Abstract
Various types of stressors are associated with maladaptive eating, but how the stressor of everyday discrimination (e.g., less respect, poorer service) relates to maladaptive eating and adaptive eating remains unclear. We examined everyday discrimination as a predictor of maladaptive and adaptive eating. Data were collected in a population-based study, Eating and Activity over Time (N=1410, ages 18-30). Everyday discrimination was categorized as none, low, moderate, or high. Outcomes included maladaptive eating (i.e., overeating and binge eating) and adaptive eating (i.e., intuitive eating and mindful eating). Modified Poisson regressions estimated the prevalence ratios (PRs) for overeating and binge eating associated with everyday discrimination. Linear regressions estimated associations between everyday discrimination and intuitive and mindful eating scores. After adjustment for age, ethnicity/race, gender, and socioeconomic status, moderate and high levels of discriminatory experiences were each associated with a significantly greater prevalence of binge eating (PR=2.2, [95% CI=1.3-3.7] and PR=3.1, [95% CI=2.0-4.7], respectively) and lower intuitive (β=−0.4, [95% CI=−0.7, −0.2] and β=−0.5 [95% CI=−0.8, −0.3], respectively), and mindful eating scores (β=−0.3, [95% CI=−0.6, −0.1] and β=−0.5 [95% CI=−0.8, −0.3], respectively) compared to young adults with no discriminatory experience. Public health efforts to prevent maladaptive eating and encourage the adoption of adaptive eating should consider the potential contribution of everyday discrimination and the need to advocate for equity and inclusion.
Keywords: Everyday Discrimination, Overeating, Binge Eating, Intuitive Eating, Mindful Eating
1. Introduction
Stressors, including discriminatory experiences, are prevalent among adults and can range from major threats to one’s well-being to subtle insults or daily hassles (1). Although research on discrimination has grown exponentially over the past decade, most studies on discrimination in maladaptive eating (e.g., overeating, binge eating, and emotional eating) have focused on discrimination that is explicitly related to ethnicity/race (2-4) and weight (5-7).
To fully understand discriminatory experiences’ impact on maladaptive eating, it is crucial to examine not only major discriminatory experiences, such as those discriminatory experiences related to ethnicity/race and weight that may affect employment but also, more subtle forms of everyday discrimination such as discrimination related to respect or customer service (8-13).
Everyday discrimination often functions as a stressor (14,15), which can prompt negative emotions that affect an individual’s cognitive capacity for self-control and self-regulation (14) and lead to lower self-worth and self-efficacy for coping from everyday discrimination related distress. Consequently, individuals who experience everyday discrimination have been shown to engage in maladaptive eating, including binge eating (9), emotional eating, or eating foods high in fat and sugar (9,16,17), as a means to cope with or avoid the stress arising from such experiences (8,9,18,19).
Few studies of everyday discrimination and eating have extended the outcomes beyond maladaptive eating to include adaptive eating (20). Adaptive eating, such as intuitive and mindful eating, is gaining attention as an effective weight management method and is associated with positive health outcomes (21-27). Intuitive eating and mindful eating are two distinct but related eating behaviors. Intuitive eating is defined as a tendency to eat when one is hungry; eat the food one desires; understand how food is associated with the body’s physical sensation; and use these physical cues to determine what, when, and how much to eat (28,29). Mindful eating emphasizes paying attention to the present moment while eating (30) and to food’s effect on the senses as well as being aware of one’s physical and emotional sensations in response to eating (31). Both intuitive and mindful eating focus on using internal and physiological hunger and satiety cues rather than emotional or external cues to eat (25,28,29,32). To date, only a small number of studies have identified predictors of intuitive eating and mindful eating (20,33,34), none of which have examined discrimination as a potential predictor. Thus, it remains unclear whether everyday discriminatory experiences are predictors and barriers of adaptive eating. Exploring experiences of everyday discrimination as determinants of maladaptive and adaptive eating has implications at both the individual and the societal levels, including tailoring support for health behaviors, as well as developing policies and programs to reduce and prevent discrimination and its impacts.
In response to the gaps identified in the literature, this study primarily aims to examine the association of everyday discrimination with maladaptive eating (i.e., overeating and binge eating) and adaptive eating (i.e., intuitive eating and mindful eating) in a large population-based, racially and sociodemographically diverse sample of young adults. We hypothesized that experiences of everyday discrimination would be associated with a greater prevalence of maladaptive eating (overeating and binge eating) and lower adaptive eating scores (intuitive eating and mindful eating).
2. Methods
2.1. Study Design and Population
Eating and Activity over Time (EAT 2018) is the follow-up study of Eating and Activity in Teens (2010), an epidemiologic study examining eating, activity, and weight-related health and associated factors among middle-school and senior high school students in Minneapolis-St. Paul, Minnesota (N=2793) (35-37). At EAT 2018, participants were followed-up through online or mailed paper surveys. All study procedures were approved by the University of Minnesota’s Institutional Review Board Human Subjects Committee.
This present cross-sectional study was carried out using survey data from EAT 2018, collected in 2017-2018 from 1568 emerging adults. Participants with missing information about discriminatory experiences (n=54), eating behaviors (n=32), or key covariates (n=72) were excluded, leaving an analytic sample size of 1410 participants. The analytic sample of 1410 represents 90% of the 1568 respondents to EAT 2018. Participants in the present study had a mean age of 22.0 ±2.0 (range 18-30) years, and 59% were women.
