Abstract
Background
To determine the incidence of concomitant intra-articular glenohumeral injuries in patients undergoing surgical management from distal clavicle fractures (DCF) with shoulder arthroscopy and their impact on outcome.
Methods
This systematic review was conducted following the PRISMA guidelines. PubMed, EMBASE, and Virtual Health Library databases were accessed in October 2021. All the clinical studies evaluating the surgical management of DCF and using concomitant intra-operatory shoulder arthroscopy were included. Studies that did not specify the concomitant injury type were not eligible. Data from the incidence of intra-articular glenohumeral injuries, injury type, length of the follow-up, and clinical outcomes were retrieved. The quantitative content assessment was performed using the STROBE statement checklist. Evaluation of the publication bias of the included studies was performed using the risk of bias assessment tool for systematic reviews.
Results
Data from five retrospective and five prospective cohort studies were analyzed. Eight of the included studies were conducted on patient cohorts with Neer type II injuries. Data pooling revealed a mean of 17.70% of concomitant glenohumeral injuries, whereas 84.21% of them required additional surgical management (Table 1). Rotator cuff injuries, labral tears, and biceps pulley lesions were the most common concomitant injuries.
Conclusion
Preoperative MRI or diagnostic arthroscopy to evaluate glenohumeral associated injuries to DCF should be recommended.
Keywords: Glenohumeral, Distal clavicle fractures, Arthroscopy
Introduction
Clavicle fractures account approximately 2.6–4% of all fractures in the adult population [1, 2]. Of them, distal clavicle fractures (DCF) account up to 28% [1, 2]. The majority of DCF occur after a direct fall over the shoulder or, in smaller part, after a fall on outstretched hand [3–6]. Management of DCF can be challenging. Most classifications for DCF are mainly based on the configurations of bone fragments (stable or unstable) and the location in relation to the coracoclavicular ligaments [3, 7–10]. Stable lesions can be treated conservatively; however, failing to identify unstable lesions could result in pseudoarthrosis/nonunion and poor shoulder function [11–14]. Several surgical techniques have been described to manage unstable DCF, but to the best of our knowledge, no consensus has been reached [11, 15–18]. Surgical management can be categorized as rigid (locking and hook plates) and elastic (Kirshner-wire fixation, tension band wiring, suture anchors, button suture systems) fracture fixation, or a combination of both. The surgical procedure can be open, arthroscopically assisted, or fully arthroscopic [17, 19].
The incidence of associated lesion after DCF is highly variable [6, 20–24]. Preoperative physical examination to investigate concomitant injuries to DCF can be difficult because of pain and inflammation. Moreover, MRI or diagnostic arthroscopy of the glenohumeral joint to investigate associated is not routinely performed [24]. This systematic review investigated the incidence of concomitant intra-articular glenohumeral injuries in patients undergoing surgical management of DCF using concomitant intra-operative shoulder arthroscopy.
Methods
Search strategy
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [25]. Two independent reviewers (T.M.F., J.M.H.) accessed PubMed, EMBASE, and Virtual Health Library databases in October 2021. The following terms "distal clavicle fracture" and "arthroscopy” were used alone and in combination with the Boolean operators AND and OR. Inclusion and exclusion criteria were established before the search and were used to identify potentially eligible studies by title and abstract screening. Disagreements between reviewers were resolved by a third investigator (E.P.). The bibliography of the included studies was screened by hand to identify additional studies.
Eligibility criteria
All the clinical studies evaluating the surgical management of DCF and using concomitant intra-operatory shoulder arthroscopy were included. Only studies in English were included. Only studies published in peer reviewed journal with a minimum of 5 patients were considered. Reviews, comments, opinions, and editorials were not eligible. Studies which reported data on insolated DCF without arthroscopy were not eligible. Studies which did not specify the concomitant injury type were also not eligible. Studies which reported shoulder injuries associated with DCF in other forms rather than a direct arthroscopic visualization were not included.
