Abstract
This review was focused on global data analysis and risk factors associated with morbidity and mortality of coronavirus disease 2019 from different countries, including Bangladesh, Brazil, China, Central Eastern Europe, Egypt, India, Iran, Pakistan, and South Asia, Africa, Turkey and UAE. Male showed higher confirmed and death cases compared to females in most of the countries. In addition, the case fatality ratio (CFR) for males was higher than for females. This gender variation in COVID-19 cases may be due to males' cultural activities, but similar variations in the number of COVID-19 affected males and females globally. Variations in the immune system can illustrate this divergent risk comparatively higher in males than females. The female immune system may have an edge to detect pathogens slightly earlier. In addition, women show comparatively higher innate and adaptive immune responses than men, which might be explained by the high density of immune-related genes in the X chromosome. Furthermore, SARS-CoV-2 viruses use angiotensin-converting enzyme 2 (ACE2) to enter the host cell, and men contain higher ACE2 than females. Therefore, males may be more vulnerable to COVID-19 than females. In addition, smoking habit also makes men susceptible to COVID-19. Considering the age-wise distribution, children and older adults were less infected than other age groups and the death rate. On the contrary, more death in the older group may be associated with less immune system function. In addition, most of these group have comorbidities like diabetes, high pressure, low lungs and kidney function, and other chronic diseases. Due to the substantial economic losses and the numerous infected people and deaths, research examining the features of the COVID-19 epidemic is essential to gain insight into mitigating its impact in the future and preparedness for any future epidemics.
Abbreviations: COVID-19, Coronavirus disease 2019; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus-2
Keywords: COVID-19, SARS-CoV-2, Pandemic, One-health, Epidemiology, Mortality
1. Introduction
By the end of December 2019, Wuhan, Hubei Province, China, reported outbreaks of severe pneumonia with unknown causes in human residents (Wang et al., 2020a). The responsible pathogen was identified as Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), and the disease it caused was referred to as Coronavirus Disease-19 (COVID-19) (Lai et al., 2020). Coronaviruses are enveloped, icosahedral symmetric particles and one of the major groups of viruses within the order Nidovirales, suborder Coronavirinae, and family Coronaviridae. Coronaviridae is categorized as the Letovirinae and Orthocoronavirinae subfamilies. Letovirinae includes the genus named as Alphaletovirus, whereas Orthocoronaviridae is ranked into four genera: Alphacoronavirus (αCoV), Betacoronavirus (βCoV), Gammacoronavirus (γCoV), and Deltacoronavirus (δCoV) (Cui et al., 2019; Helmy et al., 2020). COVID-19 is an acute respiratory infectious disease, which spreads mainly through the respiratory tract via droplets, respiratory secretions transferred from an infected person, or to a lesser degree with direct contact with contaminated fomites. The incubation period of this disease varies from 2 to 14 days (average five days) (Lee and Hsueh, 2020). Some cases have an incubation period of 21–27 days (Bai et al., 2020). On October 9, 2021, a total of 238,275,286 cases of COVID-19 cases were confirmed worldwide, including 4,861,159 deaths (Worldometer COVID-19 CORONAVIRUS PANDEMIC, 2020).
Due to the enormous economic losses and the numerous infected people and deaths, research examining the features of the COVID-19 epidemic is vital to gain insight into mitigating its impact in the future and preparedness for any future epidemics. Therefore, in this review, we analysed the global data and risk factors associated with morbidity and mortality of COVID-19 in different countries, including Africa, Bangladesh, Brazil, China, Eastern Europe, Egypt, India, Iran, Pakistan, Poland, Turkey and UAE.
2. COVID-19 morbidity, mortality, and associated risk factors in China
In central China, Wuhan is the largest and capital city of Hubei Province, also known as the “Chicago of China”. It is considered central China's leading economic and industrial part, and the estimated population is over 11 million (ECDC Outbreak of Acute Respiratory Syndrome Associated with a Novel Coronavirus, China: First Local Transmission in the EU/EEA − Third Update, 2020). Towards the end of 2019, cases of mysterious pneumonia were reported around the globe. In late December 2019, patients with similar symptoms of concentrated pneumonia with unknown aetiology were also informed in Wuhan. The massive public movement at Chinese New Year escalated the epidemic outspread all over China, turning into a severe public health crisis, and deaths were also reported (Rehman et al., 2020). The Chinese government and researchers responded swiftly, and after intense etiological and sequencing investigation, it was concluded that the SARS-CoV-2 virus causes the ongoing viral pneumonia epidemic. On January 30, 2020, the World Health Organization (WHO) had stated it as a public health emergency, and later on, March 11 has announced it was a global pandemic (WHO Coronavirus Disease 2019 (COVID-19) Situation Report – 76, 2020). Therefore, the researcher's utmost priority was to trace the SARS-CoV-2 natural inhabitants' and origin to minimise health risk restricting the cross-species and human-to-human transmission. For genetic diversity understanding, systematic whole genome-based molecular phylogenetic analysis and comparative genomic studies revealed that SARS-CoV-2 belongs to Betacoronavirus genera conduced to concentrated pneumonia outbreaks. The phylogenetic analysis based on the full-length genome indicated that SARS/SARS-like CoVs are the eminent ancestor, including two Bat SARS-like CoVs (ZC45 and ZXC21) as adjoining relatives of SARS-CoV-2 (Rehman et al., 2020).
Moreover, full-length sequence analysis demonstrated a higher sequence resemblance (~96%) with RaTG13 identified from Yunnan Province far away from Wuhan, pointing towards a transitional host for decussating species barrier (Zhang et al., 2020; Zhou et al., 2020). Then pangolin-derived CoVs were also considered for the epidemic; however, human SARS-CoV-2 possesses a furin cleavage site that was not observed in the spike protein of both pangolin and RaTG13 CoVs. Furthermore, Rhinolophus malayanus isolated CoV (RmYN02) had insertions in spike protein share high genome homology (93.3%) was also believed as a probable predecessor for SARS-CoV-2 (Zhang et al., 2020).
Wuhan city as a transport hub station and connecting cities have a higher traffic volume connection with Wuhan. Public movement at the Chinese New Year causes the infected person to spread quickly throughout the country, resulting in an epidemic outbreak. The infection rate of COVID-19 was observed much more than SARS which took six months, while SARS-CoV took 54 days to spread throughout the country (Gundel, 2005); factors faced by China hindering the management of the initial COVID-19 cases were undefined aetiology, controlled release of information to the public, public anxiety, and backlash against restrictive movement measures. Additionally, the choice between dealing with viruses of unknown aetiology and nature and alleviating possible public panic in politically and culturally sensitive times contributed to lies and cover-ups (Shangguan et al., 2020). Weak capacities for the autonomous management of local health structures do not ensure timely response to crises. The privatisation of public hospitals contributed to a lack of public health resources to treat affected patients (Shangguan et al., 2020; Public Health Ontario Review of “The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020.”, 2020). So far (October 2021), Hubei Province was the hotspot of COVID-19 patients, with confirmed 96,410 cases and 4636 deaths (Table 1 ). Other provinces of China have a lower infection rate.
Table 1.
Province-wise distribution of COVID-19 cases, death, and case fatality rate till October 8, 2021, in China (Mainland).
| Division | Confirmed Cases | Deaths | Recovered | Case fatality ratio (%) |
|---|---|---|---|---|
| Hubei | 68,148 | 4512 | 63,627 | 6.62 |
| Guangdong | 1963 | 08 | 1922 | 0.4 |
| Zhejiang | 1291 | 01 | 1279 | 0.07 |
| Henan | 1288 | 22 | 1259 | 1.7 |
| Shanghai | 1277 | 07 | 1174 | 0.5 |
| Hunan | 1020 | 04 | 1015 | 0.4 |
| Anhui | 992 | 06 | 985 | 0.6 |
| Xinjiang | 980 | 03 | 952 | 0.3 |
| Heilongjiang | 949 | 13 | 936 | 1.4 |
| Beijing | 947 | 09 | 932 | 1 |
| Jiangxi | 935 | 01 | 934 | 0.1 |
| Shandong | 848 | 07 | 841 | 0.8 |
| Sichuan | 783 | 03 | 735 | 04 |
| Jiangsu | 676 | 0 | 666 | 0 |
| Chongqing | 589 | 06 | 582 | 1 |
| Shaanxi | 484 | 03 | 438 | 0.6 |
| Fujian | 461 | 01 | 423 | 0.2 |
| Hebei | 373 | 06 | 362 | 1.6 |
| Inner Mongolia | 307 | 01 | 282 | 0.3 |
| Tianjin | 289 | 03 | 266 | 1 |
| Liaoning | 288 | 02 | 280 | 0.6 |
| Shanxi | 218 | 0 | 213 | 0 |
| Yunnan | 217 | 02 | 209 | 0.9 |
| Gansu | 181 | 02 | 177 | 1 |
| Hainan | 171 | 06 | 165 | 3.5 |
| Jilin | 157 | 02 | 155 | 1.2 |
| Guizhou | 147 | 02 | 145 | 1.3 |
| Ningxia | 75 | 0 | 75 | 0 |
| Qinghai | 18 | 0 | 18 | 0 |
| Overall | 96,410 | 4636 | 90,677 | 4.8 |
Source: https://cn.bing.com/search?q=Coronavirus+statistics+in+China+(mainland).
Despite the dominant factor that elevates the spread of COVID-19 throughout the country, the Government of the Chinese took serious comprehensive and national response actions to combat the COVID-19 and has attained practical consequences based on empirical evidence. Some of the crucial strategies adopted by the government to reduce the COVID-19 epidemic are the following: i) Wuhan city that was the epicentre of the epidemic was first declared as a quarantine area and on January 23, 2020, ii) the quarantine radius was broadened to the other cities of Hubei Province, and up to January 30, 45 million individuals were quarantined (Du et al., 2020). iii) All public transportation, including subway, ferry, and bus services, was closed, and railway stations, expressways, airports temporarily shut down. iv) All new year celebrations and gatherings were cancelled. v) The incubation period of COVID-19 can last up to 14 days, so all the residents were self-quarantined in their homes to prevent the virus from the spread. vi) All public places such as restaurants, cinemas, shopping centres, and schools were closed, and staff of the community committees was deployed to distribute food, medicine, and medical supplies to all residents. vii) Two particular field hospitals Huoshenshan and Leishenshan hospitals, with a capacity of approximately 2400 beds, were constructed to provide the medical facilities (Shangguan et al., 2020). viii) To treat more than 14,000 suspected, mild, and close contact patients, all more critical sites, including convention centres and stadiums, were changed into 14 mobile cabin hospitals. ix) Additionally, in the epidemic area, the Chinese People's Liberation Army and other provinces dispatched medical teams of more than 42,600 medical staff to Hubei province to ensure to provide the medical facilities (Shangguan et al., 2020; Du et al., 2020). x) Digital technologies were also utilised to control the situation. Health codes were provided on widely used mobile apps Alipay and WeChat, and everyone was registered. The QR code colour showing red, yellow, or green indicate the health status of an individual. To enter or leave any community, assigned QR code scanning was made compulsory, which helped trace the route of confirmed cases and identify their close contact. These measures are indeed helpful to control the epidemic. xi) China Ministry of Education postpones the new semester opening time in kindergartens, primary and secondary schools, and universities on January 27. Internet technologies were used to reduce the delay in education, and virtual education platforms were introduced. Many Universities played a significant role in preventing and controlling the pandemic, opening up a free of cost educational platform for society (Wang et al., 2020b).
Conclusively, China's strict control actions have been evidenced to minimise the epidemic spread significantly. Furthermore, China provides result-oriented approaches that prove the best practices to reduce and eradicate the COVID-19.
3. COVID-19 morbidity, mortality scenario and associated risk factors in Bangladesh
Bangladesh, a densely populated country (with 162 million people and the eighth-most populous country in the world) of Southeastern Asia, is no exception and has already faced the devastating complexion in the health care system, daily social life and domestic economy (Rahman et al., 2020). The first official case of COVID-19 was confirmed in Bangladesh on March 8 with three positive cases (two men and one woman), of which those two men returned from Italy- the epidemic centre of COVID-19 at that time (Bangladesh Confirms First Case of Coronavirus, 2020). The 1st death (a 70-year-old male) was recorded on March 18, 2020 (Reuters Bangladesh Reports First Coronavirus Death -Officials, 2020). However, specialists speculated that the disease entered the country before those cases but could not be detected for adequate monitoring. After confirmed cases, the government tried to prevent the spread of COVID-19 by postponing all public gatherings, reducing international flights, imposing thermal scanner checking, shutting down educational institutions, ascribing 14 days of imperative quarantine to people coming from abroad, and deploying the army, among others.