As attrition from EAT 2010 to EAT 2018 did not occur completely at random, inverse probability weighting (IPW) was used for all analyses to minimize potential response bias due to missing data (38,39) and to extrapolate back to the original EAT 2010 school-based sample. Weights for IPW were derived as the inverse of the estimated probability that an individual responded to EAT 2018 based on several characteristics reported in 2010, including demographics, past year frequency of dieting, and weight status. There were no significant differences between the analytic sample of this study and the full EAT 2010 sample in demographic characteristics, dieting, or weight status (p>0.9). In the weighted analytic sample of this study, the ethnicity/race distribution was 20 % White, 28% African American or Black, 20% Asian American, 17% Hispanic, 4% Native American, and 11% mixed or other.
2.2. EAT Survey Development
Test-retest reliability of measures was assessed at EAT 2010 in a diverse sample of 129 adolescents over a week. At EAT 2018, test-retest reliability of measures was measured twice within a period of three weeks in a diverse sample of 112 emerging adults (35,40,41).
2.3. Measurements
2.3.1. Everyday discrimination questions
In epidemiological studies, limited numbers of items are generally used to lessen the burden of participants completing the survey. For this reason, of the five-item short version of the Everyday Discrimination Scale (42,43), three everyday discriminatory experiences that have been reported to be most prevalent (44,45) were used to assess everyday discrimination in this study. Those three discriminatory experiences include being treated with less respect or courtesy than others, receiving poor service, and other people acting as if they think you are not smart or clever. Responses were scored on a 5-point scale from “never” to “at least once a week”. Items were summed, with higher scores indicating greater everyday discrimination. Based on prior studies (46) and by examining the distribution of the summed scores, scores were further categorized into quartiles: none (score=0), low (score > 0 and ≤2), moderate (score >2 and ≤6), and high (> 6). Details of the verbatim questions and response options are described in Table 1.
Table 1.
Variables assessed in the study and description of each survey items
| Variables | Description | Response options | Psychometric Properties | |
|---|---|---|---|---|
| Everyday discrimination (42,43,62-64) | Everyday discrimination was assessed with the following three items You are treated with less respect or courtesy than other people You received poorer service than other people in restaurants and stores People act as if they think you are not smart or clever |
1=Never 2=Less than once a year 3=A few times a year 4=A few times a month 5=At least once a week A summed score of everyday discrimination was categorized into “none [score=0],” “low [score > 0 and ≤ 2],” “moderate [score >2 and <6],” and “high [≥ 6]” |
test-retest r=.7 at EAT 2018 | |
| Maladaptive Eating | Overeating (47,48,65) | Overeating was assessed with the item “In the past year, have you ever eaten so much food in a short period of time that you would be embarrassed if others saw you (binge-eating)?”. | Yes, no | test-retest % agreement = 90% for overeating at EAT 2018 |
| Binge eating (48) | Among a subset of participants who confirmed overeating (“In the past year, have you ever eaten so much food in a short period of time that you would be embarrassed if others saw you (binge-eating)?”, sense of loss of control was further assessed with the question, “During the times when you ate this way, did you feel you couldn’t stop eating or control what or how much you were eating?” |
Yes (to “overeating” and “sense of loss of control”), no | test-retest percent k=.6 for binge eating at EAT 2018 | |
| Adaptive Eating | Intuitive Eating (29) | Intuitive eating was assessed with items adapted from the Intuitive Eating Scale: “I stop eating when I feel full,” “I eat everything that is on my plate, even if I’m not that hungry,” and “I trust my body to tell me how much to eat,” |
0 = “hardly ever,” 1 = “sometimes,” 2 = “much of the time,” 3= “almost always.” The second item, “I eat everything that is on my plate, even if I’m not that hungry”was reverse scored. Each item related to intuitive eating was summed, and possible scores ranged from 0 to 9, with higher scores indicating higher levels of intuitive eating. |
McDonald’s ω = .6 at EAT 2018 test-retest r=.6 at EAT 2018 |
| Mindful Eating (50) | Mindful eating was assessed with the following items adapted from the Mindful Eating Questionnaire: “I eat so quickly that I don’t taste what I’m eating,” “I snack without noticing that I am eating” “Before I eat I take a moment to appreciate the colors and smells of my food” and “I taste every bite of food that I eat.” |
0 = “hardly ever”, 1= “sometimes”, 2= “much of the time”, 3= “almost always” The first two items were reverse coded. Each item related to mindful eating was summed, and possible score ranged from 0 to 12, with higher scores indicating higher levels of mindful eating. |
McDonald’s ω = .5 at EAT 2018 test-retest r=.7 at EAT 2018 |
|
| Sociodemographic variable (66-68) | Age was calculated from the question “what Is your birthdate? (month, day, year of birth)” Gender was assessed with the question, “Are you (1) male, (2) female, (3) different identity?” Ethnicity/race was assessed with the question: “Do you think of yourself as?” (1) White, (2) Black or African American, (3) Hispanic or Latino, (4) Asian American, (5) Native Hawaiian or Pacific Islander, (6) American Indian or Native American, Other SES was determined based on the highest education level of either parent with adjustments made for free/reduced price school meals, family public assistance receipt, and parent employment status. Weights and heights were measured by trained staff following standardized procedures to calculate BMI (kg/m2) |
Age test-retest correlation = 1.0 Ethnicity/race test–retest agreement = 98%–100% |
2.3.2. Maladaptive eating and adaptive eating
Variables for this study include maladaptive eating (i.e., overeating and binge eating) and adaptive eating (i.e., intuitive eating and mindful eating). Items used to assess overeating and binge eating were adapted from the Minnesota Adolescent Health Survey (47) and Questionnaire on Eating and Weight Patterns-Revised (48). Items used to assess intuitive eating and mindful eating were adapted from the Intuitive Eating Scale (49) and Mindful Eating Questionnaire (50), respectively. Details of maladaptive eating and adaptive eating are provided in Table 1.