Data extraction
Two independent investigators (T.M.F., J.M.H) performed data extraction. Studies generalities (author, year, type of study, and level of evidence) were extracted. Data from the following endpoints were retrieved: number of patients, classification, incidence of intra-articular glenohumeral injuries, injury type, length of the follow-up, clinical outcomes.
Methodological quality assessment
The quantitative content assessment was performed using the Strengthening the Reporting of Observational Studies in Epidemiology: the STROBE statement checklist (SSc) [26].
Assessment of publication bias
Evaluation of the publication bias of the included studies was performed using the risk of bias assessment tool for systematic reviews (ROBIS) [27]. This tool was developed to assess the risk of bias in systematic reviews and meta-analysis. The ROBIS is composed by three parts: (1) assessment of relevance (optional), (2) identification of concerns with the review process (study eligibility criteria; identification and selection of studies; data collection and study appraisal; and synthesis and findings), and (3) evaluation of the risk of bias in the review process, results and conclusions.
Statistical analysis
The statistical analysis was performed using IBM SPSS Version 19 and Microsoft Excel 2016 (Microsoft, USA). Data were presented in tables using absolute values, standard deviations, and percentages from individual studies. Values of P < 0.05 were considered statistically significant.
Results
Search results
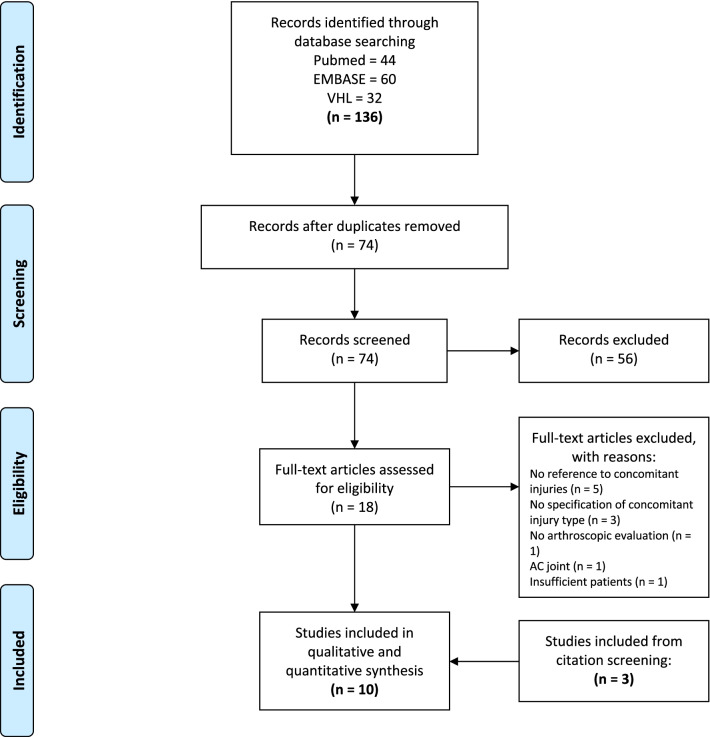
The initial literature search yielded 74 potentially relevant records after the removal of duplicates (N = 27). Titles and abstracts were screened, and 18 articles for full-text evaluation were retrieved. Seven studies met the predetermined eligibility criteria [21–24, 28–30], and three additional studies were included after citation screening [31–33] (Fig. 1). There were five retrospective [21, 24, 28, 31, 32] and five prospective cohort studies [22, 23, 29, 30, 33].
Fig. 1.
Flow chart of the literature search
Methodological quality assessment
The SSc was used to assess the quality of individual studies in the present investigation (Table 1). The average SSc value was 26.30 of 32 (range 22–31), indicating a good quality of the methodological assessment.
Table 1.