Despite adopting all these measures, the spread of COVID-19 could not be controlled within Bangladesh. As of October 4, 2021, 9,794,490 COVID-19 tests were conducted in 146 laboratories throughout the country. By RT-PCR, GeneXpert, and Rapid Antigen tests, Bangladesh has confirmed 1,557,964 (15.91%) COVID-19 cases, accounting for 0.7% of total cases globally and 27,573 deaths having a 1.77% case fatality ratio (CFR). Of total COVID-19 cases, 0.7%, 1.77%, and 97.5% were recorded as active, death, and recovered cases, respectively. The epi-week 30 (July 26 to August 1) 2021 had the most weekly cases (99,693) and the most daily cases (16,230) with the epi-week 30. The highest weekly death (1736) occurred in week 31 (02–08 August) of 2021, with the highest daily death of 264 occurring on August 5th and 10th of that year. In division-wise, the highest COVID-19 reported death cases were recorded in Dhaka (58.9% and 43.6%, respectively). In contrast, both were lowest in the Mymensingh division (2.4% and 3.0%, respectively), though the Dhaka division revealed the lowest CFR (1.31%), whereas the Khulna division exhibited the highest CFR (3.18%) (WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update (MMWU), 2021) (Table 2 ).
Table 2.
Division-wise distribution of COVID-19 cases, death, and case fatality rate (World Health Organization, 2021. COVID-19 Bangladesh situation reports.
| Division | Cases | Deaths | Case fatality ratio (%) |
|---|---|---|---|
| Dhaka | 916,973 | 12,017 | 1.31 |
| Chottogram | 239,862 | 5589 | 2.33 |
| Rajshahi | 98,044 | 2028 | 2.07 |
| Khulna | 112,080 | 3564 | 3.18 |
| Sylhet | 54,140 | 1253 | 2.31 |
| Rangpur | 55,005 | 1354 | 2.46 |
| Barishal | 45,038 | 934 | 2.07 |
| Mymensingh | 36,822 | 834 | 2.26 |
| Overall | 1,557,964 | 27,573 | 1.77 |
However, many cases may be undetected in the country due to the utmost shortage of testing assays. The number of tests is pivotal to reveal the exact situation of COVID-19, especially death and recovery cases. Nevertheless, at the beginning of the COVID-19 outbreak, very few tests were performed to detect the cases with limitations and a severe scarcity of testing kits- that is why the positive results were under satisfaction at the initial stage. After passing the time, the number of testing was gradually increased, but in recent times, it decreased again.
As per the WHO report on COVID-19 in Bangladesh, till August 30, 2021 (WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update (MMWU), 2021), the male showed higher confirmed (67%) and death (65%) cases compared to female (33% and 35%, respectively), the case fatality ratio (CFR) for males was higher than females. This gender variation in COVID-19 cases may be due to the cultural activities of males in Bangladesh. In Bangladesh, males mainly dominate outdoor activities and have to communicate with almost every class of people, demonstrating males as more vulnerable to COVID-19 than females. However, similar kinds of variations in the number of COVID-19 affected males and females globally. Variations in the immune system can illustrate this divergent risk comparatively higher in males than females. The female immune system may have an edge to detect pathogens slightly earlier. In addition, women show comparatively higher innate and adaptive immune responses than men because of having a high density of immune-related genes in the X chromosome (Griffith et al., 2020; Sharma et al., 2020).
Furthermore, SARS-CoV-2 viruses use SARS-CoV receptor angiotensin-converting enzyme 2 (ACE2) to enter the host cell, and men contain higher ACE2 than females. Therefore, males may be more vulnerable to COVID-19 than females (Mukherjee and Pahan, 2021; Jackson et al., 2021). In addition, smoking habits also might make men susceptible to COVID-19. Some scholars believe the prevalence of COVID-19 in Chinese men was higher than among women because the smoking rate among Chinese men was much higher than among women (Underner et al., 2020).
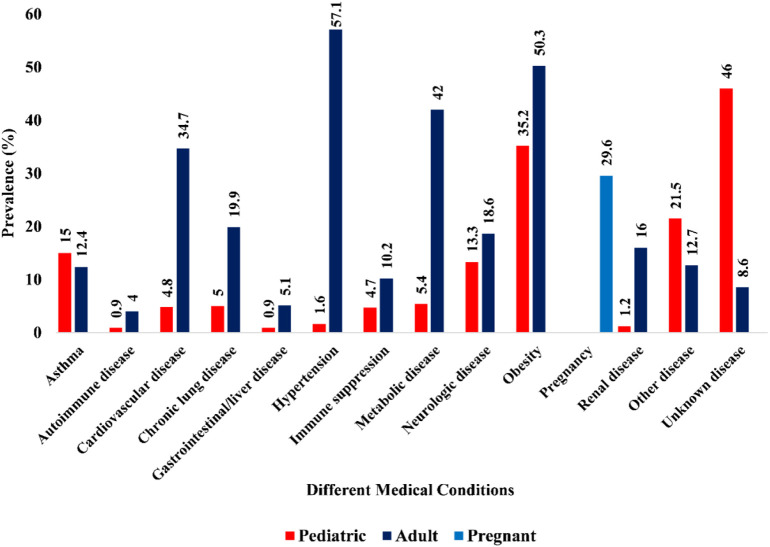
Considering the age-wise distribution, children and older adults were less infected compared to other age groups and the death rate augmented with age. The age group of 25–34 years accounts for the bulk of COVID-19 cases (24%), followed by 23% for the group of 35–44 years, 17% for 45–54 years, 12% for 55–64 years, 10% for 15–24 years, 7% for 65–74 years, 4% for 14 years and below, and the remaining 3% in the age group of 75 and above. The age group 65–74 years accounts for 30.5% of all recorded deaths, followed by 55–64 years (25.4%), 75–84 years (14.5%), 45–54 years (14.1%), 35–44 years (6.5%), 85 years and above (5.1%), and under 35 years (4%) (WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update (MMWU), 2021). Comparatively less infection in child and older people maybe because of staying at home mostly. On the contrary, more death in the older group may be associated with less immune system function. Most of this group has comorbidities like diabetes, high pressure, low lungs and kidney function, and other chronic diseases (Fig. 1 ).
Fig. 1.
Cases of COVID-19 associated with different medical conditions. Data are included from March 1, 2020, to August 31, 2021 (CDC Laboratory Confirmed COVID-19 Associated Hospitalizations, 2021).
The frontline COVID-19 fighters, e.g., physicians, medical staff, nurses, polices, journalists, law enforcement officers, judiciary members, the army, and others, were infected (more than 20,000) with the SARS-CoV-2 the rampant run of the current pandemic situation. As of May 3, 2021, a high CFR (5.36%) was revealed within frontline doctors. However, the number of death of nurses and medical staff could not be recorded. The highest number of doctors affected were recorded in Dhaka (852) districts, followed by Chittagong (492) and Sylhet (349) districts. In addition, 812 nurses and 471 medical staff were infected in Dhaka city with the COVID-19 (Bangladesh Medical Association District Wise Total Number of Affected Doctor, Nurse, and Staff (COVID 19 +), 2021). Police headquarters' data showed that most police were affected in Dhaka Metropolitan Police (2330) among 11,431 infected cases. In addition, more than 11,500 police members were in quarantine, with 4781 isolated cases and 7463 recovered cases (DhakaTribune Covid-19 Battering Frontline Fighters in Bangladesh, 2020).
Bangladesh is at risk with rising non-communicable diseases (NCDs) like which accounts 67% of total deaths (cardiovascular diseases- 30%, cancers- 12%, chronic respiratory diseases- 10%, diabetes- 3% and other NCDs- 12%); only 26% and 7% of total deaths occur due to communicable and injuries, respectively, (WHO Noncommunicable Diseases (NCD) Country Profiles, 2018). However, these NCDs are playing a pivotal role in the morbidities due to COVID-19. Moreover, a person having multiple comorbidities who have COVID-19 is at greater mortality risk. NCDs, e.g., heart diseases, hypertension, diabetes, chronic obstructive pulmonary diseases, malnutrition, among others, contribute to COVID-19 in Bangladesh (Al Mahtab et al., 2020). In Bangladesh, 48% of males smoke, which is a significant factor for severe COVID-19 by damaging the lungs severely and affecting other parts of the body (WHO COVID-19 and NCDs, 2020). In addition, about 50% of aged Bangladeshis hold multiple comorbid conditions that have potentialities to put them at high risk for the severe form of COVID-19 (Hossain et al., 2015).
Furthermore, 26% and 62% of aged Bangladeshis are facing malnourished and at risk of malnutrition conditions, respectively, (Ferdous et al., 2009) that also reveals them at risk for COVID-19. With the augmentation of the number of COVID-19 patients, the healthcare system of Bangladesh faced a worse situation and reached the brink of collapse. The hospitals and clinics become the source of the transmission of COVID-19 through the infected patients to another healthy person who visits for treatment purposes. In addition, the increasing COVID-19 morbidities reveal the scarcity of ICU, ventilator supports, and oxygen cylinders in the communities and rural clinics (Haque, 2020). In the initial stage of the COVID-19 outbreak, the policymakers and health professionals lack the coordination that results in the expansion of COVID-19 into the community level. With the outbreak of COVID-19, the Bangladesh government tried to tackle the spread of the disease by postponing mass gatherings. However, several mass gatherings have been ensued in the amid of COVID-19 juncture, e.g. occurring of special prayer Raipur in Lakshmipur district with more than ten of thousands of people; voting in three constituencies (Dhaka city, Pabna, and Naogoan) of the national parliament; celebrating different religious festivals; attending of more than hundreds of thousands of people in the funeral of famous persons without taking any protective measures; travelling to tourist sites, among others (Axios Thousands in Bangladesh Gather at Funeral despite Coronavirus Lockdown, 2020; Anadolu Agency Bangladesh to Hold 3 By-Elections amid Pandemic, 2020). In addition, thousands of government and non-government service and readymade garment factory workers from northern and southern Bangladesh returned to their workplace, especially in Dhaka city, Gazipur, Narayanganj, Chittagong, ignoring their lives and the outbreak of COVID-19. Furthermore, the expansion of local markets helped to spread COVID-19 at the community level.
Robust implementation of the strict protocol for social distance was not possible by Bangladesh Government, as millions of people all over the country, particularly in Dhaka, had to come out for their basic needs. Social distance protocol recommended by WHO could not be maintained during public transportation, gathering in public offices and banks, living in slums. Dhaka city, the capital of Bangladesh, has about 20 million populace, and it is designated as the epicentre of the COVID-19 pandemic in Bangladesh. More than 1 million slum possessors and marginal communities reside in the city's vicinity who lack adequate hygienic management, especially toilets/bathrooms and water facilities. That is why these facilities have to be shared within several families (Anwar et al., 2020) and thus probably allowing the spread of COVID-19 among them rapidly. A recent cross-sectional epidemiological study in Dhaka city was conducted by the Institute of Epidemiology, Disease Control and Research and the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDRB,B). The study revealed that 45% of people, including 74% slum dwellers, hold COVID-19 antibodies (The Daily Star 45% of Dhaka Dwellers Exposed to Covid-19, IEDCR Survey Says, 2020). However, enforcement of social distance law is almost impossible in high density.
4. COVID-19 morbidity, mortality, and associated risk factors in India
In the middle of October 2020, more than 7.8 million people were infected due to COVID-19 in India. India is the second-largest affected country in the world). Nearly one percentage (0.6%) of the population was infected with this virus among the total population. The disease's morbidity and mortality pattern depend on population density, comorbidities, mode of transmission, nature of the virus, and environmental condition (Transformingindia, 2021).
4.1. Population density and COVID-19 cases
The density leads to closer contact and more interaction among residents, making them potential hotspots for the rapid spread of emerging infectious diseases (Hamidi et al., 2020). According to Census 2011, the average population density in India is 382 km2. The states of Maharashtra (20.9%), Andhra Pradesh (10.2%), Karnataka (10.2%) and Tamil Nadu (9.0%) share 50% of confirmed cases and 60.4% of COVID-19 deaths in India. The state of Maharashtra shares 36.5% of deaths among the national total (Https://Www.Worldometers.Info/Coronavirus/Country/India/, 2020). The population density in these states is above the national average. Further, in India, higher mortality has been noted in densely populated cities such as Mumbai, Delhi and Chennai compared with the smaller urban centres.