2.3.3. Covariates
Covariates used for this study include age, ethnicity/race, gender, socioeconomic status, and body mass index (BMI) assessed in EAT 2018. Details are provided in Table 1.
2.4. Statistical Analysis
Participants’ demographic characteristics are presented as descriptive statistics. T-tests and chi-square tests were performed to examine differences among none, low, moderate, and high levels of discriminatory experiences. To estimate the associations between everyday discriminatory experiences and the prevalence of overeating and binge eating, multivariable modified Poisson regression models (51) were run, and prevalence ratios (PRs) and 95% confidence intervals (CIs) were reported. To examine the associations of discriminatory experiences with each adaptive eating outcome (intuitive eating and mindful eating scores), multivariable linear regression models were conducted. For each linear regression model, β coefficients and 95% CIs were reported. Interactions between gender and each discriminatory experience were tested to determine whether the associations between discriminatory experiences and eating behaviors statistically differed between women and men. Interaction terms between gender and discriminatory experience predicting eating behaviors were not statistically significant (p=.43 for overeating, p=.21 for binge eating, p=.08 for intuitive eating, and p=.63 for mindful eating); thus, we did not stratify analyses by gender. For our primary analyses, models were adjusted for age, ethnicity/race, gender, and parental socioeconomic status. Body mass index (BMI) in EAT 2018 was further adjusted in the fully adjusted models, to address the potential that higher body weight increases likelihood of experiencing everyday discrimination, engagement in maladaptive eating, and difficulty in adopting adaptive eating. All models were weighted so that the estimates reflect the original EAT 2010 sample population. Statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC).
3. Results
3.1. Everyday discrimination across sociodemographic variables
Of the 1410 participants, 34% (n=475) were categorized as having experienced no discrimination; 14% (n=204) had low discrimination; 29% (n=412) had moderate discrimination; and 23% (n=319) had high discrimination (Table 2). The prevalence of experiences of everyday discrimination was lower in the normal weight category (BMI between 18.5 and 24.9) than in other weight categories. No significant differences in discrimination were found by age, ethnicity/race, gender, or parental socioeconomic status. (Table 2).
Table 2.
Demographic characteristics of the analytic sample with and without everyday discrimination (N=1410)
| Everyday discrimination | ||||||
|---|---|---|---|---|---|---|
| None (N=475, 34 %) |
Low (N=204, 14%) |
Moderate (N=412, 29%) |
High (N=319, 23%) |
P value | All participants N=1410 |
|
| Age in years M±SD | 22.0±2.0 | 21.9±1.9 | 22.2±2.0 | 22.1±2.0 | .2 | 22.0±2.0 |
| Ethnicity/Race, n (row %) | .3 | |||||
| White | 122 (36) | 60 (17) | 107 (31) | 56 (16) | 345 | |
| Black or African American | 111 (38) | 37 (12) | 90 (29) | 64 (21) | 302 | |
| Hispanic or Latino | 83 (34) | 30 (12) | 67 (28) | 64 (26) | 244 | |
| Asian American | 100 (32) | 49 (16) | 89 (27) | 81 (25) | 319 | |
| Native Hawaiian/other Pacific Islander | 3 (39) | 1 (16) | 3 (31) | 1 (14) | 8 | |
| American Indian/Native American | 16 (29) | 7 (13) | 15 (28) | 17 (30) | 55 | |
| Other | 40 (30) | 20 (14) | 41 (30) | 36 (26) | 137 | |
| Gender, n (row %) | .5 | |||||
| Women | 265 (32) | 120 (14) | 250 (30) | 194 (24) | 829 | |
| Men | 208 (37) | 82 (14) | 160 (28) | 121 (21) | 571 | |
| Not specified | 2 (17) | 2 (18) | 2 (20) | 4 (45) | 10 | |
| SES, n (row %) | .2 | |||||
| Low | 183 (37) | 71 (14) | 143 (27) | 117 (22) | 514 | |
| Low-middle | 101 (33) | 37 (12) | 94 (31) | 77 (24) | 309 | |
| Middle | 80 (36) | 36 (15) | 58 (24) | 58 (25) | 232 | |
| Middle-high | 77 (33) | 38 (17) | 66 (30) | 46 (20) | 227 | |
| High | 34 (26) | 22 (16) | 51 (41) | 21 (17) | 128 | |
| BMI, n (row %) | <.01 | |||||
| <18.5 | 17 (33) | 7 (13) | 18 (34) | 11 (20) | 53 | |
| 18.5-24.9 | 208 (36) | 90 (15) | 190 (33) | 102 (17) | 590 | |
| 25.0-29.9 | 123 (33) | 59 (15) | 100 (25) | 103 (28) | 385 | |
| ≥ 30.0 | 127 (33) | 48 (13) | 104 (27) | 103 (27) | 382 | |
Note: Percentage is weighted to reflect the original population-based sample of EAT 2010, while n represents observed count
SES= socioeconomic status
Everyday discrimination categories: None (everyday discrimination summary score=1.0), low (score 1.3-1.6), moderate (score 2.0-2.6), high (score >3.0)
Among the 475 participants who had not experienced any discrimination, 13% (n=61) reported overeating, and 6% (n=33) reported binge eating. The mean intuitive eating score was 5.8 (SD = 1.7), and the mean mindful eating score was 8.0 (SD = 2.0), where higher scores indicate greater intuitive and mindful eating (Table 3). Proportions of overeating and binge eating increased, and intuitive eating and mindful eating scores decreased, across the everyday discrimination categories (Table 3).