STROBE Statement checklist score of included cohort studies
| Study | Years | Level of evidence | Score (max. 32) |
|---|---|---|---|
| Dey Hazra et al. [31] | 2020 | IV | 29 |
| Helfen et al. [24] | 2018 | IV | 31 |
| Kuner et al. [32] | 2018 | IV | 26 |
| Sautet et al. [21] | 2018 | IV | 25 |
| Xiong et al. [29] | 2018 | IV | 29 |
| Blake et al. [22] | 2017 | IV | 22 |
| Cisneros and Reiriz [28] | 2017 | IV | 25 |
| Beirer et al. [23] | 2015 | IV | 26 |
| Kraus et al. [33] | 2015 | IV | 27 |
| Loriaut et al. [30] | 2013 | IV | 23 |
Assessment of publication bias
The risk of bias in the review was low (Fig. 2). A low heterogeneity among the included studies was observed in the arthroscopic assessment of intra-articular glenohumeral concomitant injuries, in the standardization of the surgical procedure, and postoperative management. Most studies clearly defined the type of lesion and referred to standardized classifications.
Fig. 2.
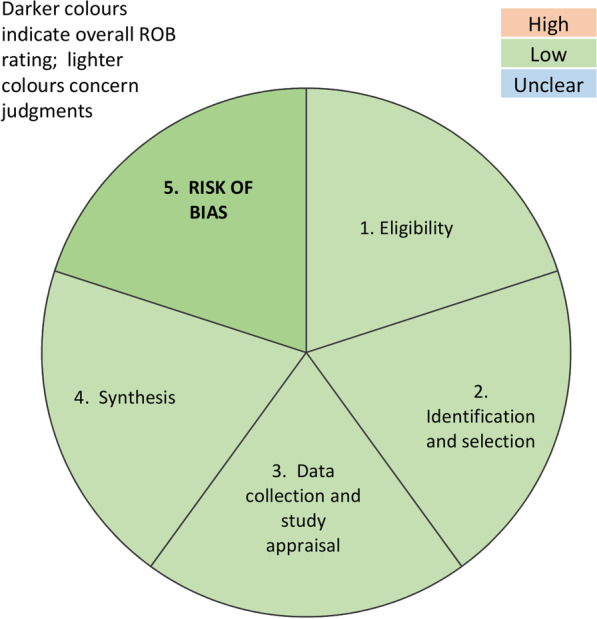
Assessment of publication bias
Synthesis of Results
Eight of the included studies were conducted on patient cohorts with Neer type II injuries [21, 22, 24, 28–30, 32, 33]. Data pooling revealed a mean of 17.70% of concomitant glenohumeral injuries, whereas 84.21% of them required additional surgical management (Table 2).
Table 2.
Incidence of intra-articular injuries in distal clavicular fractures and injury type among the included studies
| Study | Number of patients | Fracture classification | Incidence of intra-articular injuries | Injury type | Follow-up (mean) | Outcomes |
|---|---|---|---|---|---|---|
|
Dey Hazra et al. [31] 2020 Retrospective cohort study |
8 | Jäger and Breitner IIA/Neer IIB | 37.5% (3 patients) |
Labral tear (1) SLAP lesion (1) Pulley lesion (1) Biceps tendon lesion (1) PASTA – Ellman A1 (1) SSC partial rupture – Fox and Romeo 2 (1) SGHL injury (1) |
36 (36.6 ± 14.3) months |
Outcome differences were not evaluated Additional surgical treatment was required in patients with concomitant injuries |
|
Helfen et al. [24] 2018 Retrospective cohort study |
41 | Neer type II | 27% (11 patients) |
SLAP lesion (1) SSP transmural tears (3) SSP partial ruptures (5) SSC partial rupture (1) Pulley lesion (1) Bankart lesions (2) |
12 months |
No outcome differences in Constant score and Oxford shoulder score were found regarding concomitant injuries Additional surgical treatment, other than debridement, was required in 5 patients with concomitant injuries Out of 11 patients with concomitant glenohumeral injuries, five of them were diagnosed during the primary arthroscopy, and six of them during the diagnostic arthroscopy at the time of hardware removal In the subgroup of existing concomitant injuries, out of all measured functional outcome parameters implant removal and late arthroscopy benefitted patients' functional outcomes |
|
Kuner et al. [32] 2018 Retrospective cohort study |
20 | Neer type II | 0% | None | 12–50 (18.7) months | |
|
Sautet et al. [21] 2018 Retrospective cohort study |
14 | Neer type IIb | 0% | None | 6–55 (20) months | |
|
Xiong et al. [29] 2018 Prospective cohort study |
28 | Neer type II | 14.29% (4 patients) |
Bankart lesion (1) Rotator cuff injury (1) Glenolabral articular disruption (1) Acromioclavicular joint arthritis (1) |