4.2. Comorbidities and mortality
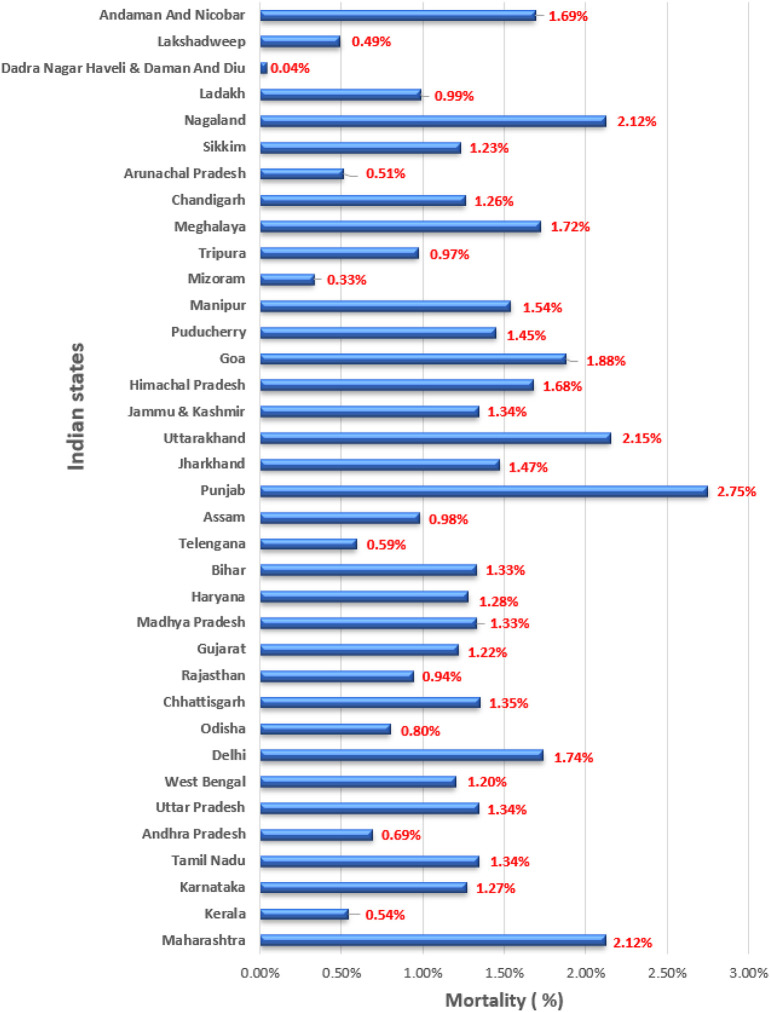
India, unfortunately, has a high burden of non-communicable diseases (NCDs), especially heart diseases, Diabetes and Respiratory diseases. The study in 2017, “India: Health of the Nation's States”, also revealed that among the total deaths observed, 61.8%, 27.5% and 10.7% were NCDs, communicable diseases and injuries, respectively, in India (ICMR Disease Burden Trends in the States of India 1990 to 2016, 2017). Comorbidities and conditions that have been commonly observed in COVID-19 patients in India include hypertension, diabetes, heart disease, asthma, chronic obstructive pulmonary disease (COPD), low immunity, malignancy, bronchitis, and chronic neuromuscular disease, among others (Singh et al., 2020). “The health ministry's analysis also shows that 53% of the COVID-19 cases were aged 60 years and above, notably elderly people and those with comorbidities are at higher risk of mortality. The WHO reported that globally, the highest percentage of cases had been reported in the 25–39 age group, with approximately 50% of cases in the 25–64 age group. However, the percentage of deaths increases with age, and approximately 75% of deaths are in those aged 65 years and above. The state wise mortality was shown in Fig. 2 .
Fig. 2.
Details of Indian state-wise percentage of morality due to COVID-19 as of 06.10.2021 (Source: https://www.mygov.in/covid-19).
4.3. Environmental conditions
A more significant number of COVID-19 infections started to spread from March 2020. The Government of India has implemented the nation wise lockdown on March 24 and extended it up to August 2020. Most Indian states are summer (April to June) and monsoon (July to September). Nowadays, the lockdown has withdrawn all the states of India (Indian TV-News India TV News. Looking at Gradual Withdrawal of Lockdown, 2020), and most of the Indian states started to receive the monsoon. This favourable situation may support the virus spread in India.
4.4. Epidemiological factors
The estimated population of India in 2020 is 1,380,004,385, according to UN data. India population is equivalent to 17.7% of the total world population, and it is the second-most populous country after China. The Indian state-wise mortality and morbidity data were collected up to October 15, 2020, from the Ministry of Health, India (Ministry of Health and family Welfare, Government of India, 2021). The state-wise total population, male population, female population, density per sq. km, population above 60 ages, number of literates, number of public-private hospitals, number of literates, persons below the poverty line, Per capita income at constant-current prices, religion, number of vegetarian, non-vegetarian persons, number of tobacco smoker and the number of alcohol drinkers. The data were checked for normality by the Shapiro-Wilk test, and the Spearman correlation analysis determined the relationship between COVID-19 cases, deaths, and epidemiological factors. The correlation coefficients are measured from −1 to +1, and the sign of the Spearman correlation indicates the relationship between the analysed variables. The COVID-19 cases showed a significant positive correlation with total population (r = 0.65, p < 0.001), population of male (r = 0.64, p < 0.001), population of female (r = 0.66, p < 0.001), number of persons above 60 years (r = 0.35, p < 0.05), number of literatures (r = 0.72, p < 0.001), population below poverty line (r = 0.41, p < 0.05) and number of private hospitals (r = 0.42, p < 0.05). Similarly, COVID-19 mortality showed a significant positive correlation with total population (r = 0.52, p < 0.01), population of male (r = 0.51, p < 0.01), population of female (r = 0.52, p < 0.01) and number of literatures (r = 0.60, p < 0.001).
Despite the vast population, India effectively controlled the spread by adopting lockdowns and relaxation the lockdowns in a phased manner. Indian media also came hand in hand with the government and sensitised the people about regular hand washing, compulsory masks, and avoiding crowded places. Strict regulations for interstate and intra-state movement also helped reduce the COVID-19 spread. Further, India efficiently managed the vaccination programme for a larger population of people, one of the most extensive vaccination drives of a kind. The Indian healthcare system was given a red alert to handle the COVID-19 case, and special wards were established. By adopting the intelligent strategies, India efficiently reduced the COVID-19 spread and related deaths.
5. COVID-19 morbidity, mortality, and associated risk factors in Pakistan
The Islamic Republic of Pakistan is in Southern Asia that has a multi-cultural and ethnic society that hosts one of the youngest, largest refugee populations (Afghanistan). Despite its proximity with China, it remained Coronavirus-free until February 26, when a young man from Karachi (metropolitan city of Pakistan) tested positive after returning from Iran. After a brief hiatus following the first case, COVID-19 cases spiked as more pilgrims returned (Iran and Saudi Arabia) tested positive for the virus (Abid et al., 2020). According to statistics by the National Command Operation Centre (NCOC), Pakistan (Government of Pakistan, n.d.), COVID-19 patients soared past 105,839 with 930 (0.87%) cases in Islamabad, 434,139 with 12,724 (2.93%) cases in Punjab, 461,258 with 7451 (1.61%) cases in Sindh, 175,012 with 5608 (3.20%) cases in KPK, 33,004 with 349 (1%) cases in Balochistan, 10,338 with 186 (1.80%) cases in GB, 34,278 with 738 (2.15%) cases in AJK (Table 3 ).
Table 3.
Province-wise distribution of COVID-19 cases, death, and case fatality rate till October 6 2021.
| Division | Cases | Deaths | Case fatality ratio (%) |
|---|---|---|---|
| Islamabad | 105,839 | 930 | 0.87 |
| Punjab | 434,139 | 12,724 | 2.93 |
| Sindh | 461,258 | 7451 | 1.61 |
| KPK | 175,012 | 5608 | 3.20 |
| Balochistan | 33,004 | 349 | 1 |
| GB | 10,338 | 186 | 1.80 |
| AJK | 34,278 | 738 | 2.15 |
| Overall | 1253,868 | 27,986 | 2.23 |
According to the data collected, Pakistan appeared to pass the Coronavirus peak in mid-June of 1st episode. However, fewer cases have been reported daily since August started. The cases have attributed the curve's flattening to a combination of successfully targeted lockdowns by the government and pre-existing immunity in the population. There might, however, be small spikes in cases till October 15, 2020.
The distribution of COVID-19 in Pakistan is heavily concentrated in a few key cities. The city of Karachi (as of September 5, 2020) has recorded about 84,000 confirmed cases, making up about 28% of all cases of COVID-19 in Pakistan. Meanwhile, Lahore, the country's second-largest city, has recorded (as of September 52,020) 49,000 cases of COVID-19, making up about 16% of the country's cases. Islamabad Capital Territory and Peshawar District also have both recorded over 10,000 cases. Karachi, Lahore, Islamabad, and Peshawar account for about 163,000 cases, which make up nearly 55% of the country's total confirmed cases.
Further, in Pakistan, higher mortality has been noted in densely populated cities such as Karachi, Lahore, and Islamabad than in the smaller urban centres. The health experts said that women had less exposure to gatherings than men as they did not contract the infection more than males. It is also reported that COVID-19 killed fewer women than men (Scavone et al., 2020). Some reports also said that not only among ordinary people but the number of positive cases and deaths was also higher among male health workers as compared to female health workers (Dawn Covid-19 Kills More Men than Women in KP: Report, 2021). Since the advent of the epidemic, 2481 healthcare providers have got an infection in the province, including 1810 men and 671 women (Government of Pakistan, n.d.). They considered causes that include less exposure of women to crowded places, such as congregations, jobs, and hormonal effects. In Pakistan may be fewer causes of COVID-19. Females have different hormones than males, providing them safety against Coronavirus and heart attack (Foresta et al., 2021). Some people believe that as compared to men, women wore a veil, which acted as a facemask, so they have fewer Corona cases in Pakistan. Except to all, adherence to social distancing measures, hand-washing and wearing masks are the main precautions against COVID-19. All people, including men, women, transgender people and children, should follow the standard operating procedures (Ozaslan et al., 2020). A few vulnerable factors faced by Pakistan that caused hindrance to managing the COVID-19 were undetermined aetiology, which results in depression, hostility, and high anxiety-like negative psychological behaviour among the public.
Furthermore, strict government policy to control the information led the people unaware of COVID-19, and the public was remained improvised. Additionally, the choice between dealing with viruses of unknown aetiology and nature and alleviating notorious public panic in politically and culturally sensitive times leads to lies and cover-ups (Ozaslan et al., 2020; Junejo et al., 2020; Junejo et al., 2021; Battegay et al., 2020). Weak capacities for the autonomous management of local health structures do not ensure timely response to crises. Eventually, the privatisation of many public hospitals leads to a lack of public health resources to treat affected patients (Junejo et al., 2021; Battegay et al., 2020). Other essential factors that came under a critical lens in Pakistan, such as religious, political, health, sports and unemployment, should be discussed here. Starting from C, returning followers from Iran, a Tablighi Jamaat religious gathering and prayer congregations could cause concern due to their potential to exacerbate the outbreak in the country. However, sops were followed during five-time prayers later, and hence there was no spike in the cases reported. In a report on June 16, at least 97 members of national and provincial assemblies across political lines tested positive for COVID-19, and six of them succumbed to death (Arab News “Virus Infects 97 Politicians in Pakistan”, 2021). The situation gradually worsened, and the Government of Pakistan announced a Rs 2.5 trillion loss due to the COVID-19 in April 2020. After a short break, the government started to uplift the ban on many exports, including Afghan and China, after taking COVID-19 measures. When we saw the doctors and co-workers, COVID-19 also infected healthcare workers and co-workers in Pakistan, and the ratio is so high (Khalid and Savaiz, 2020). Fears of COVID-19 did not stop in sports that suspended the last two essential matches of Pakistan Super League (PSL) 2020 and other sports. Moreover, The COVID-19 is considered the most significant factor causing the unemployment rate to increase, particularly daily wage workers. Pakistan estimates that the unemployment will reach 6.65 million in the 2020–2021 fiscal year, compared to the previous fiscal year) (Government of Pakistan, n.d.).
Eventually, a second wave of the pandemic exploded, according to the authorities, on October 28, 2020. The ground was all set for such a situation in Pakistan (Ali et al., 2020). However, the terrifying slice is that circulation of the SARS-CoV-2 will not stop here, and COVID-19 can probably become a source of persistent infection. The first wave claimed 6795 lives, infected 332,186, left behind 632 on ventilators and suffered millions. Now we must watch the fourth episode. It just started in the country on June 25, 2021, and now has subsided after an intelligent lockdown in the various cities of Pakistan.
