in patients with schizophrenia. Schizophr Res. 2014;160(1–3):163–168. doi: 10.1016/j.schres.2014.10.027 [DOI] [PubMed] [Google Scholar]
- 74.Lebert L, Turkington D, Freeston M, et al. Rumination, intolerance of uncertainty and paranoia in treatment resistant psychosis. Psychosis. 2020;13(1):65–70. doi: 10.1080/17522439.2020.1798489 [DOI] [Google Scholar]
- 75.Chadwick P, Taylor KN, Abba N. Mindfulness groups for people with psychosis. Behav Cogn Psychother. 2005;33(3):351–359. doi: 10.1017/S1352465805002158 [DOI] [Google Scholar]
- 76.Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1(3):177–182. doi: 10.1007/s12671-010-0023-4 [DOI] [Google Scholar]
- 77.Barcaccia B, Baiocco R, Pozza A, et al. The more you judge the worse you feel. A judgemental attitude towards one’s inner experience predicts depression and anxiety. Pers Individ Dif. 2019;138:33–39. doi: 10.1016/j.paid.2018.09.012 [DOI] [Google Scholar]
- 78.Nakajima M, Takano K, Tanno Y. Mindfulness relates to decreased depressive symptoms via enhancement of self-insight. Mindfulness. 2018;10(5):894–902. doi: 10.1007/s12671-018-1049-2 [DOI] [Google Scholar]
- 79.De Lissnyder E, Koster EHW, Goubert L, et al. Cognitive control moderates the association between stress and rumination. J Behav Ther Exp Psychiatry. 2012;43(1):519–525. doi: 10.1016/j.jbtep.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 80.Greeson JM, Zarrin H, Smoski MJ, et al. Mindfulness meditation targets transdiagnostic symptoms implicated in stress-related disorders: understanding relationships between changes in mindfulness, sleep quality, and physical symptoms. Evid Based Complement Alternat Med. 2018;2018:4505191. doi: 10.1155/2018/4505191 [DOI] [PMC free article] [PubMed] [Google Scholar]