Table 3.
Maladaptive and adaptive eating by experiences of everyday discrimination (N=1410)
| Eating behaviors | ||||
|---|---|---|---|---|
| Maladaptive eating | Adaptive eating | |||
| Everyday discrimination | Overeating n (row %) |
Binge eating n (row %) |
Intuitive eating M±SD |
Mindful eating M±SD |
| None (N=475) | 61 (13) | 33 (6) | 5.8±1.7 | 8.0±2.0 |
| Low (N=204) | 41 (20) | 18 (9) | 5.7±1.9 | 7.6±2.1 |
| Moderate (N=412) | 98 (23) | 58 (14) | 5.4±1.7 | 7.7±1.9 |
| High (N=319) | 93 (29) | 65 (20) | 5.3 ±1.8 | 7.5±2.1 |
Note: Percentage is weighted to reflect the original population-based sample of EAT 2010, while n represents observed count
3.2. Associations between everyday discrimination and maladaptive eating
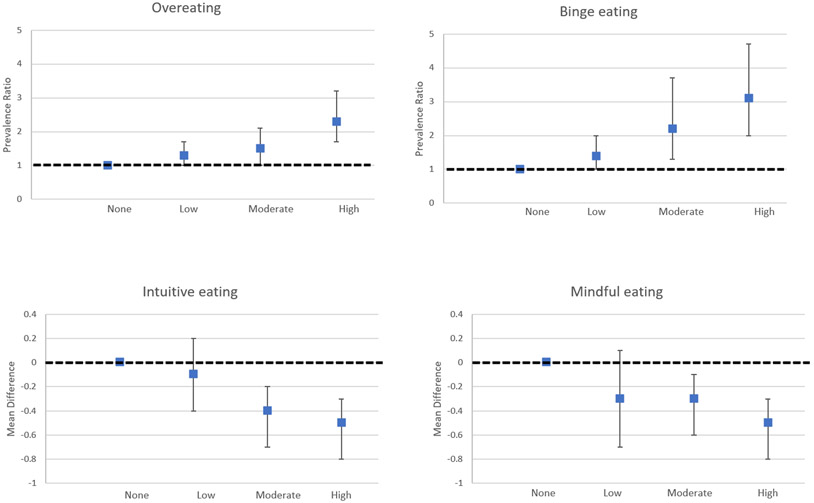
Among young adults, relative to no discrimination, a high level of everyday discrimination was associated with overeating (PR=2.3, [95% CI=1.7-3.2]) after adjustment for sociodemographic variables. High and moderate levels of everyday discrimination were each associated with binge eating (PR=3.1, [95% CI=2.0-4.7] and PR=2.2 [95% CI=1.3-3.7], respectively) (Figure 1, Table 4). Associations of moderate everyday discrimination with overeating and associations of low level of everyday discrimination with overeating and binge eating showed greater prevalence of overeating and binge eating than those with no discrimination, although the point estimates were modest, and the 95% CI overlapped the null value. Little to no change in results was observed after further adjustment for BMI.
Figure 1. Association between experience of everyday discrimination and eating behaviors (N=1410).
Adjusted for age, gender, race, and parental socioeconomic status
Dotted lines refer to the null value
Higher intuitive and mindful eating scores refer to greater intuitive eating and mindful eating
Table 4.
Associations between experience of everyday discrimination and eating behaviors (N=1410)
| Everyday discrimination |
Overeating PR (95% CI) |
Binge eating PR (95% CI) |
Intuitive eating β (95% CI) |
Mindful eating β (95% CI) |
|
|---|---|---|---|---|---|
| Model 1 | None (N=475) | 1.0 (ref) | 1.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Low (N=204) | 1.3 (1.0-1.7) | 1.4 (1.0-2.0) | −0.1 (−0.4, 0.2) | −0.3 (−0.7, 0.1) | |
| Moderate (N=412) | 1.5 (1.0-2.1) | 2.2 (1.3-3.7) * | −0.4 (−0.7, −0.2) * | −0.3 (−0.6, −0.1) * | |
| High (N=319) | 2.3 (1.7-3.2) * | 3.1 (2.0-4.7) * | −0.5 (−0.8, −0.3) * | −0.5 (−0.8, −0.3) * | |
| Model 2 | None (N=475) | 1.0 (ref) | 1.0 (ref) | 0.0 (ref) | 0.0 (ref) |
| Low (N=204) | 1.3 (0.9-1.8) | 1.4 (0.9-2.1) | −0.1 (−0. 5, 0.3) | −0.1 (−0.7, 0.3) | |
| Moderate (N=412) | 1.3 (0.9-2.1) | 2.1 (1.1-4.0) * | −0.4 (−0.7, −0.2) * | −0.4 (−0.7, −0.2) * | |
| High (N=319) | 2.4 (1.6-3.6) * | 3.2 (1.9-5.5) * | −0. 6 (−0.9, −0.3) * | −0. 6 (−0.9, −0.3) * |
Note. PR = prevalence ratio; CI = confidence interval.
denotes statistical significance
Model 1 adjusted for age, race, gender, and parental socioeconomic status
Model 2 adjusted for model 1 and BMI
3.3. Associations between everyday discrimination and adaptive eating
High and moderate levels of everyday discrimination were each associated with lower scores of intuitive eating (β= −0.5 [95% CI = −0.8, −0.3] and β= −0.4 [95% CI= −0.7, −0.2], respectively) and mindful eating (β = −0.5 [95% CI= −0.8, −0.3] and, β= −0.3, [95% CI = −0.6, −0.1], respectively) relative to no discrimination, after the adjustment for sociodemographic variables. Low everyday discrimination was associated with lower scores of intuitive eating and mindful eating than those with no discrimination, although the 95% CI included the null values (Figure 1, Table 4). There was little to no change in the results in the fully adjusted models.