6. COVID-19 morbidity, mortality, and associated risk factors in Iran
In Iran, the number of positive cases or patients with COVID-19 diagnosed based on PCR test from January 3, 2020, to October 12, 2021, is about 5,716,394 people (WHO Novel-Coronavirus-2019, 2020). The number of recovered patients among the total Covid cases in Iran has reached 5,593,526 by October 12, 2021 (WHO Novel-Coronavirus-2019, 2020). Though the total number of recovered patients still seems acceptable; Because of not considering the protocols, social distances in public gatherings (at least 2 m (WHO Novel-Coronavirus-2019, 2020)) and also not wearing a three-layer mask; some irresponsible people of the community have had the worst effect on this pandemic in Iran. Also, because of the genetic mutation of the COVID-19 virus, unfortunately, from the beginning of the pandemic, from Februray19,2020 in the city of Qom to October 12, 2021, 122,868 people in the whole country have died. Since the mortality rate among all positive cases was 2.14% on October 12. According to WHO, 97.85% of people have recovered until October 12, 2021. The number of recoveries has reached 5,593,526 (WHO Novel-Coronavirus-2019, 2020) in Iran; it is hopeful of anticipating a more significant number of recoveries, considering the efforts of medical staff working in hospitals. Of course, the public closure of the bazaar (excluding pharmacies and grocery stores and hospitals) for at least 2 weeks in the cities which have the highest restrictions, such as Tehran and hospitalising patients in independent places such as hotels and places reduced the possibility of contact between the patients and healthy. Considering other principles, will be effective in managing the “Corona pandemic”. So, according to the above description, extreme health care and the quarantine are the most important duties for the community. The percentage of deaths among the total number of definite patients in Iran is equal to 2.14%. Alliance and taking the social distances seriously, also effective vaccination, are the keys to success in controlling the global pandemic of this virus. Of course, it should be noted that more than 200 million people in all countries of the world have been infected with “corona” so far. Over 190 million of these patients have recovered; therefore, the pandemic peak has been successfully controlled in most countries and Iran.
7. COVID-19 morbidity, mortality, and associated risk factors in Turkey
Turkey is a large, roughly rectangular peninsula that bridges southeastern Europe and Asia. The year 2020 opened a new chapter in the history of this region when a man who had returned to Turkey from Europe tested positive on March 11, 2020 (Genç, 2021). On October 6, 2021, the updated COVID-19 situation of Turkey has 7,296,879 confirmed cases, 6,751,667 recoveries, and 65,137 deaths (Worldometer). The rapid increase of the confirmed cases in Turkey did not overburden the public healthcare system (DW News, 2020), and the preliminary case-fatality rate remained lower than in many European countries (Hasell et al., 2020). Discussions mainly attributed these to the country's relatively young population and the high number of available intensive care units. However, sociological aspects such as dietary similarities can also play a role in the population response to the pandemic. The COVID-19 in these countries was compering to others in the world (especially to GI symptoms).
8. COVID-19 morbidity, mortality, and associated risk factors in Egypt
By October 9, 2021, 310,745 cases of COVID-19 and 17,619 deaths had been reported in Egypt (WHO Coronavirus Disease 2019 (COVID-19) Situation Report – 76, 2020). The Egyptian Ministry of Health confirmed the first case of SARS-CoV-2 in the country on February 14 at Cairo International Airport involving a Chinese tourist. Egyptian authorities notified the WHO, and the infected person had been placed in isolation at the hospital. Strict control measures were subsequently applied to monitor those who came into close contact with the Chinese person where the others tested negative for COVID-19 (Breaking: Egypt Reports First Case of Coronavirus, 2020). In late February, multiple foreign cases associated with travel to Egypt showed symptoms of SARS-CoV-2, including two persons from the United States and two persons from Tunisia. On March 1, 2020, Egypt recorded the second case of SARS-CoV-2 (Egypt Detects Second Case of New Coronavirus: Health Ministry, 2020). On March 6, the Egyptian government and WHO announced 12 new cases of COVID-19 among Egyptian workers on Nile cruise ships travelling from Aswan to Luxor (Twelve Asymptomatic Coronavirus Cases Registered on Nile Cruise Ship, 2020). All those workers who tested positive for COVID-19 did not show any signs of the disease. According to the molecular analysis, the virus source was from a Taiwanese-American woman on the ship (Egypt-Nile-Coronavirus, n.d.).
Some authors stated that older age and elevated serum ferritin were significant risk factors for severe COVID-19 among Egyptian patients. Bacterial co-infection and multidrug resistance among patients with COVID-19 in Upper Egypt are common. The climate (higher temperature and low humidity) may significantly decrease the infection rate with COVID-19. In Upper Egypt, the higher temperature and low humidity of the climate caused a decline in the infection rate of COVID-19, especially in spring and summer compared with other countries worldwide with a high incidence of COVID-19 (Medhat and El Kassas, 2020). BCG vaccination has been included as a compulsory vaccination program since 1974. According to this theory, the relatively low rates of COVID-19 infections and mortalities in Egypt may be partially attributed to the country's early intake of BCG vaccination (Medhat and El Kassas, 2020). Mostafa et al. (2020) found that breast milk samples from the COVID-19–positive mothers after the first lactation were negative for the virus. The authors stated that breastfeeding is effective against infectious diseases because it strengthens the immune system by transferring antibodies from the mother and other anti-infective factors; therefore, all confirmed or suspected COVID-19 mothers with any symptoms should follow standard infant feeding guidelines with appropriate precautions (Breastfeeding Advice during the COVID-19 outbreak, n.d.).
Some studies (Abdel Wahed et al., 2020) assessed the Egyptian Health Care Workers' knowledge, attitudes, and perception regarding COVID-19. Unavailability of personal protective equipment (PPE), fear of transmitting the disease to their families, and social stigma were the most frequently reported reasons for increased risk perception. The first case of death in Egypt was recorded on March 8, 2020. Many COVID-19 deaths (˃30 cases) during the first wave in Egypt were recorded between May 29–August 2, 2020, and the highest daily reported death cases were recorded on June 27, 2020. The case fatality rates have elevated from 5.7% in the third week of March to reach 8.5% in the second week of April, followed by a slow decline to 2.6% in the fourth week of May. The first week of August showed the highest fatality rates of 15.1%, which decreased to 9.9% at the end of August. Fluctuation in the fatality rates was recorded from September to October, with the highest rate (13.9%) in the third month of September and the lowest rate (7%) in the fourth month of October. Again, fluctuation in the fatality rates was recorded over the period from December 2020 to September 2021.
Recently one study (Ramadan et al., 2020) reported that older age has contributed to COVID-19 severity among Egyptian patients compared to children in terms of contracting the virus and the fitness of the immune response. People older than 53 years were significant factors associated with increasing the risk of COVID-19 severity and mortality among Egyptian patients (Ramadan et al., 2020; Khamis et al., 2021). Females have a more robust immune response than males, and due to this phenomenon, they have low susceptibility to viral infections (Safdar et al., 2021). The risk assessment revealed no significant association between gender and COVID-19 severity and mortality among Egyptian patients (Ramadan et al., 2020; Khamis et al., 2021). Psychological distress during the COVID-19 pandemic is a gender-related factor which female Egyptian physicians were at higher risk for developing psychological distress during the COVID-19 pandemic (Sehsah et al., 2021). Obesity is also associated with increased mortality among COVID-19 Egyptian patients (Khamis et al., 2021), but there is no significant association between smoking and COVID-19 in the studied Egyptian patients (Ramadan et al., 2020; Khamis et al., 2021). There is also the relationship between job and COVID-19, and the most frequently reported reasons for increased risk perception were fear of transmitting the disease to their families and social stigma (Abdel Wahed et al., 2020). Among Egyptian physicians, chronic diseases (Sehsah et al., 2021) and comorbidities (El-Sokkary et al., 2021) are potential risk factors associated with COVID-19. Diabetes mellitus, hypertension, ischemic heart disease, chronic kidney disease, chronic obstructive pulmonary disease, other chronic diseases were significant risk factors associated with COVID-19 severity and mortality among Egyptian patients (Khamis et al., 2021).
9. Factors contributing to a low mortality rate of COVID-19 in South Asia and Africa
South Asia and Africa constitute many countries that are developing in nature. It is to be noted that there are genetically and antigenically related SARS-CoV-2 viruses that might already exist among animals and humans. Therefore, there may be a possibility that the people in these countries might have been already exposed to mild, non-SARS-CoV-2 viruses that can stimulate immunity against SARS-CoV-2. Due to cross-immunity, contact with domestic animals, low water quality, low food quality and other personal practices might have been a few reasons for infections due to non-SARS-CoV-2 viruses. Non-SARS-CoV-2 viruses that share antigens with virulent SARS-CoV-2 viruses might be present in contaminated air, water, food, and domestic animals. These environmental factors in the developing countries of South Asia and Africa might have been acted as the primary source for infection with non- SARS-CoV-2 viruses. African region showed significantly low COVID-19 cases and deaths. Several researchers have already established that SARS-CoV-2 like viruses already existed in these communities.
10. COVID-19 morbidity, mortality, and associated risk factors in Central-Eastern Europe
Central-Eastern Europe is a broad and not precise term that cannot be easily defined based on historical, sociological, or economic criteria. Countries of this part of the world share many similarities yet remain different. The year 2020 opened a new chapter in the history of this region, revealing the unknown aspect of their similarity–the population response to the COVID-19 pandemics. The pandemic outbreak in Western Europe started and progressed with many mortal cases and the paralyses of health services. The Central and Eastern part of the continent also reported thousands of cases, but, fortunately, without such horrific mortality. This fact is a topic of the scientific debate worldwide trying to explain the cause of this observation. The number of infections and deaths in countries of Central-Eastern Europe is shown in Table 4 .
Table 4.
Distribution of COVID-19 cases, death, and case fatality rate in Central-Eastern Europe till October 6, 2021.
| Country | Cases | Deaths | Case fatality ratio (%) |
|---|---|---|---|
| Bosnia and Herzegovina | 238,458 | 10,802 | 4.53 |
| Bulgaria | 511,666 | 21,320 | 4.17 |
| Belarus | 549,817 | 4228 | 0.77 |
| Croatia | 411,917 | 8722 | 2.12 |
| Czechia | 1,696,016 | 30,485 | 1.80 |
| Estonia | 160,832 | 1383 | 0.86 |
| Greece | 668,811 | 15,012 | 2.24 |
| Hungary | 825,799 | 30,253 | 3.66 |
| Latvia | 164,801 | 2773 | 1.68 |
| Lithuania | 342,827 | 5134 | 1.50 |
| Macedonia | 193,458 | 6758 | 3.49 |
| Montenegro | 133,767 | 1965 | 1.47 |
| Poland | 2,914,962 | 75,774 | 2.60 |
| Kosovo | 160,195 | 2954 | 1.84 |
| Moldavia | 301,431 | 6927 | 2.30 |
| Romania | 1,303,900 | 38,260 | 2.93 |
| Serbia | 981,329 | 8531 | 0.87 |
| Slovakia | 419,473 | 12,697 | 3.03 |
| Slovenia | 298,270 | 4597 | 1.54 |
| Ukraine | 2,482,518 | 57,526 | 2.32 |
Data suggest the disproportion between the high cumulative number of cases with infection and low death number. This observation suggests certain factors that promote effective transmission of the virus and low mortality from COVID-19. Indeed, there cannot be one aspect that leads to these observations, but the explanation might be a mix of a few hypotheses (Jurgiel et al., 2020). To those having the most significant impact, we should include:
-
•
The younger age of the population; the countries of this region have younger ages of the population compared to the age in Western Europe.
-
•
Economic structure: most people of the region work in the first and second sectors (industrial, agricultural, manufacturing). Mines, factories, or big agricultural farms are crowding places, thus promoting a spread of COVID-19.
-
•
The spread rate of COVID-19 heavily depends on population density, which is medium or low in some Central-Eastern European countries
-
•
The high air pollution: Central and Eastern Europe are the most polluted, promoting the easier spread of the virus.
-
•
The high rate of vaccination, extensive use of attenuated vaccines, such as OPV and BCG immunization (some studies suggest it can have a protective effect, influencing the low mortality).
-
•
Genetic polymorphisms lower the vulnerability to infection.