7–160 (57) months |
Concomitant injuries were repaired arthroscopically at the time of fracture fixation Rehabilitation time was lengthened in patients with concomitant injuries Outcome differences were not evaluated |
|
Blake et al. [22] 2017 Prospective cohort study |
17 | Neer type II | 0% | None | The mean duration from surgery to the most recent follow-up was 12 months | |
|
Cisneros and Reiriz [28] 2017 Retrospective cohort study |
9 | Neer type IIb | 22.22% (2 patients) | Rotator cuff tears (2) | 46–52 (49) months |
Concomitant injuries were repaired when detected Outcome differences were not evaluated |
|
Beirer et al. [23] 2015 Prospective cohort study |
28 | Jäger and Breitner I, II, and III | 46% (13 patients) |
SLAP (4) Pulley lesions – Habermeyer III (3) PASTA (1) SSC lesion – Fox and Romeo II (1) |
Additional surgical treatment was required in 8 of 13 (61.54%) patients with concomitant injuries Outcome differences were not evaluated |
|
|
Kraus et al. [33] 2015 Prospective cohort study |
20 | Neer type II | 10% (2 patients) | SSC tear – Fox and Romero I and II (2) | 13–38 (23) months |
Patients with concomitant injuries required surgical treatment Outcome differences were not evaluated |
|
Loriaut et al. [30] 2013 Prospective cohort study |
24 | Neer type IIb | 8.33% (2 patients) |
Rotator cuff injury (1) Labral tear (1) |
24–51 (35) months |
Patients with concomitant injuries required surgical repair Outcome differences were not evaluated |
| Total | 209 | 17.70% |
Helfen et al. [24] assessed the clinical outcomes in patients with and without concomitant injuries, finding no differences in Constant and Oxford shoulder score at last follow-up. Xiong et al. [29] reported a prolonged rehabilitation in patients with concomitant injuries. Concomitant glenohumeral injuries were summarized (Table 3).
Table 3.
Distribution of concomitant injuries according to their type in distal clavicular fractures among the included studies
| Injury type (number of injuries) | % |
|---|---|
| ROTATOR CUFF INJURY (19) | 50.00 |
| SSP partial ruptures (5) | 26.32 |
| SSC tears (5) | 26.32 |
| Non-specified (4) | 21.05 |
| SSP transmural tears (3) | 15.79 |
| PASTA (2) | 10.53 |
| LABRAL TEAR (12) | 31.58 |
| SLAP lesion (6) | 50 |
| Bankart lesions (3) | 25 |
| Non-specified (2) | 16.67 |
| Glenolabral articular disruption (1) | 8.33 |
| PULLEY LESION (5) | 13.16 |
| OTHER INJURIES (2) | 5.26 |
| Biceps tendon lesion (1) | |
| SGHL injury (1) |
The bold values correspond to the total of those types of injuries
PASTA: partial articular supraspinatus tendon avulsion; SGHL: superior glenohumeral ligament; SLAP: superior labrum anterior–posterior; SSC: subscapularis; SSP: supraspinatus
Discussion
The present systematic review highlighted that 17.70% of patients with acute DCF evidenced concomitant glenohumeral injuries. Rotator cuff injuries, labral tears, and biceps pulley lesions were the most common concomitant injuries, requiring additional surgical treatment in 84.21% of cases. This incidence is similar to those reported following after acromioclavicular dislocations [20]. This similarity may result from to the similar mechanism of injury [6]. Preoperative MRI or diagnostic arthroscopy to evaluate glenohumeral associated injuries to DCF should be recommended.