4. Discussion
The objective of the current study was to examine the association of experiences of everyday discrimination with maladaptive and adaptive eating. In this study, we found that experiences of moderate and high levels of discrimination were associated with a greater prevalence of maladaptive eating (i.e., binge eating) and lower scores of intuitive eating (i.e., intuitive eating and mindful eating) compared to no experience of discrimination. Such relationships between discrimination and maladaptive and adaptive eating in this study were maintained even after accounting for BMI, which suggests that the association does not result from those with higher weight statuses both experiencing more discrimination and engaging in certain eating behaviors (14,15).
Our finding of a greater prevalence of maladaptive eating among participants who experienced discrimination aligns with the stress literature suggesting that perceived stress is related to eating disorder pathology, binge eating, and emotional eating (7,9,20,52-55). We further contribute to the literature by reporting significant associations even after adjustment for BMI, which further suggests that everyday discrimination is associated with maladaptive eating, irrespective of body weight. Several theories support our findings by positioning everyday discrimination as a social stressor (14,15) that has serious impacts on health outcomes (56). Stress stemming from everyday discriminatory experiences may trigger negative emotions, decrease self-control capability and impair self-regulation (14), leading individuals to engage in binge eating (9,20) or other uncontrolled eating behaviors, such as emotional eating (7,54,55), to cope with such experiences (16,17). The likelihood of engaging in maladaptive eating may be further exacerbated among individuals who face everyday discrimination due to limited strategies to combat or respond to such events (57,58).
In addition to the findings between everyday discrimination and maladaptive eating, a notable finding of the present study was that experiences of discrimination were associated with lower scores of intuitive eating and mindful eating. Our finding illustrates that everyday discrimination not only trigger engagement in maladaptive eating as a coping strategy but may also operate as barriers for adopting adaptive eating. To the best of our knowledge, only three studies have been conducted to identify predictors of intuitive eating (20,33,34), and while one study has examined the association between perceived stress and intuitive eating (20), no studies have assessed the association of everyday discrimination with intuitive or mindful eating.
Another contribution of our study was the inclusion of both men and women in the examination of the effects of everyday discrimination on maladaptive and adaptive eating. Although prior research has suggested gender differences in responses to perceived stress (59), we found associations of everyday discrimination with maladaptive and adaptive eating to be similar across women and men.
The present student’s strengths include its assessment of everyday discrimination, which is a form of discrimination that has been less frequently studied compared to more major forms of discrimination related to ethnicity/race and weight. In addition to the large number of studies examining the relationship between discrimination and health (8,60,61), we add that everyday discrimination affects eating behaviors. Our study further contributes to understanding of the relationships of daily discrimination experiences with eating behaviors in young adults (aged 18-30 years), a population that has been understudied in assessments of discrimination and eating behaviors. Another strength of our study is the large sample and inclusion of both men and women, which allowed to control for sociodemographic variables and BMI. Using data from a population-based study, rather than from clinical samples, broadens the applicability of our findings to a more generally healthy population. Despite our study’s strengths, we acknowledge several limitations. First, participants were drawn from the Minneapolis-St. Paul metropolitan area, which limits the study’s generalizability to other geographical regions outside of the midwestern United States. Second, experiences of discrimination were retrospectively assessed and self-reported, which raises the possibility of recall bias. Third, the retrospectively assessed experiences of discrimination using three items from the Everyday Discrimination Scale (EDS) short version rather than the full measure further limits our ability to understand how a broader array of everyday discriminatory experiences impacts eating behaviors. Relatedly, the attributions for everyday discriminatory experiences (e.g., weight, race, gender) were not assessed. Thus, our study does not allow us to examine the extent to which the attribution of discrimination may modify the association of discrimination with eating behaviors. Fourth, maladaptive eating behaviors (i.e., overeating and binge eating) were assessed using single yes/no items. Although brief assessment tools are commonly used in large epidemiologic surveys to assess health at a populational level and lessen the burden on participants, the usage of single items such as these may result in measurement errors. Fifth, caution should be exercised in interpreting the results, given that we used a cross-sectional design, which limits our ability to draw longitudinal inferences about exposure to everyday discrimination and eating behaviors. Last, intuitive and mindful eating measures were found to have low internal consistency, which was likely due to the limited numbers of items.
Our study has several implications for future research. The high prevalence of everyday discrimination and its association with maladaptive and adaptive eating indicates that these types of previously understudied experiences deserve greater research attention. Further research is required to examine (1) the underlying causes and nature of everyday discrimination as well as disrespectful attitudes and behaviors against others, (2) the mechanisms underlying the relationships between everyday discrimination and maladaptive and adaptive eating, (3) the identification of individuals who are more likely to be affected by everyday discrimination, and (4) resources and strategies to help develop resilience against the effects of everyday discrimination. For example, studies suggest that social support and coping style (e.g., confrontation, positive reappraisal) are potential moderators of everyday discrimination and depressive symptoms (8). However, whether these findings hold when applied to maladaptive and adaptive eating remains unclear. Identifying moderators may further assist in identifying individuals who are especially vulnerable or resilient to the effects of discrimination on eating behaviors.