-
•
An initial strain of the virus
-
•
Climate factors
There are also seemingly trivial hypotheses, which can shed light on the similarity of Centro-European countries. Sociological aspects such as dietary similarities can also play a role in the population response to the pandemic. All countries of Central and Eastern Europe are well-known due to the products prepared from fermentation; the most popular dish, Sauerkraut exists in every language (Polish: kapusta kwaszona, Belarusian: квашаная капуста). The influence of lactic acid bacteria on the proper functioning of the immune system is well-known. Some suggest that it might play a protective role via modulation of the gut microbiota and immune system, especially in cell-induced response. It might affect the symptoms of the COVID-19 in these countries compering to others in the world (especially to GI symptoms).
Lately, we have observed a rapid increase in the number of cases and deaths in Central-Eastern Europe, referred to as the second wave of the pandemic. Those changes result from many factors, mainly due to the appearance of the new strain of the virus, the collapse of national health services, and the paradoxical effect of an initial low percentage of the infected population. The new SARS-CoV-2 variant from B.1.1.7 lineage with its higher transmissibility spread rapidly in Central-Eastern Europe during the third wave, causing a rampageous increase in the infections. That process was even more efficient in the nation, with such a low immunized population spared at the pandemic's beginning. The rise in hospitalization resulted in the collapse of the national health services, which are in the majority under-financed in Eastern-European countries. This situation deprived numerous patients of the proper medical help and led to the inglorious “record number” in mortality.
For October 2021, the number of infections and deaths rises in Central-Eastern Europe, determining the 4th wave of the pandemic. Similarly, to the previous waves, the rise is caused by the new variant – Delta, which analogously to B.1.1.7 lineage, has a higher spreadability. However, due to the vaccination and natural immunization of the population, the increase in infections and deaths has slower dynamics.
Therefore, we highlight that even in the population attributed to protection factors, there is still a need for an appropriate and strict approach to the pandemic. The strategy of 3 T's – Test, Treat, Track – should not have been eased, even in fortunate moments of epidemiological stabilization.
The SARS-CoV-2 pandemic affected Central-Eastern Europe differently in each of the waves. Firstly, with high morbidity and low mortality, due to the possible protecting factors of the population. However, the second and third waves had utterly different, horrific courses resulting from the new variant and the failure of the health systems overwhelmed by unprecedented numbers of patients. The ongoing situation and the future of the pandemic are unknown, yet the vaccination remains our hope for the come-back to everyday life.
11. COVID-19 and associated risk factors in Brazil
So far, Brazil has 21.499.074 confirmed cases of COVID-19 and 598.829 deaths. If analyses by region, the southeast has the highest number of reported cases and deaths (39.1% and 47.4%, respectively), followed by the regions northeast (22.3% and 19.5%, respectively), south (19.3% and 15.6%, respectively), midwest (10.6% and 9.6%, respectively) and north (8.6% and 7.8%, respectively) (Brasil Coronavírus Brasil COVID-19, 2021). The southeast region has the highest CFR (3.38%), while the South region has the lowest CFR (2.25%) (Table 5 ).
Table 5.
Division-wise distribution of COVID-19 cases, death and case fatality rate (Brasil Coronavírus Brasil COVID-19, 2021).
| Division | Cases | Deaths | Case fatality ratio (%) |
|---|---|---|---|
| Southeast | 8.407.378 | 284.281 | 3.38 |
| Northeast | 4.803.969 | 117.049 | 2.44 |
| South | 4.159.429 | 93.615 | 2.25 |
| Midwest | 2.281.330 | 57.329 | 2.51 |
| North | 1.846.968 | 46.555 | 2.52 |
| Brazil | 21.499.074 | 598.829 | 2.79 |
The Ministry of Health has published the Guidelines for Diagnosis and Treatment of COVID-19, which contains general measures to prevent and combat infection caused by SARS-CoV-2. Among the measures, we highlight hand washing, wearing a mask, social distance, respiratory etiquette and food security (Secretaria de Vigilância et al., 2020). Unfortunately, although several measures have been implemented, Brazil appears as the third country with the most reported cases, behind only the United States of America and India (WHO Index @ Covid19, 2020).
To establish possible causes of the number of confirmed cases in the country, we first need to consider a territorial extension. Brazil possess 8,510,820,623 km 2 (Instituto Brasileiro de Geografia e Estatística (IBGE), 2019) with a population estimated at 210.147,125 (Brasil, 2019) in the year 2019.
As it is a continental country, the pandemic develops in conditions closely linked to regionality. Issues such as demography and geography of the region, access to basic sanitation and hygiene items, the structure of the local health system, number of unemployed people or informal workers and the economy must be taken into account in each region and city, individually. In addition, political issues and corruption make it difficult to control the pandemic. Regarding the basic sanitation in the states, the average rate of urban service by water network indicates values above 90% in the Federal District and in 18 states, namely, Paraná, Roraima, Mato Grosso do Sul, São Paulo, Tocantins, Mato Grosso, Goiás, Rio Grande do Sul, Santa Catarina, Piauí, Bahia, Sergipe, Rio de Janeiro, Minas Gerais, Paraíba, Rio Grande do Norte, Espírito Santo, and Pernambuco. In the range of 80% to 90%, Alagoas and Amazonas appear; in the range below, between 60% and 80%, the states Ceará, Maranhão, Acre and Rondônia appear; and in the penultimate range, from 40% to 60%, are Pará and Amapá. The last has an urban water service index equal to 40.4% in 2017. The average urban service index with sewage collection network points to above 70% only in the Federal District and in three states: São Paulo, Minas Gerais, and Paraná. In the range of 40% to 70%, seven other states appear: Rio de Janeiro, Espírito Santo, Goiás, Mato Grosso do Sul, Roraima, Bahia and Paraíba; in the range below, from 20% to 40%, there are nine states: Mato Grosso, Rio Grande do Sul, Ceará, Tocantins, Pernambuco, Sergipe, Rio Grande do Norte, Santa Catarina, and Alagoas; while in the penultimate range, from 10% to 20%, there are four states: Maranhão, Piauí, Acre and Amazonas. Finally, there are three states in the smallest range, less than 10%: Pará, Amapá and Rondônia (Brasil Ministério Do Desenvolvimento Regional, 2019).
Only 22,41% of the Brazilian population has a private health plan, and the Other 77.59% mainly depends on the Unified Health System (SUS). In Brazil, the number of ICU beds went from 46.045 in December 2019 (pre-pandemic period) to 60.265 (post-pandemic) in April 2020, which represents a rise of 14.220 beds (23,59%). However, from these 14.220 new beds, only 3.104 are from the SUS and are available to the entire population. Going in the opposite direction, the private sector installed about 11.116 beds from the 14.220 quoted above. Regarding the needs of the UTI beds, the north region, for example, has about 18,43 million inhabitants, representing approximately 8,77% of the country's population. Of these, 90,72% are exclusively dependent on SUS and dispute 1.793 beds from UTI SUS, which means that there is approximately one SUS for Every 9.325 people. On the other hand, the northeast region has about 57,07 million people, representing approximately 27,15% of the country's population. From these, 88,43% depends solely on SUS, disputing 5.968 beds, which means that there is one bed for every 8.456 people (de Souza et al., 2020).
It is essential to mention seasonal contagious infectious diseases, increasing the risk of death from COVID-19. An example of that is dengue (Câmara et al., 2007), a disease that has significant seasonal occurrence in hot months, corresponds to the first semester of the year and the beginning of the pandemic of SARS-CoV-2 in the country (Brasil, 2020). The 2017 epidemiological bulletin published by the Health Surveillance Secretariat of Health points to a number of 249,056 probable dengue cases in Brazil that year (Brasil, 2020).
The relation between the confirmed cases, the economic crisis and unemployment, must be better studied since low-income people and out of the labour market tends to ignore the social distancing in the search for subsistence.
According to official data (Instituto Brasileiro de Geografia e Estatística (IBGE), 2020), the unemployment rate in Brazil in September–October-November and October–November-December 2019 was 11.2 and 11%, respectively. In May–June-July 2020, with the pandemic ongoing, the unemployment rate was 13.8%. The survey carried out by the IBGE (Instituto Brasileiro de Geografia e Estatística (IBGE), n.d.) on unemployment, income, leave, remote work and other effects of the pandemic at work points to an unemployment rate between 09/20 and 09/26/2020 of 14.4%.
In 2014, the south and southeast region states concentrated more than 71,35% of the gross domestic product (PIB), accommodating 56,26% of the population; meanwhile, the northeast, participating with 13.93% on the PIB, was accommodating 27.69% of the population. This analysis demonstrates the abyss between north/northeast and South/southeast, securing the maintenance of the social inequalities between the two blocks (Espacial et al., 2020).
The average real monthly income of all White people's jobs (R$ 2.999) was more significant than the ones observed for brown people (R$ 1.719) and black (R$ 1.673). As a result, white people have shown an income of 29.9%, superior to the national average (R$ 2.308); meanwhile, brown and black people presented income 25.5% and 27.5%, respectively, inferior to the national average in 2019 (Instituto Brasileiro de Geografia e Estatística (IBGE), 2020).
Another spotlight data is that 1 in 5 Brazilian workers received less than half of the minimum wage in 2019. The average income between the 20% with lesser work income was just R$ 471 in 2019 (Amorim, 2020).
Although the Federal Government has implemented a social protection program for the most vulnerable population, called Emergency Aid, to people in socioeconomic vulnerability, the amount was not able to guarantee people's subsistence, taking many of them to the streets to perform informal work activities to supplement family income (Brasil Decreto No 10.316 de 07 de Abril de 2020, 2020; DECRETO No 10.488, 2020; Brasil Decreto No 10.661, de 26 de Março de, 2021) (DECRETO No 10.488, 2020; Decreto No 10.316 de 07 de Abril de, 2020; DECRETO No 10.412, DE 30 DE JUNHO DE, 2020; DECRETO No 10.661, DE 26 DE MARÇO DE, 2021).
According to a survey, Brazil possesses 38,8 million people who work informal jobs, representing 41,4% (Informalidade No País Atinge Quase 40 Milhões de Pessoas, Diz IBGE, 2019).
The problems generated by the pandemic culminate in a more significant public expenditure of resources, especially concerning the structuring of health units and the purchase of medicines and personal protective equipment.
An example of that was the collapse lived in the town of Manaus, the capital of the state of Amazonas, who is suffered from the lack of oxygen supply at the beginning of the year 2021, and which soon went through the interior of the state (Crise Do Oxigênio: Um Mês Após Colapso Em Hospitais, Manaus Ainda Depende de Doações Do Insumo. G1, 2021). The lack of oxygen might have led to the death of more than 30 people in the days of 14 and 15 of January when the capital reached its peak in the lack of input (Documentos Mostram Que Mais de 30 Morreram Nos Dois Dias de Colapso Por Falta de Oxigênio Em Manaus. G1, 2021).
Several diversions of public resources have already been investigated throughout the pandemic in Brazil. The Federal Police launched several operations to investigate deviations, irregular use of resources and fraud in bidding for funds destined to combat COVID-19 (Operação Cobiça Fatal Desarticula Associação Criminosa Envolvida Em Fraude à Licitação, 2020; Polícia Federal Apura Aplicação Irregular de R$ 1,8 Milhão No Combate Ao Coronavírus Em Santana/AP, 2020; Polícia Federal Deflagra 5a Fase Da Operação Xeque-Mate Que Investiga Desvios de Recursos Na Paraíba, 2020).
There is no denying that corruption plays a fundamental role in the morbidity and mortality in the country since once these resources are diverted or arrive late to the health system, they end up exposing the vulnerable population to the disease without medical or hospital diagnosis or support.
Efficiency in controlling the pandemic is due to the coordination of measures adopted in all spheres. Unfortunately, in Brazil, the federal public response is uncoordinated (The Lancet COVID-19 in Brazil: “So What?”, 2020).
The federal senate, in 2021, approved the creation of a Parliamentary Committee of Inquiry (CPI) of COVID-19, which will investigate actions and omissions from the federal government in the battle against the pandemic and the collapse of the health at the state of Amazonas at the beginning of 2021 (CPI Da Covid é Criada Pelo Senado. 2021, 2021).
Recently, we had the first governor to be impeached in an impeachment process in the history of the Republic. The governor is accused of leading a scheme of corruption in the health’s area during the construction of campaign hospitals (Mendes, 2021). These measures demonstrate difficulty in reaching consensus in a country with so many political disputes. In addition, the federal government has made several changes in the role of the Minister of Health during the pandemic, which made the enabling of beds from the ICU that depends on transfers from the federal government (Mariz, 2020; Arreguy, 2020; Queiroga, n.d.).
Underreporting is a problem that aggravates crisis management caused by the new Coronavirus. In Brazil, low availability of RT-PCR (reverse transcription-polymerase chain reaction) tests forced the Ministry of Health to recommend testing for only severe cases (Brasil Coronavírus Brasil COVID-19, 2021) at the beginning of the pandemic. Unfortunately, this factor goes against the guidelines and strategies for coping with the pandemic since the practice of testing is a primary factor as an organizational measure of the health system (Peto, 2020).