The management of concomitant injuries to the DFC have demonstrated clinical improvement and may avoid persistent symptoms and early onset of degenerative changes [34–36]. However, the current evidence is not strong enough to ascertain whether concomitant glenohumeral injuries in DCF may affect the final outcome of management of these injuries.
DCF have been traditionally managed through open approaches with very satisfying outcomes, and further imaging or arthroscopic assessments are related to increased surgical time and costs [28, 37]. However, the acute pain following an acute DCF, or the administration of pain medications, may jeopardize the presence of concomitant shoulder injuries. Therefore, the presence of concomitant injuries should be evaluated using preoperative MRI or diagnostic arthroscopy in patients with DCF. Whether to combine the management of DCF with a simultaneous or delayed additional glenohumeral intervention should be evaluated for each patient, and surgery should be individualized.
This study has several limitations. The small number of included studies and relatively small sample size is the most important limitation of the present systematic review. The retrospective nature of 50% (5 of 10) of included studies increases the risk of selection bias. None of the included studies performed randomization or blinding, thus increasing the risk of detection bias. Most of the included studies were conducted on patients with DCF type II according to the Neer [7]. Thus, results from this systematic review may be not fully generalized. Further high-quality investigations should be performed to overcome current limitations and to evaluate the efficacy and safety of simultaneous glenohumeral interventions.
Conclusion
17.70% of patients with a DCF evidenced concomitant glenohumeral injuries. Rotator cuff injuries, labral tears, and biceps pulley lesions were the most common concomitant injuries, requiring additional surgical treatment in 84.21% of cases. Preoperative MRI or diagnostic arthroscopy to evaluate glenohumeral associated injuries to DCF should be recommended.
Acknowledgements
None.
Abbreviations
- SSc
STROBE statement checklist
- ROBIS
Risk of bias assessment tool for systematic reviews
- PASTA
Partial articular supraspinatus tendon avulsion
- SGHL
Superior glenohumeral ligament
- SLAP
Superior labrum anterior–posterior
- SSC
Subscapularis
- SSP
Supraspinatus
Authors' contribution
TMF: conceptualization, methodology, validation, formal analysis, investigation, data curation, writing—original draft, visualization. FM & EP: validation, resources, writing—review & editing, supervision. KA: validation, resources, writing—review & editing, supervision. DRM: validation, resources, writing—review & editing, supervision. NM & JMH: conceptualization, methodology, validation, formal analysis, investigation, data curation, writing—review & editing, supervision, project administration. All authors have read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial support for the research, authorship, and/or publication of this article.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available throughout the manuscript.
Declarations
Ethics approval and consent to participate
The present study complies with ethical guidelines.
Consent for publication
Not applicable.
Competing interests
Prof. Nicola Maffulli is Editor in Chief of the Journal of Orthopedic Surgery and Research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Theodorakys Marín Fermín, Email: theodorakysmarin@yahoo.com.
Filippo Migliorini, Email: migliorini.md@gmail.com.
Emmanuel Papakostas, Email: epapacostas@gmail.com.
Khalid Al-Khelaifi, Email: khalid.alkhelaifi@aspetar.com.
David Ricardo Maldonado, Email: davidricardoms@gmail.com.
Jean Michel Hovsepian, Email: jmichelh@gmail.com.
Nicola Maffulli, Email: n.maffulli@qmul.ac.uk.