Our findings also have several implications regarding clinical practice. Foremost, the finding that everyday discrimination may be a potential risk factor for maladaptive eating and may interfere with adaptive eating highlights the importance of interpersonal discriminatory experiences and developing strategies that target and reduce these maladaptive events in order to support and adopt adaptive eating. This finding further illustrates that it is not sufficient to address these behaviors by focusing only on behavioral change. Support should be offered to ameliorate the impact of stress in the form of everyday discrimination on eating behaviors as well as further assistance in processing and managing reactions to discrimination, which will facilitate the development of resilience and the adoption of adaptive coping strategies.
Given our study’s cross-sectional design, longitudinal studies that examine the association between discriminatory experiences and eating behaviors are necessary. If such studies report similar findings to ours, such findings may further call attention for the heightened need for policies and programs that advocate for equity and inclusion. Furthermore, because everyone may play a role in the existence and occurrence of everyday discrimination and if individuals who experience everyday discrimination are truly engaging in maladaptive eating as a coping mechanism or a reaction to their negative emotions associated with such experiences, our findings may suggest the importance of broadly encouraging more respectful attitudes and behaviors toward others and offering help to individuals who experienced everyday discrimination to be fully equipped to cope with or respond to such experiences.
5. Conclusion
This study provides unique information about the associations of everyday types of discrimination with maladaptive and adaptive eating among young adults. As hypothesized, everyday experiences of discrimination were associated with a greater prevalence of overeating and binge eating and lower scores of intuitive and mindful eating. Therefore, a reduction om discrimination must be considered a main strategic goal to prevent the practice of maladaptive eating and to increase the adoption of adaptive eating.
Funding source
Data collection for the study was supported by Grant Numbers R01HL127077 and R35HL139853 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). Cynthia Yoon’s time was supported by Award Number T32DK083250 (PI: Robert W. Jeffery) from the National Institute of Diabetes and Digestive and Kidney Diseases. Vivienne Hazzard’s time was supported by Award Number T32MH082761 (PI: Scott Crow) from the National Institute of Mental Health. Rebecca Emery’s time was supported by the National Center for Advancing Translational Sciences under TL1 R002493 (PI: Fulkerson) and UL1 TR002494 (PI: Blazar). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institute of Diabetes and Digestive and Kidney Diseases, or National Institute of Mental Health, the National Institutes of Health, or National Center for Advancing Translational Sciences.
Footnotes
Ethics Statement
All research was performed in accordance with the Declaration of Helsinki. The Institutional Review Board Human Subjects Committee at the University of Minnesota approved all protocols used in EAT 2018 and all participants provided informed consent before taking part in study procedures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Luo Y, Xu J, Granberg E, Wentworth WM. A Longitudinal Study of Social Status, Perceived Discrimination, and Physical and Emotional Health Among Older Adults. Res Aging. 2012. May 14;34(3):275–301. [Google Scholar]
- 2.Striegel-Moore RH, Dohm F-A, Pike KM, Wilfley DE, Fairburn CG. Abuse, Bullying, and Discrimination as Risk Factors for Binge Eating Disorder. Am J Psychiatry. 2002;159(11):1902–7. [DOI] [PubMed] [Google Scholar]
- 3.Johnson P, Risica PM, Gans KM, Kumanyika SK. Association of Perceived Racial Discrimination with Eating Behaviors and Obesity among Participants of the SisterTalk Study. J Natl Black Nurses Assoc. 2012;23(1):34–40. [PMC free article] [PubMed] [Google Scholar]
- 4.Longmire-Avital B, Mcqueen C. Exploring a relationship between race-related stress and emotional eating for collegiate Black American women. Women Heal. 2019;59(3):240–51. [DOI] [PubMed] [Google Scholar]
- 5.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of Weight Bias: Implications for Binge Eating and Emotional Well-being. Obesity. 2007. Jan 1;15(1):19–23. [DOI] [PubMed] [Google Scholar]
- 6.Puhl RM, Luedicke J. Weight-Based Victimization Among Adolescents in the School Setting: Emotional Reactions and Coping Behaviors. J Youth Adolesc. 2012. Jan 15;41(1):27–40. [DOI] [PubMed] [Google Scholar]
- 7.Sutin AR, Robinson E, Daly M, Terracciano A, Sutin AR. Weight Discrimination and Unhealthy Eating-related Behaviors. Appetite. 2016;102:83–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pascoe EA, Smart Richman L. Perceived Discrimination and Health: A Meta-Analytic Review. Psychol Bull. 2009;135(4):531–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durso LE, Latner JD, Hayashi K. Perceived Discrimination Is Associated with Binge Eating in a Community Sample of Non-Overweight, Overweight, and Obese Adults. Obes Facts. 2012;5:869–80. [DOI] [PubMed] [Google Scholar]