The use of medication without proven scientific evidence may also have contributed to morbidity and mortality. There are cases of purchase of these drugs that make up the “COVID kit” being delivered to the population upon prior consultation, diagnosis and medical prescription, specifically those seeking primary health care, to allow the early treatment of patients with COVID- 19 (Governo de Mato Grosso Compra Lotes de “Kit-Covid” Para Distribuir Aos 141 Municípios, n.d.; Geovana, 2020). In addition, many people fail to compress proven effective measures, such as social distance, because they believe in the effectiveness of these drugs in case of contamination by the virus.
In a study realized with 11.330 adults, it was possible to see that remdesivir, hydroxychloroquine, lopinavir and interferon had little or no effects on patients hospitalized with COVID-19, as indicated by general mortality, the onset of ventilation and length of hospital stay (N. Engl. J. Med., 2021).
In a statement, a pharmaceutical company, developer of Ivermectin claimed their position about the use of the medicine during the pandemic of COVID-19. However, after analysis, the scientists from the company have observed, until the moment, not a single scientific base to a potential therapeutical effect. Furthermore, against the COVID-19 from pre-clinic studies, there is no significant evidence of the clinical activity or clinical efficiency on patients of COVID-19 and the alarming lack of security data in most studies (Merck Statement on Ivermectin Use During the COVID-19 Pandemic, n.d.).
The flexibilization of the restriction measures without having the collaboration from the people may lead to an increase in the number of cases, being necessary new restrictions (Quatro Meses Após Flexibilização, 2020), which in addition to damage the health and economy areas, leads to a lower population adherence due to the prolonged period of restrictions and flexibilities.
The holding of municipal elections in the country, followed by the Christmas celebration, new year and vacations, could contribute to the rise of the number of cases in the country (Campanha Eleitoral Ajudou a Aumentar Casos Da Covid-19 No Brasil, Afirma Médico, 2020; Covid-19: Após Festas de Fim de Ano, Testes Positivos Crescem Até 38% Em Laboratórios de Campinas. G1, 2021).
However, although several factors favour the continuity and escalation of the pandemic, the population still has a free, unrestricted and universal health system, the Unified Health System (SUS) (Jairnilson and Paim, 2011). Among all the aspects pointed out during the pandemic, the SUS is undoubtedly strengthened. Although it needs improvement, the system is fundamental in such an unequal country, mainly because it is not a system that discriminates or predilects. Its importance can be exemplified in the excerpt of Law 8.080 / 90, (Brasil, 1990) known as the Organic Health Law, which brings as principles and guidelines the universality of access to health services at all levels of assistance and comprehensive care. In addition to the various social inequalities that plague the already vulnerable Brazilian population, such as lack of basic sanitation, access to essential health services, unemployment, and low income, it is clear that the political and economic instability that occurs in Brazil, as well as corruption, ends up catalyzing the pandemic and potentiate inequalities. Therefore, public policies aimed mainly at the poorest population must be implemented to minimise the damage caused by the pandemic to the population, whether directly or indirectly. Even having worked beyond its operating limit at various times during the pandemic, the SUS is unique and essential for the population. It is a system that does not discriminate against any individual who uses it. Therefore, investing in SUS is fundamental for health promotion in Brazil.
12. Factors contributing to low mortality rate of COVID-19 in UAE
The United Arab Emirates (UAE) is a federation of seven small Emirates or states, namely, Abu Dhabi, Dubai, Sharjah, Ajman, Fujairah, Ras Al Khaimah and Umm Al Quwain. Based on 2021 statistics, the population of UAE is estimated to be 9.99 million, approximately 90% of whom live either in Dubai, Abu Dhabi or Sharjah. The country is ethnically very diverse with over 85% of the population being expatriates from nearly 200 different countries 1. Due to the large proportion of single expatriate workforce, mostly from the Indian subcontinent, UAE has a very unusual gender and age distribution; males constitute nearly 70% of the population and more than 65% are in the 25-to-54 year age range (United Arab Emirates Population Statistics, 2021).
UAE has a highly developed and well-established healthcare infrastructure capable of delivery world-class service. This is exemplified in the way the country managed the COVID-19 pandemic. As of 1st December 2021, UAE reported a total of 742,278 PCR confirmed COVID-19 cases, with only 2148 deaths (CMR: 0.289%) (Ritchie et al., 2020). Majority of the patients with severe disease were males, often with one or more commodities, such as diabetes, hypertension, obesity, liver and cardiovascular diseases (Hannawi et al., 2021; Hosani et al., 2021). Notably, the mean age of UAE cases tended to be lower than that reported in many other countries, reflecting the younger population of the country. The highest peak of cases and deaths occurred in January 2021.
The overall mortality rate in UAE was much lower than many other highly developed nations, including UK, US, Germany and France.2 There are a number factors which are likely to have contributed to the low mortality seen in UAE. UAE reported its first cases on 29th Jan 2020 in a family of four who travelled from Wuhan, China (Alsuwaidi et al., 2021). UAE government's early, decisive and measured interventions were central in controlling the outbreak and limiting the burden on the healthcare systems. Emergency response systems were swiftly activated, policies and guidelines were quickly developed, disseminated and implemented, and new facilities for handling COVID-19 were established in record time (Al Hosany et al., 2021). Travel restrictions started as early as Jan 31 with suspension of all flights from China, except Beijing. On 9th Feb, the Health Ministers of the six neighboring Gulf countries announced cross-border preventive measures. Travel restrictions were gradually extended to other countries reporting high rates of infection. By April, a number of other containment and mitigation measures were introduced, including, suspension of public events, closure of educational institutions and introduction of online teaching (Al Kaabi et al., 2021). Tourist attractions, entertainment destinations, and places of public worship were suspended. Moreover, early implementation of social distancing, mandatory use of face masks, and rigorous contract tracing and isolation, were fundamental in containing and controlling the outbreak (Al Kaabi et al., 2021).
Other essential measures and policies swiftly implemented early in the outbreak, included, free health care and treatment for all COVID-19 patients, establishing field hospitals and drive-through PCR testing, and introduction of digital platforms for recoding tests and facilitating quarantine and isolation procedures (Al Hosany et al., 2021; Al Kaabi et al., 2021). Indeed, the country had the highest PCR testing rates in the world (Al Kaabi et al., 2021). UAE was also among the first to launch phrase III clinical trial for COVID-19 inactivated vaccine (Sinopharm) in July 2020 (Crasto, 2021). The vaccine was approved for emergency use at the end of September 2020 and rolled out for mass vaccination by December. In addition to the inactive vaccine, the mRNA (Pfizer) vaccine was also used. By July 2021, more 65% of the population had been fully vaccinated and booster doses were being introduced. As of December 2021, a staggering 98% of the population had received at least 1 dose (Ritchie et al., 2020).
To summarize, UAE's early and decisive response to the pandemic, coupled with implementation of appropriate public health measures and world-class healthcare facilities, contributed to limiting the mortality from COVID-19. Having a young population is also likely to have helped.
13. Conclusion
Novel coronavirus (SARS-CoV-2) pandemic is a global health problem jeopardizing all the components of health, society, and the environment. Impact on health varies from asymptomatic cases to mortality. It depends on the strain of virus involved, patient's health and immune status, age, sex, another disease, among others. Therefore, the case fatality ratio (%) varies a lot among analysed countries. Nevertheless, it remains an unanswered question whether all COVID-19 cases are registered in all countries. However, regular monitoring of the COVID-19 pandemic situations based on epidemiological factors and consistently directing resources allocation for patients based on their requirements and opportunities should be implemented to give a strong hypothesis on the impacts of COVID-19 in regular human life to actualise effective prevention strategies. In addition, immunopathological studies should be performed to detect the severity of COVID-19 and develop effective therapeutics. Although very recently, vaccines have been developed against SARS-CoV-2, their availability is questionable. Even the WHO itself has expressed concern about vaccine availability to cover the majority of the world's population at risk. Therefore, it is crucial to identify the risk factors in detail to take intervention measures to control the pandemic.
CRediT authorship contribution statement
Sina Salajegheh Tazerji, Fatemeh Shahabinejad, Mohammad Ali Rad and Mahya Tokasi studied and analysed the geographical area of Iran. The analysis of the geographical area of Eastern Europe - Poland was performed by Krzysztof J. Filipiak, Lukasz Szarpak, Tomasz Dzieciatkowski and Jan Jurgiel. Phelipe Magalhães Duarte alone analysed and wrote the information of Brazil. Md. Tanvir Rahman, Md. Abdus Sobur, Md. Saiful Islam and Adnan Ahmed provided information on Bangladesh and Rasha Gharib, Mohamed N.F. Shahen, Awad A Shehata and Mohamed Fawzy analysed and wrote about Egypt. Yashpal Singh Malik, Ganesh Balasubramanian and Vinodhkumar OR were in charge of surveying the geographical area of Southeast Asia and India, Kannan Subbaram, in collaboration with Shaik Syed Ali Pakeer and Sheeza Ali, focused on Africa and South Asia. Muhammad Safdar, Yasmeen Junejo, Muhammad Saeed, Umair Younus and Muhammad Sajjad Khan reviewed and wrote information about Pakistan. Saif Ur Rehman and Mehmet Ozaslan reviewed and disseminated information from China and Turkey, respectively. Gulfaraz Khan focused on United Arab Emirates. Muhammad Safdar, Sina Salajegheh Tazerji, Mahya Tokasi and professor Rasha Gharieb and Alfonso J. Rodriguez-Morales were in charge of the final review, completion and final editing.
Funding
Not applicable.
Availability of data and materials
All data analysed or generated during this study are included in this publication and its additional files.
Ethical approval
We have followed all ethical approvals for this study.
Informed consent
All authors have read and approved the contents and manuscript.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
We want to thank Dr. Baharak Akhtardanesh, Professor, The Department of Clinical Sciences, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Iran and Dr. Farrokhreza Kabir, Assistant professor, The Department of Clinical Sciences, Faculty of specialized Veterinary Medicine, Science and Research Branch, Islamic Azad University, Tehran, Iran for their critical comments on this paper.
Edited by Hee-Jeong Im Sampen
Footnotes
All authors have equally contributed.
References
- Abdel Wahed W.Y., Hefzy E.M., Ahmed M.I., Hamed N.S. Assessment of knowledge, attitudes, and perception of health care workers regarding COVID-19, a cross-sectional study from Egypt. J. Community Health. 2020;45:1242–1251. doi: 10.1007/s10900-020-00882-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abid K., Bari Y.A., Younas M., Tahir Javaid S., Imran A. Progress of COVID-19 epidemic in Pakistan. Asia Pac. J. Public Health. 2020;32:154–156. doi: 10.1177/1010539520927259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Hosany F., Ganesan S., Al Memari S., Al Mazrouei S., Ahamed F., Koshy A., et al. Response to COVID-19 pandemic in the UAE: a public health perspective. J. Glob. Health. 2021;27(11):03050. doi: 10.7189/jogh.11.03050. (Mar) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Kaabi N., Zhang Y., Xia S., Yang Y., Al Qahtani M.M., Abdulrazzaq N., et al. Effect of 2 inactivated SARS-CoV-2 vaccines on symptomatic COVID-19 infection in adults: a randomized clinical trial. JAMA. 2021;326(1):35–45. doi: 10.1001/jama.2021.8565. Jul 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Mahtab M., Akbar S.M., Mahtab M., Choudhury N., Islam M.A., Bhuyan M.A., Ashab E., Haque M.J., Hoque S.M.M., Huq A.F., et al. Treatment of COVID-19 Patients at a Medical College Hospital in Bangladesh. Euroasian J. Hepato-Gastroenterol. 2020;10:27–30. doi: 10.5005/jp-journals-10018-1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali A., Zhongren M., Baloch Z. Covid-19 in Pakistan and potential repercussions for the world: is the infection on the verge of endemicity? BMJ. 2020;m1909 doi: 10.1136/bmj.m1909. [DOI] [PubMed] [Google Scholar]
- Alsuwaidi A.R., Al Hosani F.I., ElGhazali G., Al-Ramadi B.K. The COVID-19 response in the United Arab Emirates: challenges and opportunities. Nat. Immunol. 2021;22(9):1066–1067. doi: 10.1038/s41590-021-01000-5. (Sep) [DOI] [PubMed] [Google Scholar]
- Amorim D. Diz IBGE; UOL: 2020. Um Em Cada Cinco Trabalhadores Tem Renda Média de R$ 471. [Google Scholar]
- Anadolu Agency Bangladesh to Hold 3 By-Elections amid Pandemic 2020. https://www.aa.com.tr/en/asia-pacific/bangladesh-to-hold-3-by-elections-amid-pandemic/1951025
- Anwar S., Nasrullah M., Hosen M.J. COVID-19 and Bangladesh: challenges and how to address them. Front. Public Health. 2020;8:154. doi: 10.3389/fpubh.2020.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arab News “Virus Infects 97 Politicians in Pakistan” Arab News. 2021. https://www.arabnews.com/node/1690811/world
- Arreguy J. 2020. Após 4 Meses Interino, Pazuello Assume Saúde e Minimiza Convívio Com Covid. UOL. Available online: https://noticias.uol.com.br/saude/ultimas-noticias/redacao/2020/09/16/apos-4-meses-como-interino-general-pazuello-assume-ministerio-da-saude.htm. [Google Scholar]
- Axios Thousands in Bangladesh Gather at Funeral despite Coronavirus Lockdown. (n.d.). https://www.axios.com/bangladesh-coronavirus-funeral-f2397c5c-d295-4cb3-bab3-37482debd633.html 2020.