References
- 1.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. doi: 10.1097/00003086-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Robinson CM. Fractures of the clavicle in the adult: epidemiology and Classification. J Bone Jt Surg Ser B. 1998;80(3):476–484. doi: 10.1302/0301-620X.80B3.0800476. [DOI] [PubMed] [Google Scholar]
- 3.Stanley D, Trowbridge E, Norris S. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Jt Surg Br. 1988;70(3):461–464. doi: 10.1302/0301-620X.70B3.3372571. [DOI] [PubMed] [Google Scholar]
- 4.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elb Surg. 2002;11(5):452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 5.Krüger-Franke M, Köhne G, Rosemeyer B. Ergebnisse operativ behandelter lateraler Klavikulafrakturen [Outcome of surgically treated lateral clavicle fractures] Unfallchirurg. 2000;103(7):538–544. doi: 10.1007/s001130050580. [DOI] [PubMed] [Google Scholar]
- 6.Nuber GW, Bowen MK. Acromioclavicular Joint Injuries and Distal Clavicle Fractures. J Am Acad Orthop Surg. 1997;5(1):11–18. doi: 10.5435/00124635-199701000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Neer CS. Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma Inj Infect Crit Care. 1963;3(2):99–110. doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Allman FL. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Jt Surg Am. 1967;49(4):774–784. doi: 10.2106/00004623-196749040-00024. [DOI] [PubMed] [Google Scholar]
- 9.Craig E. Fractures of the clavicle. In: Rockwood F, Matsen C, editors. The shoulder. Philadelphia: WB Saunders; 1990. pp. 367–412. [Google Scholar]
- 10.Cho C-H, Kim B-S, Kim D-H, Choi C-H, Dan J, Lee H. Distal clavicle fractures: a new classification system. Orthop Traumatol Surg Res. 2018;104(8):1231–1235. doi: 10.1016/j.otsr.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131(4):525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 12.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Jt Surg Am. 2004;86(4):778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture: 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64(1):87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 14.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Jt Surg Am. 2004;86(7):1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19(7):392–401. doi: 10.5435/00124635-201107000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Ockert B, Wiedemann E, Haasters F. Laterale Klavikulafraktur. Klassifikationen und Therapieoptionen TT – [Distal clavicle fractures. Classifications and management] Unfallchirurg. 2015;118(5):397–406. doi: 10.1007/s00113-015-0003-1. [DOI] [PubMed] [Google Scholar]
- 17.Sambandam B, Gupta R, Kumar S, Maini L. Fracture of distal end clavicle: a review. J Clin Orthop Trauma. 2014;5(2):65–73. doi: 10.1016/j.jcot.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boonard M, Sumanont S, Arirachakaran A, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(6):1065–1078. doi: 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]
- 19.Vannabouathong C, Chiu J, Patel R, et al. An evaluation of treatment options for medial, midshaft, and distal clavicle fractures: a systematic review and meta-analysis. JSES Int. 2020;4(2):256–271. doi: 10.1016/j.jseint.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruiz Ibán MA, Moreno Romero MS, Diaz Heredia J, Ruiz Díaz R, Muriel A, López-Alcalde J. The prevalence of intraarticular associated lesions after acute acromioclavicular joint injuries is 20%. A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2020;29:2024–2038. doi: 10.1007/s00167-020-05917-6. [DOI] [PubMed] [Google Scholar]