- 10.Gee GC, Spencer MS, Chen J, Takeuchi D. A Nationwide Study of Discrimination and Chronic Health Conditions Among Asian Americans. Am J Public Health. 2007;97(7):1275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler RC, Mickelson KD, & Williams DR, Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of percieved discrimination in the United States. J Health Soc Behav. 1999;40(3):208–230. [PubMed] [Google Scholar]
- 12.Hunte HER. Original Contribution Association Between Perceived Interpersonal Everyday Discrimination and Waist Circumference Over a 9-Year Period in the Midlife Development in the United States Cohort Study. Am J Epidemiol. 2011;173(11):1232–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Connor DB, Jones F, Conner M, McMillan B, Ferguson E. Effects of Daily Hassles and Eating Style on Eating Behavior. Heal Psychol. 2008. Jan;27:S31. [DOI] [PubMed] [Google Scholar]
- 14.Inzlicht M, Mckay L, Aronson J. Stigma as Ego Depletion How Being the Target of Prejudice Affects Self-Control. Psychol Sci. 2006;17(3):262–9. [DOI] [PubMed] [Google Scholar]
- 15.Major B, O’Brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. [DOI] [PubMed] [Google Scholar]
- 16.Adam TC, Espel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–58. [DOI] [PubMed] [Google Scholar]
- 17.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneumroendocrinology. 2001;26:37–49. [DOI] [PubMed] [Google Scholar]
- 18.Major B, Quinton W, McCoy S. Antecedents and consequences of attributions to discrimination: Theoretical and empirical advances. In: Advances in experimental social psychology. San Diego: Academic Press; 2002. p. 251–300. [Google Scholar]
- 19.Jackson JS, Knight KM, Rafferty JA. Race and Unhealthy Behaviors: Chronic Stress, the HPA Axis, and Physical and Mental Health Disparities Over the Life Course. Am J Public Health. 2010;100(5):933–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arvel € A-Reijonen EJ€, Karhunen L, Sairanen E, Rantala S, Laitinen J, Puttonen S, et al. High perceived stress is associated with unfavorable eating behavior in overweight and obese Finns of working age. Appetite. 2016;103:249–58. [DOI] [PubMed] [Google Scholar]
- 21.Lofgren I. Mindful Eating: An Emerging Approach for Healthy Weight Management. Am J Lifestyle Med. 2015;9(3):212–6. [Google Scholar]
- 22.Denny KN, Loth K, Eisenberg ME, Neumark-Sztainer D, Kara Denny RN. Intuitive eating in young adults: Who is doing it, and how is it related to disordered eating behaviors? Appetite. 2013;60(1):13–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dyke N Van, Drinkwater EJ. Relationships between intuitive eating and health indicators: literature review. Public Health Nutr. 2013;17(8):1757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Camilleri GM, Méjean C, Bellisle F, Andreeva VA, Kesse-Guyot E, Hercberg S, et al. Intuitive eating is inversely associated with body weight status in the general population-based NutriNet-Santé study. Obesity. 2016. May 1;24(5):1154–61. [DOI] [PubMed] [Google Scholar]
- 25.Dalen J, Smith BW, Shelley BM, Sloan AL, Leahigh L, Begay D. Pilot study: Mindful Eating and Living (MEAL): Weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complement Ther Med. 2010;18:260–4. [DOI] [PubMed] [Google Scholar]
- 26.Bacon L, Stern JS, Van Loan MD, Keim NL. Size Acceptance and Intuitive Eating Improve Health for Obese, Female Chronic Dieters. J Am Diet Assoc. 2005;105:929–36. [DOI] [PubMed] [Google Scholar]
- 27.Madden CEL, Leong SL, Gray A, Horwath CC, El Madden C, Leong SL, et al. Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutr. 2012. Dec;15(12):2272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tribole E, & Resch E. Intuitive eating: A recovery book for the chronic dieter. New York: St. Martin’s Press; 1995. [Google Scholar]
- 29.Tylka TL. Development and psychometric evaluation of a measure of intuitive eating. J Couns Psychol. 2006;53(2):226–240. [Google Scholar]
- 30.Hendrickson KL, Rasmussen EB. Effects of mindful eating training on delay and probability discounting for food and money in obese and healthy-weight individuals. Behav Res Ther. 2013;51:399–409. [DOI] [PubMed] [Google Scholar]
- 31.Kristeller J, Wolever RQ, Sheets V. Mindfulness-Based Eating Awareness Training (MB-EAT) for Binge Eating: A Randomized Clinical Trial. Mindfulness (N Y). 2014. Feb 1;5(3):282–97. [Google Scholar]
- 32.Avalos LC, Tylka TL. Exploring a Model of Intuitive Eating With College Women. J Couns Psychol. 2006;53(4):486–97. [Google Scholar]
- 33.Andrew R, Tiggemann M, Clark L. Predictors of Intuitive Eating in Adolescent Girls. J Adolesc Heal. 2015;56:209–14. [DOI] [PubMed] [Google Scholar]
- 34.Nevanpera N, Hopsu L, Kuosma E, Ukkola O, Uitti J, Laitinen J. Occupational burnout, eating behavior, and weight among working women. Am J Clin Nutr. 2012;95:934–43. [DOI] [PubMed] [Google Scholar]
- 35.Larson NI, Wall MM, Story MT, Neumark-Sztainer DR. Home/family, peer, school, and neighborhood correlates of obesity in adolescents. Obesity. 2013;21(9):1858–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Neumark-Sztainer D, Wall MM, Larson N, Story M, Fulkerson JA, Eisenberg ME, et al. Secular trends in weight status and weight-related attitudes and behaviors in adolescents from 1999 to 2010. Prev Med (Baltim). 2012;54(1):77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arcan C, Larson N, Bauer K, Berge J, Story M, Neumark-Sztainer D. Dietary and weight-related behaviors and body mass index among hispanic, hmong, somali, and white adolescents. J Acad Nutr Diet. 2014;114(3):375–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Little RJA. Survey nonresponse adjustments for estimates of means. Int Stat Rev. 1986;54(2):139–57. [Google Scholar]