- Bai Y., Yao L., Wei T., Tian F., Jin D.-Y., Chen L., Wang M. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangladesh Confirms First Case of Coronavirus 2020. https://www.aa.com.tr/en/asia-pacific/bangladesh-confirms-first-case-of-coronavirus-/1758924
- Bangladesh Medical Association District Wise Total Number of Affected Doctor, Nurse & Staff (COVID 19 +) 2021. [Google Scholar]
- Battegay M., Kuehl R., Tschudin-Sutter S., Hirsch H.H., Widmer A.F., Neher R.A. 2019-Novel Coronavirus (2019-NCoV): estimating the case fatality rate - a word of caution. Swiss Med. Wkly. 2020;150 doi: 10.4414/smw.2020.20203. [DOI] [PubMed] [Google Scholar]
- Brasil . 1990. Lei No 8.080/90. Brasília: Diário Oficial Da União. [Google Scholar]
- Brasil . Diário Oficial Da União; Brasília: 2019. Resolução No 3, de 26 de Agosto de 2019. [Google Scholar]
- Brasil . 2020. Ministério Da Saúde. Resposta Nacional e Internacional de Enfrentamento Ao Novo Coronavírus. [Google Scholar]
- Brasil Coronavírus Brasil COVID-19 Ministério Da Saúde. 2021. https://covid.saude.gov.br
- Brasil Decreto No 10.316 de 07 de Abril de 2020 . 2020. Brasília: Diário Oficial Da União, 2020. [Google Scholar]
- Brasil Decreto No 10.661, de 26 de Março de . 2021. Brasília: Diário Oficial Da União, 2020. https://www.in.gov.br/en/web/dou/-/decreto-n-10.661-de-26-de-marco-de-2021-310836042 2020. [Google Scholar]
- Brasil Ministério Do Desenvolvimento Regional . 2019. Secretaria Nacional de Saneamento – SNS. Sistema Nacional de Informações Sobre Saneamento: Diagnóstico Dos Serviços de Água e Esgotos – 2017. Brasília: SNS/MDR, 2019. [Google Scholar]
- Breaking: Egypt Reports First Case of Coronavirus . 2020. Egyptian Streets. (February 14) [Google Scholar]
- Breastfeeding Advice during the COVID-19 outbreak.
- Câmara F.P., Theophilo R.L.G., Dos Santos G.T., Pereira S.R.F.G., Câmara D.C.P., De Matos R.R.C. Regional and dynamics characteristics of dengue in Brazil: a retrospective study. Rev. Soc. Bras. Med. Trop. 2007;40:192–196. doi: 10.1590/s0037-86822007000200009. [DOI] [PubMed] [Google Scholar]
- Campanha Eleitoral Ajudou a Aumentar Casos Da Covid-19 No Brasil, Afirma Médico . 2020. ISTOÉ. [Google Scholar]
- CDC Laboratory Confirmed COVID-19 Associated Hospitalizations 2021. https://gis.cdc.gov/grasp/COVIDNet/COVID19_5.html
- COVID-19 Bangladesh Situation Reports; 2021.
- Covid-19: Após Festas de Fim de Ano, Testes Positivos Crescem Até 38% Em Laboratórios de Campinas. G1. 2021. https://g1.globo.com/sp/campinas-regiao/noticia/2021/01/14/covid-19-apos-festas-de-fim-de-ano-testes-positivos-crescem-ate-38percent-em-laboratorios-de-campinas.ghtml Available online:
- CPI Da Covid é Criada Pelo Senado. 2021 2021.
- Crasto A. New Drug Approvals. 2021. BBIBP-CorV, Sinopharm COVID-19 vaccine.https://newdrugapprovals.org/2021/03/23/bbibp-corv-sinopharm-covid-19-vaccine/ Available online: Chicago. [Google Scholar]
- Crise Do Oxigênio: Um Mês Após Colapso Em Hospitais, Manaus Ainda Depende de Doações Do Insumo. G1 2021. https://g1.globo.com/am/amazonas/noticia/2021/02/14/crise-do-oxigenio-um-mes-apos-colapso-em-hospitais-manaus-ainda-depende-de-doacoes-do-insumo.ghtml Available online:
- Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawn Covid-19 Kills More Men than Women in KP: Report 2021. https://www.dawn.com/news/1568895
- Decreto No 10.316 de 07 de Abril de 2020. https://legislacao.presidencia.gov.br/atos/?tipo=DEC&numero=10316&ano=2020&ato=542MTUU1EMZpWT7df Available online:
- DECRETO No 10.412, DE 30 DE JUNHO DE 2020. https://www.in.gov.br/en/web/dou/-/decreto-n-10.412-de-30-de-junho-de-2020-264424956 Available online:
- DECRETO No 10.488 DE 16 DE SETEMBRO DE. 2020. https://www.in.gov.br/en/web/dou/-/decreto-n-10.488-de-16-de-setembro-de-2020-277742753 Available online:
- DECRETO No 10.661, DE 26 DE MARÇO DE 2021. https://www.in.gov.br/en/web/dou/-/decreto-n-10.661-de-26-de-marco-de-2021-310836042 Available online:
- DhakaTribune Covid-19 Battering Frontline Fighters in Bangladesh. (n.d.). https://www.dhakatribune.com/health/coronavirus/2020/07/04/covid-19-battering-frontline-fighters-in-bangladesh 2020.
- Documentos Mostram Que Mais de 30 Morreram Nos Dois Dias de Colapso Por Falta de Oxigênio Em Manaus. G1 2021. https://g1.globo.com/am/amazonas/noticia/2021/01/25/documentos-mostram-que-mais-de-30-morreram-nos-dois-dias-de-colapso-por-falta-de-oxigenio-em-manaus.ghtml Available online:
- Du R.-H., Liang L.-R., Yang C.-Q., Wang W., Cao T.-Z., Li M., Guo G.-Y., Du J., Zheng C.-L., Zhu Q., et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur. Respir. J. 2020;55:2000524. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DW News Turkey’s Public Health System Faces Coronavirus Pandemic. 2020. https://www.dw.com/en/turkeys-public-health-system-faces-coronavirus-pandemic/a-53365341
- ECDC Outbreak of Acute Respiratory Syndrome Associated with a Novel Coronavirus, China: First Local Transmission in the EU/EEA − Third Update 2020. https://www.ecdc.europa.eu/sites/default/files/documents/novel-coronavirus-risk-assessment-china-31-january-2020_0.pdf
- Egypt Detects Second Case of New Coronavirus: Health Ministry . 2020. Reuters. March. [Google Scholar]
- Egypt-Nile-Coronavirus @ Www.Nytimes.Com.
- El-Sokkary R.H., El-Kholy A., Mohy Eldin S., Khater W.S., Gad D.M., Bahgat S., Negm E.E.M., El Kholy J.A., Mowafy S., Mahmoud E., et al. Characteristics and predicting factors of corona virus disease-2019 (COVID-19) among healthcare providers in a developing country. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0245672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espacial C., Produção D.A., Pochmann M., Caetano L. 2020. Spatial Concentration of Production; pp. 1–25. [Google Scholar]
- Ferdous T., Cederholm T., Razzaque A., Wahlin A., Nahar Kabir Z. Nutritional status and self-reported and performance-based evaluation of physical function of elderly persons in rural Bangladesh. Scand. J. Public Health. 2009;37:518–524. doi: 10.1177/1403494809102778. [DOI] [PubMed] [Google Scholar]
- Foresta C., Rocca M.S., Di Nisio A. Gender susceptibility to COVID-19: a review of the putative role of sex hormones and X chromosome. J. Endocrinol. Investig. 2021;44:951–956. doi: 10.1007/s40618-020-01383-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genç K. COVID-19 in Turkey: a nation on edge. Lancet. 2021;397:1794–1796. doi: 10.1016/S0140-6736(21)01098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geovana E. Prefeitura Compra 400 Kits de Remédios Para Tratar Pacientes Com Covid-19 Em Nova União, RO. G1. 2020. https://g1.globo.com/ro/rondonia/noticia/2020/07/25/prefeitura-compra-400-kits-de-remedios-para-tratar-pacientes-com-covid-19-em-nova-uniao-ro.ghtml
- Government of Pakistan. Pakistan Statistics.
- Governo de Mato Grosso Compra Lotes de “Kit-Covid” Para Distribuir Aos 141 Municípios http://www.mt.gov.br/-/14829870-governo-de-mato-grosso-compra-lotes-de-kit-covid-para-distribuir-aos-141-municipios Available online:
- Griffith D.M., Sharma G., Holliday C.S., Enyia O.K., Valliere M., Semlow A.R., Stewart E.C., Blumenthal R.S. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev. Chronic Dis. 2020;17 doi: 10.5888/pcd17.200247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundel S. Towards a new typology of crises. J. Conting. Crisis Manag. 2005;13:106–115. doi: 10.1111/j.1468-5973.2005.00465.x. [DOI] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic?: Early findings and lessons for planners. J. Am. Plan. Assoc. 2020;86:495–509. doi: 10.1080/01944363.2020.1777891. [DOI] [Google Scholar]
- Hannawi S., Hannawi H., Naeem K.B., Elemam N.M., Hachim M.Y., Hachim I.Y., et al. Clinical and laboratory profile of hospitalized symptomatic COVID-19 patients: case series study from the first COVID-19 center in the UAE. Front. Cell. Infect. Microbiol. 2021;11 doi: 10.3389/fcimb.2021.632965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque A. The COVID-19 pandemic and the public health challenges in Bangladesh: a commentary. JHR. 2020;34:563–567. doi: 10.1108/JHR-07-2020-0279. [DOI] [Google Scholar]
- Hasell J., Ortiz-Ospina E., Ritchie H., Roser M. 2020. “Coronavirus Pandemic (COVID-19)”. Our World in Data.https://ourworldindata.org/coronavirus [Google Scholar]
- Helmy Y.A., Fawzy M., Elaswad A., Sobieh A., Kenney S.P., Shehata A.A. The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. J. Clin. Med. 2020;9 doi: 10.3390/jcm9041225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosani F.A., Aden B., Memari S.A., Mazrouei S.A., Ajab S., Abid M., et al. Epidemiology of asymptomatic and symptomatic Coronavirus Disease 2019 confirmed cases in the Emirate of Abu Dhabi, United Arab Emirates: observational study. Medicine (Baltimore) 2021;100(12):e25219. doi: 10.1097/MD.0000000000025219. Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain S.S., Khan A., Gulshan J., Roy P.K., Sadia F., Alam M.S. Bangladesh Bureau of Statistics (BBS), Elderly Population in Bangladesh: Current Features and Future Perspectives. Population Monograph. 2015. http://203.112.218.65:8008/WebTestApplication/userfiles/Image/PopMonographs/elderlyFinal.pdf
- Https://Www.Worldometers.Info/Coronavirus/Country/India/ 2020. [Google Scholar]
- ICMR Disease Burden Trends in the States of India 1990 to 2016 . 2017. Report. https://www.healthdata.org/sites/default/files/files/policy_report/2017/India_Health_of_the_Nation%27s_States_Report_2017.pdf. [Google Scholar]
- Indian TV-News India TV News. Looking at Gradual Withdrawal of Lockdown 2020. https://www.indiatvnews.com/news/india/lockdown-4-0-withdrawal-relaxation-pm-modi-meeting-cms-limited-trains-economic-activities-all-details-616336
- Informalidade No País Atinge Quase 40 Milhões de Pessoas, Diz IBGE . 2019. Folha de São Paulo. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística (IBGE). 2019.