- 21.Sautet P, Galland A, Airaudi S, Argenson J-N, Gravier R. Arthroscopy-assisted fixation of fracture of the distal part of the clavicle by subcoracoid suture and clavicle button. Orthop Traumatol Surg Res. 2018;104(8):1237–1240. doi: 10.1016/j.otsr.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 22.Blake MH, Lu MT, Shulman BS, Glaser DL, Huffman GR. Arthroscopic cortical button stabilization of isolated acute neer type ii fractures of the distal clavicle. Orthopedics. 2017;40(6):e1050–e1054. doi: 10.3928/01477447-20170925-06. [DOI] [PubMed] [Google Scholar]
- 23.Beirer M, Zyskowski M, Crönlein M, et al. Concomitant intra-articular glenohumeral injuries in displaced fractures of the lateral clavicle. Knee Surg Sport Traumatol Arthrosc. 2017;25(10):3237–3241. doi: 10.1007/s00167-015-3875-2. [DOI] [PubMed] [Google Scholar]
- 24.Helfen T, Siebenbürger G, Haasters F, Böcker W, Ockert B. Concomitant glenohumeral injuries in Neer type II distal clavicle fractures. BMC Musculoskelet Disord. 2018;19(1):24. doi: 10.1186/s12891-018-1944-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 26.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 27.Whiting P, Savović J, Higgins JPT, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–234. doi: 10.1016/j.jclinepi.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cisneros LN, Reiriz JS. Management of unstable distal third clavicle fractures: clinical and radiological outcomes of the arthroscopy-assisted conoid ligament reconstruction and fracture cerclage with sutures. Eur J Orthop Surg Traumatol. 2017;27(3):373–380. doi: 10.1007/s00590-017-1925-9. [DOI] [PubMed] [Google Scholar]
- 29.Xiong J, Chen JH, Dang Y, Zhang DY, Fu ZG, Zhang PX. Treatment of unstable distal clavicle fractures (Neer type II): a comparison of three internal fixation methods. J Int Med Res. 2018;46(11):4678–4683. doi: 10.1177/0300060518788245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loriaut P, Moreau PE, Dallaudière B, Pélissier A, Vu HD, Massin P, Boyer P. Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1429–1433. doi: 10.1007/s00167-013-2772-9. [DOI] [PubMed] [Google Scholar]
- 31.Dey Hazra RO, Blach R, Ellwein A, Lill H, Jensen G. 3-Year results of arthroscopic management of lateral clavicle fractures: case series and literature review. Obere Extremität. 2020;15:111–117. doi: 10.1007/s11678-020-00565-1. [DOI] [Google Scholar]
- 32.Kuner E, Beeres FJP, Babst R, Schoeniger R. Which lateral clavicle fractures can be treated by an arthroscopic-assisted endobutton procedure? An analysis of risk factors. Arch Orthop Trauma Surg. 2019;139(3):331–337. doi: 10.1007/s00402-018-3075-x. [DOI] [PubMed] [Google Scholar]
- 33.Kraus N, Stein V, Gerhardt C, Scheibel M. Arthroscopically assisted stabilization of displaced lateral clavicle fractures with coracoclavicular instability. Arch Orthop Trauma Surg. 2015;135(9):1283–1290. doi: 10.1007/s00402-015-2271-1. [DOI] [PubMed] [Google Scholar]
- 34.Millett PJ, Horan MP, Maland KE, Hawkins RJ. Long-term survivorship and outcomes after surgical repair of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2011;20(4):591–597. doi: 10.1016/j.jse.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 35.Sullivan S, Hutchinson ID, Curry EJ, Marinko L, Li X. Surgical management of type II superior labrum anterior posterior (SLAP) lesions: a review of outcomes and prognostic indicators. Phys Sportsmed. 2019;47(4):375–386. doi: 10.1080/00913847.2019.1607601. [DOI] [PubMed] [Google Scholar]
- 36.Björnsson Hallgren HC, Holmgren T. Good outcome after repair of trauma-related anterosuperior rotator cuff tears-a prospective cohort study. J Shoulder Elbow Surg. 2020;S1058–2746(20):30790–30794. doi: 10.1016/j.jse.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 37.Kim DW, Kim DH, Kim BS, Cho CH. Current concepts for classification and treatment of distal clavicle fractures. Clin Orthop Surg. 2020;12(2):135–144. doi: 10.4055/cios20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available throughout the manuscript.