- 39.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–95. [DOI] [PubMed] [Google Scholar]
- 40.Bucchianeri MM, Eisenberg ME, Neumark-Sztainer D. Weightism, Racism, Classism, and Sexism: Shared Forms of Harassment in Adolescents. J Adolesc Heal. 2013;53:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neumark-Sztainer D, Wall M, Fulkerson JA, Larson N. Changes in the frequency of family meals from 1999-2010 in the homes of adolescents: Trends by sociodemographic characteristics. J Adolesc Heal. 2013;52(2):201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams D, Yu Y, Jackson J. Racial Differences in Physical and Mental Health Socio-economic Status, Stress and Discrimination. J Health Psychol. 1997;2(3):335–51. [DOI] [PubMed] [Google Scholar]
- 43.Sternthal MJ, Slopen N, Williams DR. Racial Disparities in Health: How Much Does Stress Really Matter? Du Bois Rev. 2011;8(1):95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ann & Robert H. Lurie Children’s Hospital of Chicago;, Stanley Manne Children’s Research Institute. Everyday Experiences of Discrimination Among Chicago Parents. 2021. [Google Scholar]
- 45.Taylor RJ, Forsythe-Brown I, Mouzon DM, Keith VM, Chae DH, Chatters LM. Prevalence and correlates of everyday discrimination among black Caribbeans in the United States: the impact of nativity and country of origin. Ethn Heal. 2017. Jul 4;24(5):463–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whitaker KM, Everson-Rose SA, Pankow JS, Rodriguez CJ, Lewis TT, Kershaw KN, et al. Experiences of Discrimination and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). Am J Epidemiol. 2017;186(4):445–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blum R, Harris L, Resnick MRK. Technical Report on the Adolescent Health Survey. Univ Minnesota Adolesc Heal Progr. 1989; [Google Scholar]
- 48.Yanovski S. Questionnaire on Eating and Weight Patterns-Revised (QEWP-R). Obes Res. 1993;1:319–24. [Google Scholar]
- 49.Tylka TL, & Kroon Van Diest AM (2013). The Intuitive Eating Scale–2: Item refinement and psychometric evaluation with college women and men. J Couns Psychol. 2013;60(1):137–153. [DOI] [PubMed] [Google Scholar]
- 50.Framson C, Kristal AR, Schenk J, Littman AJ, Zeliadt S, Benitez D. Development and Validation of the Mindful Eating Questionnaire. J Am Diet Assoc. 2009;109(8):1439–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am J Epidemiol Hopkins Bloom Sch Public Heal All rights Reserv. 2004;159(7):702–6. [DOI] [PubMed] [Google Scholar]
- 52.Kwan MY, Gordon KH, Minnich AM. An examination of the relationships between acculturative stress, perceived discrimination, and eating disorder symptoms among ethnic minority college students. Eat Behav. 2018. Jan 1;28:25–31. [DOI] [PubMed] [Google Scholar]
- 53.Striegel-Moore RH, Dohm F-A, Kraemer HC, Schreiber GB, Taylor CB, Daniels SR. Risk factors for binge-eating disorders: An exploratory study. Int J Eat Disord. 2007. Sep;40(6):481–7. [DOI] [PubMed] [Google Scholar]
- 54.Greeno C, Wing R. Stress-induced eating. Psychol Bull. 1994;115(3):444–64. [DOI] [PubMed] [Google Scholar]
- 55.Groesz L, McCoy S, Carl J, Saslow L, Stewart J, Adler N, et al. What is eating you? Stress and the drive to eat. Appetite. 2012;58:717–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80–94. [PubMed] [Google Scholar]
- 57.Puhl R, Brownell KD. Ways of coping with obesity stigma: review and conceptual analysis. Eat Behav. 2003;4:53–78. [DOI] [PubMed] [Google Scholar]
- 58.Puhl RM, Brownell KD. Confronting and Coping with Weight Stigma: An Investigation of Overweight and Obese Adults*. Obesity. 2006. Oct;14(10):1802–15. [DOI] [PubMed] [Google Scholar]
- 59.Chao A, Grey M, Whittemore R, Reuning-Scherer J, Grilo CM, Sinha R. Examining the mediating roles of binge eating and emotional eating in the relationships between stress and metabolic abnormalities Compliance with ethical standards Conflict of interest HHS Public Access. J Behav Med. 2016;39(2):320–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived Racial/Ethnic Harassment and Tobacco Use Among African American Young Adults. Am J Public Heal Bennett al ∣ Peer Rev ∣ Res Pract. 2005;95(2):238–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carr D, Friedman MA. Is Obesity Stigmatizing? Body Weight, Perceived Discrimination, and Psychological Well-Being in the United States*. J Health Soc Behav. 2005;46:244–59. [DOI] [PubMed] [Google Scholar]
- 63.Jackson SE, Beeken RJ, Wardle J. Obesity, Perceived Weight Discrimination, and Psychological Well-Being in Older Adults in England. Obesity. 2015. May 1;23(5):1105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sutin AR, Terracciano A. Perceived Weight Discrimination and Obesity. PLoS One. 2013;8(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Heal. 2004;35(5):350–9. [DOI] [PubMed] [Google Scholar]
- 66.Sherwood NE, Wall M, Neumark-Sztainer D, Story M for CDC R. Effect of Socioeconomic Status on Weight Change Patterns in Adolescents. Prev Chronic Dis. 2009;6(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- 67.Neumark-Sztainer D, Story M, Hannan PJ, Croll J. Overweight status and eating patterns among adolescents: where do youths stand in comparison with the healthy people 2010 objectives? Am J Public Health. 2002;92(5):844–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gibson R. Principles of nutritional assessment. 2nd edn. New York: Oxford University Press; 2005. [Google Scholar]