- Instituto Brasileiro de Geografia e Estatística (IBGE) 2020. Pesquisa Nacional Por Amostra de Domicílios Contínua - PNAD Contínua. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística (IBGE) Desocupação, Renda, Afastamentos, Trabalho Remoto e Outros Efeitos Da Pandemia No Trabalho. https://covid19.ibge.gov.br/pnad-covid/trabalho.php Available online:
- Jackson C.B., Farzan M., Chen B., Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 2021 doi: 10.1038/s41580-021-00418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jairnilson P., Paim J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377:1778–1797. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- Junejo Y., Ozaslan M., Safdar M., Khailany R.A., Rehman S., Yousaf W., Khan M.A. Novel SARS-CoV-2/COVID-19: origin, pathogenesis, genes and genetic variations, immune responses and phylogenetic analysis. Gene Rep. 2020;20 doi: 10.1016/j.genrep.2020.100752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junejo Yasmeen, Ozaslan Mehmet, Safdar Muhammad. Novel SARS-COV-2/COVID-19: an update of prevalence, modes of transmission, clinical manifestations, prevention and management. Zeugma Biol. Sci. 2021;2(3):1–5. [Google Scholar]
- Jurgiel J., Dzieciątkowski T., Szarpak Ł., KJ F. 2020. What Have We Learned about COVID-19 in 2020? [Google Scholar]
- Khalid A., Savaiz E. 2020. COVID-19 takes its toll on dentistry in Pakistan too. Dentistry Today.https://www.dentistrytoday.com/news/todays-dental-news/item/7074-covid-19-takes-its-toll-on-dentistry-in-pakistan-too [Google Scholar]
- Khamis T., Naseem A., Khamis A., Petrucka P. The COVID-19 pandemic: a catalyst for creativity and collaboration for online learning and work-based higher education systems and processes. JWAM. 2021;13:184–196. doi: 10.1108/JWAM-01-2021-0010. [DOI] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P.-I., Hsueh P.-R. Emerging Threats from Zoonotic Coronaviruses-from SARS and MERS to 2019-NCoV. J. Microbiol. Immunol. Infect. = Wei mian yu gan ran za zhi. 2020;53:365–367. doi: 10.1016/j.jmii.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariz R. Troca de Ministros Na Saúde Atrasou Opção de Novas UTIs Pelo Brasil. Época. 2020. https://epoca.globo.com/brasil/troca-de-ministros-na-saude-atrasou-operacao-de-novas-utis-pelo-brasil-24440313 Available online:
- Medhat M., El Kassas M. COVID-19 in Egypt: uncovered figures or a different situation? J. Glob. Health. 2020;10 doi: 10.7189/jogh.10.010368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes G. Wilson Witzel Sofre Impeachment e Perde Direitos Por Cinco Anos. Congresso Em Foco. 2021. https://congressoemfoco.uol.com.br/governo/impeachment-wilson-witzel/
- Merck Statement on Ivermectin Use During the COVID-19 Pandemic.
- Ministry of Health and family Welfare, Government of India . 2021. Https://Www.Mygov.in/Covid-19. [Google Scholar]
- Mostafa A.S., Abdalbaky A., Fouda E.M., Shaaban H.H., Elnady H.G., Hassab-Allah M., Rashad M.M., El Attar M.M., Alfishawy M., Hussien S.M., et al. Practical approach to COVID-19: an Egyptian pediatric consensus. Egypt Pediatric Association Gaz. 2020;68:28. doi: 10.1186/s43054-020-00037-9. [DOI] [Google Scholar]
- Mukherjee S., Pahan K. Is COVID-19 gender-sensitive? J. NeuroImmune Pharmacol. 2021;16:38–47. doi: 10.1007/s11481-020-09974-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repurposed antiviral drugs for Covid-19 — interim WHO solidarity trial results. N. Engl. J. Med. 2021;384:497–511. doi: 10.1056/nejmoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operação Cobiça Fatal Desarticula Associação Criminosa Envolvida Em Fraude à Licitação 2020. http://www.pf.gov.br/imprensa/noticias/2020/06-noticias-de-junho-de-2020/operacao-cobica-fatal-combate-fraude-a-licitacao Available online:
- Ozaslan M., Safdar M., Kilic I.H., Khailan A. R Practical measures to prevent COVID-19: a mini-review. J. Biol. Sci. 2020;20:100–102. doi: 10.3923/jbs.2020.100.102. [DOI] [Google Scholar]
- Peto J. Covid-19 mass testing facilities could end the epidemic rapidly. BMJ. 2020;368 doi: 10.1136/bmj.m1163. [DOI] [PubMed] [Google Scholar]
- Polícia Federal Apura Aplicação Irregular de R$ 1,8 Milhão No Combate Ao Coronavírus Em Santana/AP 2020. http://www.pf.gov.br/imprensa/noticias/2020/05-noticias-de-maio/policia-federal-apura-aplicacao-irregular-de-r-1-8-milhao-no-combate-ao-coronavirus-em-santana-ap Available online:
- Polícia Federal Deflagra 5a Fase Da Operação Xeque-Mate Que Investiga Desvios de Recursos Na Paraíba 2020. http://www.pf.gov.br/imprensa/noticias/2019/10/policia-federal-deflagra-5a-fase-da-operacao-xeque-mate-que-investiga-desvios-de-recursos-na-paraiba Available online:
- Public Health Ontario Review of “The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020.” 2020. https://www.publichealthontario.ca/-/media/documents/ncov/research-cdc-epidemiological-characteristics.pdf?la=en [PMC free article] [PubMed]
- Quatro Meses Após Flexibilização Amazonas Volta a Adotar Restrições Contra Covid-19. Veja o Que Fica Proibido. 2020 https://g1.globo.com/am/amazonas/noticia/2020/09/25/quatro-meses-apos-flexibilizacao-amazonas-volta-a-adotar-restricoes-contra-covid-19-veja-o-que-fica-proibido.ghtml [Google Scholar]
- Queiroga, M.M. Assume Como Ministro Da Saúde Em Cerimônia Fechada. Poder360 Available online: https://www.poder360.com.br/governo/marcelo-queiroga-assume-como-ministro-da-saude-em-cerimonia-fechada/.
- Rahman M., Sobur M., Islam M., Toniolo A., Nazir K. Is the COVID-19 pandemic masking dengue epidemic in Bangladesh? J. Adv. Vet. Anim. Res. 2020;7:218. doi: 10.5455/javar.2020.g412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramadan H.K.-A., Mahmoud M.A., Aburahma M.Z., Elkhawaga A.A., El-Mokhtar M.A., Sayed I.M., Hosni A., Hassany S.M., Medhat M.A. Predictors of severity and co-infection resistance profile in COVID-19 patients: first report from upper Egypt. Infect. Drug Resist. 2020;13:3409–3422. doi: 10.2147/IDR.S272605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehman S.U., Shafique L., Ihsan A., Liu Q. Vol. 9. 2020. Evolutionary Trajectory for the Emergence of Novel Coronavirus SARS-CoV-2. Pathogens (Basel, Switzerland) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuters Bangladesh Reports First Coronavirus Death -Officials 2020. https://www.reuters.com/article/health-coronavirus-bangladesh-idUSL4N2BB384
- Ritchie H., Mathieu E., Rodés-Guirao L., Appel C., Giattino C., Ortiz-Ospina E., et al. 2020. Coronavirus Pandemic (COVID-19). Our World in Data [Internet]https://ourworldindata.org/coronavirus/country/united-arab-emirates Mar 5 [cited 2021 Dec 6]; Available from: [Google Scholar]
- Safdar Muhammad, Khan Muhammad Sajjad, Karim Abdulkarim Yasin, Omar Shwan Ali, Smail Shukur Wasman, Saeed Muhammad, Zaheer Sana, et al. SNPs at 3′ UTR of APOL1 and miR-6741-3p target sites associated with kidney diseases more susceptible to SARS-COV-2 infection: in silco and in vitro studies. Mamm. Genome. 2021:1–12. doi: 10.1007/s00335-021-09880-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scavone C., Brusco S., Bertini M., Sportiello L., Rafaniello C., Zoccoli A., Berrino L., Racagni G., Rossi F., Capuano A. Current pharmacological treatments for COVID-19: what’s next? Br. J. Pharmacol. 2020;177:4813–4824. doi: 10.1111/bph.15072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secretaria de Vigilância, Legisla P., Governo O.S.D.O., CDC, Covid-, D, WHO, Prevention, C. for D.C. and; Saúde, E.M.; Disease, C.; Infection, C, et al. Diagnóstico E Covid-19 Covid-19. Health Alert. Network. 2020;0:1–37. [Google Scholar]
- Sehsah R., Gaballah M.H., El-Gilany A.-H., Albadry A.A. Psychological distress among Egyptian physicians during COVID-19 pandemic. Int. Arch. Occup. Environ. Health. 2021;94:731–740. doi: 10.1007/s00420-020-01624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shangguan Z., Wang M.Y., Sun W. What caused the outbreak of COVID-19 in China: from the perspective of crisis management. IJERPH. 2020;17:3279. doi: 10.3390/ijerph17093279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma G., Volgman A.S., Michos E.D. JACC: Case Reports. Vol. 2. 2020. Sex differences in mortality from COVID-19 pandemic; pp. 1407–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A.K., Gupta R., Ghosh A., Misra A. Diabetes in COVID-19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:303–310. doi: 10.1016/j.dsx.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Souza C.D.F., de Paiva J.P.S., Leal T.C., da Silva L.F., Santos L.G. Spatiotemporal Evolution of Case Fatality Rates of COVID-19 in Brazil, 2020. J. Bras. Pneumol. 2020;46:e20200208. doi: 10.36416/1806-3756/e20200208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Daily Star 45% of Dhaka Dwellers Exposed to Covid-19, IEDCR Survey Says 2020. https://www.thedailystar.net/45-percent-dhaka-dwellers-exposed-covid-19-iedcr-survey-says-1976777
- The Lancet. Vol. 395. 2020. The Lancet COVID-19 in Brazil: “So What?”; p. 1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Transformingindia . 2021. Https://Transformingindia.Mygov.in/Covid-19/?Sector=myth-Busters&type=en#scrolltothis. [Google Scholar]
- Twelve Asymptomatic Coronavirus Cases Registered on Nile Cruise Ship . 2020. Reuters. March 6. [Google Scholar]
- Underner M., Peiffer G., Perriot J., Jaafari N. Tabagisme et maladie à coronavirus 2019 (COVID-19) Rev. Mal. Respir. 2020;37:433–436. doi: 10.1016/j.rmr.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Arab Emirates Population Statistics 2021. https://www.globalmediainsight.com/blog/uae-population-statistics/ [Internet]. Official GMI Blog. [cited 2021 Dec 5]. Available from:
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Cheng Z., Yue X.-G., McAleer M. Risk management of COVID-19 by universities in China. JRFM. 2020;13:36. doi: 10.3390/jrfm13020036. [DOI] [Google Scholar]
- WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update (MMWU) 2021. https://cdn.who.int/media/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who_ban_sitrep_84_20211004.pdf?sfvrsn=18804279_9
- WHO Coronavirus Disease 2019 (COVID-19) Situation Report – 76 2020. https://reliefweb.int/report/world/coronavirus-disease-2019-covid-19-situation-report-76-5-april-2020
- WHO COVID-19 and NCDs. (n.d.). https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/covid-19-and-ncds 2020.
- WHO Index @ Covid19 . Vol. 1. 2020. Who.Int. Https://Covid19.Who.Int/ [Google Scholar]
- WHO Noncommunicable Diseases (NCD) Country Profiles, 2018. (2018). 30% 12%. 2018. https://www.who.int/nmh/countries/bgd_en.pdf?ua=1 2018.
- WHO Novel-Coronavirus-2019 . 2020. @ Www.Who.Int. [Google Scholar]
- Worldometer COVID-19 CORONAVIRUS PANDEMIC . 2020. HTTPS://WWW.WORLDOMETERS.INFO/CORONAVIRUS/ [Google Scholar]
- Zhang T., Wu Q., Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr. Biol. 2020;30:1346–1351.e2. doi: 10.1016/j.cub.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H., Chen X., Hu T., Li J., Song H., Liu Y., Wang P., Liu D., Yang J., Holmes E.C., et al. A novel bat coronavirus closely related to SARS-CoV-2 contains natural insertions at the S1/S2 cleavage site of the spike protein. Curr. Biol. 2020;30:2196–2203.e3. doi: 10.1016/j.cub.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data analysed or generated during this study are included in this publication and its additional files.